Contents
What Is Functional Medicine?
What is it and why do we need it?
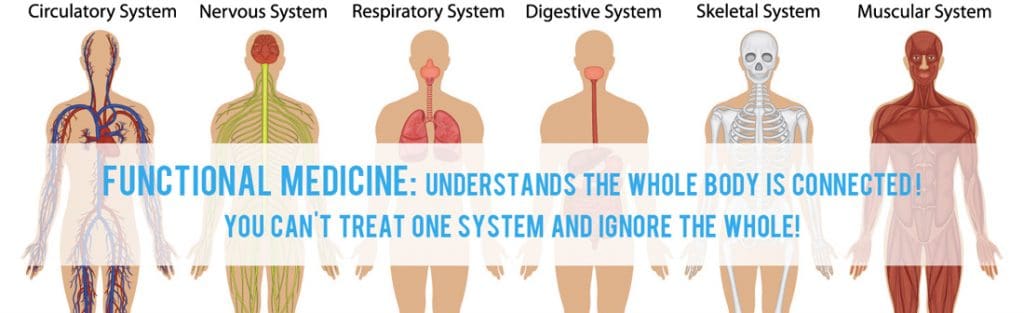
Functional medicine is an evolution in the practice of medicine that better addresses the healthcare needs of the 21st century. By shifting the traditional disease-centered focus of medical practice to a more patient-centered approach, functional medicine addresses the whole person, not just an isolated set of symptoms. Functional medicine practitioners spend time with their patients, listening to their histories and looking at the interactions among genetic, environmental, and lifestyle factors that can influence long-term health and complex, chronic disease. In this way, functional medicine supports the unique expression of health and vitality for each individual.
By changing the disease-centered focus of medical practice to this patient-centered approach, our physicians are able to support the healing process by viewing health and illness as part of a cycle in which all components of the human biological system interact dynamically with the environment. This process helps to seek and identify genetic, lifestyle, and environmental factors that may shift a person�s health from illness to well-being.
Why Do We Need Functional Medicine?
- Our society is experiencing a sharp increase in the number of people who suffer from complex, chronic diseases, such as diabetes, heart disease, cancer, mental illness, and autoimmune disorders like rheumatoid arthritis.
- The system of medicine practiced by most physicians is oriented toward acute care, the diagnosis and treatment of trauma or illness that is of short duration and in need of urgent care, such as appendicitis or a broken leg.
- Unfortunately, the acute-care approach to medicine lacks the proper methodology and tools for preventing and treating complex, chronic disease.
- There�s a huge gap between research and the way doctors practice. The gap between emerging research in basic sciences and integration into medical practice is enormous�as long as 50 years� particularly in the area of complex, chronic illness.
- Most physicians are not adequately trained to assess the underlying causes of complex, chronic disease and to apply strategies such as nutrition, diet, and exercise to both treat and prevent these illnesses in their patients.
How Is Functional Medicine Different?
What is it and why do we need it?
| How is Functional Medicine Different?
Functional medicine involves understanding the origins, prevention, and treatment of complex, chronic disease. Hallmarks of a functional medicine approach include:
|
Why Do We Need Functional Medicine?
- Our society is experiencing a sharp increase in the number of people who suffer from complex, chronic diseases�such as diabetes, heart disease, cancer, mental illness, and autoimmune disorders like rheumatoid arthritis.
- The system of medicine practiced by most physicians is oriented toward acute care,�the diagnosis and treatment of trauma or illness that is of short duration and in need of urgent care, such as appendicitis or a broken leg. Physicians apply specific, prescribed treatments such as drugs or surgery that aim to treat the immediate problem or symptom.
- Unfortunately, the acute-care approach to medicine lacks the proper methodology and tools for preventing and treating complex, chronic disease.�In most cases it does not take into account the unique genetic makeup of each individual or factors such as environmental exposures to toxins and the aspects of today�s lifestyle that have a direct influence on the rise in chronic disease in modern Western society.
- There�s a huge gap between research and the way doctors practice.�The gap between emerging research in basic sciences and integration into medical practice is enormous�as long as 50 years�particularly in the area of complex, chronic illness.
