
MVA’s Recovery and Healing at El Paso Back Clinic
Common Motor Vehicle Accidents in El Paso: Recovery and Healing at El Paso Back Clinic®
Motor vehicle accidents, or MVAs, are a big issue in El Paso. This city sits on the border, with lots of trucks and cars zooming on roads like I-10 and Loop 375. Accidents often result from drivers not paying attention, drinking, or speeding. They can lead to injuries like neck pain or broken bones. At El Paso Back Clinic®, we help people heal from these injuries. Our team, led by Dr. Alexander Jimenez, uses integrative chiropractic care. This mixes spine fixes with massage, exercise, and healthy eating tips. It treats the whole body and mind. In this article, we discuss common crashes in El Paso, the harm they cause, and how our clinic supports recovery. We draw on Dr. Jimenez’s expertise at our locations in El Paso, TX.
El Paso has many crashes each year. Recent data shows thousands of wrecks, with injuries and even deaths. The border sees heavy truck traffic, upping the risks. Dust storms or rain-slick roads. Work zones add hazards. Knowing this helps folks drive safely. At El Paso Back Clinic®, we see many patients from these events. Our care focuses on pain relief and full health.
Common Types of Motor Vehicle Accidents in El Paso
El Paso’s roads mix locals, visitors, and cross-border traffic. This leads to jam-ups and crashes. Here are the key types:
- Distracted Driving Accidents: Phones or snacks pull drivers’ eyes from the road. In El Paso, this sparks many wrecks. Texting hits hard at spots like Mesa and Stanton streets. Texas-wide, it caused over 84,000 crashes in one year.
- Drunk or Impaired Driving: Booze or drugs slow folks down. Crashes spike nights and weekends. It’s a top cause in Texas spots like El Paso. They pop up near fun zones like Cincinnati Avenue.
- Speeding-Related Crashes: Too fast means tough stops. It makes up 30% of Texas wrecks. On I-10 and Loop 375, speed leads to bad hits. Winds make it worse.
- Rear-End Collisions: Cars bump backs from close follows or late brakes. Common on Loop 375 in traffic or near shops like Cielo Vista. Distractions or weather help cause them.
- Intersection Crashes: Red-light runs or no yields cause side smacks. Over half happen at crossings like Montana or Zaragoza. The Spaghetti Bowl adds mess. Stop sign skips are big faults.
- Pedestrian Incidents: Walkers get struck when drivers miss spots or speed. Downtown, schools, or UTEP see many. Poor walks led to many deaths lately.
- Truck Accidents: Border hauls mean big trucks everywhere. Thousands cross yearly. Recent counts show many truck wrecks with injuries. Tired drivers, heavy loads, or blind areas cause them. Spots like I-10, US-54, and Loop 375 are hot.
Pile-ups hit in storms on I-10. Lane changes in builds confuse. Hit-runs occur in town. Stay alert, slow down, and watch out for trucks to avoid.
At El Paso Back Clinic®, we treat folks from all these. Our team knows border traffic woes. We offer care plans for quick heals.
Common Injuries Sustained in Motor Vehicle Accidents
MVAs jolt bodies hard. Sudden moves cause hidden hurts. Here are the usual ones:
- Whiplash: Neck snaps cause pain, stiffness, headaches, and dizziness. Top in rear-ends.
- Neck and Back Sprains: Pulls or tears cause pain and reduced movement. Low back twists.
- Soft Tissue Damage: Bruises, rips in muscles. Swell, stiff. Deep ones last.
- Headaches: From whiplash or bumps. They linger.
- Herniated Discs: Spine pads slip, pinch nerves. Pain shoots.
- Fractures: Breaks from hits. Ribs puncture lungs. Bad ones need ops. Limbs, spine too.
- Traumatic Brain Injuries (TBIs): Head knocks cause mix-ups, forgetfulness, and eye issues. Change lives, cost lots.
Shoulders, knees, and inside bleed too. Burns and scars are possible. Trucks crush more. Walkers break bones, heads. Minor ones spark worry or PTSD.
At our clinic, we spot these early. Dr. Jimenez’s team uses checks to plan care.
How These Injuries Occur
Crashes stop or hit fast. Bodies fly in cars. Belts save, but force hurts. Rear-ends jerk heads, stretch necks for whiplash. Sides twist spines for sprains, disc slips. Heads hit for TBIs. Knees dash-bang for sprains. Moves inflame tissues. Trucks smash small cars, break bones. Walkers fly, land hard. Signs may be delayed, so check soon.
We urge quick visits. Our El Paso spots offer fast help.
Integrative Chiropractic Care at El Paso Back Clinic® for MVA Recovery
Our integrative care treats all of you. We fix spines hands-on, easing pain without pills or cuts first. Mixes old ways with massage, PT, and nutrition. Speeds heal, drops swell. Here’s our approach:
- Spinal Adjustments: Move bones right, cut nerve pinch, up move. Great for whiplash, back.
- Massage Therapy: Loosens muscles, breaks scars. Boosts blood, drops swell in tissues.
- Physical Therapy: Builds strong, flexible. Restores after sprains and breaks.
- Nutritional Support: Food advice; adds fight-swell, up mood.
- Other Therapies: Needle work or disc pull. Ease pain, stress.
We speed recovery, hit the body and feelings. Start in 72 hours, best. Stops long pain. Our functional medicine finds roots.
Insights from Dr. Alexander Jimenez and El Paso Back Clinic®
Dr. Alexander Jimenez, DC, APRN, FNP-BC, has headed El Paso Back Clinic® for 30+ years. He excels in MVA, which includes injuries like whiplash and TBIs. We use functional medicine, nutrition, and rehab. Holistic care heals body and mind from trauma. Cases show fast recovery from car and truck hits. Border traffic brings many to us. Our spots at 11860 Vista Del Sol and 6440 Gateway East offer full care. Call 915-850-0900 for help.
Conclusion
El Paso MVAs from busy roads hurt many. From whiplash to TBIs, harms vary. El Paso Back Clinic® gives natural healing. We cut pain, restore movement. See us after crashes. Safe drives prevent woes. Visit elpasobackclinic.com or call for wellness.
References
A2X Law. (n.d.). El Paso car crash statistics. https://www.a2xlaw.com/el-paso-car-crash-statistics
Abrar and Vergara. (n.d.). El Paso car accident statistics. https://theavlawyer.com/el-paso-car-accident-lawyer/statistics/
Altitude Health. (n.d.). Comprehensive care: Integrating chiropractic, physiotherapy, naturopathy, and more for motor vehicle accident recovery. https://www.altitudehealth.ca/comprehensive-care-integrating-chiropractic-physiotherapy-naturopathy-and-more-for-motor-vehicle-accident-recovery/
Amaro Law Firm. (n.d.). El Paso truck accident lawyer. https://amarolawfirm.com/el-paso-truck-accident-lawyer/
Amanda Demanda Injury Lawyers. (n.d.). What Texas cities have the most car accidents?. https://www.callamandademanda.com/blog/tx-cities-most-accidents/
Arnold & Itkin. (n.d.). El Paso truck accident attorneys. https://www.arnolditkin.com/el-paso-personal-injury/truck-accidents/
Azam Injury Law. (n.d.). El Paso motor vehicle accident lawyer – Free help. https://azaminjurylaw.com/area-we-serve/el-paso/motor-vehicle-accident-lawyer/
Dr. Alexander Jimenez, DC, APRN, FNP-BC, IFMCP, CFMP, ATN ♛. (n.d.). LinkedIn profile. https://www.linkedin.com/in/dralexjimenez/
Harmonson Law Firm. (n.d.). El Paso car accident lawyer. https://www.clarkharmonsonattorney.com/el-paso-tx/car-accident-lawyer/
Harmonson Law Firm. (n.d.). El Paso pedestrian accident attorney. https://www.clarkharmonsonattorney.com/el-paso-tx/pedestrian-accident-lawyer/
Injury Medical Clinic PA. (n.d.). Injury specialists. https://dralexjimenez.com/
Inlet Integrated Health Centre. (n.d.). Common injuries from motor vehicle accidents and how chiropractic, physiotherapy, and kinesiology can help. https://www.inletintegratedhealth.com/post/common-injuries-from-motor-vehicle-accidents-and-how-chiropractic-physiotherapy-and-kinesiology-ca
James Kennedy, P.L.L.C. (n.d.). El Paso rear-end collisions attorneys | Free consultation. https://www.epinjury.com/personal-injury/car-accident-crash-wreck/rear-end-collisions
Labinoti Law Firm. (n.d.). El Paso motor vehicle accident attorney. https://www.labinotilaw.com/office-locations/el-paso/personal-injury/motor-vehicle-accident/
MVAMVP. (n.d.). Why chiropractic care is essential after a motor vehicle accident. https://mvamvp.com/why-chiropractic-care-is-essential-after-a-motor-vehicle-accident/
Nix Patterson, LLP. (n.d.). El Paso car accident lawyers. https://nixlaw.com/el-paso/car-accident-lawyers/
Sodhi, R. (n.d.). What you should know about the role of chiropractic and massage in motor vehicle accident recovery. https://www.alwc.ca/role-of-chiropractic-care-and-massage-for-accident-recovery/
Spectrum Therapy Consultants. (n.d.). Motor vehicle accident injuries. https://spectrumtherapyconsultants.com/physical-therapy-services/motor-vehicle-accident-injuries/
The Neck and Back Clinics. (n.d.). Your first chiropractic appointment after a car accident: What to expect and prepare. https://theneckandbackclinics.com/first-chiropractic-appointment/
The Neck and Back Clinics. (n.d.). What are your chiropractic treatment options after a car accident?. https://theneckandbackclinics.com/what-are-your-chiropractic-treatment-options-after-a-car-accident/
The Russo Firm. (n.d.). Where do most El Paso car accidents occur?. https://therussofirm.com/where-do-most-el-paso-car-accidents-occur/

Sports Injuries and How El Paso Back Clinic Heals Athletes
Sports and physical activity are part of everyday life in El Paso. From running and weight training to football, soccer, and basketball, people of all ages stay active year-round. While this active lifestyle is healthy, it also leads to a high number of sports-related musculoskeletal injuries—especially when combined with the region’s heat, rough ground, and uneven terrain.
At El Paso Back Clinic, sports injury care focuses on restoring spinal alignment, joint mobility, muscle balance, and overall movement quality. When chiropractic care is combined with nurse practitioner (NP) support, athletes receive complete, coordinated care that promotes healing, performance, and long-term injury prevention.
Clinical observations from Dr. Alexander Jimenez, DC, APRN, FNP-BC, show that athletes recover more efficiently when spine health, joint mechanics, muscle function, and medical oversight are addressed together rather than separately.
Why Sports Injuries Are So Common in El Paso
El Paso presents unique physical challenges for athletes and active individuals. The environment itself can increase stress on the musculoskeletal system.
Common contributing factors include:
-
High temperatures, which increase fatigue and dehydration
-
Hard and uneven surfaces, stressing feet, ankles, knees, and hips
-
Year-round activity, limiting rest and recovery
-
High-impact sports, such as football and basketball
-
Repetitive movement patterns, common in running and training
When the spine and joints are not moving properly, the body compensates. Over time, these compensations increase injury risk and slow healing (NIAMS, n.d.).
Common Sports-Related Musculoskeletal Injuries Seen in El Paso
Sprains and Strains
Sprains and strains are among the most frequently treated injuries at El Paso Back Clinic.
-
Sprains affect ligaments
-
Strains affect muscles or tendons
Common areas include:
-
Ankles
-
Knees
-
Hamstrings
-
Lower back
These injuries often occur during quick movements, twisting, jumping, or improper warm-ups (Orthospine Centers, n.d.).
Knee Injuries (ACL, Meniscus, Runner’s and Jumper’s Knee)
Knee injuries are especially common in sports that involve cutting, jumping, or sudden stops.
Typical knee problems include:
-
ACL tears
-
Meniscus tears
-
Patellar tendonitis (jumper’s knee)
-
Runner’s knee
Misalignment in the spine, hips, or feet can increase stress on the knee joint, making chiropractic care an important part of recovery (Spectrum Therapy Consultants, n.d.).
Tendonitis and Overuse Injuries
Tendonitis develops when tendons are repeatedly stressed without enough recovery.
Common forms include:
-
Tennis elbow
-
Golfer’s elbow
-
Achilles tendonitis
-
Patellar tendonitis
These injuries often worsen slowly and are common in athletes who push through pain (Woodlands Sports Medicine, n.d.).
Shin Splints and Stress Fractures
Lower-leg injuries are common in runners and field athletes.
These include:
-
Shin splints
-
Foot stress fractures
-
Tibial stress injuries
Hard surfaces, worn footwear, and poor biomechanics increase the risk of these injuries (CTX Foot & Ankle, n.d.).
Hip Labral Tears
Hip labral tears affect the cartilage that stabilizes the hip joint.
Common symptoms include:
-
Deep hip or groin pain
-
Clicking or locking sensations
-
Reduced range of motion
These injuries are common among athletes who frequently twist, pivot, or sprint (Texas Spine Clinic, n.d.).
Rotator Cuff and Shoulder Injuries
Shoulder injuries often occur in athletes who lift, throw, or absorb contact.
Common issues include:
-
Rotator cuff strains or tears
-
Shoulder impingement
-
Joint instability
Shoulder pain is often linked to spinal and postural imbalances that chiropractic care addresses (Marque Medical, n.d.).
Lower Back Pain and Sciatica
Lower back pain is one of the most common complaints among athletes.
Contributing factors include:
-
Muscle strain
-
Core weakness
-
Poor posture
-
Spinal joint restrictions
When spinal alignment is compromised, nerve irritation such as sciatica may occur (Marque Medical, n.d.).
How Chiropractic Care at El Paso Back Clinic Helps Sports Injuries
Chiropractic care at El Paso Back Clinic focuses on restoring proper motion to the spine and joints. This allows the nervous system, muscles, and joints to work together efficiently.
Chiropractic treatment may include:
-
Spinal adjustments
-
Extremity joint adjustments (knees, hips, ankles, shoulders)
-
Soft-tissue therapy
-
Mobility and flexibility work
-
Postural correction
Improving alignment reduces stress on injured tissues and supports natural healing (Vista Hills Chiropractic, n.d.).
Benefits of Chiropractic Care for Athletes
Athletes receiving chiropractic care often experience:
-
Reduced pain and stiffness
-
Improved joint mobility
-
Better balance and coordination
-
Faster recovery times
-
Lower risk of repeat injuries
Clinical experience shows that addressing spinal alignment early improves outcomes across many sports injuries (Jimenez, n.d.).
The Role of Nurse Practitioners in Integrated Sports Injury Care
Nurse practitioners (NPs) play an important role in sports injury management by providing medical oversight and coordination of care.
NPs may assist by:
-
Performing initial evaluations
-
Ordering diagnostic imaging (X-ray, MRI)
-
Managing pain and inflammation
-
Coordinating physical therapy
-
Monitoring healing progress
This medical support ensures injuries are accurately diagnosed and treated safely (NIAMS, n.d.).
Functional and Preventive Approach to Recovery
NPs often use a functional approach that looks beyond the injured area.
This includes evaluating:
-
Movement patterns
-
Training load
-
Nutrition and hydration
-
Sleep and recovery habits
-
Inflammation levels
Addressing these factors helps athletes heal fully and return stronger.
Coordinated Care: Chiropractic, NP, and Rehabilitation
One of the strengths of El Paso Back Clinic is coordinated care. Chiropractic care and NP oversight work together with rehabilitation to create a clear recovery plan.
A coordinated plan may include:
-
Chiropractic adjustments for alignment
-
Rehabilitation exercises for strength and stability
-
Medical monitoring for healing progress
-
Gradual return-to-sport planning
This team-based approach improves outcomes and reduces setbacks (Southwest Chiropractors, n.d.).
PRP Therapy and Advanced Recovery Options
For certain injuries, platelet-rich plasma (PRP) therapy may be recommended.
PRP may support healing for:
-
Tendon injuries
-
Ligament sprains
-
Knee injuries
-
Early osteoarthritis
NPs evaluate whether PRP is appropriate and coordinate care alongside chiropractic treatment and rehabilitation (Desert Institute of Sports Medicine, n.d.).
Clinical Example: Knee Injury Recovery at El Paso Back Clinic
Based on clinical observations from Dr. Jimenez, a typical knee injury recovery plan may include:
-
NP evaluation to diagnose the injury
-
Imaging to assess ligament or cartilage damage
-
Chiropractic care to improve spinal, hip, and knee alignment
-
Rehabilitation exercises to restore strength and stability
-
PRP therapy, when appropriate
-
Performance monitoring to prevent re-injury
This integrated approach supports long-term joint health and athletic performance.
Preventing Future Sports Injuries
Prevention is a major focus at El Paso Back Clinic.
Key strategies include:
-
Proper warm-ups and mobility work
-
Strengthening core and stabilizing muscles
-
Maintaining hydration in hot conditions
-
Correcting posture and movement patterns
-
Allowing adequate recovery time
Chiropractic and NP care help identify small problems before they become serious injuries (Texas Children’s Hospital, n.d.).
Long-Term Benefits of Integrated Sports Injury Care
Athletes who receive integrated care often experience:
-
Faster recovery
-
Fewer recurring injuries
-
Improved flexibility and strength
-
Better overall performance
-
Greater confidence in movement
Treating the spine, joints, muscles, and nervous system together leads to a more complete recovery.
Conclusion
Sports injuries are common in El Paso due to the climate, terrain, and high levels of physical activity. Injuries such as sprains, strains, knee injuries, tendonitis, back pain, and stress fractures can limit performance if not treated properly.
At El Paso Back Clinic, chiropractic care restores alignment and mobility, while nurse practitioners provide diagnostics, medical oversight, and coordinated treatment options. Together, this approach supports full recovery, injury prevention, and long-term performance.
Clinical experience from Dr. Alexander Jimenez shows that athletes recover best when care focuses on the whole musculoskeletal system—not just the painful area.
