
by Dr Alex Jimenez | Functional Medicine, Gluten Free Diet, Wellness
Gluten Free: During a visit to my orthopedist I made a confession: �I stopped eating gluten and�this might sound a little crazy, but�a lot of my joint pain disappeared.
She smiled broadly and said, �You�re not the first person to say that.�
See�How Gluten Can Cause Joint Pain
I stopped eating gluten because couple of friends suggested it might relieve some unexplained symptoms I was experiencing, like fatigue and mild joint pain. I had strong doubts, but my primary care doctor and I had run out of ideas (I was waiting to see a specialist), so I figured I had nothing to lose.
See�Rheumatoid Arthritis and Fatigue
Within a week of going on a gluten-free diet, my fatigue, joint pain, and many other symptoms disappeared.
The Connection Between Gluten & Joint Pain
It turns out, researchers have long known that people with autoimmune forms of arthritis, such as�rheumatoid�
arthritis�and�psoriatic arthritis, are at higher risk for celiac disease,1, 2�an autoimmune disorder triggered by gluten.
See�Inflammatory Arthritis
More recently, medical experts have begun to acknowledge the connection between gluten and joint pain described as non-pathologic (unrelated to disease).
Both my orthopedist and primary care provider agree that my gluten-free diet is probably keeping my joint pain and other
symptoms of inflammation in check.
See�An Anti-Inflammatory Diet for Arthritis
Wait, Don�t Go Gluten Free Yet�
Before you throw away your pasta and cereal in search of joint pain relief, consider these factors:
See�Arthritis Treatment Specialists
- You might experience gluten withdrawal.Many people report that their inflammatory symptoms initially got worse after starting their gluten free diet. This withdrawal stage can last days or even weeks, so you may not want to go gluten free right before a big event, like a vacation, holiday, or the start of a newjob.
No single treatment or lifestyle habit can eliminate the symptoms of arthritis, but going gluten-free may be an option worth trying as part of your overall treatment plan.
By�Jennifer Flynn
Learn More
Turmeric and Curcumin for Arthritis
Dietary Supplements for Treating Arthritis
References

by Dr Alex Jimenez | Gluten Free Diet, Natural Health, Wellness
More and more people are following a gluten-free diet, but if they have no medical reason to do so they could actually be risking their health, a top expert says.
“The evidence is mounting against any health benefits from a gluten-free diet for those people without a medical reason,” John Douillard tells Newsmax Health.
Gluten is a naturally occurring protein present in cereal grains, especially wheat, which is responsible for the elastic texture of dough.
Traditionally, gluten was considered harmless unless eaten by people with celiac disease, whose digestive systems are unable to handle it.
But recently the idea of eating gluten-free has caught on, and the number of people following such a diet tripled in the five years between 2009 and 2014, while the number of those with celiac disease remained stable, research shows.
On the other hand, a pair of large studies, published in the past few months, has found those people who eat little gluten could be at risk of developing coronary heart disease, as well as diabetes.
Douillard is a chiropractor, certified addiction professional, and the author of “Eat Wheat,” along with six previous health books.
An expert in the field of natural heath, he is also former player development director and nutrition counselor for the New Jersey Nets NBA team. He has also appeared on the Dr. Oz Show, and featured in many national publications.
Here are excerpts from his recent interview with Newsmax Health.
Q: How did you get interested in gluten?
A: People would come to me with digestive problems and I’d tell them to get off wheat and they’d feel better for a short time, but after awhile, their problems would return. The same thing happened with dairy, or nuts. The problem wasn’t actual these specific foods. But, as the medical profession started making medical recommendations to get off of wheat, people began treating it like a poison.
Q: Who should not eat gluten?
A: People with celiac disease shouldn’t eat wheat, but that’s only about 1 percent to 3 percent of the population. There also may be those that don’t have celiac disease, but say they are sensitive to it, so they may be right to avoid it. But that’s an estimated 2 percent to 13 percent of the population. This leaves a third of the population that eliminated gluten from their diet under the misperception it is unhealthy. They are the ones missing out on the benefits of wheat.
Q: How did the idea that gluten is bad catch on?
