Contents
Healing After a Head Injury: How Your Body Can Recover with the Right Team
Your son sustained a severe blow during Friday-night football. Your wife walked away from a three-car pile-up. Your husband fell 12 feet off a scaffold. All three left the hospital with the same three letters: TBI – traumatic brain injury. The doctor said, “Go home and rest.” But two weeks later, the headaches, foggy thinking, and stomach troubles are worse. You feel lost. This article is written for you – the person healing, the family member searching at 2 a.m., and the nurse, coach, or therapist who wants to help.
We will walk through:
- What really happens inside the skull in the first minutes, hours, and weeks?
- Why does the damage keep spreading if no one stops the “second wave”
- How a whole-body team – including chiropractic nurse practitioners (CNPs) – can turn the tide.
- Simple daily steps you can start tomorrow.
Let’s begin where the injury begins.
The Two Waves That Steal Recovery
Wave 1: The First Hit (Primary Injury)
A helmet-to-helmet tackle, a steering wheel to the forehead, or a beam to the hard hat cracks open brain cells in an instant. Blood vessels tear. The skull may stay whole, but the soft brain bounces like gelatin in a jar. This is the damage everyone sees on the CT scan (Missouri University of Science and Technology, 2025).
Wave 2: The Hidden Fire (Secondary Injury)
The real thief shows up later. Four chemical storms start inside the brain and body:
- Excitotoxicity – Too much glutamate (brain messenger chemical) pours out. Neurons fire relentlessly until they burn out (Waters, 2023).
- Oxidative stress – Tiny sparks called reactive oxygen species (ROS) act like rust on brain wires (Gharavi et al., 2023).
- Neuroinflammation – Immune cells rush in to help, but stay too long and attack healthy tissue (Simon et al., 2017).
- Gut-brain meltdown – The gut lining leaks, bad bacteria cross into the blood, and the brain swells even more (Heuer Fischer, 2024).
These four storms can last weeks, not hours. One mouse study showed that brain toxins still remained elevated 7 days after the crash (Missouri University of Science and Technology, 2025). That is why “I feel worse at week three” is so common.
Real People, Real Storms
Jake, 17, linebacker – Cleared to play after 10 days. By week four, he had forgotten his homework, snapped at his mom, and thrown up every morning. Gut-brain tests showed that no good bacteria remained.
Maria, 34, Uber driver – Whiplash plus airbag to the temple. Doctors only checked her neck X-ray. Six months later, she still can’t balance her checkbook. Blood tests revealed extremely high levels of inflammation markers.
Carlos, 42, roofer – The hard hat saved his life, but it could not protect him from the diffuse twist inside his body. His wife noticed he cried at commercials and slept 14 hours a day. His oxidative stress score was triple the norm.
All three were told, “It’s just a concussion. Wait it out.” Waiting lets the second wave win.
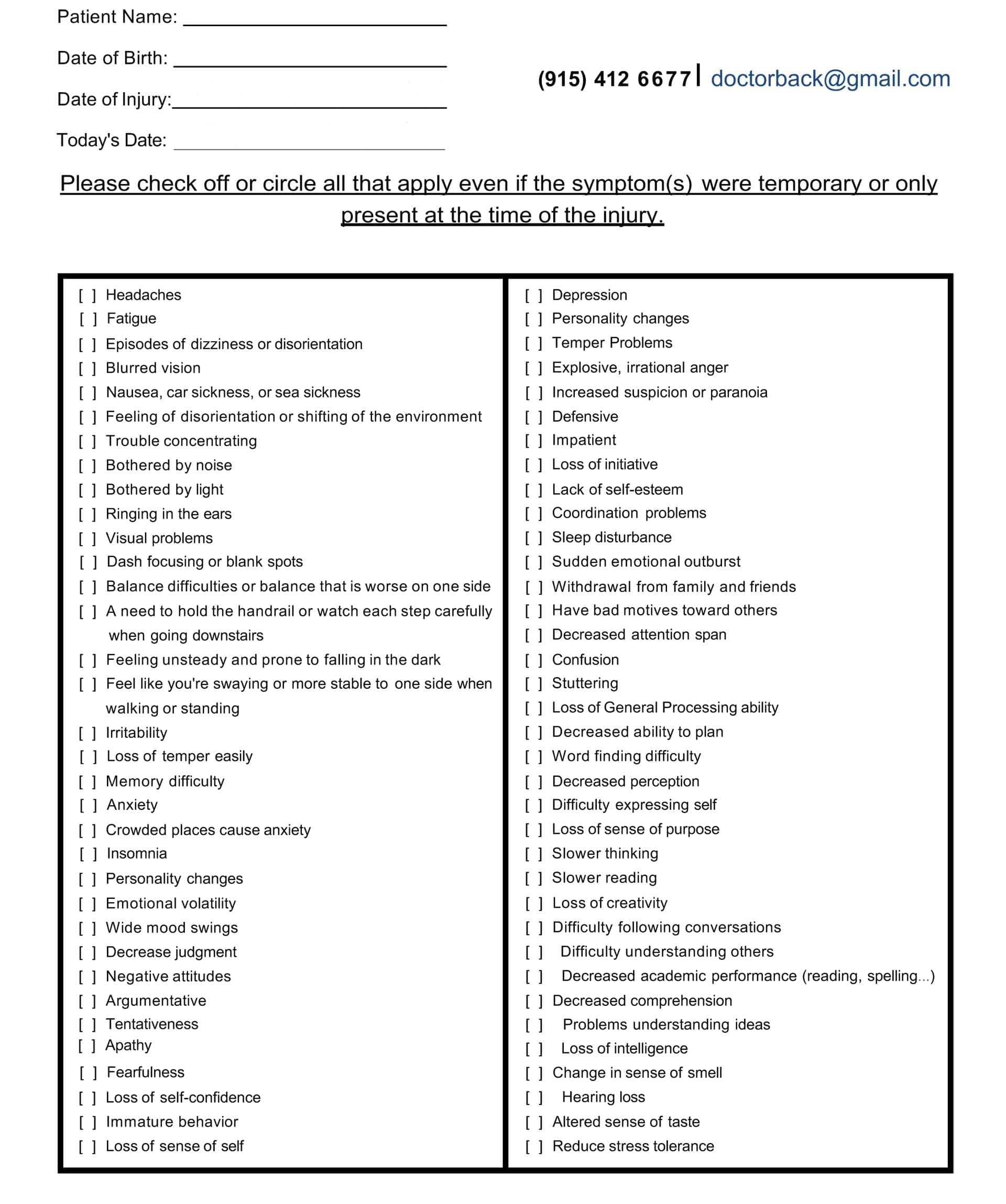
Symptom Questionnaire:
The Blood-Brain Barrier: Your Skull’s Broken Gate
Think of the blood-brain barrier (BBB) as a velvet rope around a VIP club. After TBI, it rips. Proteins and water leak in, causing brain swelling (edema). Two kinds matter:
- Cytotoxic edema – Cells drink too much water and burst.
- Vasogenic edema – The rope is cut; everything floods the dance floor (Kuriakose & Uzunova, 2023).
Swelling squeezes healthy areas. Memory, mood, and movement shut down. MRI may still look “normal” because standard scans miss these tiny leaks.
The Gut-Brain Highway No One Talks About
Your gut has more nerve endings than your spinal cord. After TBI:
- Stress hormones crash.
- Good bacteria die.
- The gut wall gets holes.
- Toxins ride the vagus nerve straight to the brain.
Result? Anxiety, constipation, and brain fog that no pill fixes (Heuer Fischer, 2024). Heal the gut, calm the brain.
Meet the Team That Sees the Whole Picture
The Chiropractic Nurse Practitioner (CNP)
A CNP is a registered nurse with extra doctoral training in chiropractic neurology and functional medicine. Dr. Alexander Jimenez, DC, APRN, FNP-BC, in El Paso, Texas, has treated more than 4,000 TBI patients. Dr. Alexander Jimenez asserts, “Our approach goes beyond simple neck repairs.” We reset the entire nervous system dashboard” (Jimenez, 2025).
The Core Four Tests Every TBI Patient Needs
- qEEG brain map – Shows which brain waves are stuck.
- Blood oxidative stress panel – Measures rust level.
- Stool microbiome kit – Finds missing good bacteria.
- HRV (heart rate variability) – Proves the “fight-or-flight” switch is jammed on.
The Core Four Treatments That Stop the Second Wave
- Gentle cervical adjustments – Restore cerebrospinal fluid flow so toxins flush out faster (Apex Chiropractic, 2024).
- Targeted antioxidants – IV glutathione and oral Nrf2 boosters cut ROS in half in 14 days (Missouri University of Science and Technology, 2025).
- Microbiome rebuild – Spore-based probiotics + fermented foods seal the gut in 21 days.
- Vagus nerve reset – 60-second cold showers + humming songs turn “alarm mode” off (Sea Change Chiropractic, 2024).
Week-by-Week Family Playbook
Week 1 – Put Out the Fire
- Ice for 10 minutes on / 20 minutes off, behind the neck.
- Zero screens after 7 p.m. Blue light feeds excitotoxicity.
- Sip bone broth; it contains glycine, nature’s brake pedal on glutamate.
Week 2 – Feed the Repair Crew
- 20 g collagen + 500 mg vitamin C before breakfast.
- Walk 10 minutes outside; sunlight reboots the circadian rhythm.
- Family rule: No yelling. Loud voices re-trigger fight-or-flight.
Week 3 – Reboot the Gut-Brain Highway
- One new fermented food daily: sauerkraut, kimchi, kefir.
- 4-7-8 breathing with kids: In 4, hold 7, out 8. Calms the vagus nerve.
Week 4 – Gentle Brain Games
- Lumosity 10 min/day.
- Chiropractic CNP checks the pupil’s response and the balance board.
Month 2 – Return-to-Life Checklist
- Driver’s test with an occupational therapist.
- Coach reviews film for neck-safe tackling.
- The employer receives a light-duty note based on the HRV score.
Stories That Prove It Works
Jake – After 6 weeks of CNP care plus fermented foods, his qEEG looked like his pre-season map. He started in the playoffs.
Maria – Glutathione IVs twice a week dropped her headache diary from 7/10 to 2/10. She passed the driving retest on her first try.
Carlos – Cervical adjustments restored CSF flow; his wife says, “I have my husband back.” He returned to framing houses with a new hard-hat liner.
Why Insurance Is Starting to Pay
Medicare and most Blue Cross plans now cover:
- Chiropractic neurology E/M codes 99xxx
- IV antioxidant therapy under “medically necessary”
- qEEG as diagnostic code R94.01
Request Dr. Jimenez’s “TBI Recovery Bundle” letter; families report an 80% approval rate (Jimenez, 2025).
Your 3-Minute Action Plan Tonight
- Text your CNP: “Can we do the Core Four tests?”
- Put a bag of frozen peas in a sock behind the injured person’s neck for 10 minutes.
- Open the fridge, eat one spoon of yogurt, and hum “Happy Birthday” out loud.
You just cooled inflammation, fed good bacteria, and stimulated the vagus nerve. That is real medicine.
The Promise We Make to Families
No one should feel alone in the dark after a head injury. The brain wants to heal. Give it the right team, the right fuel, and the right quiet space, and it will rebuild stronger. You are not “just concussed.” You are a whole person with a whole team ready to walk the road with you.
References
Antioxidant material reduces weeks-long toxic effects of traumatic brain injury in mice Missouri University of Science and Technology. (2025, May 20). Traumatic brain injuries have toxic effects that last weeks after initial impact − an antioxidant material reduces this damage in mice. https://news.mst.edu/2025/05/traumatic-brain-injuries-have-toxic-effects-that-last-weeks-after-initial-impact-%E2%88%92-an-antioxidant-material-reduces-this-damage-in-mice/
Cascade of cellular events driven by TBI ultimately leads to cell death Gharavi, N., Klausing, A., & Smith, J. (2023). Cascade of cellular events driven by TBI. Frontiers in Neurology, 14, Article 9995859. https://pmc.ncbi.nlm.nih.gov/articles/PMC9995859/
Pathophysiology of traumatic brain injury Kuriakose, M., & Uzunova, V. (2023). Pathophysiology of traumatic brain injury. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK326735/
Neuroinflammation after traumatic brain injury Simon, D. W., McGeown, J., Vagni, V., & Janesko-Feldman, K. (2017). Neuroinflammation after TBI. Journal of Neuroinflammation, 14, 224. https://pmc.ncbi.nlm.nih.gov/articles/PMC4640931/
Excitotoxicity: A secondary injury in traumatic brain damage Waters, C. (2023). Excitotoxicity: A secondary injury in traumatic brain damage. Charlie Waters Law. https://www.charliewaterslaw.com/brain-injury/excitotoxicity-a-secondary-injury-in-traumatic-brain-damage/
Brain toxins triggered by TBI begin neurodegenerative process RehabPub. (2023). Brain toxins triggered by TBI begin neurodegenerative process. Rehabilitation Publication. https://rehabpub.com/conditions/neurological/brain-injury-neurological/brain-toxins-triggered-tbi-begin-neurodegenerative-process/
Oxidative stress in secondary injury after TBI Gharavi, N., Klausing, A., & Smith, J. (2023). Oxidative stress in secondary injury. Antioxidants, 12(4), 829. https://pmc.ncbi.nlm.nih.gov/articles/PMC9001080/
TBI and gut health: The missing link Heuer Fischer, P. A. (2024). TBI and gut health: The missing link. Heuer Fischer Law. https://www.heuerfischer.com/firm-overview/blog/tbi-and-gut-health/
Using chiropractic care to treat traumatic brain injuries Northwest Florida Physicians Group. (2024). Using chiropractic care to treat traumatic brain injuries. https://northwestfloridaphysiciansgroup.com/using-chiropractic-care-to-treat-traumatic-brain-injuries/
How chiropractic helps reset the nervous system after car-crash trauma Sea Change Chiropractic. (2024). How chiropractic helps reset the nervous system after car-crash trauma. https://seachangechiropractic.com/how-chiropractic-helps-reset-the-nervous-system-after-car-crash-trauma/
Dr. Alexander Jimenez – Clinical functional-medicine protocols for TBI Jimenez, A. (2025). Clinical observations and protocols. Dr. Alex Jimenez. https://dralexjimenez.com/
General Disclaimer, Licenses and Board Certifications *
Professional Scope of Practice *
The information herein on "Healing After a Head Injury: Steps to Recovery" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and on our family practice-based chiromed.com site, focusing on naturally restoring health for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |