Auto Accident Injuries
Back Clinic Auto Accident Injuries Chiropractic and Physical Therapy Team. Many automobile accidents occur throughout the world every year, affecting a wide number of individuals, both physically and mentally. From neck and back pain to bone fractures and whiplash, auto accident injuries and their associated symptoms can challenge the daily lives of those who experienced unexpected circumstances.
Dr. Alex Jimenez’s collection of articles discusses auto injuries caused by trauma, including which specific symptoms affect the body and the particular treatment options available for each injury or condition resulting from an auto accident. Being involved in a motor vehicle accident can not only lead to injuries but they can be full of confusion and frustrations.
It is very important to have a qualified provider specializing in these matters completely assess the circumstances surrounding any injury. For more information, please feel free to contact us at (915) 850-0900 or text to call Dr. Jimenez personally at (915) 540-8444.

MVA’s Recovery and Healing at El Paso Back Clinic
Common Motor Vehicle Accidents in El Paso: Recovery and Healing at El Paso Back Clinic®
Motor vehicle accidents, or MVAs, are a big issue in El Paso. This city sits on the border, with lots of trucks and cars zooming on roads like I-10 and Loop 375. Accidents often result from drivers not paying attention, drinking, or speeding. They can lead to injuries like neck pain or broken bones. At El Paso Back Clinic®, we help people heal from these injuries. Our team, led by Dr. Alexander Jimenez, uses integrative chiropractic care. This mixes spine fixes with massage, exercise, and healthy eating tips. It treats the whole body and mind. In this article, we discuss common crashes in El Paso, the harm they cause, and how our clinic supports recovery. We draw on Dr. Jimenez’s expertise at our locations in El Paso, TX.
El Paso has many crashes each year. Recent data shows thousands of wrecks, with injuries and even deaths. The border sees heavy truck traffic, upping the risks. Dust storms or rain-slick roads. Work zones add hazards. Knowing this helps folks drive safely. At El Paso Back Clinic®, we see many patients from these events. Our care focuses on pain relief and full health.
Common Types of Motor Vehicle Accidents in El Paso
El Paso’s roads mix locals, visitors, and cross-border traffic. This leads to jam-ups and crashes. Here are the key types:
- Distracted Driving Accidents: Phones or snacks pull drivers’ eyes from the road. In El Paso, this sparks many wrecks. Texting hits hard at spots like Mesa and Stanton streets. Texas-wide, it caused over 84,000 crashes in one year.
- Drunk or Impaired Driving: Booze or drugs slow folks down. Crashes spike nights and weekends. It’s a top cause in Texas spots like El Paso. They pop up near fun zones like Cincinnati Avenue.
- Speeding-Related Crashes: Too fast means tough stops. It makes up 30% of Texas wrecks. On I-10 and Loop 375, speed leads to bad hits. Winds make it worse.
- Rear-End Collisions: Cars bump backs from close follows or late brakes. Common on Loop 375 in traffic or near shops like Cielo Vista. Distractions or weather help cause them.
- Intersection Crashes: Red-light runs or no yields cause side smacks. Over half happen at crossings like Montana or Zaragoza. The Spaghetti Bowl adds mess. Stop sign skips are big faults.
- Pedestrian Incidents: Walkers get struck when drivers miss spots or speed. Downtown, schools, or UTEP see many. Poor walks led to many deaths lately.
- Truck Accidents: Border hauls mean big trucks everywhere. Thousands cross yearly. Recent counts show many truck wrecks with injuries. Tired drivers, heavy loads, or blind areas cause them. Spots like I-10, US-54, and Loop 375 are hot.
Pile-ups hit in storms on I-10. Lane changes in builds confuse. Hit-runs occur in town. Stay alert, slow down, and watch out for trucks to avoid.
At El Paso Back Clinic®, we treat folks from all these. Our team knows border traffic woes. We offer care plans for quick heals.
Common Injuries Sustained in Motor Vehicle Accidents
MVAs jolt bodies hard. Sudden moves cause hidden hurts. Here are the usual ones:
- Whiplash: Neck snaps cause pain, stiffness, headaches, and dizziness. Top in rear-ends.
- Neck and Back Sprains: Pulls or tears cause pain and reduced movement. Low back twists.
- Soft Tissue Damage: Bruises, rips in muscles. Swell, stiff. Deep ones last.
- Headaches: From whiplash or bumps. They linger.
- Herniated Discs: Spine pads slip, pinch nerves. Pain shoots.
- Fractures: Breaks from hits. Ribs puncture lungs. Bad ones need ops. Limbs, spine too.
- Traumatic Brain Injuries (TBIs): Head knocks cause mix-ups, forgetfulness, and eye issues. Change lives, cost lots.
Shoulders, knees, and inside bleed too. Burns and scars are possible. Trucks crush more. Walkers break bones, heads. Minor ones spark worry or PTSD.
At our clinic, we spot these early. Dr. Jimenez’s team uses checks to plan care.
How These Injuries Occur
Crashes stop or hit fast. Bodies fly in cars. Belts save, but force hurts. Rear-ends jerk heads, stretch necks for whiplash. Sides twist spines for sprains, disc slips. Heads hit for TBIs. Knees dash-bang for sprains. Moves inflame tissues. Trucks smash small cars, break bones. Walkers fly, land hard. Signs may be delayed, so check soon.
We urge quick visits. Our El Paso spots offer fast help.
Integrative Chiropractic Care at El Paso Back Clinic® for MVA Recovery
Our integrative care treats all of you. We fix spines hands-on, easing pain without pills or cuts first. Mixes old ways with massage, PT, and nutrition. Speeds heal, drops swell. Here’s our approach:
- Spinal Adjustments: Move bones right, cut nerve pinch, up move. Great for whiplash, back.
- Massage Therapy: Loosens muscles, breaks scars. Boosts blood, drops swell in tissues.
- Physical Therapy: Builds strong, flexible. Restores after sprains and breaks.
- Nutritional Support: Food advice; adds fight-swell, up mood.
- Other Therapies: Needle work or disc pull. Ease pain, stress.
We speed recovery, hit the body and feelings. Start in 72 hours, best. Stops long pain. Our functional medicine finds roots.
Insights from Dr. Alexander Jimenez and El Paso Back Clinic®
Dr. Alexander Jimenez, DC, APRN, FNP-BC, has headed El Paso Back Clinic® for 30+ years. He excels in MVA, which includes injuries like whiplash and TBIs. We use functional medicine, nutrition, and rehab. Holistic care heals body and mind from trauma. Cases show fast recovery from car and truck hits. Border traffic brings many to us. Our spots at 11860 Vista Del Sol and 6440 Gateway East offer full care. Call 915-850-0900 for help.
Conclusion
El Paso MVAs from busy roads hurt many. From whiplash to TBIs, harms vary. El Paso Back Clinic® gives natural healing. We cut pain, restore movement. See us after crashes. Safe drives prevent woes. Visit elpasobackclinic.com or call for wellness.