References
El Paso Center Family & Sports Medicine. (n.d.). Musculoskeletal injuries. https://www.elpasocenterfamilyandsportsmed.com/services/musculoskeletal-injuries
Orthospine Centers. (n.d.). Understanding common sports injuries. https://orthospinecenters.com/understanding-common-spring-sports-injuries-prevention-techniques-and-the-role-of-the-musculoskeletal-system/
Spectrum Therapy Consultants. (n.d.). Sports injuries and physical therapy. https://spectrumtherapyconsultants.com/physical-therapy-services/sports-injuries/
Texas Spine Clinic. (n.d.). Sports injuries. https://www.texasspineclinic.com/sports-injuries/
Gonzalez, C. (n.d.). Sports medicine in El Paso. https://www.carlosgonzalezmd.com/sports-medicine-el-paso.html
Texas Children’s Hospital. (n.d.). Most common sports injuries. https://www.texaschildrens.org/content/wellness/most-common-sports-injuries
NIAMS. (n.d.). Sports injuries. https://www.niams.nih.gov/health-topics/sports-injuries
Marque Medical. (n.d.). Most common sports injuries. https://marquemedical.com/most-common-sports-injuries-by-vanessa-fitzgerald/
Woodlands Sports Medicine. (n.d.). Common sports injuries. https://www.woodlandssportsmedicine.com/blog/6-common-sports-injuries
CTX Foot & Ankle. (n.d.). Top sports injury diagnoses. https://www.ctxfootankle.com/top-sport-injury-diagnoses/
Vista Hills Chiropractic. (n.d.). Sports injury chiropractic care. https://www.vistahillschiropracticelpasotx.com/sports-injury
Desert Institute of Sports Medicine. (n.d.). PRP therapy services. https://desertinstituteep.com/services-1
Jimenez, A. (n.d.). Clinical insights. https://dralexjimenez.com/

Avoiding Common Christmas Accidents This Holiday
Avoiding Common Christmas Accidents: Prevention and Recovery at El Paso Back Clinic®
The Christmas season fills homes with lights, laughter, and loved ones. But it can also bring unexpected risks. From slips on icy paths to burns in the kitchen, holiday accidents happen more often than you might think. In El Paso, Texas, where winter weather can mix with the festive rush, these issues send many seeking help. Distracted or drunk driving spikes too, making roads risky. At El Paso Back Clinic®, we focus on wellness chiropractic care to help you prevent and heal from these mishaps. This article explains common Christmas accidents, their causes, and tips for prevention. It also shows how our integrative approach, led by Dr. Alexander Jimenez, DC, APRN, FNP-BC, offers holistic recovery. Using spinal adjustments, massage, nutritional guidance, and NP-partnered care, we support your body’s natural healing to help you have a pain-free holiday.
Common Christmas Holiday Accidents at El Paso Back Clinic®
At our clinic in El Paso, TX, we see a rise in holiday-related injuries each year. These range from home mishaps to road incidents. Here’s a list of the most common ones we treat.
- Falls: Decorating ladders or icy El Paso sidewalks leads to slips. These cause sprains, fractures, or head trauma. Nationwide, about 160 decorating falls occur daily, accounting for half of decorating injuries. Kids might tumble from unstable trees or during outdoor fun.
- Fires: Faulty lights, dry trees, or candles spark fires. In homes across Texas, Christmas tree fires average 155 per year, causing injuries and property damage. We advise checking decorations to avoid these dangers.
- Burns: Holiday cooking with hot oil or deep fryers can result in scalds. Touching lit decorations adds risk. Turkey fryers alone cause 5 deaths and 60 injuries annually. Even hot foods like fried treats can burn mouths.
- Cuts: Knife slips while wrapping or carving happen often. Broken glass ornaments or toy packaging lead to ER visits – about 6,000 yearly for gift-opening cuts.
- Strains: Lifting decorations, gifts, or snow strains muscles. Back issues account for 15% of holiday accidents, and 11,500 ER visits are due to shoveling. In El Paso, our patients often come in after heavy lifting.
- Alcohol-Related Incidents: Festive drinks cause falls or “holiday heart” – heart rhythm problems from overdrinking. This leads to dizziness and more.
- Food Poisoning: Rushed meals with undercooked food or leftovers breed bacteria. About 48 million cases occur in the U.S. each year, peaking during holidays.
- Injuries Related to Toys and Gifts: Choking on small parts injures 251,700 kids yearly. Faulty gifts cause cuts or trips.
- Distracted or Drunk Driving: Busy El Paso roads see more crashes from texting or drinking. Drunk driving deaths rose to 1,013 in December 2021.
These issues increase ER visits by 5-12% in the U.S. and by over 80,000 in the UK during festivities. At El Paso Back Clinic®, we help locals recover quickly.
Causes of Holiday Injuries Seen at Our Clinic
Many injuries stem from everyday tasks gone wrong. To stop recurrences, we at El Paso Back Clinic® pinpoint these causes.
- Overexertion: Heavy lifting, like trees or bags, strains backs. Bending incorrectly causes 80% of lower back pain. Travel luggage accounts for 72,000 doctor visits each year.
- Cooking: Burns from oils or knives in busy kitchens. One in ten child injuries comes from cooking. Grease fires are frequent.
- Decorating: Ladder falls, electrical shocks, or ornament cuts. Decorating sends 13,000 to ERs yearly. Cord trips cause 2,000 injuries.
- Accidents on the Road or at Home: Distracted driving in El Paso’s traffic or at home. Stress slows reflexes.
Winter sports add 186,000 injuries, though they are less common here. Plants like mistletoe can poison if eaten.
Prevention Tips from El Paso Back Clinic®
Prevent accidents with simple steps. Our team at El Paso Back Clinic® shares these to keep your holidays safe.
- For Falls: Use stable ladders and salt icy paths. Get help when climbing.
- For Fires and Burns: Inspect wires, water trees, and use LED candles. Watch stoves closely.
- For Cuts and Strains: Cut safely and lift with your knees. Team up for heavy items.
- For Alcohol and Driving: Designate a driver or use a ride. Drink moderately.
- For Food and Toys: Cook thoroughly and chill food fast. Pick safe, age-appropriate toys.
Keep a first aid kit handy and manage stress. Visit us for pre-holiday check-ups.
How Integrative Chiropractic Care at El Paso Back Clinic® Helps
If injured, turn to El Paso Back Clinic® for natural healing. Our integrative chiropractic care, in partnership with NPs, treats the whole person. Dr. Alexander Jimenez, with over 30 years in El Paso, observes that holiday injuries often stem from poor posture or stress, leading to misalignment of the spine. We use non-invasive techniques to ease pain without meds or surgery.
- Adjustments for Spinal and Joint Pain: Realign the spine to relieve strain from falls or lifts. This boosts movement and cuts swelling.
- Massage and Physiotherapy for Muscle Problems: Ease tension from overwork. Improves circulation for faster recovery.
- NP-Led Care for Holistic Wellness: Our NPs manage overall health, including burn care and effects of poisoning, with a natural focus.
- Nutrition Guidance: Counter rich holiday foods with diet tips to aid digestion and immunity. Fiber-rich choices help.
- Managing Underlying Conditions: Reduce stress hormones for better sleep and mood. Prevents further harm.
Dr. Jimenez’s team uses functional medicine to develop personalized plans that address issues like sciatica from slips. Chiropractic enhances the nervous system for better health during the holidays.
Enjoy a Healthy Holiday with El Paso Back Clinic®
Make Christmas memorable for the right reasons. Know the risks, prevent them, and seek our care if needed. At El Paso Back Clinic®, we’re here for your wellness. Contact us in El Paso, TX, for expert chiropractic support. Happy holidays!
References
D’Amore Law Group. (n.d.). What are the most common Christmas-related injuries?
Relias. (n.d.). 12 holiday mishaps.
TorkLaw. (n.d.). Top 5 most common accidents during Christmas holidays.
St. John Ambulance. (n.d.). Tinsel trauma: Hazardous Christmas statistics.
Journalist’s Resource. (n.d.). Seasonal holiday injuries: A research roundup.
Bramnick Law. (n.d.). Common Christmas injuries and how to avoid them.
Clark Fountain. (n.d.). The most common injuries during the holiday season.
William D. Shapiro Law, Inc. (n.d.). 5 common holiday injuries and safety tips.
We Can Help Law. (n.d.). The most common Christmas accidents.
DBL Law. (n.d.). Top Christmas injuries.
Santa Rosa Orthopaedics. (n.d.). Keep your holidays merry: How to avoid common holiday accidents.
Knecht Chiropractic Clinic. (n.d.). Top reasons chiropractic care helps through the holidays.
Elite Learning. (n.d.). 10 common holiday injuries and how to avoid them.
UCLA Health. (n.d.). 7 common holiday injuries and accidents (and how to avoid them).
Haffner Law. (n.d.). Common accidents and injuries during the holidays.
PVHMC. (2024). Holiday safety: Protecting yourself during this busy time.
Victoria ER. (n.d.). Holiday injury prevention tips.
Jimenez, A. (n.d.). Injury specialists.
LinkedIn. (n.d.). Dr. Alexander Jimenez, DC, APRN, FNP-BC, IFMCP, CFMP, ATN.

Sports Injury Help Online: Your Virtual Recovery Guide
Fast Sports Injury Help Online: How Telemedicine Guides Diagnosis, Rehab, and Return to Play

A massage therapist treats the injury of a professional athlete at El Paso Back Clinic
Telemedicine is changing how athletes get help after an injury. When a chiropractor and a nurse practitioner (NP) work together online, they can guide recovery from many sports injuries without the need for an in-office visit. This is especially helpful for athletes who travel, live far from clinics, or are balancing school, work, family, and training.
In this article, we’ll break down how an integrated chiropractor–NP telemedicine team can:
-
Do virtual exams from a distance
-
Share treatment plans and coordinate care
-
Support at-home rehab, nutrition, and mental health
-
Help with urgent issues like a possible concussion during games
-
Reduce unnecessary ER visits while still protecting your safety
1. Why telemedicine matters for sports injuries
Telemedicine is more than a video call. It is a structured way to deliver health care at a distance using secure video, phone, apps, and online tools. Johns Hopkins Medicine notes that telemedicine improves comfort, convenience, and access, especially for people who would otherwise struggle to travel or fit visits into a busy schedule. Hopkins Medicine
For athletes, that matters because:
-
Practices and games already take up time.
-
Travel teams may compete hours away from home.
-
Injuries often happen suddenly—during a weekend tournament, camp, or late-night match.
Telehealth physical therapy and sports services now let athletes receive full evaluations and guided rehab sessions from home, with real-time video coaching. SportsMD+1 Research shows telehealth physical therapy is effective for many orthopedic and sports-related conditions, including non-surgical and post-surgical rehab. PMC
At the same time, sports medicine researchers have shown that telehealth can support concussion care, including baseline testing, diagnosis, and follow-up—especially in rural or resource-limited settings. PMC+1
2. What is an integrated chiropractor + NP telemedicine team?
An integrated team means the chiropractor and nurse practitioner work together instead of in separate silos.
-
The nurse practitioner (NP) focuses on your overall health, medical history, medications, imaging, and underlying conditions (like asthma, diabetes, or heart issues).
-
The chiropractor focuses on your spine, joints, muscles, and movement patterns, using guided tests, posture checks, and therapeutic exercises delivered remotely.
In Dr. Alexander Jimenez’s clinical model in El Paso, Texas, the same provider is both a board-certified family nurse practitioner and a chiropractor, which allows one clinician to blend medical and musculoskeletal care through telemedicine for neck pain, low back pain, headaches, and sports injuries. El Paso, TX Doctor Of Chiropractic+2El Paso, TX Doctor Of Chiropractic+2
When the chiropractor and NP are separate providers, they can still share:
-
Notes and findings in the same electronic health record
-
Imaging reports and lab results
-
Exercise programs and rehab goals
-
Messages with athletic trainers, physical therapists, and coaches
This two-pronged approach helps create one unified plan that covers:
-
Medical needs (diagnosis, prescriptions, imaging)
-
Musculoskeletal needs (joint mechanics, muscle balance, posture)
-
Functional goals (return to sport, position-specific demands)
3. How a virtual sports injury exam works
A telemedicine visit is structured and systematic, not just a quick chat.
3.1 Before the visit
You’ll usually:
-
Complete an online intake form about symptoms, past injuries, and sport.
-
Upload any previous X-rays, MRIs, or reports, if available.
-
Test your camera, microphone, and Wi-Fi connection. SportsMD+1
3.2 During the visit: what the NP does
The nurse practitioner can:
-
Take a detailed medical history:
-
How the injury happened
-
Any prior concussions, surgeries, or chronic conditions
-
Current medications and allergies
-
-
Screen for red flags like chest pain, severe shortness of breath, uncontrolled bleeding, or signs of serious head injury. telehealth.hhs.gov+1
-
Order diagnostic imaging (X-ray, MRI, CT) if needed.
-
Write or adjust prescriptions, such as:
-
Pain medications (when appropriate)
-
Muscle relaxants
-
Anti-inflammatory medications
-
-
Coordinate referrals to orthopedics, neurology, or emergency care if telemedicine alone is unsafe. OrthoLive+1
3.3 During the visit: what the chiropractor does
Over secure video, the chiropractor can:
-
Observe posture and alignment (standing, sitting, walking).
-
Guide you through movement tests, for example:
-
Bending, rotating, or side-bending the spine
-
Squats, lunges, or single-leg balance
-
Shoulder or hip range of motion
-
-
Identify pain patterns that suggest sprain, strain, tendinopathy, or joint irritation. sportsandexercise.physio+1
-
Teach safe at-home movements, such as:
-
Gentle mobility drills
-
Core stability exercises
-
Isometrics to protect healing tissue
-
In his telemedicine work, Dr. Jimenez describes using these virtual exams to track changes in pain, strength, and mobility from week to week, adjusting exercise progressions and ensuring athletes are not overloading injured tissue. El Paso, TX Doctor Of Chiropractic+1
3.4 Typical flow of a telemedicine sports injury visit
-
NP and chiropractor (or dual-licensed provider) review your history and goals.
-
Guided movement and functional tests help narrow down the likely diagnosis.
-
The NP decides whether imaging or labs are needed.
-
The chiropractor designs initial movement and pain-reduction strategies.
-
You leave with a clear home plan and follow-up schedule.
4. Building a shared treatment plan online
After the virtual exam, the team builds a plan that blends medical and musculoskeletal care. Telehealth orthopedic and sports practices report four consistent benefits from this style of care: improved access, reduced costs, better quality and safety, and higher patient satisfaction. OrthoLive
Typical parts of a shared plan include:
-
Diagnosis and injury stage
-
Example: Grade I ankle sprain, acute hamstring strain, patellofemoral pain, mild lumbar strain.
-
-
Medical actions (NP)
-
Medication plan
-
Imaging orders
-
Clear guidelines for when to go to urgent care or ER
-
-
Chiropractic and movement actions
-
Joint and spinal stabilization work
-
Mobility and flexibility progression
-
Posture and movement training specific to your sport position
-
-
Rehab schedule
-
How often you meet on video
-
How many daily or weekly exercises
-
When to retest speed, strength, or sport-specific skills
-
Telehealth sports physiotherapy services emphasize that virtual care works best when the athlete receives personalized exercise programs, regular online check-ins, and careful progression from injury to return to play. sportsandexercise.physio+1
5. Conditions that respond well to integrated telemedicine care
Research and real-world practice show that many sports injuries can be evaluated and managed, at least partly, through telemedicine. SportsMD+1
5.1 Common injuries suited for telemedicine
-
Mild to moderate ankle sprains
-
Knee pain related to overuse (patellofemoral pain, mild tendinopathy)
-
Hamstring or quadriceps strains
-
Shoulder overuse injuries (swimmer’s shoulder, rotator cuff strain)
-
Back and neck pain from training load, lifting, or collisions
-
Mild muscle contusions without signs of fracture
Telehealth physical therapy has shown promise in non-operative and post-operative sports rehab, especially when therapists guide exercise, monitor progress, and adjust programs in real time. PMC+1
5.2 How the NP and chiropractor divide roles
The NP can:
-
Confirm whether the injury is stable enough for home care.
-
Check for other health issues (asthma, heart conditions, bleeding disorders).
-
Manage medications and monitor side effects.
The chiropractor can:
-
Analyze movement patterns that caused or worsened the injury.
-
Design sport-specific rehab drills (for pitchers, runners, lifters, etc.).
-
Coordinate with physical therapists and athletic trainers to align load, volume, and recovery strategies. El Paso, TX Doctor Of Chiropractic+1
Dr. Jimenez’s clinical work often combines telemedicine visits with in-clinic follow-ups, advanced imaging review, and collaboration with physical therapy and sports training teams to keep athletes progressing without re-injury. El Paso, TX Doctor Of Chiropractic+1
6. Telemedicine and concussion: quick decisions from a distance
Concussions and suspected head injuries are a special case. A missed or delayed diagnosis can put an athlete at serious risk.
A systematic review found that telehealth has been used successfully for concussion baseline testing, diagnosis, and management, especially in military and rural settings. PMC+1 Another review focused on sideline telehealth, where sports medicine physicians assist trainers in real time through video connections during games. PMC+1
SportsMD describes “teleconcussion,” where athletes can quickly access concussion specialists via telehealth instead of waiting days or weeks for in-person care. SportsMD
6.1 How telemedicine helps when you suspect a concussion
During or shortly after a game, a telemedicine visit can help:
-
Review how the head impact occurred (direct hit, whiplash, fall).
-
Check acute symptoms, such as:
-
Headache
-
Dizziness
-
Nausea or vomiting
-
Vision changes
-
Confusion or memory loss
-
-
Guide a brief neurological exam and balance checks via video. PMC+1
-
Decide whether the athlete must leave the game immediately and seek emergency care.
Telemedicine programs in school sports have also been used to minimize risk by providing teams with rapid access to sports medicine expertise, rather than relying solely on coaches to decide whether a player is safe to continue. NFHS+1
6.2 Role of the integrated team
-
The NP can determine whether emergency imaging or ER evaluation is needed, arrange teleconcussion follow-ups, and manage symptom-relief medications when appropriate.
-
The chiropractor can later help with neck pain, posture, and vestibular-related issues—such as balance and coordination problems—once the acute phase is stable and medical clearance is given.
7. At-home rehab and return-to-play through telemedicine
Telehealth lets rehab follow you to your home, hotel room, or training camp.
