Contents
How Traumatic Brain Injuries Affect Posture: From Balance Issues to Abnormal Stiffening and How Chiropractic Care Can Help

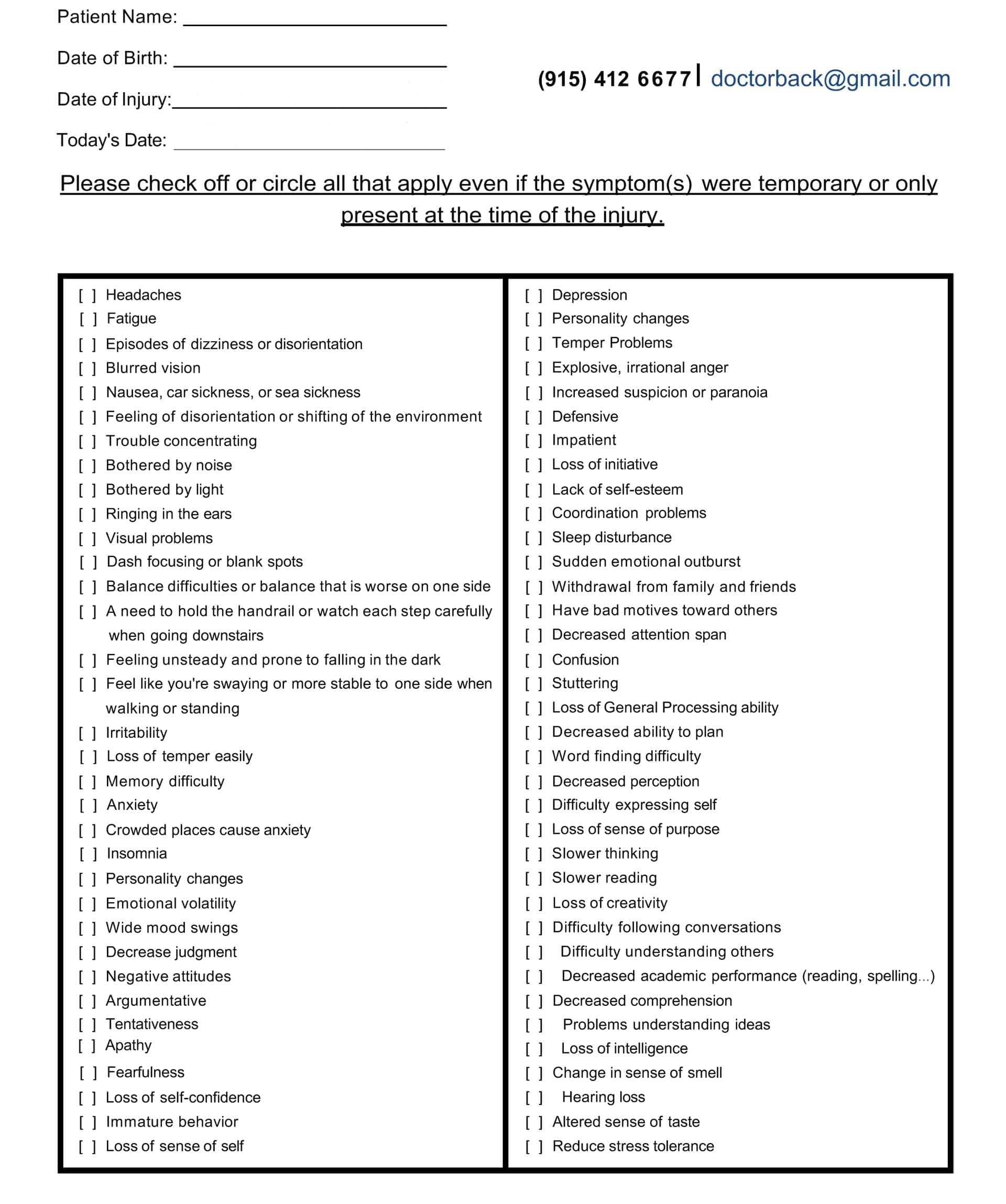
The doctor consults with the patient using the medical traumatic brain injury symptom questionnaire.
Traumatic brain injuries, or TBIs, happen when a sudden bump or blow to the head damages the brain. These injuries can range from mild, like a concussion, to severe, where the brain suffers major harm. One key way TBIs impact the body is through changes in posture—the way we hold and balance ourselves. In mild cases, individuals may experience persistent balance issues that make standing or walking difficult. In severe cases, the body can lock into stiff, unnatural positions known as abnormal posturing. TBIs can also cause the spine to shift out of place, especially in the neck and upper back areas, leading to more issues like headaches and dizziness.
This article explores these effects in detail. It examines how damage to specific brain areas, such as those involved in sensory processing, vision, or inner ear balance, can disrupt postural control. We will also discuss how chiropractic care, which focuses on fixing spine alignments, can help by improving nerve signals, blood flow, and body coordination. Drawing from medical sources and experts, such as Dr. Alexander Jimenez, a chiropractor with over 30 years of experience, we see how integrated treatments support recovery without the need for drugs or surgery.