References
A2X Law. (n.d.). El Paso car crash statistics. https://www.a2xlaw.com/el-paso-car-crash-statistics
Abrar and Vergara. (n.d.). El Paso car accident statistics. https://theavlawyer.com/el-paso-car-accident-lawyer/statistics/
Altitude Health. (n.d.). Comprehensive care: Integrating chiropractic, physiotherapy, naturopathy, and more for motor vehicle accident recovery. https://www.altitudehealth.ca/comprehensive-care-integrating-chiropractic-physiotherapy-naturopathy-and-more-for-motor-vehicle-accident-recovery/
Amaro Law Firm. (n.d.). El Paso truck accident lawyer. https://amarolawfirm.com/el-paso-truck-accident-lawyer/
Amanda Demanda Injury Lawyers. (n.d.). What Texas cities have the most car accidents?. https://www.callamandademanda.com/blog/tx-cities-most-accidents/
Arnold & Itkin. (n.d.). El Paso truck accident attorneys. https://www.arnolditkin.com/el-paso-personal-injury/truck-accidents/
Azam Injury Law. (n.d.). El Paso motor vehicle accident lawyer – Free help. https://azaminjurylaw.com/area-we-serve/el-paso/motor-vehicle-accident-lawyer/
Dr. Alexander Jimenez, DC, APRN, FNP-BC, IFMCP, CFMP, ATN ♛. (n.d.). LinkedIn profile. https://www.linkedin.com/in/dralexjimenez/
Harmonson Law Firm. (n.d.). El Paso car accident lawyer. https://www.clarkharmonsonattorney.com/el-paso-tx/car-accident-lawyer/
Harmonson Law Firm. (n.d.). El Paso pedestrian accident attorney. https://www.clarkharmonsonattorney.com/el-paso-tx/pedestrian-accident-lawyer/
Injury Medical Clinic PA. (n.d.). Injury specialists. https://dralexjimenez.com/
Inlet Integrated Health Centre. (n.d.). Common injuries from motor vehicle accidents and how chiropractic, physiotherapy, and kinesiology can help. https://www.inletintegratedhealth.com/post/common-injuries-from-motor-vehicle-accidents-and-how-chiropractic-physiotherapy-and-kinesiology-ca
James Kennedy, P.L.L.C. (n.d.). El Paso rear-end collisions attorneys | Free consultation. https://www.epinjury.com/personal-injury/car-accident-crash-wreck/rear-end-collisions
Labinoti Law Firm. (n.d.). El Paso motor vehicle accident attorney. https://www.labinotilaw.com/office-locations/el-paso/personal-injury/motor-vehicle-accident/
MVAMVP. (n.d.). Why chiropractic care is essential after a motor vehicle accident. https://mvamvp.com/why-chiropractic-care-is-essential-after-a-motor-vehicle-accident/
Nix Patterson, LLP. (n.d.). El Paso car accident lawyers. https://nixlaw.com/el-paso/car-accident-lawyers/
Sodhi, R. (n.d.). What you should know about the role of chiropractic and massage in motor vehicle accident recovery. https://www.alwc.ca/role-of-chiropractic-care-and-massage-for-accident-recovery/
Spectrum Therapy Consultants. (n.d.). Motor vehicle accident injuries. https://spectrumtherapyconsultants.com/physical-therapy-services/motor-vehicle-accident-injuries/
The Neck and Back Clinics. (n.d.). Your first chiropractic appointment after a car accident: What to expect and prepare. https://theneckandbackclinics.com/first-chiropractic-appointment/
The Neck and Back Clinics. (n.d.). What are your chiropractic treatment options after a car accident?. https://theneckandbackclinics.com/what-are-your-chiropractic-treatment-options-after-a-car-accident/
The Russo Firm. (n.d.). Where do most El Paso car accidents occur?. https://therussofirm.com/where-do-most-el-paso-car-accidents-occur/

Telemedicine in Integrative Injury Care Benefits
The Role of Telemedicine in Integrative Injury Care at El Paso Back Clinic: Providing Full Support for Car Accident, Work, and Sports Injuries in El Paso, TX
A doctor of chiropractic and a nurse practitioner review the MRI of a patient following a motorcycle collision.
In El Paso, TX, getting injured in a car crash, at work, or during sports can be tough. But at El Paso Back Clinic®, a top wellness chiropractic care spot, new tools like telemedicine make getting help simpler. Telemedicine uses video calls and online apps to let health experts care for you from home. This article explores how the clinic’s integrative nurse practitioner (NP) and chiropractor team up with telemedicine to provide comprehensive injury care. This covers virtual check-ups, treatment planning, and long-term help. It’s super useful for folks who can’t easily move or get to the clinic. The team also shares tips on eating, working out, and daily habits to speed up healing. They keep everything organized and documented for the best outcomes.
El Paso Back Clinic® focuses on functional medicine and holistic healing. Led by Dr. Alexander Jimenez, who is both a chiropractor (DC) and a family nurse practitioner (FNP-BC), the clinic combines conventional medicine with natural approaches to treat injuries. Telemedicine here means you can get exams, diagnoses, and follow-ups without leaving home. This is great for busy El Paso residents or for those who are hurting too much to travel. The clinic’s approach considers your whole body, with the NP and chiropractor working together to create plans that fit your life.
What Is Integrative Care at El Paso Back Clinic?
At El Paso Back Clinic®, integrative care means a team of doctors, therapists, and nutritionists working together to fully heal you. For car accident injuries like whiplash or back strains, the chiropractor adjusts your spine while the NP manages pain and checks for deeper issues. They make custom plans using evidence-based methods.
- Common Injuries Treated: Neck pain from crashes, work lifts causing strains, or sports-related twists leading to sprains.
- Why Choose Integrative?: It targets the cause, not just pain, blending adjustments with lifestyle changes.
- Telemedicine’s Role: Allows remote care, so you start healing right away from home.
This method helps with lasting health. For sports fans in El Paso, tips on better nutrition can speed up recovery (Dallas Accident and Injury Rehab, n.d.).
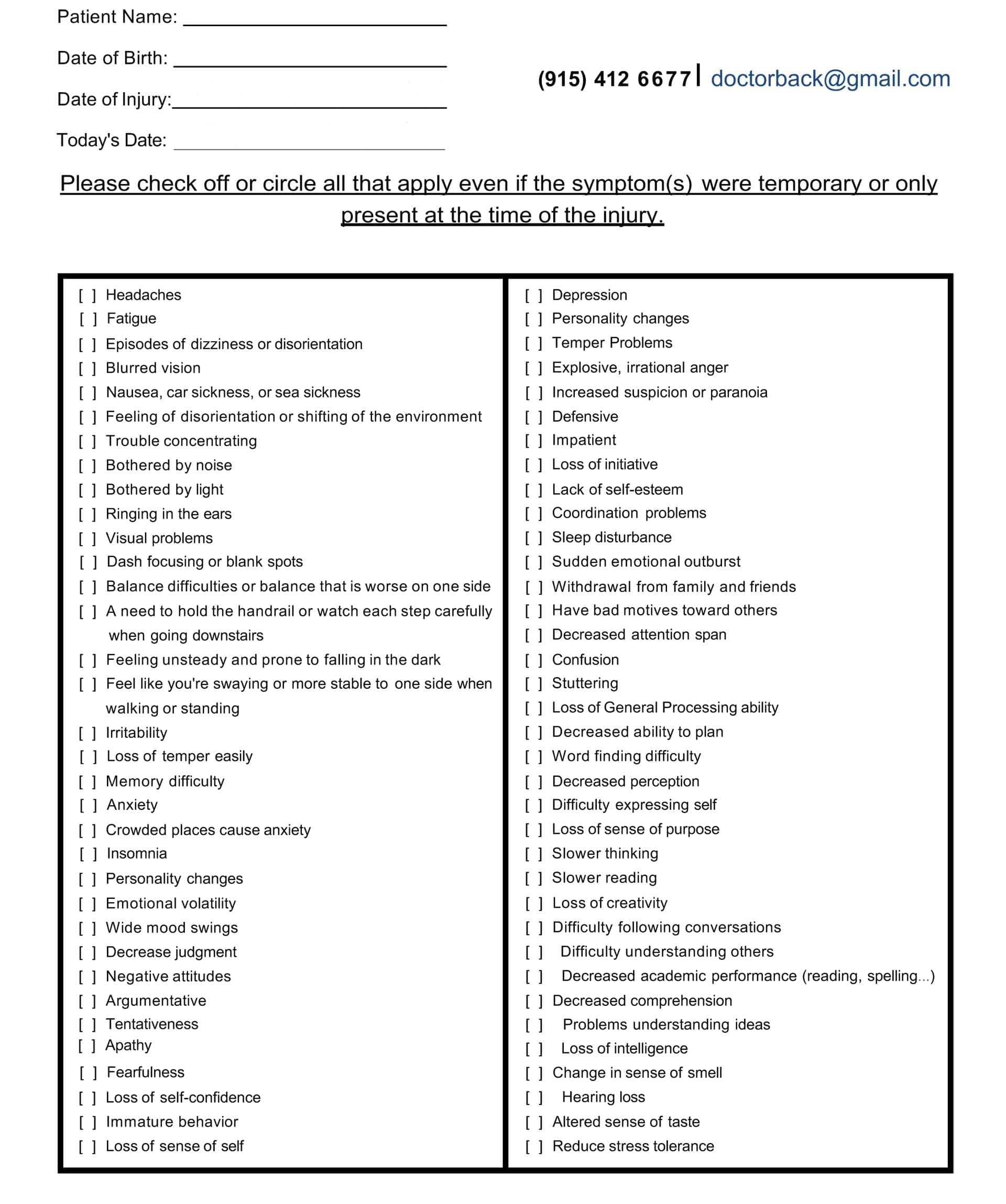
Head Injury/Traumatic Brain Injury Symptom Questionnaire
Virtual Examinations: How El Paso Back Clinic Does It Remotely
Telemedicine at El Paso Back Clinic® starts with virtual exams. You connect via secure video from your phone or computer. Dr. Jimenez or the team talks to you about your injury.