Telehealth physical therapy programs show several key benefits: increased accessibility, reduced travel burden, and the ability to continue personalized plans even when athletes are on the road. SportsMD+2SportsMD+2
7.1 Common tele-rehab tools
An integrated chiropractor–NP team may use:
-
Video exercise sessions where the provider:
-
Demonstrates exercises
-
Watches your form from different angles
-
Makes real-time corrections
-
-
Secure messaging for quick questions about pain flare-ups or modifications. ATI+1
-
Remote monitoring apps, where you log:
-
Pain levels
-
Step counts or training minutes
-
Completion of home exercises
-
-
Progress checks every 1–2 weeks to advance the plan or adjust if pain increases.
7.2 Examples of tele-rehab goals
-
Acute phase (first days)
-
Protect the injured area
-
Control swelling and pain
-
Maintain gentle mobility where safe
-
-
Subacute phase (1–4 weeks)
-
Restore the normal range of motion
-
Begin light strengthening and balance work
-
Fix faulty movement patterns
-
-
Return-to-play phase
-
Add power, agility, and sport-specific drills
-
Monitor for any return of pain or instability
-
Clear the athlete for full competition once the criteria are met
-
Telehealth sports physio services emphasize a “injury to return-to-play” continuum, where the same remote team oversees each phase to avoid gaps in care. sportsandexercise.physio+1
8. Lifestyle, nutrition, and mental health support from afar
Sports injuries are never just physical. Pain, sudden time off from sport, and stress about losing a starting spot can weigh heavily on athletes.
Telemedicine makes it easier to address the whole person, not just the injured body part:
-
Nutrition – Remote visits can cover:
-
Protein and calorie needs during healing
-
Anti-inflammatory food choices
-
Hydration strategies for training and games SportsMD+1
-
-
Sleep and recovery habits – Online coaching about sleep routines, stretching, and scheduling lighter days can support healing. SportsMD
-
Mental health – some telemedicine platforms connect athletes with sports psychologists or counselors for stress, anxiety, or mood changes after injury. Programs that highlight telemedicine for athlete health care note that virtual visits help athletes stay engaged in care without derailing their training or school schedules. Nully Medical LLC+2Nully Medical LLC+2
In Dr. Jimenez’s integrative model, telemedicine visits often combine pain management, mobility training, nutritional guidance, and coaching on long-term wellness so that athletes return to sport stronger and healthier, not just “cleared.” El Paso, TX Doctor Of Chiropractic+2LinkedIn+2
9. Benefits for remote and traveling athletes
Telemedicine is especially valuable if you:
-
Live in a rural area with limited access to sports medicine. Hopkins Medicine+1
-
Travel often for tournaments, camps, or professional seasons. Nully Medical LLC+1
-
Have trouble arranging rides, time off work, or childcare. Hopkins Medicine+1
Telehealth platforms built for sports and orthopedic care highlight these advantages:
-
Faster access to specialists who may be in another city or state. OrthoLive+1
-
Fewer missed practices or school days.
-
Less time sitting in traffic or waiting rooms.
-
Continuous oversight of rehab, even during road trips. SportsMD+1
In school and youth sports, telemedicine programs have also been used to minimize risk by providing real-time medical input during events and improving response to injuries. NFHS+1
10. When telemedicine is not enough: red flags
Telemedicine is powerful, but it is not a replacement for emergency or in-person care when certain warning signs are present. National telehealth guidance stresses that some situations require hands-on exams or urgent evaluation. telehealth.hhs.gov+1
If you experience any of the following, seek in-person or emergency care immediately:
-
Loss of consciousness, seizure, or severe confusion after a hit to the head
-
Repeated vomiting, severe headache, or worsening neurologic symptoms
-
Clear deformity of a bone or joint, or inability to bear weight at all
-
Suspected fracture with severe swelling or visible misalignment
-
Chest pain, shortness of breath, or signs of allergic reaction
-
Suspected spinal injury with numbness, weakness, or loss of bowel/bladder control
In these cases, telemedicine can still play a role after emergency care—for follow-up visits, rehab planning, and coordination between specialists, the NP, and the chiropractor. PMC+1
11. Clinical observations from Dr. Alexander Jimenez, DC, APRN, FNP-BC
Dr. Alex Jimenez’s clinics in El Paso integrate telemedicine, chiropractic care, and nurse practitioner services for personal injury and sports trauma. His clinical experience offers several practical insights: El Paso, TX Doctor Of Chiropractic+2El Paso, TX Doctor Of Chiropractic+2
1. Telemedicine speeds up early decisions.
Athletes can be evaluated within hours of an injury—sometimes the same day—without waiting for an in-person slot. This helps determine quickly whether an athlete can manage at home, needs imaging, or must seek urgent or emergency care.
2. Dual-scope evaluation reduces gaps.
Because Dr. Jimenez is both a chiropractor and an NP, he can:
-
Interpret imaging and lab results
-
Address inflammation, pain, and sleep issues medically
-
Analyze biomechanics, joint function, and movement patterns
-
Coordinate with attorneys and athletic organizations when injuries occur in organized sports or school settings El Paso, TX Doctor Of Chiropractic+1
3. Telemedicine helps keep athletes compliant.
Through secure messaging and remote check-ins, many athletes are more likely to complete their exercises and follow nutrition or recovery plans. This lines up with broader telehealth research showing high patient satisfaction and good adherence when care is accessible and flexible. OrthoLive+1
4. Hybrid care works best.
Dr. Jimenez often uses a hybrid model: telemedicine for triage, education, home-based rehab progressions, and imaging review, plus targeted in-clinic visits for hands-on care when necessary. This mirrors national trends where telemedicine is integrated into, not replacing, in-person sports and orthopedic care. El Paso, TX Doctor Of Chiropractic+1
12. Practical tips for athletes using telemedicine for sports injuries
To get the most out of a telemedicine visit with an NP and chiropractor, prepare like you would for a big game.
Before your visit
-
Write down:
-
When and how the injury happened
-
What makes it better or worse
-
Medications and supplements you take
-
-
Set up your space:
-
Good lighting
-
Enough room to walk, squat, or lie down
-
A stable surface for your phone or laptop
-
-
Have gear ready:
-
Resistance bands or light weights (if you have them)
-
A chair, wall, or countertop for balance work
-
During your visit
-
Be honest about your pain level and limitations.
-
If you are worried about a concussion, clearly describe all symptoms, even if they seem minor. SportsMD+1
-
Ask about clear return-to-play criteria:
-
Pain goals
-
Strength targets
-
Functional tests (jumping, sprinting, cutting)
-
After your visit
-
Follow the home exercise program and track your progress.
-
Use the patient portal or app to ask questions if pain changes or if you have trouble with a movement. ATI+1
-
Schedule regular follow-up telehealth visits so your plan can be adjusted as you improve.
13. Putting it all together
An integrated chiropractor and nurse practitioner telemedicine team gives athletes a powerful, flexible way to:
-
Get fast evaluations after a sports injury
-
Receive coordinated medical and musculoskeletal care
-
Follow individualized rehab plans at home
-
Access nutrition and mental health support
-
Lower the chance of unnecessary ER visits, while still protecting safety
From major health systems like Johns Hopkins to specialized sports platforms, and from youth leagues to professional levels, the evidence continues to grow that telemedicine—when used wisely—can make sports medicine more accessible, more coordinated, and more athlete-friendly. InjureFree+3Hopkins Medicine+3OrthoLive+3
In real-world practice, clinicians like Dr. Alexander Jimenez show how blending chiropractic care, nurse practitioner expertise, and telemedicine can keep athletes moving forward—even when they are injured, on the road, or far from a clinic. El Paso, TX Doctor Of Chiropractic+2El Paso, TX Doctor Of Chiropractic+2
References
Hasselfeld, B. W. (2025). Benefits of telemedicine. Johns Hopkins Medicine. Hopkins Medicine
InjureFree Team. (2024). Technology Fridays “Breaking boundaries – the power of telemedicine in sports expertise at your fingertips!”. InjureFree. InjureFree
Kim, B. I., et al. (2022). Telehealth physical therapy for sports medicine and orthopedic care. Journal of Telemedicine and Telecare. (Summary from PMC article). PMC
National Federation of State High School Associations. (2015). Telemedicine programs provide latest in risk minimization. NFHS. NFHS
Nully Medical LLC (Savoie, L.). (2025). The power of telemedicine in athlete health care. Nully Medical. Nully Medical LLC+1
Sports & Exercise Physio. (n.d.). Telehealth physiotherapy for sports injuries. Retrieved December 3, 2025. sportsandexercise.physio
SportsMD Editors. (2023). Concussion urgent care specialist near you – consider teleconcussion. SportsMD. SportsMD
SportsMD Editors. (2025). The benefits of telehealth physical therapy. SportsMD. SportsMD+2SportsMD+2
Subramanyam, V., et al. (2021). The role of telehealth in sideline management of sports-related injuries. Current Sports Medicine Reports. PMC+1
Telehealth.hhs.gov. (2025). Telehealth for physical therapy: Getting started. U.S. Department of Health and Human Services. telehealth.hhs.gov
Toresdahl, B. G., et al. (2021). A systematic review of telehealth and sport-related concussion: Baseline testing, diagnosis, and management. Orthopaedic Journal of Sports Medicine. PMC+1
Jimenez, A. (2025a). How Dr. Alex Jimenez uses telemedicine, chiropractic, and NP care to treat pain. DrAlexJimenez.com. El Paso, TX Doctor Of Chiropractic
Jimenez, A. (2025b). Telemedicine injury care: Virtual assessments and follow-up. DrAlexJimenez.com. El Paso, TX Doctor Of Chiropractic
Jimenez, A. (2025c). How telemedicine keeps injury patients on track: Clinical and legal benefits. LinkedIn. LinkedIn
Jimenez, A. (n.d.). El Paso, TX Doctor of Chiropractic. DrAlexJimenez.com. Retrieved December 3, 2025. El Paso, TX Doctor Of Chiropractic
Ortholive. (2018). Five ways telehealth helps sports doctors improve their practice. OrthoLive Blog. OrthoLive
Ortholive. (2021). How can telehealth help the orthopedic practice?. OrthoLive Blog. OrthoLive
Cora Physical Therapy. (2024). How telehealth physical therapy works. CORA Blog. CORA Physical Therapy
ATI Physical Therapy. (n.d.). Online physical therapy services. Retrieved December 3, 2025. ATI

Integrative Chiropractic Therapy Telemedicine Guide
Integrative Chiropractic Therapy Meets Telemedicine: A Path to Better Pain Relief

A doctor of chiropractic and a nurse practitioner show a patient an X-ray image of the spine post-slip and fall injury
In today’s fast-paced world, many people deal with ongoing pain or injuries that disrupt daily life. Neck aches from desk work, throbbing headaches that won’t quit, or sore muscles from weekend sports can make simple tasks feel overwhelming. That’s where integrative chiropractic therapy steps in, blending hands-on adjustments with modern tools like telemedicine and nurse practitioner support. This approach lets patients get expert care without always leaving home, making treatment easier and more effective.