A: Originally, people with celiac disease were told to avoid gluten but the idea caught on that it was good for other people as well, and now gluten-free has become a buzzword and it’s grown into a $16 billion industry. They’re even put “gluten free” on foods that never had any gluten in them, like yogurt.
Q: What’s the problem with gluten?
A: People who promulgate a gluten-free diet contend we aren’t genetically capable of eating gluten but that’s wrong. The University of Utah did a study that found evidence of wheat and barley in the teeth of ancient humans 3 ½ million years ago. The Paleo diet says to avoid grains, but if you talk to anthropologists, you’ll find out there’s nothing Paleo about this. Ancient humans gathered wheat berries to fuel them for the whole day. Most experts agree we didn’t start cooking out own meat until 500,000 years ago, so we had wheat in our teeth millions of years before that.
Q: What are the gluten-free people missing out on?
A: In addition to new studies that show wheat may lower diabetes and heart disease risk, wheat is a natural probiotic, and people who don’t eat it have less good microbes in their microbiome and more bad ones. They also are more likely to have weaker immune systems, because research finds eating the indigestible part of wheat helps to strengthen to strengthen it. In addition, people who follow the MIND Diet and the Mediterranean diet, both which permit whole grains, reduce their risk of Alzheimer’s disease.
Q: If it’s not gluten, what is the problem with the way we eat?
A: The problem is our reliance on processed foods. One study showed that our reliance on processed food increases metabolic syndrome (the condition that hikes heart disease and diabetes risk) by 141 percent. On the other hand, eating whole gains and whole wheat reduced it by 38 percent. So it’s processed foods we need to eliminate from our diet.
Here are Douillard’s 5 tips to digest gluten more easily:
1. Choose bread with only these ingredients: Organic whole wheat, water, salt, and an organic starter.
2. Sprouted soaked breads typically found in the refrigerator section are much easier to digest.
3. Avoid any bread or any packaged foods with cooked or heated vegetable oils. These are preservatives and indigestible.
4. Think seasonal eating. Eat more grains in the fall when they are harvested and less in the spring and summer.
5. Start your day with a beet, apple, and celery drink to amp up your digestive strength and spice your food with spices such as: ginger, cumin, coriander, fennel, and cardamon.
by Dr Alex Jimenez | Gluten Free Diet
A new study found that gluten-free diets could increase cardiovascular risk in people without celiac disease. The study claims that gluten-free diets among people without celiac disease is not associated with risk of coronary heart disease, but such diets result in a low intake of whole grains, which are linked to cardiovascular benefits.
Researchers say that gluten-free diets among people without celiac disease should not be encouraged, as people could miss out on the benefits of whole grains.
Researchers say that gluten-free diets among people without celiac disease should not be encouraged. Image credit: iStock.com / Everyday Health
People with celiac disease, on the other hand, usually have to follow gluten-free diets because the protein found in wheat, barley, and rye can cause them to develop gastrointestinal issues.
Gluten-free diets should not be encouraged to people without celiac disease
The study was published in the BMJ on May 2, and researchers noted that cutting out gluten unless medically necessary can increase a person�s risk of cardiovascular problems. The researchers analyzed data from 64,714 women and 45,303 men who worked in the health industry, each of whom had no history of heart disease.
Subjects were asked to fill a detailed food questionnaire in 1986, and they were required to update it every four years until 2010. The scientists noted that they saw no significant association between gluten intake and heart disease risk.
�Long term dietary intake of gluten was not associated with risk of coronary heart disease. However, the avoidance of gluten may result in reduced consumption of beneficial whole grains, which may affect cardiovascular risk,� wrote the researchers on the study.
Gluten is a storage protein found in wheat, rye, and barley, and it is known to trigger inflammation and intestinal damage in people with celiac disease. According to the researchers, celiac disease is present in 0.7 percent of the U.S. population, and because it is associated with an increased risk of coronary heart disease, patients are recommended to shift to a gluten-free diet.
 Gluten is a storage protein found in wheat, rye, and barley, and it is known to trigger inflammation and intestinal damage in people with celiac disease. Image credit: Thankheavens.com.au
Gluten is a storage protein found in wheat, rye, and barley, and it is known to trigger inflammation and intestinal damage in people with celiac disease. Image credit: Thankheavens.com.au
The study claims that currently many people reduce gluten in their diet because they believe that it will lead to general health benefits. A national survey showed that in 2013 nearly 30 percent of adults in the U.S. reported that they were cutting off or reducing their gluten intake. However, the researchers noted that despite the rising trend in gluten restriction, no study has linked gluten with the risk of coronary heart disease in people without celiac disease.
�Although people with and without celiac disease may avoid gluten owing to a symptomatic response to this dietary protein, these findings do not support the promotion of a gluten restricted diet with a goal of reducing coronary heart disease risk,� warned the researchers.
Researchers concluded their study saying that it found no evidence of gluten diets and coronary disease among male and female health professionals analyzed for more than 25 years and that further research is needed to investigate the link between gluten and cardiovascular problems, as their study was merely observational.
Source: The BMJ




 There are 3 known types of negative reactions to wheat proteins, collectively known as wheat protein reactivity: wheat allergy (WA), gluten sensitivity (GS),�and celiac disease (CD). Of the 3, only CD is known to involve autoimmune reactivity, generation of antibodies, and intestinal mucosal damage. Wheat allergy involves the release of histamine by way of immunoglobulin (Ig) E cross-linking with gluten peptides and presents within hours after ingestion of wheat proteins. Gluten sensitivity is considered to be a diagnosis of exclusion; sufferers improve symptomatically with a gluten-free diet (GFD) but do not express antibodies or IgE reactivity.1
There are 3 known types of negative reactions to wheat proteins, collectively known as wheat protein reactivity: wheat allergy (WA), gluten sensitivity (GS),�and celiac disease (CD). Of the 3, only CD is known to involve autoimmune reactivity, generation of antibodies, and intestinal mucosal damage. Wheat allergy involves the release of histamine by way of immunoglobulin (Ig) E cross-linking with gluten peptides and presents within hours after ingestion of wheat proteins. Gluten sensitivity is considered to be a diagnosis of exclusion; sufferers improve symptomatically with a gluten-free diet (GFD) but do not express antibodies or IgE reactivity.1 A 28-year-old man presented to a chiropractic teaching clinic with complaints of constant muscle fasciculations of 2 years� duration. The muscle fasciculations originally started in the left eye and remained there for about 6 months. The patient then noticed that the fasciculations began to move to other areas of his body. They first moved into the right eye, followed by the lips,�and then to the calves, quadriceps, and gluteus muscles. The twitching would sometimes occur in a single muscle or may involve all of the above muscles simultaneously. Along with the twitches, he reports a constant �buzzing� or �crawling� feeling in his legs. There was no point during the day or night when the twitches ceased.
A 28-year-old man presented to a chiropractic teaching clinic with complaints of constant muscle fasciculations of 2 years� duration. The muscle fasciculations originally started in the left eye and remained there for about 6 months. The patient then noticed that the fasciculations began to move to other areas of his body. They first moved into the right eye, followed by the lips,�and then to the calves, quadriceps, and gluteus muscles. The twitching would sometimes occur in a single muscle or may involve all of the above muscles simultaneously. Along with the twitches, he reports a constant �buzzing� or �crawling� feeling in his legs. There was no point during the day or night when the twitches ceased.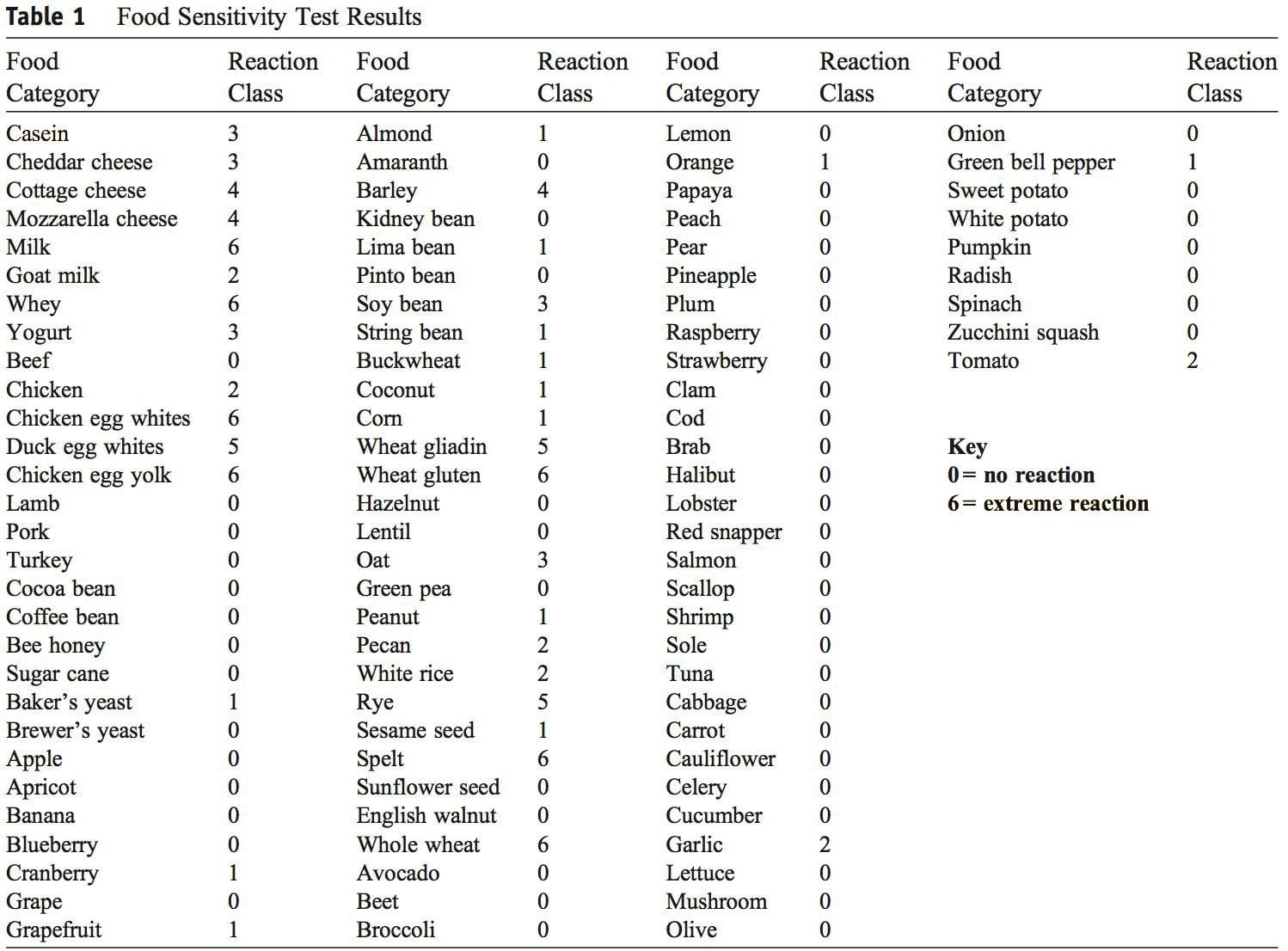 Discussion
Discussion The authors could not find any published case studies related to a presentation such as the one�described here. We believe this is a unique presentation of wheat protein reactivity and thereby represents a contribution to the body of knowledge in this field.
The authors could not find any published case studies related to a presentation such as the one�described here. We believe this is a unique presentation of wheat protein reactivity and thereby represents a contribution to the body of knowledge in this field. This report describes improvement in chronic, widespread muscle fasciculations and various other systemic symptoms with dietary change. There is strong suspicion that this case represents one of
This report describes improvement in chronic, widespread muscle fasciculations and various other systemic symptoms with dietary change. There is strong suspicion that this case represents one of
 Gluten is a storage protein found in wheat, rye, and barley, and it is known to trigger inflammation and intestinal damage in people with celiac disease. Image credit: Thankheavens.com.au
Gluten is a storage protein found in wheat, rye, and barley, and it is known to trigger inflammation and intestinal damage in people with celiac disease. Image credit: Thankheavens.com.au