- Most physicians are not adequately trained to assess the underlying causes�of complex, chronic disease and to apply strategies such as nutrition, diet, and exercise to both treat and prevent these illnesses in their patients.
How is Functional Medicine Different?
Functional medicine involves�understanding the�origins, prevention, and treatment�of complex, chronic disease. Hallmarks of a functional medicine approach include:
- Patient-centered care.�The focus of functional medicine is on patient-centered care, promoting health as a positive vitality, beyond just the absence of disease. By listening to the patient and learning his or her story, the practitioner brings the patient into the discovery process and tailors treatments that address the individual�s unique needs.
- An integrative, science-based healthcare approach.�Functional medicine practitioners look �upstream� to consider the complex web of interactions in the patient�s history, physiology, and lifestyle that can lead to illness. The unique genetic makeup of each patient is considered, along with both internal (mind, body, and spirit) and external (physical and social environment) factors that affect total functioning.
- Integrating best medical practices.�Functional medicine integrates traditional Western medical practices with what is sometimes considered �alternative� or �integrative� medicine, creating a focus on prevention through nutrition, diet, and exercise; use of the latest laboratory testing and other diagnostic techniques; and prescribed combinations of drugs and/or botanical medicines, supplements, therapeutic diets, detoxification programs, or stress-management techniques.
Functional medicine is more than just a different approach to healthcare, it is an entirely different philosophy about how we both provide and consume healthcare.� I can honestly say that in my practice, I don�t treat diseases, but rather I treat patients; some of whom have diseases and some do not.� I focus on normalizing the underlying physiology and restoring healthy function through nutrition and lifestyle changes.
People often have significant symptoms and they feel sick, but they don�t meet the technical requirements for a particular diagnosis.� In many offices this means that they don�t get any treatment at all, but for my patients, this is just the beginning.� I work with my patients to discover the dysfunctional patterns that lead to their symptoms, and then develop strategies to correct these patterns and restore optimal health. �
The functional medicine approach to the treatment of chronic disease is one that is based not on one agent or modality as the curative or palliative solution. It is holistically centered on the principle that restoration of proper cellular metabolism, through reducing cumulative toxic load and oxidative stress to the body, will allow normalization of mitochondrial respiration, cellular energy production, and ultimately to a reduction of the signs and symptoms of chronic disease. While many nutritionally-oriented doctors realize that standard nutritional support protocols alone are quite beneficial for cases of mild to moderate chronic disease, more severe cases often require a more comprehensive functional approach.
This functional medicine philosophy and approach was initially developed for clinical use in chronic fatigue patients with excellent results, and because of the commonality observed in many chronic conditions, it has been used over the years in other disorders with great success, including fibromyalgia, rheumatoid arthritis, and auto-immune disorders.1-8 The seminal work of Bland, Rigden, Cheney, and others in the treatment of chronic fatigue syndrome has served as a successful template, and this approach is now used in the treatment of a broad range of chronic diseases1-7.
The functional medicine philosophy is centered on the premise that a breakdown of the intestinal mucosa by the chronic ingestion of food and water-based toxins, and the use of common prescription and over-the-counter drugs (such as antibiotics and NSAIDS), can lead to dysbiosis and a hyperpermeable intestinal mucosa, or leaky gut syndrome. This intestinal hyperpermeablility can result in the intestinal mucosa failing to act as a selective barrier, leading to the crossing of food-based toxins and partially digested food proteins through the intestinal mucosa and into the systemic blood supply. The eventual result is an increase in food allergies and increased toxic load. (see Figure 1).
This increased toxic load can, over time, lead to increased stress on the liver and its ability to adequately detoxify these substances through phase I and II pathways. This will ultimately result in increased systemic tissue toxicity.
Increased tissue toxicity is thought to be a major trigger for mitochondrial dysfunction, which results in an inability of the body’s cells, including the muscle cells, to efficiently utilize oxygen dependent aerobic metabolic pathways. This accounts for the majority of ATP production. Decreased cellular ATP production can account for many (if not all) of the symptoms and signs associated with many chronic disease states, such as chronic fatigue syndrome (CFS) and fibromyalgia (FMS).
Increased intestinal permeability can also result in partially digested medium to large food proteins entering the blood supply and acting as antigens. The resulting antigen-antibody complexes seem to have an affinity for the synovium of articulations, This results in an inflammatory response in the joint linings commonly seen in arthritidies such as rheumatoid arthritis (RA). The main therapeutic agents used initially by standard medical physicians in the treatment of RA are (ironically) NSAIDs. NSAIDs, according to the PDR, result in increased intestinal permeability. Is it possible that the traditional allopathic treatment for arthritidies has only resulted in palliating the patient’s symptoms, while actually exacerbating the disease?
The functional medicine therapeutic strategy is, therefore, centered around repairing the intestinal mucosa, correcting any intestinal dysbiosis, providing substances to the body to aid tissue detoxification, reducing oxidative stress, and ultimately promoting a return of normal cellular metabolism. Assessment begins by determining intestinal health and the functional reserve of the liver and its detoxification abilities. This is commonly done with the help of patient symptom questionnaires, such as the a metabolic screening questionnaire and functional laboratory studies, such as the lactulose/mannitol challenge for evaluating intestinal permeability, and the complete digestive stool analysis (CDSA) for detecting markers of digestion, absorption, and colonic flora. Detoxification ability of the liver can be assessed via the caffeine clearance and conjugation metabolite challenge tests, which evaluate phase I (cytochrome P450) and phase II (conjugation) liver detoxification pathways (see Figure 2). These tests are not performed by standard clinical laboratories, but are available through specialized laboratories who offer functional testing.9
Once the data is collected, a treatment program (see Figure 3) is selected, which may include specific nutrients to correct any intestinal hyperpermeability (leaky gut syndrome). Individual nutrients such as L-glutamine, purified hypoallergenic rice proteins, inulin, pantothenic acid, and antioxidants can be used, however, a formulary medicinal food10,11 is usually much easier and more practical to use clinically. Digestion and absorption difficulties suggested on the CDSA can be treated with the temporary use of pancreatic enzymes and HCL (if indicated) in patients without gastritis or ulcers. Dysbiosis, a term used to describe an imbalance of colonic flora, can be addressed by the administration of lactobacillus acidophilus and probiotics such as fructooligosaccharides (FOS).
Any pathogenic bacteria, yeast, or parasites detected on the CDSA should be treated with the prescription (or natural) agents suggested by the sensitivity tests on the CDSA. These may include nonprescription substances such as berberine, garlic, citrus seed extract, artemisia, uva ursi, and others. This program of gut restoration is described by Bland, Rigden, Cheney, and others as the “Four R’ approach.3-4.
“Four R” Approach to Gastrointestinal Restoration
Remove: Eradicate any pathogenic microflora, yeast and/or parasites with natural or prescription agents suggested on the CDSA (i.e., berberine/goldenseal, garlic, artemesia, citrus seed extract, uva ursi, etc.).
Eliminate known allergenic foods and/or follow a modified elimination diet by avoiding dairy and gluten containing foods, and emphasizing fresh nonprocessed foods.
Replace: Provide pancreatic multidigestive enzymes and HCL if appropriate, particularly if markers of malabsorption are present on the CDSA.
Reinoculate: Administer lactobacillus acidophilus, bifidobacteria and probiotics such as fructooligosaccharides (FOS) and inulin.
Repair: Provide nutrients to support gastrointestinal mucosal integrity, such as L-glutamine, antioxidants, glutathione, N-acetylcystein (NAC), zinc, pantothenic acid, medium chain triglycerides (MCTs), fiber, etc.
After intestinal issues have been effectively corrected, upregulation of liver detoxification pathways can be accomplished by providing nutrients which are used in phase I biotransformation and phase II conjugation pathways. These may include individual nutrients such as N-acetyl cysteine, methionine, cysteine, glycine, glutamic acid, glutathione and antioxidant nutrients (see Figure 3). However, the use of a specifically designed formulary medicinal food products are much more practical and efficient to use clinically.
Patients with elevated phase I cytochrome P450 enzyme activity and slow phase II conjugation activity should be treated with antioxidant therapy before detoxification begins. This slows the production of highly toxic biotransformed intermediate molecules which increase oxidative stress on the body.
This should all be combined with a diet which emphasizes fresh foods, and eliminates processed and allergenic foods. This will reduce the patients dietary toxic load (exotoxins), while the intestinal program will reduce gastrointestinal derived toxins (endotoxins). Following a modified elimination diet which eliminates the ingestion of gluten and dairy containing foods, and discontinuing as many drugs as possible, will also help during the detoxification process.
Many people who seek medical care do not have a clinically identifiable disease or pathology. Their problems are based in what I call �derangements or blockages in normal physiology� and present as dysfunctions in one or more organ systems that left unchecked would ultimately lead to disease and pathology. Typically these patients come to us having usually been told that everything looks normal based on the standard tests routinely run by their doctor (physical examination, urinalysis, blood tests etc.). These patients fall through the cracks of the current medical paradigm because they are neither sick from a pathological perspective (no tissue changes, no findings on diagnostic testing etc.) nor 100% well. These patients fall into a gray area of medicine and we need a different approach to be able to deal with this.
Some areas of physiology that are considered by a Functional Medicine practitioner are:
- Nutritional deficiencies or imbalances
- Inflammatory imbalances
- Digestive/intestinal imbalances
- Impaired detoxification
- Structural and/or neurological imbalances
- Oxidative stress
- Immune system dysfunction
- Hormonal and endocrine imbalances
Functional medicine practitioners know that most of our patients are by no means �normal�, but are a long way from being in a state of optimal health. Functional medicine is the way to deal with this because functional medicine is about being the ultimate medical detective.
While a more comprehensive and complete discussion of this functional approach is beyond the scope of this article, referring to the cited literature can help further clarify these procedures for the practicing clinician and provide more information on the commercially available formulary products specifically designed for use in this program (1-11).
References
- Bland J, Bralley A: Nutritional upregulation of hepatic detoxification enzymes, J Appl Nutr 44, 1992.
- Rigden S: Research study-CFIDS study preliminary report: Advances in the Diagnosis and Treatment of the Chronically Ill, 1991, Seattle.
- Rigden S: Enterohepatic resuscitation program for CFIDS, CFIDS Chron Spring, 1995.
- Cheney PR, Lapp CW: Entero-hepatic resuscitation in patients with chronic fatigue syndrome: A pyramid of nutritional therapy, CFIDS Chron Fall, 1993.
- Lanfranchi RG, et al: Fibromyalgia, chronic pain and the leaky gut syndrome. Today’s Chiropr, March/April:32-9, 1994.
- Rowe AH: Allergic fatigue and toxemia, Ann Allergy 17:9-18, 1959.
- Pressman AH: Metabolic toxicity and neuromuscular pain, joint disorders, and fibromyalgia, J Am Chiropr Assoc Sept:77-78, 1993.
- Gantz NM, Holmes GP: Treatment of patients with chronic fatigue syndrome, Drugs 36(6):855-862, 1989.
- Great Smokies Diagnostic Laboratory: 63 Zillicoa St, Ashville, NC 28801, 1-704-253-0621, www.gsdl.com.
- HealthComm International, Inc., Functional Medicine Research Center, P.O. Box 1729, Gig Harbor, WA 98335, 1-800-843- 9660, www.healthcomm.com.
- Metagenics, Inc., 971 Calle Negocio, San Clemente, CA 92673, 1-800-692-9400.
Visit Our Clinic Today!
Professional Scope of Practice *
The information herein on "Functional Medicine" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Our information scope is limited to Chiropractic, musculoskeletal, physical medicines, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somatovisceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and/or functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez, DC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, RN*, CCST, IFMCP*, CIFM*, ATN*
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807, New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Florida
Florida License RN License # RN9617241 (Control No. 3558029)
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Dr. Alex Jimenez DC, MSACP, RN* CIFM*, IFMCP*, ATN*, CCST
My Digital Business Card