For a car accident, they ask about the crash and pain spots. They watch you move, like bending or walking, to check for swelling or stiffness. Even without hands-on involvement, they spot many problems, such as muscle pulls or nerve issues (Personal Injury Firm, 2025).
Work injuries, like slips, get quick virtual checks to stop things from getting worse. The chiropractor guides home tests, such as balance checks.
- Tools in Virtual Exams: Video for movement, apps for sharing photos of injuries, or devices for vital signs.
- When It’s Not Enough: Some need in-person touches, so they schedule clinic visits at their El Paso locations.
- Sports Injury Perks: Athletes demo their moves, helping find repeat strains.
This remote setup makes getting checked easy, especially in El Paso, where traffic can be a hassle (CK Firm, 2024).
Diagnoses Through Telemedicine at the Clinic
After the exam, the team at El Paso Back Clinic® diagnoses remotely. Common ones from car accidents include whiplash or disc problems. The NP might order X-rays or MRIs, which are performed locally and shared online.
Chiropractors like Dr. Jimenez spot spinal shifts that can cause leg pain, such as sciatica. They explain it clearly on video. The NP assesses whole-body health, including whether swelling worsens.
All sessions are recorded for official documents, insurance keys, or personal injury claims (ChiroMed, n.d.).
- Diagnosis Examples: Work-related back pain, sports-related nerve hits, and crash-neck strains.
- Team Collaboration: NP handles meds; chiropractor does adjustments.
- Tips for Accuracy: Describe pain and show motions well.
This reduces wait times, allowing you to start your El Paso recovery sooner (Complete Care, n.d.).
Managing Treatment Plans Remotely from El Paso Back Clinic
The NP and chiropractor create a treatment plan together, updated via telemedicine. For a sports knee sprain, it might include rest, ice, and shown exercises.
Dr. Jimenez demonstrates stretches on camera. The NP monitors pain and adjusts treatments.
They coordinate to avoid overlaps. For work injuries, plans cover safe job returns. Everything’s online for easy tracking.
- Plan Essentials: Pain relief, movement work, and prevention advice.
- Integrative Touches: Diet tweaks to cut swelling, like more omega-3 foods.
- Telemedicine Updates: Regular video calls to tweak based on progress.
This saves time and money for El Paso patients (Jimenez, n.d.-a).
Ongoing Support and Follow-Up Care at the Clinic
Recovery needs steady help, and El Paso Back Clinic® uses telemedicine for easy follow-ups. Log in to chat about how you’re doing.
For car crash back pain, they check therapy effects and offer encouragement. Support includes mental health tips, as injuries can stress you.
Chiropractors guide home exercises on video. NPs watch for treatment side effects.
- Support Types: Mood talks, progress logs, specialist referrals.
- How Often: Weekly, early on, then less.
- For El Paso Athletes: Safe return-to-play tips, like warm-ups.
This prevents pain from lasting, helping you get back to life fast (Prescient National, n.d.).
Benefits for El Paso Residents with Mobility or Access Issues
Injuries make moving hard, especially in spread-out El Paso. Telemedicine brings care to you.
No travel needed, perfect for remote areas or difficult days. For work injuries, it means less downtime. See pros from home.
- Who Gains Most: Those pained by walking, without transport, or packed schedules.
- Access Help: Shorter waits than office visits.
- Legal Benefits: Docs care for claims without hold-ups.
This makes healing equal for all in El Paso (CK Firm, 2024).
Integrative Advice on Diet, Exercise, and Lifestyle from the Clinic
El Paso Back Clinic® shines with holistic telemedicine tips. They suggest anti-inflammatory foods, such as fruits, to aid healing.
Exercise advice includes easy yoga for pain, demonstrated online. Lifestyle shifts cover better sleep or stress cuts, like apps for calm.
For sports, they teach form to prevent re-injury.
- Diet Ideas: Omega-3 for nerves, antioxidants for fixes.
- Workout Suggestions: Stretches for range, walks for build-up.
- Life Changes: Posture tweaks, drop bad habits.
This addresses root causes for better long-term health (Dallas Accident and Injury Rehab, n.d.).
Coordination and Documentation Between NP and Chiropractor at El Paso Back Clinic
The team shares notes easily on telemedicine platforms. Dr. Jimenez, as both NP and chiropractor, bridges the roles seamlessly.
Records from calls build your file, showing progress for insurance or courts.
Therapies align, like adjustments with rest plans.
- Coordination Methods: Shared digital files, joint calls.
- Record Value: Shows timely, excellent care.
- Your Part: Update honestly for the top plans.
This leads to smooth recoveries in El Paso (Jimenez, n.d.-b).
Insights from Dr. Alexander Jimenez at El Paso Back Clinic
Dr. Alexander Jimenez, DC, APRN, FNP-BC, shares hands-on views from over 30 years at El Paso Back Clinic®. He uses telemedicine for same-day injury exams, like after crashes or sports.
He stresses integrative care for body and mind. For head injuries, he advises sleep, diet, and exercise. His dual license allows him to prescribe medications and adjust spines remotely when possible.
Jimenez highlights tests, such as MRIs, shared online. He combines adjustments in nutrition with other interventions for issues like gut health post-trauma.
- Main Observations: Injuries are linked to overall health, like nerves and digestion.
- Telemedicine in Practice: Quick virtual help for accidents, with shipped braces.
- Tips: Use posture drills and supplements for healing.
His approach shows how the clinic’s NP-chiropractor team excels (Jimenez, n.d.-a; Jimenez, n.d.-b; Jimenez, n.d.-c).
Challenges and Future of Telemedicine at El Paso Back Clinic
Telemedicine has limits, such as the need for touch for some exams. Tech glitches can happen.
But the future is promising. Better apps and AI will improve diagnoses. More insurance covers it.
The clinic trains in remote teamwork.
- Fixing Issues: Have in-person backups, help with tech.
- Coming Trends: Wearables for live data.
- Importance: Makes care more accessible and affordable in El Paso.
Conclusion
At El Paso Back Clinic® in El Paso, TX, telemedicine transforms injury care for car, work, or sports-related injuries. The integrative NP and chiropractor team, led by Dr. Jimenez, offers virtual exams for ongoing support. It includes holistic advice for better living. Ideal for mobility challenges. As Dr. Jimenez proves, this leads to quicker, fuller healing. If injured, reach out to El Paso Back Clinic® for easy, top-notch care at 915-850-0900 or visit their site.
References
Jimenez, A. (n.d.-a). El Paso, TX, doctor of chiropractic. https://dralexjimenez.com/

The Definitive Diagnostic Edge: Why El Paso Attorneys Partner with Dr. Alex Jimenez, DC, APRN, FNP-BC for Medico-Legal Causality, Advanced MRI Interpretation, and Unassailable Injury Dating
Introduction: My Personal Commitment to the Medico-Legal World—Bridging the Gap Between Clinical Science and Courtroom Proof
By Dr. Alex Jimenez, DC, APRN, FNP-BC | Board-Certified Nurse Practitioner & Chiropractor
Injury Medical Clinic PA, El Paso, Texas
The answer to the crucial question of whether the injury can be conclusively proven, dated, and causally connected to the traumatic event frequently determines the outcome of the high-stakes world of personal injury litigation.
My life’s work at Injury Medical Clinic PA is dedicated to answering this question with an unassailable “Yes.” I have spent decades developing a diagnostic and documentation protocol that transcends the limitations of standard clinical practice. For me, a patient is not just a set of symptoms; they are a complex medico-legal case requiring forensic-level analysis. I recognized early on that El Paso attorneys needed more than a standard radiologist’s report or a simple chiropractor’s diagnosis—they needed a comprehensive, integrated expert who could seamlessly bridge advanced musculoskeletal biomechanics (my foundation as a Chiropractic Physician, DC) with the rigorous standards of comprehensive medical management and documentation (my expertise as a Board-Certified Nurse Practitioner, APRN, FNP-BC).
This unique duality is the engine of our practice. I am not just treating the patient; I am building the legal case. My goal for every personal injury client referred to me is to deliver definitive diagnostic proof that withstands the most rigorous cross-examination, establishes clear causality using objective biomechanical markers, and determines a scientifically validated timeline for the injury—what I call injury dating.
This lengthy post serves as my own, in-depth guide to legal counsel, shedding light on the extent of my involvement in the evaluation of injuries. I meticulously examine the procedures that I use to assess patient cases. These procedures are indispensable for determining the root cause of an illness and for shedding light on the actual degree of disability and impairment that has resulted from traumatic events. I take great pride in my role as a professional in that I am committed to the idea that when a clinical case is brought before a jury, the attorneys representing the plaintiff have complete confidence in the credibility and scientific basis of the expert testimony that I provide.
I will deeply discuss, from my personal experience:
-
The Diagnostic Imperative: My sophisticated capability to personally stage and interpret complex Magnetic Resonance Imaging (MRI) findings, distinguishing acute trauma from pre-existing conditions using forensic principles.
-
Causality and Timing: My systematic, proprietary methodology for establishing causality and determining the precise timing (injury dating) of trauma using advanced biomechanical and physiological markers like Modic changes and Wolff’s Law.
-
The Dual-Licensed Advantage: The justification and profound benefit of treatment and testimony provided by me, a dual-licensed professional, within the El Paso legal community.
-
Expert Credibility: How attorneys frequently utilize my expert testimony as the credible, objective voice regarding injury dating, impairment, and functional loss, ensuring my documented assessments and evaluations meet the stringent Daubert Standard.
1.0 The Diagnostic Imperative: Personally Staging and Interpreting Complex MRI Findings—Going Beyond the Radiologist’s Report
In my experience, the Magnetic Resonance Imaging (MRI) scan is the single most crucial piece of objective evidence in spinal injury litigation. However, I’ve found that a standard radiologist report often focuses primarily on morphology—describing what is seen—but fails to provide the critical context of causality and chronicity necessary for a successful legal claim.
At Injury Medical Clinic PA, I do not simply accept the outside read; I forensically interpret the physiological, mechanical, and temporal signatures embedded within the MRI data myself. I personally review every single slice and sequence because my ultimate testimony depends on my deep understanding of the images.
1.1 Meeting the Daubert Standard: My Personal Protocols for Scientific Admissibility
In the medico-legal domain, any scientific evidence I present, especially complex imaging findings, must adhere to the Daubert Standard. This requires my expert testimony to be grounded in the methods and procedures of science and supported by appropriate validation (Spinal Diagnostics, n.d.). My entire documentation protocol is built around this necessity.
I personally ensure my findings are admissible by:
-
Employing Validated Methodology: I utilize diagnostic criteria and staging methods that are thoroughly established in peer-reviewed orthopedic and radiological literature, such as the classification of disc pathology and the chronology of vertebral changes (Wang et al., 2017).
-
Focusing on Objectivity: My reports meticulously cite the specific MRI pulse sequences (T1, T2, STIR) and image numbers where the pathology is visualized, allowing opposing counsel and the court to verify the data. This objectivity mirrors the rigor seen in advanced quantitative neuroimaging tools like NeuroQuant®, which are successfully used to meet the Daubert standard in TBI cases (National Institutes of Health, 2022).
-
Simplifying Complex Science: When I testify, my goal is to translate complex terms into easily digestible concepts for the jury. I do not just state a Modic 1 change is present; I explain why it’s a marker of acute trauma, making the science reliable and understandable. This is a crucial skill that attorneys rely on me for.
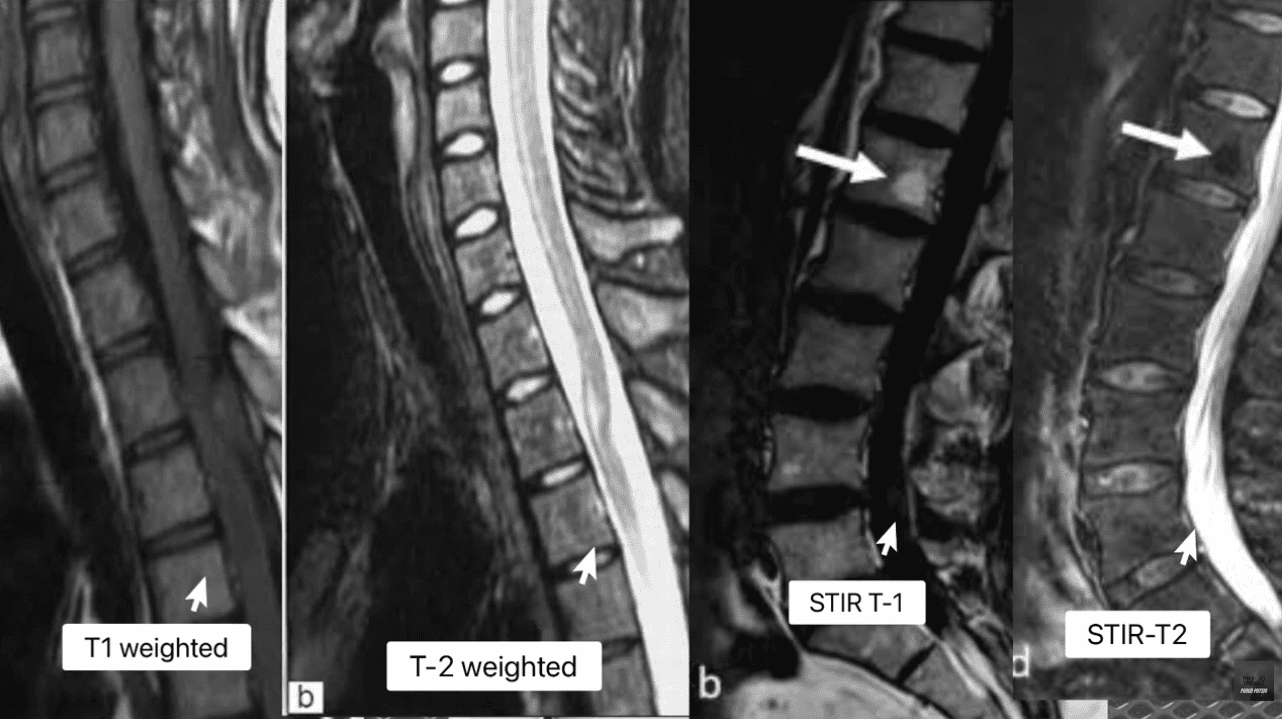
1.2 Decoding the Spinal Pathologies: My Forensic Review of T1, T2, and STIR Sequences
My method for forensic MRI interpretation depends on a nuanced understanding of various pulse sequences and their physiological meaning (Advanced MRI Interpretation, n.d.). I meticulously review the T1-weighted, T2-weighted, and Short Tau Inversion Recovery (STIR) sequences because they tell different stories about the underlying tissue pathology.
| MRI Sequence | Primary Signal (Bright) | Primary Signal (Dark) | Pathological Significance |
| T1-Weighted | Fat (Marrow), Contrast (Gadolinium) | Water (Edema, CSF), Cortical Bone | Anatomy: Excellent for visualizing fatty infiltration (chronic muscle atrophy, Modic 2) and overall anatomical structure. |
| T2-Weighted | Water (Edema, CSF), Degenerated Disc | Fat (Marron), Cortical Bone | Pathology: Crucial for identifying water, making it the primary sequence for acute inflammation, disc herniation (fluid), and spinal cord changes. |
| STIR (Fat-Suppressed) | Water (Edema, CSF, Inflammation) | Fat (Marrow) | Acuity: The definitive sequence for acute trauma. By suppressing fat signal, any remaining bright signal is unequivocally edema, confirming acute inflammation in bone or soft tissue. |
The presence of edema (abnormal fluid accumulation) in the bone marrow or soft tissues surrounding the spine is, in my professional opinion, the most powerful, objective indicator of acute trauma. This edema is the body’s immediate inflammatory response to injury and provides the temporal signature required for my precise injury dating.
1.3 Injury Dating: My Systematic Methodology for Establishing a Timeline of Trauma
The ability to accurately date an injury—to definitively state that a spinal pathology is new or acute, rather than chronic and pre-existing—is, without question, the cornerstone of a successful personal injury claim. My clinic utilizes physiological and biomechanical principles to establish this timeline with forensic precision.
1.3.1 Modic Changes: The Gold Standard for Vertebral Endplate Chronology
Modic changes are alterations in the vertebral body endplates and adjacent bone marrow, visible on MRI, that reflect different stages of pathological response. I rely on them heavily because they provide an objective and scientifically validated marker for estimating the age of an injury (Wang et al., 2017; Spinal Diagnostics, n.d.).
-
Modic Type 1 (MC1) – The Acute Signature: MC1 represents the acute inflammatory stage characterized by bone marrow edema. When I see this, I know I’m looking at an injury that is active and recent.