People often search for ways to manage these issues without relying solely on pills or surgery. Integrative chiropractic therapy combines spinal alignments and muscle work with virtual check-ins and personalized plans from nurse practitioners. Telemedicine adds the convenience of video calls and app-based tracking, allowing real-time tweaks to exercises or lifestyle tips. This mix eases symptoms and builds long-term habits for staying healthy (Mayo Clinic, 2023).
Dr. Alexander Jimenez, a chiropractor and board-certified family nurse practitioner, has seen this firsthand in his practice. With over 30 years of experience, he notes that patients with busy schedules love how virtual sessions keep them on track without missing work. “By linking chiropractic adjustments with remote monitoring, we address the whole person—not just the pain,” Jimenez shares on his professional site (Jimenez, n.d.a).
What Is Integrative Chiropractic Therapy?
Integrative chiropractic therapy goes beyond basic back cracks. It pulls together different health tools to resolve problems at their source. Think of it as a team effort: chiropractors handle spine and joint fixes, nurse practitioners check meds and overall health, and telemedicine keeps everyone connected from afar.
This method shines for everyday woes like stiff necks or lower back twinges. Patients receive in-person tweaks when needed, along with online follow-ups to track progress. Studies show this blend cuts pain faster than solo treatments, thanks to better teamwork among providers (Dallas Accident and Injury Rehab, n.d.).
Key Parts of the Approach
- Chiropractic Adjustments: Gentle pushes to realign the spine, easing nerve pressure and boosting movement.
- Nurse Practitioner Input: Pros who review symptoms, adjust plans, and spot when extra tests are needed.
- Telemedicine Tools: Apps for logging pain levels, video chats for quick advice, and wearables that share data like steps or posture.
One big win? It fits real life. A working parent with chronic neck pain can chat virtually with a nurse while doing home stretches guided by a chiropractor. This setup has grown popular since the pandemic, with more clinics offering hybrid options (National Academy of Medicine, 2023a).
Dr. Jimenez often highlights that his dual role as DC and FNP-BC enables him to spot links between spine issues and factors such as poor sleep or diet. In one case, he used telemedicine to guide a patient through posture fixes after a car accident, blending virtual coaching with occasional office visits (Jimenez, n.d.b).
The Rise of Telemedicine in Health Care
Telemedicine has changed how we think about doctor visits. No more long waits in stuffy rooms—just a quick video link from your couch. For pain and injury care, it’s a game-changer, letting experts review your form during exercises or adjust plans based on daily logs.
This tech isn’t new, but its use exploded during COVID-19. Now, it’s standard for follow-ups, especially when travel is tough. Clinics use secure portals for sharing X-rays or symptom updates, making care feel seamless (Mayo Clinic, 2023).
Benefits for Busy Lives
- Saves Time: Skip the drive; log in from anywhere with Wi-Fi.
- Better Tracking: Devices send real-time info on pain or activity, helping pros spot patterns early.
- Safer Access: Great for those in rural areas or with mobility limitations, cutting infection risks, too.
Research backs this up. A review found that telemedicine boosts patient adherence to pain plans, leading to quicker relief (Alhowimel et al., 2024). Plus, it teams up well with chiropractic work, where virtual sessions reinforce hands-on gains.
In Dr. Jimenez’s view, telemedicine shines for ongoing issues like sports strains. “We can watch a patient’s squat form live and correct it on the spot, preventing re-injury,” he posts on LinkedIn (Jimenez, n.d.c).
How Nurse Practitioners Fit In
Nurse practitioners (NPs) are like bridges in health care. Trained in both nursing and advanced practice, they handle exams, prescribe meds, and team with specialists. In integrative setups, NPs monitor how chiropractic tweaks affect overall health, like checking blood pressure after neck adjustments.
Their role grows as telemedicine expands, with them leading virtual visits. This means faster answers on whether pain signals something bigger, plus tweaks to home routines. NPs also focus on prevention, suggesting diet changes or stress tips alongside spine work (Health Coach Clinic, 2023).
Ways NPs Enhance Care
- Full Check-Ups: Review history and symptoms via video, and order tests as needed.
- Med Management: Adjust anti-inflammatories or pain relievers based on progress.
- Holistic Advice: Link pain to lifestyle, like how poor sleep worsens migraines.
This teamwork cuts errors and boosts results. For instance, an NP might flag inflammation from lab results, while a chiropractor eases the joint strain. Dr. Jimenez, as an FNP-BC, uses this daily: “My nursing background lets me see the full picture, ensuring safe, rounded care” (Jimenez, n.d.a).
Conditions That Thrive with This Integrated Approach
This combination of chiropractic, NPs, and telemedicine directly addresses common pain points. It works best for issues where movement, monitoring, and mindset all play a part. Let’s break down key ones.
Cervical and Lumbar Pain
Neck (cervical) and low back (lumbar) pain hit millions yearly, often from slouching at desks or heavy lifting. Integrative care starts with adjustments to straighten the spine, easing nerve pinches. Telemedicine follows up with posture videos and exercise demos, while NPs track inflammation via apps.
Patients see big wins: less stiffness, better mobility. A study showed that VR-guided exercises via telehealth reduced low back pain by 30% in 4 weeks (Alhowimel et al., 2024). Home setups let folks practice daily, with virtual nudges keeping them motivated.
Dr. Jimenez notes, “For lumbar issues like sciatica, we blend decompression therapy with remote nerve checks—patients report walking easier sooner” (Jimenez, n.d.b).
- Quick Tips for Home Relief:
- Gentle neck rolls during video calls.
- Lumbar stretches tracked via phone apps.
- NP-guided heat packs for flare-ups.
Chronic Migraines
Those pounding headaches can sideline anyone. Triggers like tension or poor alignment respond well to chiropractic neck work, which cuts attack frequency by up to 75% in some cases (El Paso Back Clinic, n.d.). Telemedicine adds migraine logs and trigger alerts, with NPs suggesting meds or hydration plans.
Virtual sessions teach relaxation techniques, such as audio-guided breathing exercises. This mix not only douses the fire but also prevents sparks. Research links it to fewer ER trips (Mayo Clinic, 2023).
In practice, Dr. Jimenez uses functional assessments to tie migraines to gut health, adjusting diets remotely: “Telemedicine lets us fine-tune triggers without delay” (Jimenez, n.d.c).
Athletic Injuries
From twisted ankles to pulled hamstrings, sports mishaps need quick, smart fixes. Chiropractors realign joints, NPs handle swelling with meds, and telemedicine coaches rehab moves. Wearables track healing and flag overdoing-it moments.
This approach speeds the return to play. For sudden strains, virtual evals spot issues early and blend with in-person therapy (Health Coach Clinic, 2023). One review praised telerehab for muscle recovery, noting that it matched the results of in-office treatment (Alhowimel et al., 2024).
Dr. Jimenez, working with athletes, says, “Post-game video reviews catch imbalances fast, keeping injuries from lingering” (Jimenez, n.d.a).
- Rehab Musts:
- Balance drills via app timers.
- Strength logs shared with NPs.
- Gradual return plans discussed live.
Chronic Pain Management
Lingering aches from old injuries or daily wear demand steady care. Hybrid models combine relief adjustments with telehealth monitoring to detect patterns. NPs weave in non-drug options like mindfulness apps, cutting reliance on opioids (National Academy of Medicine, 2023a).
Outcomes? The results include improved sleep, elevated mood, and enhanced function. Studies show hybrid care halves pain scores over time (National Academy of Medicine, 2023b).
Osteoarthritis Woes
Joint wear, like knee or hip osteoarthritis, stiffens life. Chiropractic eases alignment, physical therapy builds support via virtual guides, and NPs manage flare meds. This trio slows progression, boosting daily ease (Grace Medical Chiro, n.d.).