Understanding Traumatic Brain Injuries and Their Range
TBIs affect millions each year, from sports accidents to falls or car crashes. Mild TBIs, often called concussions, might seem minor at first but can have a lasting effect on how the body maintains balance. Severe TBIs, on the other hand, can cause immediate and life-threatening changes, including rigid body positions that signal deep brain damage. Balance relies on the brain working with muscles, eyes, and the inner ear systems to keep us steady. When a TBI affects these areas, posture suffers, making everyday tasks more challenging.
Research shows that even after mild TBIs heal, people can have subtle shifts in how they control their posture. For example, studies using special tests found that those with past concussions show different patterns in body sway compared to healthy people. These changes may not be apparent in basic balance checks but become visible in more detailed analyses. This means that the brain’s ability to adapt and remain stable can weaken over time, increasing the risk of falls.
In severe TBIs, the damage often hits deeper brain parts, leading to reflexive stiffening. This is the body’s way of reacting without conscious control, and it requires prompt medical attention to prevent worse outcomes.
Symptom Questionnaire:
Subtle and Long-Lasting Balance Problems from Mild TBIs
Mild TBIs don’t always cause obvious symptoms right away, but they can quietly change postural control for months or years. Postural control refers to the brain’s ability to maintain the body’s upright and balanced position during movement or rest. It involves integrating signals from the eyes (visual system), inner ear (vestibular system), and body sensors (sensory system). A TBI can disrupt any of these, leading to dizziness, unsteadiness, or trouble walking straight.
For instance, about 30% to 65% of people with brain injuries report balance issues. These problems stem from weakened muscle strength, poor coordination, or faulty signals from the central nervous system. In one study of over 900 adults with TBIs, only 16% had normal standing balance soon after injury, showing how common these issues are. Factors like age play a role—younger people under 50 tend to recover balance more quickly—but severe injuries or complications, such as infections, can worsen the condition.
These balance changes can be subtle. People might lean to one side without noticing or feel dizzy in crowded places. Over time, this affects daily life, from climbing stairs to playing sports. The brain’s vestibular system, which regulates head position and motion, is often the most severely affected, leading to ongoing instability. Visual problems, such as blurry vision, add to the mix, making it harder for the brain to process where the body is in space.
Dr. Alexander Jimenez, a chiropractor and family nurse practitioner in El Paso, Texas, notes in his clinical work that hidden TBI symptoms, such as these balance shifts, are often overlooked. He emphasizes the importance of early checks and integrative care to identify and address issues before they worsen. His approach combines chiropractic adjustments with nutrition to support long-term healing.
Severe TBIs and Abnormal Posturing: Decorticate and Decerebrate Types
In severe TBIs, the body can exhibit abnormal posturing—stiff, reflexive poses that indicate serious brain damage. These aren’t voluntary; they’re automatic responses from damaged areas of the brain. Two main types are decorticate and decerebrate posturing, both of which require urgent care.
Decorticate posturing happens when damage affects the brain’s outer layers or midbrain pathways. The arms bend inward toward the chest, with clenched fists and curled wrists. Legs stay straight and extended, toes pointing down. The flexed upper body and rigid lower body give the person a stiff and unbalanced appearance. It’s often a sign of a head injury and can happen on one or both sides. The survival rate is about 37%, which is better than the other type, but it still means coma or deep unconsciousness.
Decerebrate posturing is more severe and often associated with deeper brain damage, such as in the brainstem. Here, arms and legs extend straight out, toes point down, and the head arches back with the neck stiff. Muscles tighten rigidly, sometimes with severe spasms called opisthotonos. This extended pose signals life-threatening issues and has only a 10% survival rate. Both types respond to pain or stimuli in unconscious people and require immediate help, like breathing support or ICU care.
These postures render balance impossible, as the body becomes rigid and inflexible. They result from disrupted nerve paths that control movement. Quick treatment focuses on stabilizing the brain to stop more damage.
Spinal Misalignments from TBIs: Adding to Posture Problems
TBIs not only damage the brain, but they can also cause spinal misalignment, particularly in the cervical and thoracic regions of the neck. This occurs due to the force of the injury, such as in whiplash resulting from a car accident. Misalignments, or subluxations, mess up posture by causing uneven weight distribution and muscle strain.
Poor spinal alignment worsens TBI symptoms. Headaches intensify from pinched nerves, and dizziness increases because blood and fluid flow to the brain gets blocked. Studies show TBIs often lead to ongoing musculoskeletal pain, like in the back or shoulders, from these shifts. In one hospital study, 85% of brain injury patients had pain, often from spine issues.
Dr. Jimenez notes a connection between TBIs and spinal issues such as disc herniations, which lead to inflammation and pain. He uses chiropractic to realign the spine and reduce these effects, promoting better posture and less dizziness.
Chiropractic Integrated Care: A Path to Recovery
Chiropractic care provides a natural approach to addressing TBI-related posture issues. It begins with spinal adjustments—gentle movements to correct misalignments. This optimizes the nervous system, as the spine protects the nerves that link the brain to the body. Better alignment means clearer signals, helping with balance and coordination.
For TBIs, chiropractic care can enhance blood and cerebrospinal fluid flow to the brain, facilitating healing and reducing inflammation. This reduces headaches, dizziness, and fatigue. Integrated care incorporates sensory and motor therapies, such as balance exercises or eye movement drills, to retrain the brain. These help rebuild postural control by strengthening muscles and improving proprioception—the sense of body position.
One approach includes soft tissue massage to ease tension and rehab exercises for strength. Lifestyle tips, such as eating anti-inflammatory foods and managing stress, support overall recovery.
Dr. Jimenez’s work highlights this integration. At his clinic, he combines chiropractic with functional medicine for TBIs, focusing on root causes like spinal shifts. His insights demonstrate how adjustments can restore mobility and reduce pain, often in conjunction with a balanced diet to combat inflammation. Patients experience improved posture and reduced symptoms through personalized plans.
Chiropractic care isn’t a cure-all, but it works well in conjunction with medical care. For mild TBIs, it alleviates ongoing balance issues; for severe cases, it supports recovery after acute treatment. The costs of TBIs run high—over $13 billion annually—so non-invasive options like this can be beneficial.
Wrapping Up: Hope Through Awareness and Care
TBIs change posture in ways big and small, from wobbly balance in mild cases to rigid posturing in severe ones. Spinal misalignments add layers of trouble, worsening headaches and instability. But chiropractic integrated care provides tools to fight back—adjustments for alignment, therapies for coordination, and holistic steps for healing.
Experts like Dr. Jimenez remind us that early action and combined treatments make a difference. If you or someone you know has a TBI, talk to a doctor about these options. With the right support, achieving better posture and an improved quality of life is possible.
References
Brain Injury Association of America. (n.d.). Factors associated with sitting and standing balance. https://biausa.org/professionals/research/tbi-model-systems/factors-associated-with-sitting-and-standing-balance
Brain Injury Canada. (n.d.). Mobility. https://braininjurycanada.ca/en/effects-brain-injury/physical/mobility/
Cleveland Clinic. (n.d.). Decorticate posturing. https://my.clevelandclinic.org/health/symptoms/24969-decorticate-posturing
Flint Rehab. (n.d.). Posturing after brain injury: Types and recovery outlook. https://www.flintrehab.com/posturing-brain-injury/
HML Functional Care. (n.d.). How chiropractic neurology supports brain healing. https://hmlfunctionalcare.com/how-chiropractic-neurology-supports-brain-healing/
Impact Medical Group. (2024). Can chiropractic care help with mild traumatic brain injuries? https://www.impactmedicalgroup.com/2024/06/26/can-chiropractic-care-help-with-mild-traumatic-brain-injuries/
Jimenez, A. (n.d.). El Paso, TX, doctor of chiropractic. https://dralexjimenez.com/
Jimenez, A. (n.d.). LinkedIn profile. https://www.linkedin.com/in/dralexjimenez/
Mount Sinai. (n.d.). Decerebrate posture. https://www.mountsinai.org/health-library/symptoms/decerebrate-posture
Mount Sinai. (n.d.). Decorticate posture. https://www.mountsinai.org/health-library/symptoms/decorticate-posture
Northwest Florida Physicians Group. (n.d.). Using chiropractic care to treat traumatic brain injuries. https://northwestfloridaphysiciansgroup.com/using-chiropractic-care-to-treat-traumatic-brain-injuries/
Pinnacle Health Chiro. (n.d.). Six ways chiropractic care supports healing after TBI. https://www.pinnaclehealthchiro.com/blog/six-ways-chiropractic-care-supports-healing-after-tbi
Sosnowski, A. S., et al. (2018). Patients receiving chiropractic care in a neurorehabilitation hospital: A descriptive study. https://pmc.ncbi.nlm.nih.gov/articles/PMC5937508/
Sosnowski, D. W., et al. (2011). Previous mild traumatic brain injury and postural-control dynamics. https://pmc.ncbi.nlm.nih.gov/articles/PMC3017494/
Think Vida. (n.d.). Treating concussions with chiropractic care. https://thinkvida.com/blog/treating-concussions-with-chiropractic-care/
UF Health. (n.d.). Decerebrate posture. https://ufhealth.org/conditions-and-treatments/decerebrate-posture
General Disclaimer, Licenses and Board Certifications *
Professional Scope of Practice *
The information herein on "Traumatic Brain Injuries and Posture Impact Explained" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and on our family practice-based chiromed.com site, focusing on naturally restoring health for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |