Work Injury Health Guidelines for Low Back Pain in El Paso, TX
Low back pain represents one of the most common complaints in healthcare settings. While various injuries and conditions associated with the musculoskeletal and nervous system can cause low back pain, many healthcare professionals believe that work injury may have a prevalent connection to low back pain. For instance, improper posture and repetitive movements may often cause work-related injuries. In other cases, environmental accidents at work may cause work injuries. In any case, diagnosing the source of a patient’s low back pain to correctly determine which would be the best treatment method to restore the individual’s original health and wellness is generally challenging.
First and foremost, getting the right doctors for your specific source of low back pain is essential for finding relief from your symptoms. Many healthcare professionals are qualified and experienced in treating work-related low back pain, including doctors of chiropractic or chiropractors. As a result, several work injury treatment guidelines have been established to manage low back pain in healthcare settings. Chiropractic care focuses on diagnosing, treating, and preventing various injuries and conditions, such as LBP, associated with the musculoskeletal and nervous system. By carefully correcting the misalignment of the spine, chiropractic care can help improve symptoms of low back pain, among other symptoms. The purpose of the following article is to discuss occupational health guidelines for the management of low back pain.
Occupational Health Guidelines for the Management of Low Back Pain: an International Comparison
Abstract
- Background: The enormous socioeconomic burden of low back pain emphasizes the need to manage this problem, especially in an occupational context effectively. To address this, occupational guidelines have been issued in various countries.
- Aims: To compare available international guidelines for managing low back pain in an occupational health care setting.
- Methods: The guidelines were compared regarding generally accepted quality criteria using the AGREE instrument and also summarised regarding the guideline committee, the presentation, the target group, and assessment and management recommendations (that is, advice, return to work strategy, and treatment).
- Results and Conclusions: The results show that the guidelines variously met the quality criteria. Common flaws concerned the absence of proper external reviewing in the development process, lack of attention to organizational barriers and cost implications, and lack of information on the extent to which editors and developers were independent. There was general agreement on numerous issues fundamental to occupational health management of back pain. The assessment recommendations included diagnostic triage, screening for red flags and neurological problems, and identifying potential psychosocial and workplace barriers to recovery. The guidelines also agreed on advice that low back pain is a self-limiting condition and that remaining at work or an early (gradual) return to work, if necessary with modified duties, should be encouraged and supported.
Dr. Alex Jimenez’s Insight
Low back pain is one of the most prevalent health issues treated in chiropractic offices. Although the following article describes low back pain as a self limiting condition, the cause of an individual’s LBP can also trigger debilitating and severe pain and discomfort of left untreated. It’s important for an individual with symptoms of low back pain to seek proper treatment with a chiropractor to properly diagnose and treat their health issues as well as prevent them from returning in the future. Patients who experience low back pain for more than 3 months are less than 3 percent likely to return to work. Chiropractic care is a safe and effective alternative treatment option which can help restore the original function of the spine. Furthermore, a doctor of chiropractic, or chiropractor, can provide lifestyle modifications, such as nutritional and fitness advice, to speed up the patient’s recovery process. Healing through movement is essential for LBP recovery.
Low back pain (LBP) is one of the industrial countries’ most common health problems. Despite its benign nature and sound course, LBP is commonly associated with incapacity, productivity loss due to sick leave, and high societal costs.[1]
Because of that impact, there is an obvious need for effective management strategies based on scientific evidence derived from studies of sound methodological quality. Usually, these are randomized controlled trials (RCTs) on the effectiveness of therapeutic interventions, diagnostic studies, or prospective observational studies on risk factors or side effects. The scientific evidence, summarised in systematic reviews and meta-analyses, provides a solid basis for guidelines on managing LBP. In a previous paper, Koes et al. compared various existing clinical guidelines for managing LBP targeted at primary healthcare professionals, showing a considerable commonality.[2]
The problems in occupational health care are different. Management focuses mainly on counseling the worker with LBP and addressing the issues of assisting them to continue working or return to work (RTW) after sick listing. However, LBP is also an important issue in occupational health care because of the associated incapacity for work, productivity loss, and sick leave. Several guidelines, or sections of guidelines, have now been published dealing with the specific issues of management in an occupational health care setting. Since the evidence is international, it would be expected that the recommendations of different occupational guidelines for LBP would be more or less similar. However, it is not clear whether the guidelines meet currently accepted quality criteria.
This paper critically appraises available occupational guidelines on managing LBP and compares their assessment and management recommendations.
Main Messages
- In various countries, occupational health guidelines are issued to improve the management of low back pain in an occupational context.
- Common flaws of these guidelines concern the absence of proper external reviewing in the development process, lack of attention to organizational barriers and cost implications, and lack of information on the independence of editors and developers.
- In general, the assessment recommendations in the guidelines consisted of diagnostic triage, screening for red flags and neurological problems, and identifying potential psychosocial and workplace barriers to recovery.
- There is general agreement on advice that low back pain is a self-limiting condition and that remaining at work or an early (gradual) return to work, if necessary with modified duties, should be encouraged and supported.
Methods
Guidelines on the occupational health management of LBP were retrieved from the authors’ personal files. Retrieval was checked by a Medline search using the keywords low back pain, guidelines, and occupational up to October 2001, and personal communication with experts in the field. Policies had to meet the following inclusion criteria:
- Guidelines aimed at managing workers with LBP (in occupational health care settings or addressing occupational issues) or separate sections of policies that dealt with these topics.
- Guidelines are available in English or Dutch (or translated into these languages).
The exclusion criteria were:
- Guidelines on primary prevention (that is, prevention before the onset of the symptoms) of work-related LBP (for example, lifting instructions for workers).