Dr. Jimenez adds nutrition tweaks: “Anti-inflammatory foods, tracked remotely, pair perfectly with joint work” (Jimenez, n.d.b).
- Daily Joint Helpers:
- Low-impact walks with step counters.
- Heat therapy reminders from apps.
- NP check-ins for supplement fits.
Dizziness and Balance Blues
That woozy feeling from neck kinks or inner ear glitches? Adjustments free nerves, exercises via telehealth, steady steps, and NPs rule out other causes. Integrated plans restore confidence fast (Grace Medical Chiro, n.d.).
Real-Life Wins: Patient Stories and Expert Insights
Meet Sarah, a teacher with lumbar pain from hauling books. Traditional visits clashed with her schedule, but switching to hybrid care changed everything. Weekly video tweaks to her stretches, plus NP med reviews, dropped her pain from 8/10 to 3/10 in two months. She describes the experience as having a personal coach at her side.
Or take Mike, an avid runner sidelined by shin splints—an athletic injury classic. Dr. Jimenez’s team used telemedicine for gait analysis, blending chiropractic realigns with home drills. NPs monitored swelling remotely. Back on track in weeks, Mike credits the seamless flow.
These aren’t rare. Clinics report 80% satisfaction with hybrid models, thanks to flexibility (Dallas Accident and Injury Rehab, n.d.). Dr. Jimenez’s observations align: “In my El Paso practice, we’ve treated thousands via this method, seeing faster heals and happier lives” (Jimenez, n.d.a). His LinkedIn shares cases like TBI recovery, where posture videos aid brain rehab (Jimenez, n.d.c).
Challenges and How to Overcome Them
No system is perfect. Tech glitches or spotty internet can be frustrating, especially in rural areas. Plus, not all pains suit screens—some need hands-on feels (National Academy of Medicine, 2023b).
Solutions? Start with simple audio calls for low-bandwidth spots. Training helps patients navigate apps, and hybrid options ensure in-person when key. Policies that promote fair access, such as subsidy programs, level the field (National Academy of Medicine, 2023a).
Dr. Jimenez directly addresses this issue by providing loaner devices and step-by-step guides to ensure that no one is left behind (Jimenez, n.d.b).
Common Hurdles and Fixes
- Tech Barriers: Use voice-only options; provide tutorials.
- Privacy Worries: Stick to HIPAA-secure platforms.
- Equity Gaps: Partner with community groups for device loans.
The Future: Smarter, Wider Reach
Looking ahead, AI could predict flare-ups from app data, while VR amps up the fun of exercise. More states are approving cross-border telehealth, thereby expanding its reach (Alhowimel et al., 2024).
For chronic pain and injuries, this means fewer hospital stays and more empowered patients. Equity pushes, like audio-only coverage, ensure everyone benefits (National Academy of Medicine, 2023a).
Dr. Jimenez envisions: “With functional medicine at the core, we’ll prevent more than we treat, using telehealth to scale wellness” (Jimenez, n.d.c).
Wrapping Up: Your Next Step to Pain-Free Days
Integrative chiropractic therapy with NPs and telemedicine isn’t a fad—it’s a smart, proven path to handling cervical pain, migraines, injuries, osteoarthritis, dizziness, and more. It blends the best of touch and tech for real relief.
Ready to try? Chat with a provider about hybrid options. Small steps, like logging daily aches, can spark significant changes. As Dr. Jimenez puts it, “Healing starts with connection—virtual or not” (Jimenez, n.d.a).
References
Alhowimel, A. S., Alodaibi, F., Shirazi, S. A., Alharthi, S., Alqahtani, B., & Alrawaili, S. (2024). Innovative applications of telemedicine and other digital health solutions in pain management: A literature review. Journal of Pain Research, 17, 2563–2583. https://doi.org/10.2147/JPR.S473619
Dallas Accident and Injury Rehab. (n.d.). Integrating chiropractic care with other treatments. Comfort Rehab & Chiropractic Center of Cedar Hill. https://dallasaccidentandinjuryrehab.com/integrating-chiropractic-care-with-other-treatments/
El Paso Back Clinic. (n.d.). Integrative chiropractic care benefits in El Paso. https://elpasobackclinic.com/integrative-chiropractic-care-benefits-in-el-paso/
Grace Medical Chiro. (n.d.). Why combining different treatments works better. https://gracemedicalchiro.com/combining-different-treatments-works-better/
Health Coach Clinic. (2023). Connected care: Telemedicine and patient convenience. https://healthcoach.clinic/connected-care-telemedicine-and-patient-convenience/
Jimenez, A. (n.d.a). Injury specialists. DrAlexJimenez.com. https://dralexjimenez.com/
Jimenez, A. (n.d.b). Integrative chiropractic care benefits in El Paso. El Paso Back Clinic. https://elpasobackclinic.com/integrative-chiropractic-care-benefits-in-el-paso/
Jimenez, A. (n.d.c). Dr. Alexander Jimenez DC, APRN, FNP-BC, IFMCP, CFMP, ATN ♛ – Injury Medical Clinic PA. LinkedIn. https://www.linkedin.com/in/dralexjimenez/
Mayo Clinic. (2023). Telehealth: Technology meets health care. https://www.mayoclinic.org/healthy-lifestyle/consumer-health/in-depth/telehealth/art-20044878
National Academy of Medicine. (2023a). Integrating telehealth and traditional care in chronic pain management and substance use disorder treatment: An action agenda for building the future state of hybrid care. https://nam.edu/perspectives/integrating-telehealth-and-traditional-care-in-chronic-pain-management-and-substance-use-disorder-treatment-an-action-agenda-for-building-the-future-state-of-hybrid-care/
National Academy of Medicine. (2023b). Integrating telehealth and traditional care in chronic pain management and substance use disorder treatment [PDF]. https://nam.edu/wp-content/uploads/2023/10/Integrating-Telehealth-and-Traditional-Care-1.pdf

Telemedicine in Integrative Injury Care Benefits
The Role of Telemedicine in Integrative Injury Care at El Paso Back Clinic: Providing Full Support for Car Accident, Work, and Sports Injuries in El Paso, TX
A doctor of chiropractic and a nurse practitioner review the MRI of a patient following a motorcycle collision.
In El Paso, TX, getting injured in a car crash, at work, or during sports can be tough. But at El Paso Back Clinic®, a top wellness chiropractic care spot, new tools like telemedicine make getting help simpler. Telemedicine uses video calls and online apps to let health experts care for you from home. This article explores how the clinic’s integrative nurse practitioner (NP) and chiropractor team up with telemedicine to provide comprehensive injury care. This covers virtual check-ups, treatment planning, and long-term help. It’s super useful for folks who can’t easily move or get to the clinic. The team also shares tips on eating, working out, and daily habits to speed up healing. They keep everything organized and documented for the best outcomes.
El Paso Back Clinic® focuses on functional medicine and holistic healing. Led by Dr. Alexander Jimenez, who is both a chiropractor (DC) and a family nurse practitioner (FNP-BC), the clinic combines conventional medicine with natural approaches to treat injuries. Telemedicine here means you can get exams, diagnoses, and follow-ups without leaving home. This is great for busy El Paso residents or for those who are hurting too much to travel. The clinic’s approach considers your whole body, with the NP and chiropractor working together to create plans that fit your life.
What Is Integrative Care at El Paso Back Clinic?
At El Paso Back Clinic®, integrative care means a team of doctors, therapists, and nutritionists working together to fully heal you. For car accident injuries like whiplash or back strains, the chiropractor adjusts your spine while the NP manages pain and checks for deeper issues. They make custom plans using evidence-based methods.
- Common Injuries Treated: Neck pain from crashes, work lifts causing strains, or sports-related twists leading to sprains.
- Why Choose Integrative?: It targets the cause, not just pain, blending adjustments with lifestyle changes.
- Telemedicine’s Role: Allows remote care, so you start healing right away from home.
This method helps with lasting health. For sports fans in El Paso, tips on better nutrition can speed up recovery (Dallas Accident and Injury Rehab, n.d.).
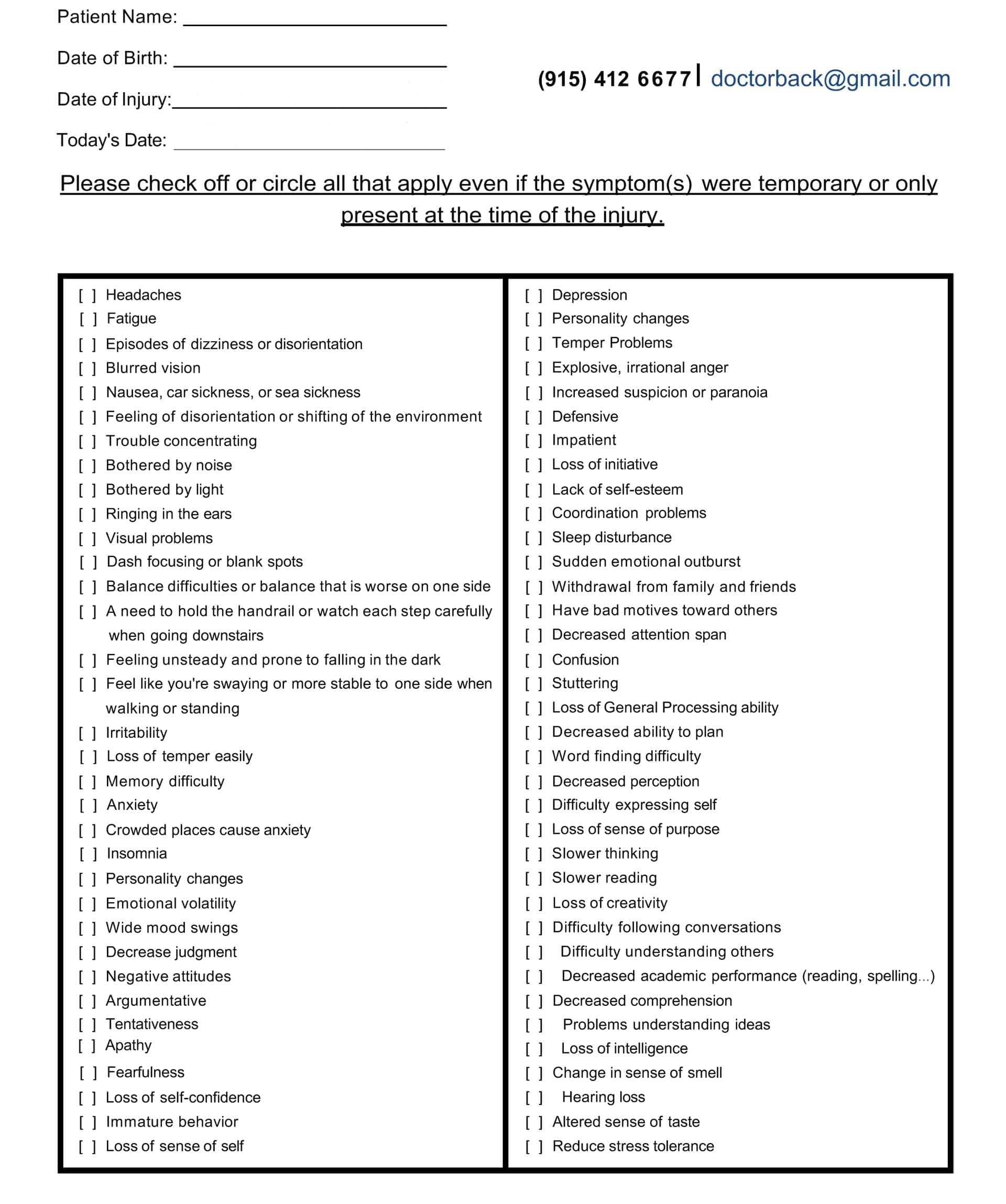
Head Injury/Traumatic Brain Injury Symptom Questionnaire
Virtual Examinations: How El Paso Back Clinic Does It Remotely
Telemedicine at El Paso Back Clinic® starts with virtual exams. You connect via secure video from your phone or computer. Dr. Jimenez or the team talks to you about your injury.
For a car accident, they ask about the crash and pain spots. They watch you move, like bending or walking, to check for swelling or stiffness. Even without hands-on involvement, they spot many problems, such as muscle pulls or nerve issues (Personal Injury Firm, 2025).
Work injuries, like slips, get quick virtual checks to stop things from getting worse. The chiropractor guides home tests, such as balance checks.
- Tools in Virtual Exams: Video for movement, apps for sharing photos of injuries, or devices for vital signs.
- When It’s Not Enough: Some need in-person touches, so they schedule clinic visits at their El Paso locations.
- Sports Injury Perks: Athletes demo their moves, helping find repeat strains.
This remote setup makes getting checked easy, especially in El Paso, where traffic can be a hassle (CK Firm, 2024).
Diagnoses Through Telemedicine at the Clinic
After the exam, the team at El Paso Back Clinic® diagnoses remotely. Common ones from car accidents include whiplash or disc problems. The NP might order X-rays or MRIs, which are performed locally and shared online.
Chiropractors like Dr. Jimenez spot spinal shifts that can cause leg pain, such as sciatica. They explain it clearly on video. The NP assesses whole-body health, including whether swelling worsens.
All sessions are recorded for official documents, insurance keys, or personal injury claims (ChiroMed, n.d.).
- Diagnosis Examples: Work-related back pain, sports-related nerve hits, and crash-neck strains.
- Team Collaboration: NP handles meds; chiropractor does adjustments.
- Tips for Accuracy: Describe pain and show motions well.
This reduces wait times, allowing you to start your El Paso recovery sooner (Complete Care, n.d.).
Managing Treatment Plans Remotely from El Paso Back Clinic
The NP and chiropractor create a treatment plan together, updated via telemedicine. For a sports knee sprain, it might include rest, ice, and shown exercises.
Dr. Jimenez demonstrates stretches on camera. The NP monitors pain and adjusts treatments.
They coordinate to avoid overlaps. For work injuries, plans cover safe job returns. Everything’s online for easy tracking.
- Plan Essentials: Pain relief, movement work, and prevention advice.
- Integrative Touches: Diet tweaks to cut swelling, like more omega-3 foods.
- Telemedicine Updates: Regular video calls to tweak based on progress.
This saves time and money for El Paso patients (Jimenez, n.d.-a).
Ongoing Support and Follow-Up Care at the Clinic
Recovery needs steady help, and El Paso Back Clinic® uses telemedicine for easy follow-ups. Log in to chat about how you’re doing.
For car crash back pain, they check therapy effects and offer encouragement. Support includes mental health tips, as injuries can stress you.
Chiropractors guide home exercises on video. NPs watch for treatment side effects.
- Support Types: Mood talks, progress logs, specialist referrals.
- How Often: Weekly, early on, then less.
- For El Paso Athletes: Safe return-to-play tips, like warm-ups.
This prevents pain from lasting, helping you get back to life fast (Prescient National, n.d.).
Benefits for El Paso Residents with Mobility or Access Issues
Injuries make moving hard, especially in spread-out El Paso. Telemedicine brings care to you.
No travel needed, perfect for remote areas or difficult days. For work injuries, it means less downtime. See pros from home.
- Who Gains Most: Those pained by walking, without transport, or packed schedules.
- Access Help: Shorter waits than office visits.
- Legal Benefits: Docs care for claims without hold-ups.
This makes healing equal for all in El Paso (CK Firm, 2024).
Integrative Advice on Diet, Exercise, and Lifestyle from the Clinic
El Paso Back Clinic® shines with holistic telemedicine tips. They suggest anti-inflammatory foods, such as fruits, to aid healing.
Exercise advice includes easy yoga for pain, demonstrated online. Lifestyle shifts cover better sleep or stress cuts, like apps for calm.
For sports, they teach form to prevent re-injury.
- Diet Ideas: Omega-3 for nerves, antioxidants for fixes.
- Workout Suggestions: Stretches for range, walks for build-up.
- Life Changes: Posture tweaks, drop bad habits.
This addresses root causes for better long-term health (Dallas Accident and Injury Rehab, n.d.).
Coordination and Documentation Between NP and Chiropractor at El Paso Back Clinic
The team shares notes easily on telemedicine platforms. Dr. Jimenez, as both NP and chiropractor, bridges the roles seamlessly.
Records from calls build your file, showing progress for insurance or courts.
Therapies align, like adjustments with rest plans.
- Coordination Methods: Shared digital files, joint calls.
- Record Value: Shows timely, excellent care.
- Your Part: Update honestly for the top plans.
This leads to smooth recoveries in El Paso (Jimenez, n.d.-b).
Insights from Dr. Alexander Jimenez at El Paso Back Clinic
Dr. Alexander Jimenez, DC, APRN, FNP-BC, shares hands-on views from over 30 years at El Paso Back Clinic®. He uses telemedicine for same-day injury exams, like after crashes or sports.
He stresses integrative care for body and mind. For head injuries, he advises sleep, diet, and exercise. His dual license allows him to prescribe medications and adjust spines remotely when possible.
Jimenez highlights tests, such as MRIs, shared online. He combines adjustments in nutrition with other interventions for issues like gut health post-trauma.
- Main Observations: Injuries are linked to overall health, like nerves and digestion.
- Telemedicine in Practice: Quick virtual help for accidents, with shipped braces.
- Tips: Use posture drills and supplements for healing.
His approach shows how the clinic’s NP-chiropractor team excels (Jimenez, n.d.-a; Jimenez, n.d.-b; Jimenez, n.d.-c).
Challenges and Future of Telemedicine at El Paso Back Clinic
Telemedicine has limits, such as the need for touch for some exams. Tech glitches can happen.
But the future is promising. Better apps and AI will improve diagnoses. More insurance covers it.
The clinic trains in remote teamwork.
- Fixing Issues: Have in-person backups, help with tech.
- Coming Trends: Wearables for live data.
- Importance: Makes care more accessible and affordable in El Paso.
Conclusion
At El Paso Back Clinic® in El Paso, TX, telemedicine transforms injury care for car, work, or sports-related injuries. The integrative NP and chiropractor team, led by Dr. Jimenez, offers virtual exams for ongoing support. It includes holistic advice for better living. Ideal for mobility challenges. As Dr. Jimenez proves, this leads to quicker, fuller healing. If injured, reach out to El Paso Back Clinic® for easy, top-notch care at 915-850-0900 or visit their site.
References
Jimenez, A. (n.d.-a). El Paso, TX, doctor of chiropractic. https://dralexjimenez.com/