- Clinical guidelines for the management of LBP in primary care.[2]
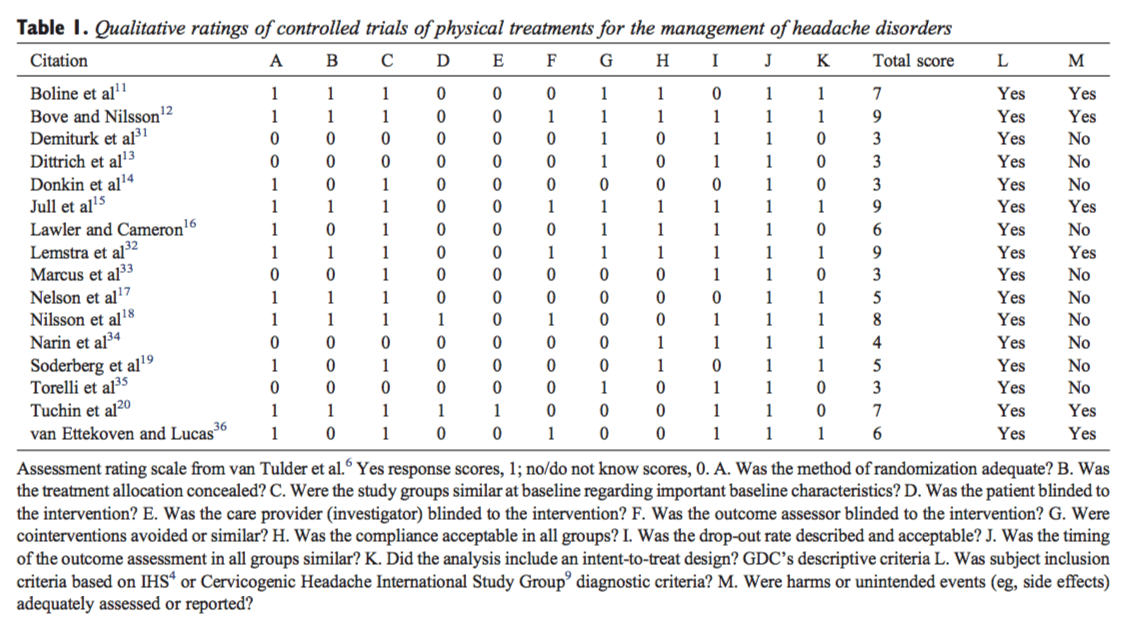
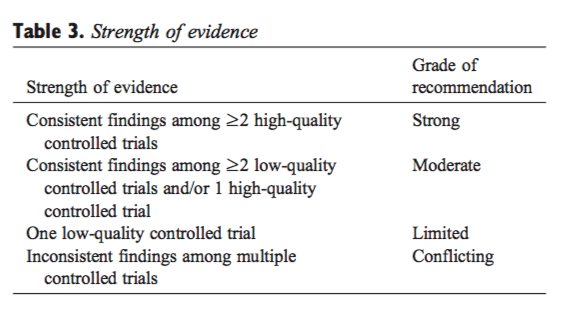
The quality of the included guidelines was appraised using the AGREE instrument, a generic tool designed primarily to help guideline developers and users assess the methodological quality of clinical practice guidelines.[3]
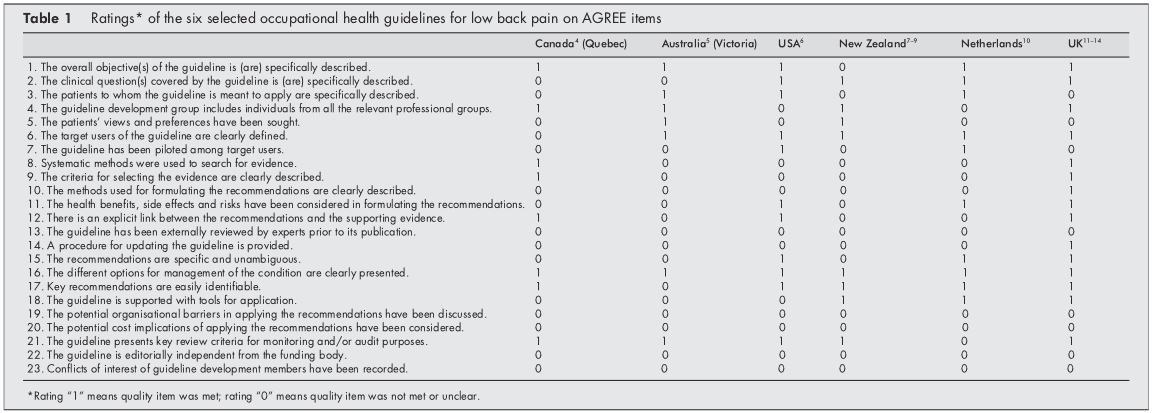
The AGREE instrument provides a framework for assessing the quality on 24 items (table 1), each rated on a four-point scale. The full operationalization is available on www.agreecollaboration.org.
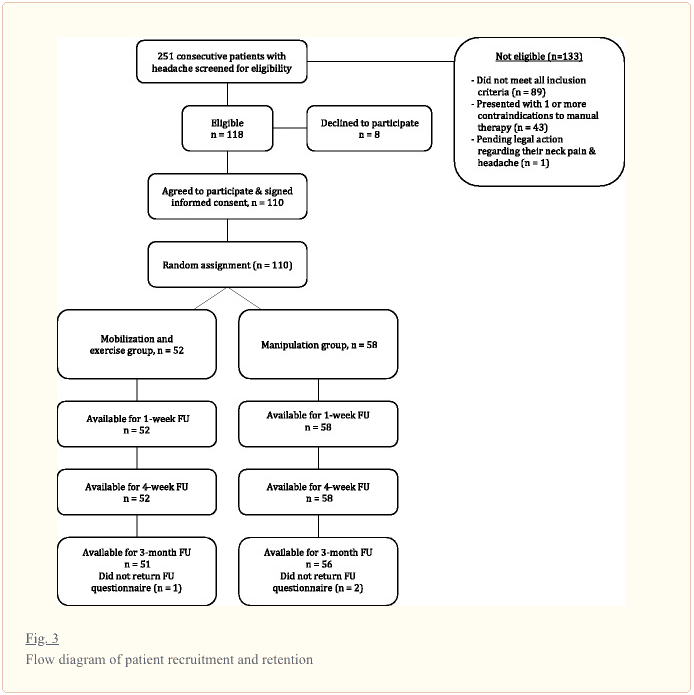
Two reviewers (BS and HH) independently rated the quality of the guidelines and then met to discuss disagreements and to reach a consensus on the ratings. When they could not agree, a third reviewer (MvT) reconciled the remaining differences and decided on the ratings. To facilitate analysis in this review, ratings were transformed into dichotomous variables of whether each quality item was or was not met.
The assessment recommendations were summarised and compared to recommendations on advice, treatment, and return to work strategies. The selected guidelines were further characterized and reached regarding the guideline committee, the presentation of the procedure, the target group, and the extent to which the recommendations were based on available scientific evidence. All of this information was extracted directly from the published guidelines.
Policy Implications
- The management of low back pain in occupational health care should follow evidence-based guidelines.
- Future occupational guidelines for managing low back pain and updates of those guidelines should consider the criteria for proper development, implementation, and evaluation of approaches as suggested by the AGREE collaboration.
Results
Selection of Studies
Our search found ten guidelines, but four were excluded because they dealt with the management of LBP in primary care,[15] were aimed at the guidance of sick-listed employees in general (not specifically LBP),[16] were intended for the primary prevention of LBP at work,[17] or were not available in English or Dutch.[18] The final selection, therefore, consisted of the following six guidelines, listed by date of issue:
(1) Canada (Quebec). A scientific approach to the assessment and management of activity-related spinal disorders. A monograph for clinicians. Report of the Quebec Task Force on Spinal Disorders. Quebec Canada (1987).[4]
(2) Australia (Victoria). Guidelines for the management of employees with compensable low back pain. Victorian WorkCover Authority, Australia (1996).[5] (This is a revised version of guidelines developed by the South Australian WorkCover Corporation in October 1993.)
(3) the USA. Occupational Medicine Practice Guidelines. American College of Occupational and Environmental Medicine. USA (1997).[6]
(4) New Zealand
(a)Active and working! Managing acute low back pain in the workplace. Accident Compensation Corporation and National Health Committee. New Zealand (2000).[7]
(b)Patient guide to acute low back pain management. Accident Compensation Corporation and National Health Committee. New Zealand (1998).[8]
(c) Assess psychosocial yellow flags in acute low back pain. Accident Compensation Corporation and National Health Committee. New Zealand (1997).[9]
(5) the Netherlands. Dutch guideline for managing occupational physicians of employees with low back pain. Dutch Association of Occupational Medicine (NVAB). Netherlands (1999).[10]
(6) the UK
(a)Occupational health guidelines for managing low back pain at work principal recommendations. Faculty of Occupational Medicine. UK (2000).[11]
(b)Occupational health guidelines for managing low back pain at work leaflet for practitioners. Faculty of Occupational Medicine. UK (2000).[12]
(c)Occupational health guidelines for managing low back pain at work evidence review. Faculty of Occupational Medicine. UK (2000).[13]
(d)The Back Book, The Stationery Office. UK (1996).[14]
Two guidelines (4 and 6) could not be evaluated independently from additional documents to which they refer (4bc, 6bd), so these documents were also included in the review.
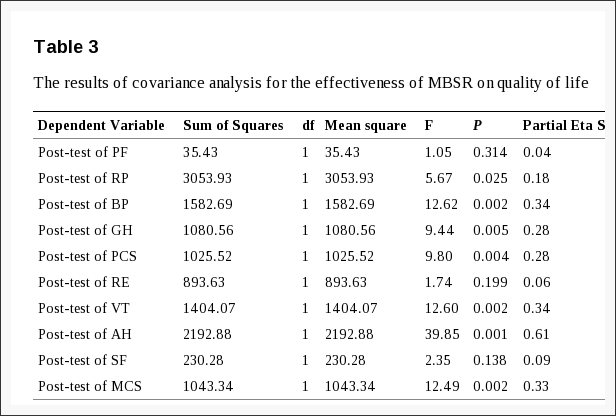
Appraisal of the Quality of the Guidelines
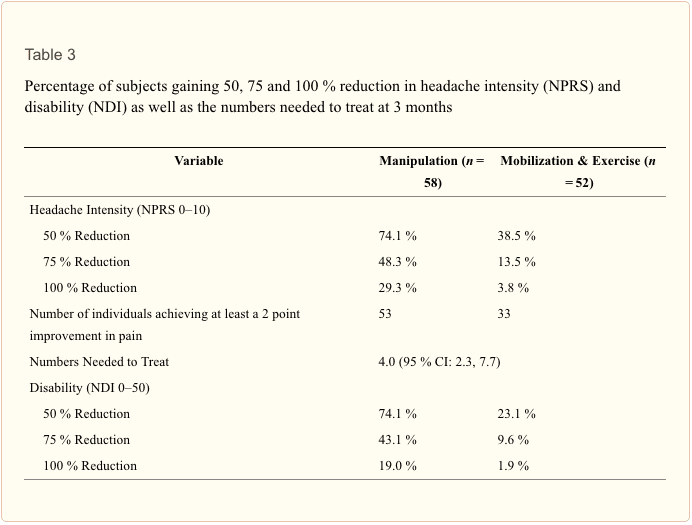
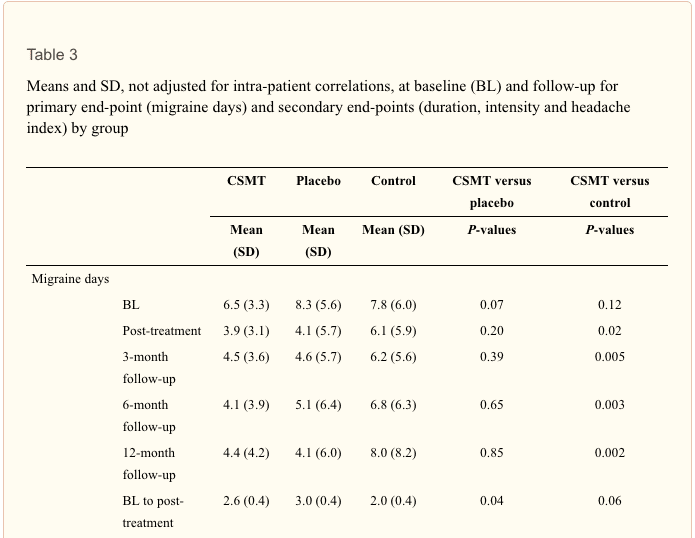
Initially, there was an agreement between the two reviewers regarding 106 (77%) of the 138 item ratings. After two meetings, the consensus was reached for all but four items, which required adjudication by the third reviewer. Table 1 presents the final ratings.
All included guidelines presented the different options for managing LBP in occupational health. In five of the six policies, the overall objectives of the procedure were explicitly described,[46, 1014] the target users of the system were clearly defined,[514] easily identifiable key recommendations were included,[4, 614] or critical review criteria were presented for monitoring and audit purposes.[49, 1114]
The results of the AGREE appraisal showed that none of the guidelines paid sufficient attention to potential organizational barriers and cost implications in implementing the recommendations. It was also unclear for all included guidelines whether or not they were editorially independent of the funding body and whether or not there were conflicts of interest for the members of the guideline development committees. Furthermore, it was unclear for all guidelines whether experts had externally reviewed the policies before publication. Only the UK guideline clearly described the method used to formulate the recommendations and provided for updating the approach.[11]
Development of the Guidelines
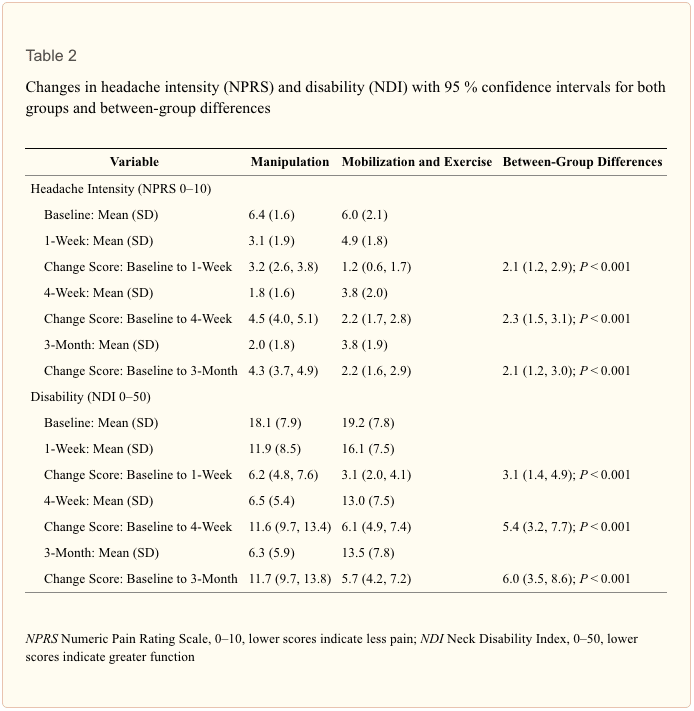
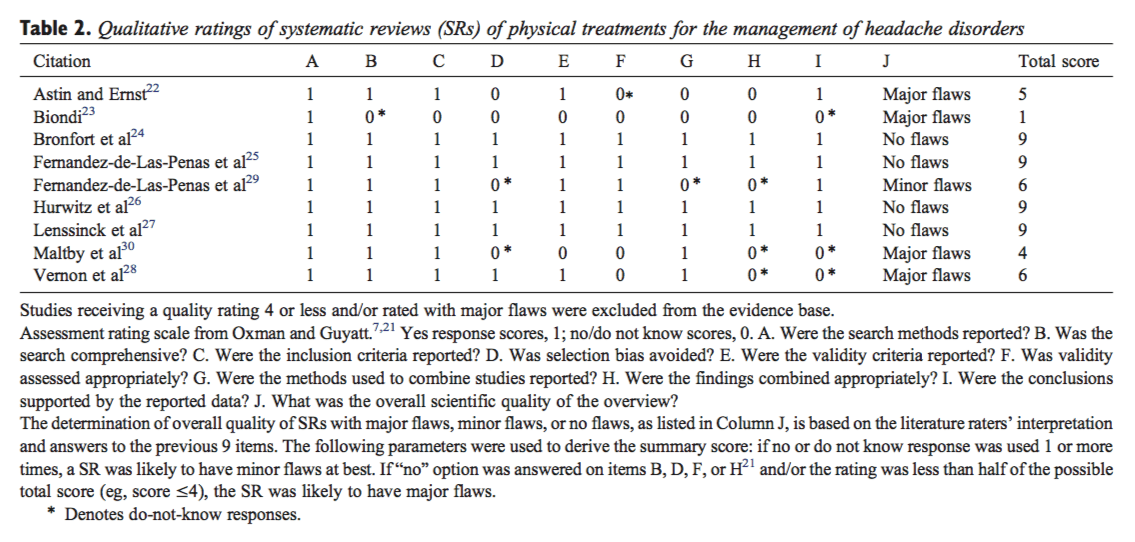
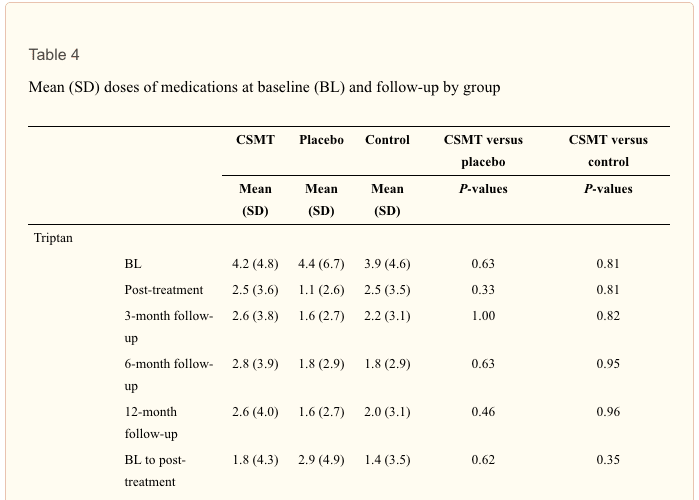
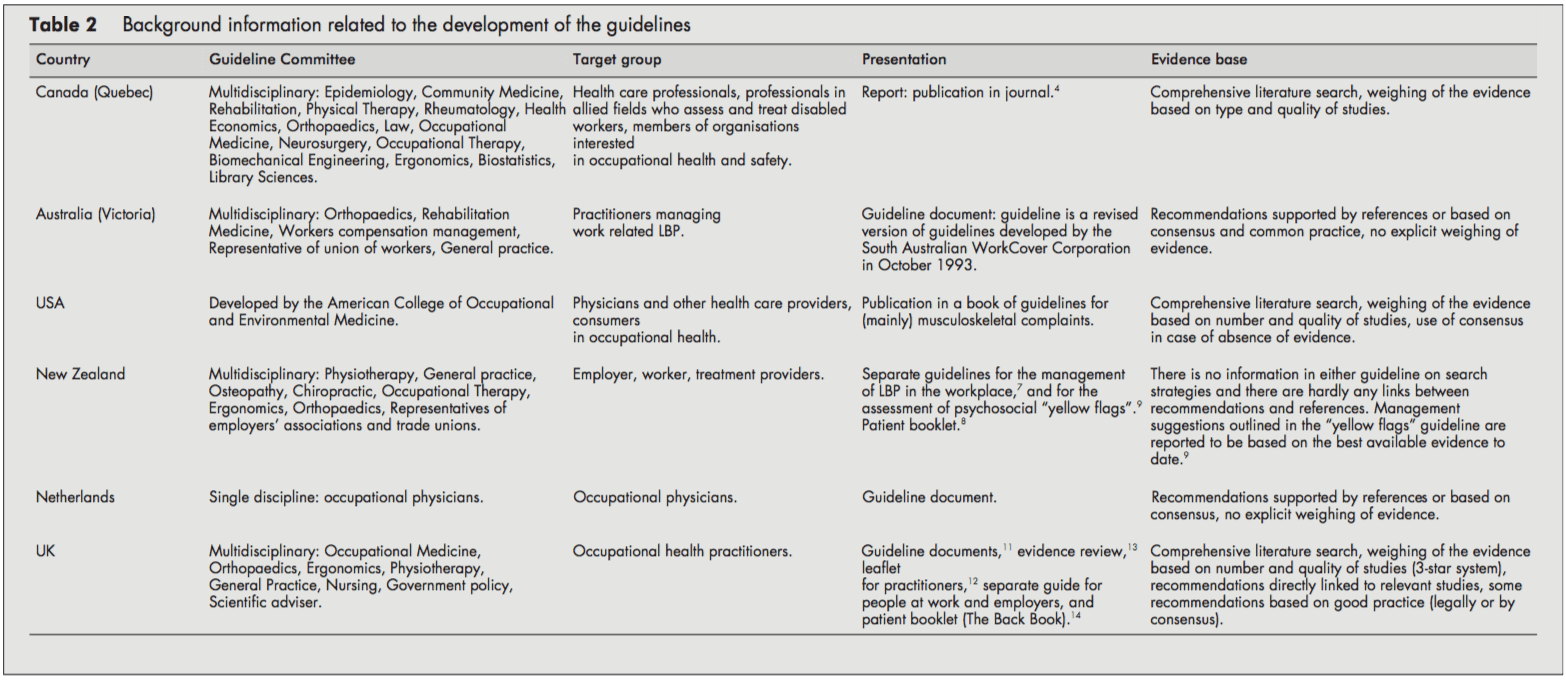
Table 2 presents background information on the development process of the guidelines.
The target users for the guidelines were physicians and other healthcare providers in the field of occupational healthcare. Several policies were also directed at informing employers, workers [68, 11, 14], or members of organizations interested in occupational health.[4] The Dutch guideline was only targeted at the occupational health physician.[10]
The guideline committees responsible for developing the guidelines were generally multidisciplinary, including disciplines like epidemiology, ergonomics, physiotherapy, general practice, occupational medicine, occupational therapy, orthopedics, and representatives of employers’ associations and trade unions. Chiropractic and osteopathic representatives were in the guideline committee of the New Zealand guidelines.[79] The Quebec task force (Canada) also included representatives of rehabilitation medicine, rheumatology, health economics, law, neurosurgery, biomechanical engineering, and library sciences. In contrast, the guideline committee of the Dutch guideline consisted only of occupational physicians.[10]
The guidelines were issued as a separate document,[4, 5, 10] as a chapter in a textbook,[6] or as several interrelated documents.[79, 1114]
The UK,[13] the USA,[6] and Canadian[4] guidelines provided information on the search strategy applied to the identification of relevant literature and the weighing of the evidence. On the other hand, the Dutch[10] and the Australian[5] guidelines supported their recommendations only by references. The New Zealand guidelines showed no direct links between suggestions and concerns [79]. The reader was referred to other literature for background information.
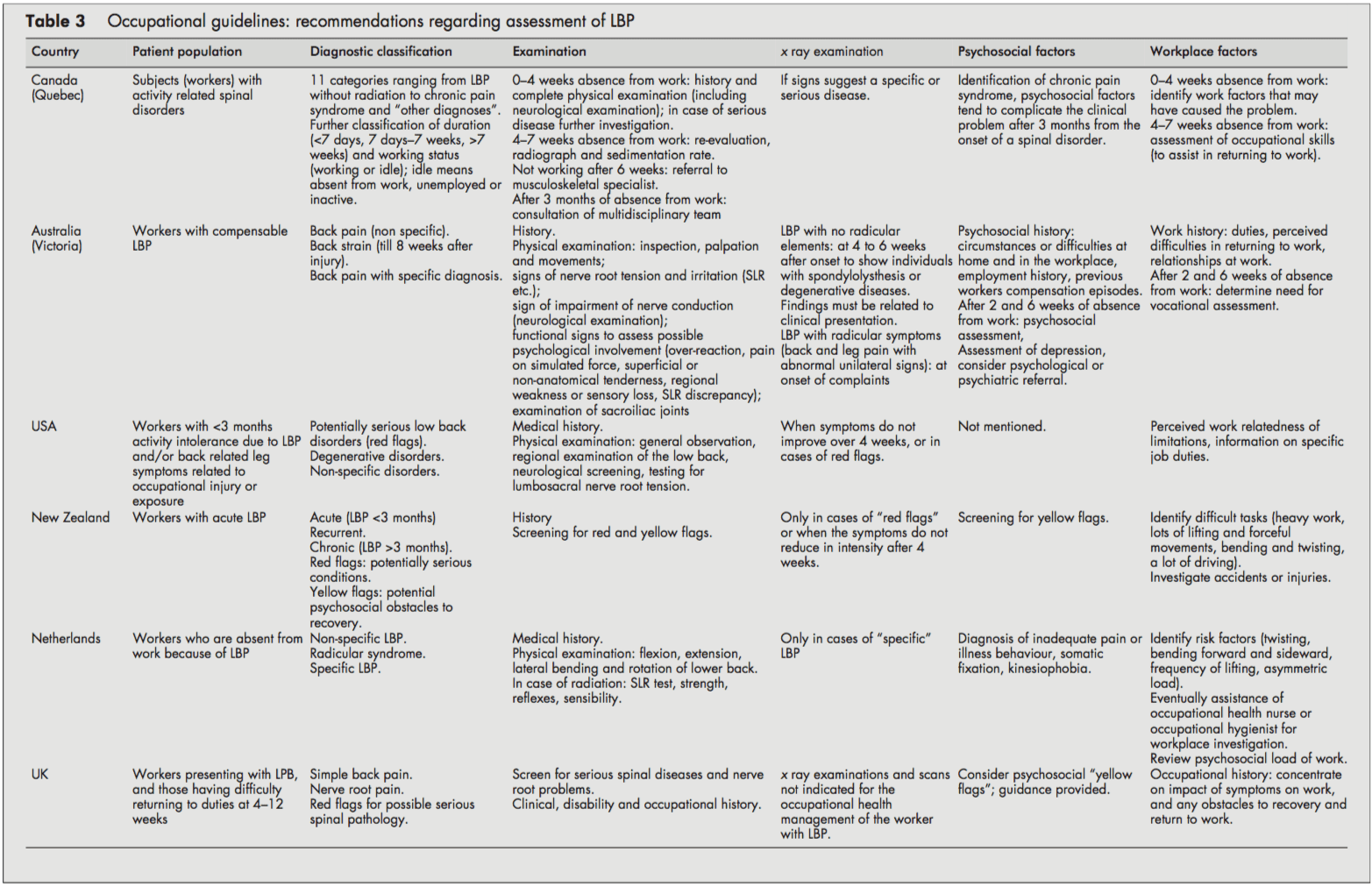
Patient Population and Diagnostic Recommendations
Although all guidelines focused on workers with LBP, it was often unclear whether they dealt with acute or chronic LBP or both. Acute and chronic LBP were often not defined, and cut-off points were given (for example, <3 months). It was usually unclear whether these referred to the onset of symptoms or absence from work. However, the Canadian guideline introduced a classification system (acute/subacute/ chronic) based on the distribution of claims of spinal disorders by time since absence from work.[4]
All guidelines distinguished specific and non-specific LBP. Specific LBP concerns the potentially serious red flag conditions like fractures, tumors, or infections, and the Dutch and UK guidelines also distinguish the radicular syndrome or nerve root pain.[1013] All procedures were consistent in their recommendations to take a clinical history and to carry out a physical examination, including neurological screening. In cases of suspected specific pathology (red flags), x-ray examinations were recommended by most guidelines. In addition, New Zealand and the US guideline also recommended an x-ray examination when symptoms did not improve after four weeks.[6, 9] The UK guideline stated that x-ray examinations are not indicated and do not assist occupational health management of the patient with LBP (distinct from any clinical indications).[1113]
Most guidelines considered psychosocial factors as yellow flags as obstacles to recovery that healthcare providers should address. The New Zealand[9] and UK guidelines [11, 12] explicitly listed factors and suggested questions to identify those psychosocial yellow flags.
All guidelines addressed the importance of the clinical history identifying physical and psychosocial workplace factors relevant to LBP, including physical demands of work (manual handling, lifting, bending, twisting, and exposure to whole-body vibration), accidents or injuries, and perceived difficulties in returning to work or relationships at work. The Dutch and the Canadian guidelines contained recommendations to carry out a workplace investigation[10] or an assessment of occupational skills when necessary.[4]
Summary of Recommendations for the Assessment of LBP
- Diagnostic triage (non-specific LBP, radicular syndrome, specific LBP).
- Exclude red flags and neurological screening.
- Identify psychosocial factors and potential obstacles to recovery.
- Identify workplace factors (physical and psychosocial) that may be related to the LBP problem and return to work.
- X-Ray examinations are restricted to suspected cases of specific pathology.
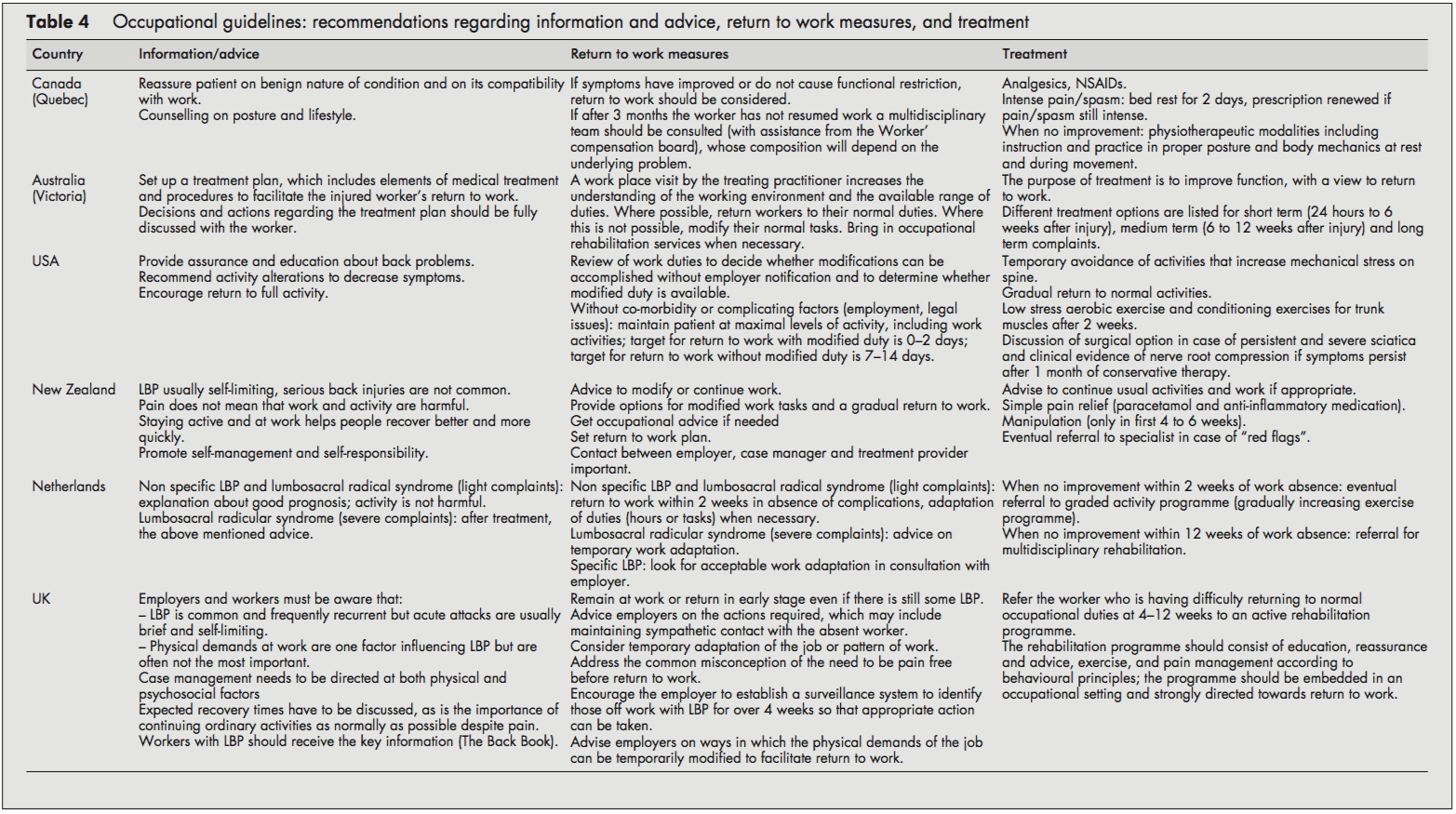
Recommendations Regarding Information and Advice, Treatment, and Return to Work Strategies
Most guidelines recommended reassuring the employee and providing information about LBP’s self-limiting nature and good prognosis. Encouragement of return to ordinary activity as generally as possible was frequently advised.
In line with the recommendation to return to regular activity, all guidelines also stressed the importance of returning to work as rapidly as possible, even if there is still some LBP and, if necessary, starting with modified duties in more severe cases. Work duties could then be increased gradually (hours and tasks) until total return to work was reached. The US and Dutch guidelines provided detailed time schedules for return to work. The Dutch approach proposed a return to work within two weeks with an adaptation of duties when necessary.[10] The Dutch system also stressed the importance of time-contingent management about a return to work.[10] The US guideline proposed every attempt to maintain the patient at maximal levels of activity, including work activities; targets for disability duration in terms of return to work were given as 02 days with modified duties and 714 days if modified duties are not used/available.[6] In contrast to the others, the Canadian guideline advised return to work only when symptoms and functional restrictions had improved.[4]
The most frequently recommended treatment options in all the included guidelines were: medication for pain relief,[5, 7, 8] gradually progressive exercise programs,[6, 10] and multidisciplinary rehabilitation.[1013] The US guideline recommended referral within two weeks to an exercise program consisting of aerobic exercises, conditioning exercises for trunk muscles, and exercise quota.[6] The Dutch guideline recommended that if there is no progress within two weeks of work absence, workers should be referred to a graded activity program (gradually increasing exercises) and, if there is no improvement by four weeks, to a multidisciplinary rehabilitation program.[10] The UK guideline recommended that workers who have difficulty returning to regular occupational duties by 412 weeks should be referred to an active rehabilitation program. This rehabilitation program should include education, reassurance and advice, a progressive vigorous exercise and fitness program, and pain management according to behavioral principles; it should be embedded in an occupational setting and directed firmly toward a return to work.[11-13] Extensive lists of possible treatment options were presented in the guidelines of Canada and Australia [4, 5], although most of these were not based on scientific evidence.
Summary of Recommendations Regarding Information, Advice, Return to Work Measures, and Treatment in Workers with LBP
- Reassure the worker and provide adequate information about LBP’s self-limiting nature and good prognosis.
- Advise the worker to continue ordinary activities or to return to regular exercise and work as soon as possible, even if there is still some pain.
- Most workers with LBP return to more or less regular duties quite rapidly. Consider temporary adaptations of work duties (hours/tasks) only when necessary.
- When a worker fails to return to work within 212 weeks (there is considerable variation in the time scale in different guidelines), refer them to a gradually increasing exercise program, or multidisciplinary rehabilitation (exercises, education, reassurance, and pain management following behavioral principles). These rehabilitation programs
should be embedded in an occupational setting.
Discussion
The management of LBP in an occupational health setting must address the relation between low back complaints and work and develop strategies aimed at a safe return to work. This review compared available occupational health guidelines from various countries. Policies are rarely indexed in Medline, so when searching for guidelines, we had to rely primarily on personal files and personal communication.
Quality Aspects and Development Process of the Guidelines
The assessment by the AGREE instrument[3] showed some differences in the quality of the guidelines reviewed, which may partly reflect the variation in the dates of development and publication of the guidelines. The Canadian guideline, for example, was published in 1987 and the Australian guideline in 1996.[4, 5] The other guidelines were more recent and incorporated a more extensive evidence base and more up to date guideline methodology.
Several common flaws related to the development process of the guidelines were shown by the assessment by the AGREE instrument. Firstly, it is important to make clear whether a guideline is editorially independent from the funding body, and whether there are conflicts of interest for the members of the guideline committee. None of the included guidelines clearly reported these issues. Further, reported external review of the guideline by clinical and methodological experts prior to publication was also lacking in all guidelines included in this review.
Several guidelines provided comprehensive information on the way relevant literature was searched and translated into recommendations.[4, 6, 11, 13] Other guidelines supported their recommendations by references,[5, 7, 9, 10] but this does not permit assessment of the robustness of the guidelines or their recommendations.
Guidelines depend on the scientific evidence, which changes over time, and it is striking that only one guideline provided for future update.[11, 12] Possibly there are updates planned for the other guidelines but they are not explicitly stated (and conversely stating there will be future update does not mean it will actually occur). This lack of reporting may also hold true for other AGREE criteria that we rated negatively. The use of the AGREE framework as a guide for both the development and the reporting of guidelines should help to improve the quality of future guidelines.
Assessment and Management of LBP
The diagnostic procedures recommended in the occupational health guidelines were largely similar to the recommendations of clinical guidelines,[2] and, logically, the main difference was the emphasis on addressing occupational issues. The reported methods for addressing workplace factors in the assessment of LBP of the individual worker concerned the identification of difficult tasks, risk factors, and obstacles for return to work by occupational histories. Obviously, these obstacles for return to work not only concern physical load factors, but also work related psychosocial problems regarding responsibilities, cooperation with co-workers, and the social atmosphere at the workplace.[10] Screening for work related psychosocial yellow flags may help to identify those workers who are at risk for chronic pain and disability.[1113]
A potentially important feature of the guidelines is that they were consistent regarding their recommendations to reassure the employee with LBP, and to encourage and support return to work even with some persisting symptoms. There is general consensus that most workers do not have to wait until they are completely free of pain before returning to work. The lists of treatment options provided by the Canadian and Australian guidelines may reflect the lack of evidence at that time,[4, 5] leaving users of the guidelines to choose for themselves. It is, however, questionable whether such lists really contribute to improved care, and in our view guideline recommendations should be based on sound scientific evidence.
The US, Dutch, and UK occupational guidelines[6, 1013] recommend that active multidisciplinary treatment is the most promising intervention for return to work, and this is supported by strong evidence from RCTs.[19, 20] However, more research is still needed to identify the optimum content and intensity of those treatment packages.[13, 21]
Despite some evidence for a contribution of workplace factors in the aetiology of LBP,[22] systematic approaches for workplace adaptations are lacking, and are not offered as recommendations in the guidelines. Perhaps this represents a lack of confidence in the evidence on the overall impact of workplace factors, a difficulty of translation into practical guidance, or because these issues are confounded with local legislation (which was hinted at in the UK guideline[11]). It may be that the participatory ergonomics intervention, which proposes consultations with the worker, the employer, and an ergonomist, will turn out to be a useful return to work intervention.[23, 24] The potential value of getting all the players onside[25] was stressed in the Dutch and the UK guidelines,[1113] but further evaluation of this approach and its implementation is required.
Development of Future Guidelines in Occupational Health Care
The purpose of this review was to give both an overview and a critical appraisal of occupational guidelines for the management of LBP. The critical appraisal of the guidelines is meant to help direct future development and planned updates of guide- lines. In the still emerging field of guideline methodology we consider all past initiatives as laudable; we recognise the need for clinical guidance, and appreciate that guidelines developers cannot wait for research to provide all the methodology and evidence required. However, there is room for improvement and future guidelines and updates should consider the criteria for proper development, implementation, and evaluation of guidelines as suggested by the AGREE collaboration.
The implementation of the guidelines is beyond the scope of this review, but it was noted that none of the guideline documents specifically described implementation strategies, so it is uncertain to what extent the target groups may have been reached, and what effects that may have had. This may be a fruitful area for further research.
The very existence of these occupational health guidelines shows that existing primary care clinical guidelines for LBP2 are considered inappropriate or insufficient for occupational health care. There is a clear perception internationally that the needs of the worker experiencing back pain are intrinsically linked to a variety of occupational issues not covered by usual primary care guidance and, consequently, practice. What emerges is that, despite the methodological flaws, considerable agreement is evident on a range of fundamental occupational health strategies for managing the worker with back pain, some of which are innovative and challenge previously held views. There is agreement on the fundamental message that prolonged work loss is detrimental, and that early work return should be encouraged and facilitated; there is no need to wait for complete symptom resolution. Although the recommended strategies vary somewhat, there is considerable agreement on the value of positive reassurance and advice, availability of (temporary) modified work, addressing workplace factors (getting all the players onside), and rehabilitation for workers having difficulty returning to work.
Acknowledgements
This study was supported by the Dutch Health Care Insurance Council (CVZ), grant DPZ no. 169/0, Amstelveen, Netherlands. J B Staal is currently working at the Department of Epidemiology, Maastricht University, PO Box 616 6200 MD Maastricht, Netherlands. W van Mechelen is also part of the Research Centre on Physical Activity, Work and Health, Body@work TNO-VUmc.
In conclusion, symptoms of low back pain are one of the most common health issues associated with work injuries. Because of it, several occupational health guidelines have been established for the management of low back pain. Chiropractic care, among other treatment methods, may be utilized in order to help the patient find relief from their LBP. Furthermore, the article above demonstrated the safety and effectiveness of a variety of traditional as well as alternative treatment options in the diagnosis, treatment and prevention of a variety of low back pain cases. However, further research studies are required in order to properly determine the efficiency of each individual treatment method. Information referenced from the National Center for Biotechnology Information (NCBI). The scope of our information is limited to chiropractic as well as to spinal injuries and conditions. To discuss the subject matter, please feel free to ask Dr. Jimenez or contact us at 915-850-0900 .
Curated by Dr. Alex Jimenez
Additional Topics: Back Pain
According to statistics, approximately 80% of people will experience symptoms of back pain at least once throughout their lifetimes. Back pain is a common complaint which can result due to a variety of injuries and/or conditions. Often times, the natural degeneration of the spine with age can cause back pain. Herniated discs occur when the soft, gel-like center of an intervertebral disc pushes through a tear in its surrounding, outer ring of cartilage, compressing and irritating the nerve roots. Disc herniations most commonly occur along the lower back, or lumbar spine, but they may also occur along the cervical spine, or neck. The impingement of the nerves found in the low back due to injury and/or an aggravated condition can lead to symptoms of sciatica.

EXTRA IMPORTANT TOPIC: Migraine Pain Treatment
MORE TOPICS: EXTRA EXTRA: El Paso, Tx | Athletes
Blank
References
2. Koes BW, van Tulder MW, Ostelo R, et al. Clinical guidelines for the management of low back pain in primary care: an international
comparison. Spine 2001;26:2504�14.
3. The AGREE Collaboration. Appraisal of Guidelines Research &
Evaluation Instrument, www.agreecollaboration.org.
4. Spitzer WO, Leblanc FE, Dupuis M. Scientific approach to the
assessment and management of activity-related spinal disorders. A monograph for clinicians. Report of the Quebec Task Force on Spinal Disorders. Spine 1987;12(suppl 7S):1�59.
5. Victorian WorkCover Authority. Guidelines for the management of employees with compensable low back pain. Melbourne: Victorian WorkCover Authority, 1996.
6. Harris JS. Occupational medicine practice guidelines. Beverly, MA: OEM Press, 1997.
7. Accident Compensation Corporation and National Health Committee. Active and working! Managing acute low back pain in the workplace. Wellington, New Zealand, 2000.
8. Accident Compensation Corporation and National Health Committee, Ministry of Health. Patient guide to acute low back pain management. Wellington, New Zealand, 1998.
9. Kendall, Linton SJ, Main CJ. Guide to assessing psychosocial yellow flags in acute low back pain. Risk factors for long-term disability and work loss. Wellington, New Zealand, Accident Rehabilitation & Compensation Insurance Corporation of New Zealand and the National Health Committee, 1997.
10. Nederlandse Vereniging voor Arbeids- en Bedrijfsgeneeskunde (Dutch Association of Occupational Medicine, NVAB). Handelen van de bedrijfsarts bij werknemers met lage-rugklachten. Richtlijnen voor Bedrijfsartsen. [Dutch guideline for the management of occupational physicians of employees with low back pain]. April 1999.
11. Carter JT, Birell LN. Occupational health guidelines for the management of low back pain at work�principal recommendations. London: Faculty of Occupational Medicine, 2000 (www.facoccmed.ac.uk).
12. Occupational health guidelines for the management of low back pain at work�leaflet for practitioners. London: Faculty of Occupational Medicine, 2000 (www.facoccmed.ac.uk).
13. Waddell G, Burton AK. Occupational health guidelines for the management of low back pain at work�evidence review. Occup Med 2001;51:124�35.
14. Roland M, et al. The back book. Norwich: The Stationery Office, 1996.
15. ICSI. Health care guideline. Adult low back pain. Institute for Clinical Systems Integration, 1998 (www.icsi.org/guide/).
16. Kazimirski JC. CMA policy summary: The physician�s role in helping patients return to work after an illness or injury. CMAJ 1997;156:680A�680C.
17. Yamamoto S. Guidelines on worksite prevention of low back pain. Labour standards bureau notification, No. 57. Industrial Health 1997;35:143�72.
18. INSERM. Les Lombalgies en milieu professionel: quel facteurs de risque et quelle prevention? [Low back pain at the workplace: risk factors and prevention]. Paris: les editions INSERM, Synthese bibliographique realise a la demande de la CANAM, 2000.
19. Lindstro?m I, Ohlund C, Eek C, et al. The effect of graded activity on patients with subacute low back pain: a randomised prospective clinical study with an operant-conditioning behavioural approach. Physical Therapy 1992;72:279�93.
20. Karjalainen K, Malmivaara A, van Tulder M, et al. Multidisciplinary biopsychosocial rehabilitation for subacute low back pain in working-age adults: a systematic review within the framework of the Cochrane Collaboration Back Review Group. Spine 2001;26:262�9.
21. Staal JB, Hlobil H, van Tulder MW, et al. Return-to-work interventions for low back pain: a descriptive review of contents and concepts of working mechanisms. Sports Med 2002;32:251�67.
22. Hoogendoorn WE, van Poppel MN, Bongers PM, et al. Physical load during work and leisure time as risk factors for back pain. Scand J Work Environ Health 1999;25:387�403.
23. Loisel P, Gosselin L, Durand P, et al. A population-based, randomised clinical trial on back pain management. Spine 1997;22:2911�18.
24. Loisel P, Gosselin L, Durand P, et al. Implementation of a participatory ergonomics program in the rehabilitation of workers suffering from subacute back pain. Appl Ergon 2001;32:53�60.
25. Frank J, Sinclair S, Hogg-Johnson S, et al. Preventing disability from work-related low-back pain. New evidence gives new hope�if we can just get all the players onside. CMAJ 1998;158:1625�31.