-
My Staging: I stage this based on the specific signal patterns: Dark on T1 and Bright on T2/STIR (Spinal Diagnostics, n.d.). The persistent bright signal on STIR is the definitive confirmation of active, acute inflammation.
-
My Testimony: I explain to attorneys that MC1 changes typically resolve or transition to the fatty Type 2 changes within approximately 6 to 8 weeks (Spinal Diagnostics, n.d.). Therefore, the presence of MC1 is a powerful, objective sign of recent trauma, often correlating directly with the patient’s reported high pain scores (Jensen et al., 2024). When a defense expert attempts to argue degeneration, my documentation of MC1 provides the irrefutable evidence of a specific, new acute event.
-
-
Modic Type 2 (MC2) – The Chronic Transition: MC2 represents the replacement of normal bone marrow with fatty tissue (Wang et al., 2017). This is a marker of a more subacute or chronic condition.
-
My Staging: I stage this based on the characteristic Bright on T1/T2 but crucially, Dark on STIR (fat-suppressed) sequence (Spinal Diagnostics, n.d.).
-
My Testimony: I use MC2 to show pre-existing degeneration, which ironically, strengthens my credibility. By acknowledging a chronic condition at one level (MC2) while simultaneously proving an acute injury at another (MC1), I demonstrate objectivity and isolate the liability to the new, acute trauma.
-
1.3.2 Wolff’s Law and My Chronological Interpretation of Bone Spurs
Further reinforcing my injury dating is my application of Wolff’s Law, a fundamental biomechanical principle that bone tissue adapts to the loads placed upon it (Spinal Diagnostics, n.d.). Chronic instability leads to the formation of osteophytes (bone spurs) as the body attempts to stabilize the segment through the piezoelectric effect (Spinal Diagnostics, n.d.).
-
The Biomechanical Timeline: I rely on scientific research confirming that it takes approximately six months for a bone spur to become radiographically visible or significant (Spinal Diagnostics, n.d.).
-
My Medico-Legal Implication: When I review a patient’s initial X-rays or CT scans following an MVA, and I find a complete absence of chronic osteophyte formation in the affected segment (e.g., C5-C6), yet the MRI shows an acute disc herniation, I have created an unassailable timeline. The absence of the six-month marker (the bone spur) provides strong supporting evidence that the soft-tissue injury is acute and causally related to the recent collision.
1.4 The Crucial Differential Diagnosis: My Approach to Acute Trauma vs. Chronic Degeneration
Distinguishing new trauma from old, asymptomatic degeneration is essential for proving the extent of damage. I use specific MRI markers to draw this clear line, transforming a murky diagnosis into legal certainty.
1.4.1 Acute-on-Chronic Injury: Quantifying Aggravation
Many accident victims have some degree of pre-existing, asymptomatic degeneration. The defense always targets this reality. My expertise lies in identifying and quantifying the acute-on-chronic injury (Spinal Diagnostics, n.d.).
The tell-tale radiological sign I look for is the clear observation of newly extruded disc material extending beyond the border of a mature, pre-existing osteophyte (Spinal Diagnostics, n.d.). The osteophyte, being a chronic boney change, acts as an anatomical baseline for pre-injury status. Any disc material that has been forcefully extruded beyond this chronic bony landmark is, by definition, new trauma and directly quantifiable aggravation. I personally measure this new extrusion and document its displacement in my reports.
1.4.2 The Vacuum Disc Phenomenon: The Irrefutable Marker of Old Pathology
I use the Vacuum Disc Phenomenon as another definitive marker of a chronic, old condition. This finding—nitrogen gas (a distinct signal void, appearing black) within the center of the disc on all MRI sequences (T1, T2, and STIR)—is a reliable sign of old, irreversible degenerative changes and instability (Spinal Diagnostics, n.d.; Advanced MRI Interpretation, n.d.).
When I find a vacuum disc at one level, I include it in my report. This establishes my objectivity, allowing me to state confidently that while one level is chronic, the adjacent, non-vacuum level that displays Modic 1 changes is acute and causally related to the MVA. This approach prevents the defense from collapsing the entire spine into a single, pre-existing condition.
1.5 Analysis of Complex Non-Disc Spinal Pathologies: The Hidden Injuries
Beyond disc herniation, I specialize in the advanced interpretation of other complex spinal pathologies frequently misunderstood or missed by general practitioners, yet vital for proving injury.
1.5.1 The Spinal Epidural Venous Plexus (Batson’s Plexus): Dural Tenting
The Spinal Epidural Venous Plexus (Batson’s Plexus) is a valveless network highly susceptible to sudden pressure changes (Advanced MRI Interpretation, n.d.). In court, I must distinguish between normal physiological changes and pathological ones.
-
My Differential Diagnosis: Trauma can cause a physiological venous dilation because a disc extrusion can push on the thecal sac—a phenomenon known as dural tenting. This must be carefully distinguished from a pathological Epidural Varix (a symptomatic dilation that causes neural compression) (Advanced MRI Interpretation, n.d.). I rely on sequences like contrast-enhanced MRI (when medically necessary) and non-contrast flow-sensitive sequences to confirm the difference. Incorrectly diagnosing normal venous dilation as a compressive pathology can undermine an entire claim, and my careful distinction preserves my credibility.
1.5.2 Post-Traumatic Muscle Changes: Fatty Infiltration of the Multifidus
The deep lumbar muscles, particularly the multifidus, are essential stabilizers. I have seen time and again how pain-induced inhibition leads to rapid structural changes in this muscle.
-
My Injury Dating and Causality: This muscle transformation begins to appear on imaging as early as 2 to 12 weeks post-injury (Spinal Diagnostics, n.d.; Central Ohio Spine and Joint, n.d.). Fatty infiltration (visible as a bright signal on T1-weighted images) is highly associated with chronic pain and instability. The degree of infiltration is a crucial prognostic indicator, correlating negatively with functional improvement (Xu et al., 2024). The presence and severity of multifidus fatty infiltration provide powerful objective evidence of chronic functional impairment and instability directly resulting from the traumatic event. I use this finding to prove permanent injury to the core stabilizing system, which is critical for future medical damages.
2.0 Establishing Causality: My Biomechanical and Legal Framework
The defense is designed to argue that a plaintiff’s pain is due to aging or unrelated issues. My documentation provides the scientific and legal rebuttals necessary to establish clear causation—a process I personally manage from the moment the patient walks through my door.
2.1 The “Eggshell Plaintiff” Doctrine: My Documentation Strategy
A foundational principle in personal injury law is the “Eggshell Plaintiff” Rule: a defendant must take the victim as they find them (Cornell Law School, n.d.). This means the defendant is fully liable for the plaintiff’s injuries, even if those injuries are more severe than they would have been in an average person due to an existing, pre-disposed condition (Rafi Law Firm, n.d.).
-
My Personal Role: Successfully applying this doctrine in court requires meticulous documentation, which I provide by:
-
Defining the Baseline: Precisely evaluating the pre-accident state (using the Vacuum Disc, Modic 2/3, and chronic osteophyte timelines). I acknowledge the pre-existing state without minimizing the new trauma.
-
Quantifying the Acute Change: Using Modic Type 1 and Acute-on-Chronic findings to objectively demonstrate the new, causally related injury (Spinal Diagnostics, n.d.).
-
Proving Exacerbation: Establishing that the traumatic event (MVA) directly aggravated the pre-existing condition, resulting in new symptoms, functional loss, and permanent impairment. My reports meticulously connect the mechanism of injury to the exacerbation, ensuring the court grasps the full scope of liability.
-
2.2 The Biomechanical Signatures of Soft Tissue and Ligamentous Injury (Whiplash)
Soft tissue injuries, or whiplash-associated disorders (WAD), are commonly challenged as subjective. My examination protocol goes beyond standard range of motion checks to confirm structural injury.
-
Occult Ligamentous Injury: I utilize the MRI’s fluid-sensitive sequences (STIR) to search for occult tears and sprains. I look for the hyperintense (bright) signal in the interspinous and supraspinous ligaments (Spinal Diagnostics, n.d.), which represents edema and tearing. This finding transforms a subjective “sprain/strain” into an objective, structural instability.
-
Facet Capsular Edema: The facet joints are often injured during MVA hyperflexion/hyperextension. I meticulously look for capsular edema or effusion (bright signal around the joint) on T2/STIR images. This is a highly specific finding for acute trauma to the joint capsule, which often correlates to localized, severe pain.
-
The Biomechanical Correlation: I thoroughly document the mechanism of injury (e.g., rear-end collision, specific speed data if available) and link the vector of force to the specific pathology found (e.g., a rear-end vector causing anterior compression and posterior ligamentous tearing) (NCBI, 2023). This correlation is crucial in court to overcome defense arguments that the forces were insufficient to cause the documented injury.
3.0 The Dual-Licensed Advantage: My DC & APRN/FNP-BC Model in El Paso
The most compelling aspect of the Injury Medical Clinic PA model, and the primary reason for my success in the medico-legal field, is my unique qualification as a dual-licensed professional. The integration of the Doctor of Chiropractic (DC) and the Advanced Practice Registered Nurse/Family Nurse Practitioner (APRN/FNP-BC) licenses creates a holistic, comprehensive, and legally powerful care model that is unmatched in the El Paso area.
3.1 Comprehensive Care Models: My Integrated Approach
I bring together the best of both worlds, creating a single source of expertise that satisfies both the clinical and legal standards of care:
-
My Role as a Chiropractic Physician (DC): I provide unparalleled expertise in spinal biomechanics, functional assessment, manual therapy, and the non-surgical management of complex musculoskeletal injuries. The DC perspective is critical for evaluating the long-term functional impairment caused by disc, facet, and ligament pathology.
-
My Role as a Nurse Practitioner (APRN/FNP-BC): I provide the essential medical framework, including the ability to prescribe medication (e.g., muscle relaxants, neuropathic agents), order and manage advanced diagnostic testing (e.g., specific, medically-prescribed MRI protocols, nerve conduction studies), manage co-morbidities, and, most crucially, write comprehensive, authoritative medical-legal reports and provide expert testimony that carries the weight of a board-certified medical professional, satisfying the standard medical scrutiny of the court.
This integration ensures the patient receives optimal physical rehabilitation alongside rigorous medical documentation, all under one practice. My reports are medical documents authored by an APRN/FNP-BC, while the therapeutic details reflect the specialized biomechanical insight of a DC. This synergy is invaluable to attorneys.
3.2 Justification for Dual-Licensed Intervention: Case Archetypes in My Practice
I manage these three case archetypes every day, and they demonstrate why my dual-licensed approach is often medically and legally necessary:
| Case Archetype | Clinical Presentation in My Clinic | My Dual-Licensed Treatment Rationale | Medico-Legal Value in My Reports |
| Type 1: Complex Cervical WAD with Radiculopathy. | Patient presents with neck pain, headaches, and confirmed numbness/tingling in the arm. MRI shows a C5-C6 disc bulge impinging on the nerve root. | My DC Expertise: Focus on specific spinal mobilization to reduce segmental dysfunction and restore cervical curve stability. My APRN Expertise: Prescribe gabapentin or NSAIDs for nerve pain, order Electromyography/Nerve Conduction Velocity (EMG/NCV) studies, and administer facet or trigger point injections if necessary (Mayo Clinic, 2024). | Causality: The combined finding of clinical radiculopathy (confirmed by NCV—a medical test I ordered) and the biomechanical trauma (my DC diagnosis) is documented under a single, authoritative medical record (my APRN report). I can objectively testify to the severity of the neurological deficit. |
| Type 2: Acute Lumbar Disc Extrusion with Failed Conservative Care. | Patient suffers acute L5-S1 disc extrusion causing severe, debilitating sciatica that is not responding to basic care. | My DC Expertise: Implement specialized non-surgical spinal decompression protocols and advanced core stabilization exercises. My APRN Expertise: Medically evaluate the patient’s pain using objective outcome measures (Oswestry Disability Index), rule out Red Flags (Cauda Equina), manage opioid/non-opioid medication, and critically, document the failure of conservative care, which justifies the trajectory toward advanced interventions or surgical consultation. | Damages & Prognosis: My comprehensive documentation of conservative care failure establishes the persistent, debilitating nature of the injury. This robust history is essential for the attorney to justify the valuation of both past and high-value future medical costs in front of a jury. |
| Type 3: Acute-on-Chronic Spinal Instability. | Patient has pre-existing, asymptomatic spinal stenosis (Modic Type 2 changes), but the MVA results in new symptoms and a new Modic Type 1 change at the adjacent level. | My DC Expertise: Focus on restoring segmental stability to the traumatized level while protecting the degenerated level. My APRN Expertise: Personally interpret the complex MRI (Modic 1 vs. Modic 2) to clearly delineate the acute injury (liability) from the pre-existing condition (eggshell) (Spinal Diagnostics, n.d.). | Defeating the Defense: My precise diagnostic report legally isolates the acute trauma (Modic 1) from the chronic degeneration (Modic 2/Vacuum Disc), providing the attorney with clear, objective evidence to apply the Eggshell Plaintiff doctrine and secure recovery for the aggravation and new injury. |
4.0 My Credible Expert Witness Testimony: Illuminating Disability and Driving Monetary Recoveries
My ultimate function for the legal community is to serve as the credible, objective voice that clarifies the patient’s impairment for the jury. My testimony is built upon the synthesis of advanced clinical diagnostics and established medico-legal principles that I personally adhere to.
4.1 The Credibility Foundation: My Daubert-Compliant Testimony
Attorneys frequently utilize my expertise because my methodology is rooted in the scientific method, ensuring my opinions are admissible under the Daubert Standard. My expert testimony is not merely anecdotal; it is a direct presentation of verifiable scientific data:
-
Measurable Markers: When I testify, I don’t just state an opinion. I point to the imaging and explain that the Modic Type 1 change is not random, but an established scientific finding with a specific 6-8 week timeline, proving the freshness of the bone trauma (Wang et al., 2017). I use analogies, like comparing the Modic 1 change to a fresh bruise on the bone, which makes the complex science undeniable to a layperson jury.
-
Biomechanically Sound Conclusions: I personally explain how the physics of the impact (the vector, the forces) translates into the specific, demonstrable injury, such as the mechanism by which a sudden flexion-extension event causes an annular tear (Paredes et al., 2023). This link between physics and physiology is critical for proving causation.
-
The Power of the Dual Role: When I stand before the court, my opinion integrates the highest standard of musculoskeletal diagnosis (DC) with the authority of advanced medical management (APRN). I am uniquely positioned to counter both the defense’s biomechanics expert and their medical expert.
4.2 My Method for Translating Pathology into Permanent Impairment and Disability
The value of a personal injury case is directly linked to the demonstrability and permanency of the injury. My detailed reports translate abstract medical findings into tangible, compelling evidence of long-term disability for the jury.
4.2.1 Quantifying Functional Loss: From Imaging to Activities of Daily Living (ADLs)
I shift the focus from what the injury looks like on an MRI to how it permanently impairs the patient’s life:
-
Multifidus Fatty Infiltration: I explain to the jury that the increased bright signal on the patient’s T1 MRI is not simply “fat,” but the objective, measurable sign of a permanent loss of spinal stability (Central Ohio Spine and Joint, n.d.). I elaborate that the muscle is no longer functional, leading to chronic instability, increased risk of re-injury, and an inability to perform basic ADLs like prolonged sitting, standing, or lifting—directly correlating to a lower quality of life and permanent functional loss.
-
Irreversible Cord Damage (Myelomalacia): If I identify Myelomalacia (softening, necrosis, and scarring of the spinal cord tissue) on a T2 image (hyperintensity within the cord), I use this to establish a definitive, catastrophic, permanent neurological injury (Spinal Diagnostics, n.d.). This finding is irreversible and dictates a life of permanent neurological deficits, which is irrefutable evidence of severe disability that warrants significant monetary recovery.
4.2.2 Linking Causality to Prognosis and Future Medical Costs
My reports connect the initial traumatic event to the long-term cost of care. This is vital for the attorney’s calculation of future medical damages.
-
Permanent Impairment Rating (PIR): I use objective prognostic indicators—such as the severity of multifidus infiltration (Xu et al., 2024), the persistence of Modic 1 changes, or the presence of irreversible ligament instability—to generate a scientifically grounded Permanent Impairment Rating (PIR) using the AMA Guides to the Evaluation of Permanent Impairment.
-
Future Medical Requirements: The report then outlines the need for future care (e.g., ongoing chiropractic maintenance, periodic APRN follow-ups, medication management, or potential injections/surgical consultations) directly necessitated by the MVA. This robust justification of future needs is critical for maximizing the final settlement or jury award.
By establishing causation, chronicity, and prognosis through my rigorous, peer-reviewed methodology, I provide the unassailable evidence necessary to maximize the plaintiff’s recovery and to position legal counsel to confidently present even the most complex clinical cases before a jury. My role is to ensure that the injury is not only treated effectively but also documented exhaustively, establishing Injury Medical Clinic PA as the premier clinic for injuries resulting from accidents in the El Paso area.
References and Diagnostic Sources
-
Alexander Orthopaedics. (2024). Common Neck Injuries After a Car Accident. https://alexanderorthopaedics.com/blog/common-neck-injuries-from-a-car-accident/
-
Central Ohio Spine and Joint (CO Spine & Joint). (n.d.). MRI Confirmation of Fatty Infiltrate in the Lumbar Multifidi: What It Means for Chronic Low Back Pain. https://cospineandjoint.com/fatty-infiltration-lumbar-multifidi-low-back-pain/
-
Cornell Law School. (n.d.). Eggshell skull rule. Legal Information Institute. https://www.law.cornell.edu/wex/eggshell_skull_rule
-
Jensen, H. M., et al. (2024). What does a Type 1 Modic change on MRI mean for chronic back pain? Eureka Health. https://www.eurekahealth.com/resources/modic-changes-type-1-mri-chronic-back-pain-en
-
Mayo Clinic. (2024). Whiplash – Diagnosis and treatment. https://www.mayoclinic.org/diseases-conditions/whiplash/diagnosis-treatment/drc-20378926
-
National Institutes of Health (NIH). (2022). Updated Review of the Evidence Supporting the Medical and Legal Use of NeuroQuant® and NeuroGage® in Patients With Traumatic Brain Injury. PMC – PubMed Central. https://pmc.ncbi.nlm.nih.gov/articles/PMC9027332/
-
National Center for Biotechnology Information (NCBI). (2023). Neck Trauma – StatPearls. NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK470422/
-
Paredes, K., et al. (2023). Annular Disc Tear – StatPearls. NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK459235/
-
Rafi Law Firm. (n.d.). The Egg-Shell Plaintiff Doctrine: What is it? And how might it affect your case? https://www.rafilawfirm.com/learn/the-egg-shell-plaintiff-doctrine-what-is-it-and-how-might-it-affect-your-case/
-
Wang, Y., et al. (2017). Pathobiology of Modic changes. PMC – PubMed Central. https://pmc.ncbi.nlm.nih.gov/articles/PMC5477843/
-
Xu, S., et al. (2024). Multifidus fat infiltration negatively influences postoperative outcomes in lumbar disc herniation following percutaneous endoscopic lumbar discectomy via the transforaminal approach. PubMed Central. https://pmc.ncbi.nlm.nih.gov/articles/PMC11756129/

Sports and Activities for TBI Recovery Success
Sports and Activities for TBI Recovery: The Role of Nurse Practitioners and Integrative Chiropractic Care

aquatic rehabilitation class for various injuries, including traumatic brain injuries
Traumatic brain injuries, or TBIs, happen when a sudden bump or blow to the head damages the brain. These injuries can come from car crashes, falls, or even sports accidents. Recovering from a TBI takes time and involves many steps to get back strength, balance, and clear thinking. One great way to help is through sports and activities tailored to a person’s needs. These are called adaptive sports. They can boost physical health and also lift moods by making people feel connected and strong. Along with that, healthcare experts like nurse practitioners and chiropractors play big parts in guiding recovery. Nurse practitioners help manage overall health and meds, while chiropractors focus on fixing spine issues and easing pain. This team approach, often called integrative care, mixes different treatments for better results.
In this article, we’ll look at sports that support TBI recovery, such as adaptive basketball and swimming. We’ll also cover calming activities such as tai chi and hiking. Then, we’ll explain how nurse practitioners and chiropractors fit into the picture, drawing on expert perspectives such as Dr. Alexander Jimenez, who combines chiropractic and nursing skills. By the end, you’ll see how these elements work together to create a comprehensive recovery plan.
Understanding TBIs and the Need for Active Recovery
A TBI can mess with how you move, think, and feel. Mild ones, like concussions, might cause headaches or dizziness. Severe ones can lead to long-term problems with balance or memory. The brain has a cool ability called neuroplasticity, which means it can rewire itself to heal. Activities that get you moving help spark this process by building new connections in the brain.
Doctors say rest is key right after a TBI, but then it’s time to add gentle exercise. Starting slow prevents more harm and builds up skills step by step. For example, light walking can improve blood flow to the brain, helping it heal faster. As you get better, more fun activities like games or outdoor adventures can keep things exciting and motivating.
- Why activities matter: They improve strength, coordination, and mood.
- Start small: Begin with easy tasks at home, like puzzles or stretching.
- Build up: Move to group activities for social support.
Research shows that staying active after a TBI lowers the risk of depression and helps people get back to daily life sooner.
Adaptive Sports for Physical and Mental Healing
Adaptive sports are regular sports modified with special tools or rules so everyone can join, regardless of their limitations. For TBI survivors, these sports target balance, hand-eye skills, and thinking on your feet. They also build confidence by letting you achieve goals in a safe way.
Many groups offer adaptive sports programs, making it easy to find local options. Here’s a look at some top ones for TBI recovery:
- Adaptive Basketball: Played in wheelchairs or with lower hoops, this sport boosts coordination and teamwork. It helps with quick decisions and arm strength, which TBIs often weaken. Groups like the National Wheelchair Basketball Association run events where players connect and stay motivated.
- Cycling: Use adaptive bikes with extra wheels for stability. Cycling improves leg strength and heart health while being low-impact on joints. It’s great for building endurance without straining the brain too much.
- Swimming: Water supports your body, making movements easier. Adaptive swimming uses floats or lanes for safety. It enhances balance and breathing control, plus the calm water reduces stress.
- Canoeing: In adaptive versions, boats have seats or handles for support. Paddling builds upper body strength and focus. Being on water also calms the mind, helping with anxiety from TBIs.
These sports aren’t just exercise—they create social bonds. Playing with others fights loneliness, a common issue after brain injuries. Studies note that adaptive sports like these keep people active and linked to their communities. One review found that they improve gait and balance in patients with brain injury.
Other Rehabilitative Activities to Enhance Balance and Well-Being
Not all recovery needs to be high-energy. Slower activities like tai chi or hiking can rebuild skills without overwhelming the brain. These focus on mindful movement, which also supports mental health.
- Tai Chi: This gentle martial art uses slow, flowing movements to improve balance and focus. For TBI patients, it reduces falls by strengthening core muscles. Classes often adapt poses for sitting if standing is difficult.
- Hiking: Adaptive hiking uses trails with smooth paths or walking sticks. It increases heart rate and provides a refreshing change of scenery. Nature-based activities like this restore energy both physically and emotionally.
- Adaptive Water Sports: Beyond swimming, try kayaking or water aerobics. These use buoyancy to reduce pressure on the body while improving coordination. Special gear, like life vests, ensures safety.
Home activities can start the process. Activities like balloon tosses or chair yoga build hand-eye coordination and flexibility. Online videos make it easy to try. As skills grow, add group classes for more challenge. Experts say even simple mobilizing, like walking circuits, aids recovery.
Special tools might be needed based on your strengths. For example, use bigger balls in games or stabilizers in cycling. Always check with a doctor to match activities to your healing stage.
The Role of Nurse Practitioners in Coordinating TBI Care
Nurse practitioners (NPs) are advanced nurses who can diagnose, treat, and manage health issues. In TBI recovery, they act as coordinators, making sure all parts of care fit together smoothly.
NPs monitor your overall health during activities. They check for signs like fatigue or headaches that might mean you’re pushing too hard. They also manage meds for pain or mood, adjusting doses as you improve. For instance, if swimming causes dizziness, an NP might suggest changes or add rest days.
In integrative teams, NPs work with other experts to create safe plans. They ensure activities like canoeing don’t clash with your meds or other treatments. Their focus on whole-person care includes emotional support to help with stress during recovery.
Dr. Alexander Jimenez, a chiropractor and family nurse practitioner, notes that NPs play a key role in linking brain health to daily wellness. His observations show they help with sleep and nutrition, which in turn boost activity benefits. This approach ensures activities are effective and safe.
Integrative Chiropractic Care: Supporting Spine and Pain Management
Chiropractors specialize in spine health, which is crucial after a TBI since head injuries often affect the neck. Integrative chiropractic combines adjustments with other therapies, such as exercises, for full recovery.
Chiropractors realign the spine to ease pressure on nerves, reducing headaches and improving balance. For TBI patients, this can help with dizziness from vestibular issues. They also manage pain without heavy meds, using hands-on techniques.
In recovery plans, chiropractors include exercises such as postural training and balance drills. These complement sports by building a strong base. For example, after an adaptive basketball session, a session might address any spine shifts from play.
Dr. Jimenez’s clinical work highlights how chiropractic aids brain healing. He uses gentle adjustments to improve blood flow and nerve function, key for TBIs. His teams integrate this with nutrition and rehab activities, such as light walking, to prevent reinjury. One method he supports is vestibular rehab, which pairs well with sports for better coordination.
- Benefits of integrative chiropractic:
- Reduces inflammation and pain.
- Improves mobility for activities.
- Prevents future issues through education.
Combining chiropractic with NP care creates a strong support system. NPs handle meds and monitoring, while chiropractors focus on physical fixes.
Combining Sports, Activities, and Professional Care for Best Results
The best TBI recovery programs combine adaptive sports, calming activities, and expert guidance. Start with a plan from your healthcare team. For example, begin with tai chi for balance, then add cycling as strength grows.
Community outings, like group hikes, apply skills in real life. These build confidence and social ties. Equine therapy, like therapeutic riding, is another option—horses’ movements aid gait and emotional health.
Dr. Jimenez observes that nutrition supports this, like anti-inflammatory foods for brain repair. His work shows that stress management is key, as it affects outcomes.
Track progress with tools like journals or apps. Adjust as needed with your NP or chiropractor. Over time, this leads to independence and joy in activities.
Challenges and Tips for Success
Recovery isn’t always smooth. Fatigue or setbacks can happen. Tips include:
- Listen to your body—rest when needed.
- Use adaptive gear for safety.
- Join support groups for motivation.
With patience, most people see big gains. Studies show stepwise returns to activity, like in sports protocols, work well.
Conclusion
Recovering from a TBI through sports like adaptive basketball or activities like hiking builds both the body and the mind. Nurse practitioners coordinate safe care, while integrative chiropractic handles pain and alignment. Experts like Dr. Jimenez show how this blend speeds healing. Stay active, seek help, and celebrate small wins to pave the way for a brighter path ahead.
References
- Brain Injury Center. (n.d.). Fun Fitness Routines for Brain Injury Survivors. https://www.braininjurycenter.org/blog/?article=223
- Krysalis Consultancy. (n.d.). Over 200 Home Activities for Brain Injury Survivors. https://www.krysalisconsultancy.co.uk/resources/item/over-200-home-activities-for-brain-injury-survivors
- Powell, J. H. (2012). Traumatic Brain Injury in Sports: A Review. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC3400421/
- Illinois CMS. (n.d.). Traumatic Brain Injury Recovery. https://cms.illinois.gov/benefits/stateemployee/bewell/getmoving/traumatic-brain-injury-recovery.html
- Groth, S. (n.d.). Horses as Healers. Refubium. https://refubium.fu-berlin.de/bitstream/handle/fub188/31010/Horses%20as%20Healers%2C%20Svenja%20Groth%20-%20Refubium.pdf?sequence=1&isAllowed=y
- Essential Chirocare. (n.d.). Benefits of Physical Therapy for a TBI. https://www.essentialchirocare.com/regaining-your-function-reducing-pain-and-more-the-benefits-of-physical-therapy-for-a-tbi
- Encompass Health. (n.d.). Community Outings for Individuals with Brain Injuries. https://www.encompasshealth.com/health-resources/articles/community-outings-for-individuals-with-brain-injuries
- Atlas Wellness. (n.d.). Natural Recovery from Concussion and TBI. https://atlaswellness.com/natural-recovery-from-concussion-and-tbi/
- My Balance Matters. (n.d.). Chiropractic Care for Concussions. https://www.mybalancematters.com.au/articles/chiropractic-care-for-concussions-a-holistic-approach-to-recovery-and-rehabilitation
- Jimenez, A. (n.d.). Dr. Alex Jimenez’s Website. https://dralexjimenez.com/
- Flint Rehab. (n.d.). Activities for Brain Injury Patients. https://www.flintrehab.com/activities-for-brain-injury-patients/
- Jimenez, A. (n.d.). LinkedIn Profile. https://www.linkedin.com/in/dralexjimenez/

Tests Used for Brain Injuries in Chiropractic Care
Tests Used for Brain Injuries at El Paso Back Clinic® in El Paso, TX

Doctor of Chiropractic and Nurse Practitioner show the imaging result to the patient post-auto-injury rehabilitation with mild brain injury
Brain injuries can strike without warning, from a simple slip at home to a tough hit during sports or a car crash on El Paso’s busy roads. At El Paso Back Clinic® in El Paso, TX, our team of wellness chiropractic care experts knows how vital it is to spot these issues early. We blend chiropractic skills with modern tools to help patients heal and get back to life. Led by Dr. Alexander Jimenez, DC, APRN, FNP-BC, our clinic focuses on whole-body wellness, using safe, non-invasive methods to check for head injuries.
This article dives into the tests we use at El Paso Back Clinic® to find brain injuries. We cover hands-on checks, brain function tests, and high-tech scans. Our goal is to give you clear info so you can seek help fast. Early detection means better recovery and fewer long-term problems.
The Importance of Spotting Brain Injuries Early at Our Clinic
Traumatic brain injuries (TBIs) happen when a bump or jolt shakes the brain. Mild ones, like concussions, might cause short-term headaches or dizziness. Serious cases can lead to lasting memory issues or mood changes. At El Paso Back Clinic®, we see many patients from local accidents or sports-related injuries, and we emphasize prompt action.
Our integrative approach mixes chiropractic care with nurse practitioner expertise. Dr. Jimenez uses his dual training to create custom plans. We check the spine, nerves, and brain together because a head injury often affects the neck as well.
- Common signs: Headaches, confusion, nausea, or trouble balancing.
- Why act fast: Stops swelling or bleeding from getting worse.
- Our edge: Our wellness focus means we look at lifestyle and nutrition, too.
Research backs our methods—early tests lead to stronger outcomes (Pickett et al., 2024). At our El Paso, TX clinic, we guide you through every step.
Starting with Neurological Assessments for Head Injuries
At El Paso Back Clinic®, every brain injury check begins with basic neurological tests. These quick exams help us see how the brain responds right away. No need for big machines; it’s all about skilled observation.
We rely on the Glasgow Coma Scale (GCS) to grade injury severity. The Glasgow Coma Scale (GCS), which scores from 3 to 15, assesses eye opening, verbal response, and motor response. High scores mean mild issues; low ones signal urgency. Our team, including Dr. Jimenez, uses GCS to quickly decide on next steps (Bussières et al., 2022).
We also use the Standardized Assessment of Concussion (SAC). This tests memory and focus with simple questions. For athletes, the Sport Concussion Assessment Tool 5 (SCAT5) adds balance and neck checks. Kids receive the Child SCAT5 version.
- GCS breakdown:
- Eyes: 1 (none) to 4 (spontaneous).
- Verbal: 1 (silent) to 5 (oriented).
- Motor: 1 (none) to 6 (obeys commands).
- SAC quick tips: Asks things like “What month is it?” or repeats word lists.
- SCAT5 extras: Includes symptom checklists and coordination drills.
Dr. Jimenez notes that these tests often reveal neck problems linked to head injuries. At our wellness clinic, we adjust spines to ease related pain.
Hands-On Physical Exams to Uncover Hidden Issues
Physical checks are key at El Paso Back Clinic®. We touch and move areas to find pain, weakness, or limits. This builds on your story about how the injury happened.
Reflex tests tap spots, like the knees, to check nerve pathways. Odd responses might point to brain trouble. The Balance Error Scoring System (BESS) tests stability—stand in poses and count errors. It’s useful for detecting dizziness associated with TBIs (Sillevis et al., 2018).
We measure how far you can move your neck or head without pain. Strength tests have you push against our hands. These help link head injuries to spine misalignments.
- BESS poses:
- These include the double-leg stance, single-leg stance, and tandem pose.
- Perform the exercises on both firm ground and foam to increase the challenge.
- The errors to avoid include having hands off the hips, keeping eyes open, and falling.
- Reflex checks: Hammer taps for quick reactions.
- Motion tests: Gentle turns to spot restrictions.
For El Paso locals in car wrecks, these exams guide our chiropractic adjustments. Dr. Jimenez observes that early physical checks prevent chronic issues.
Cognitive Testing to Measure Brain Function
Head injuries can fog thinking. At El Paso Back Clinic®, we use cognitive tests such as ImPACT to assess memory and reaction time. This computer-based tool is perfect for concussion assessment, as it allows you to compare your scores to norms or baselines.
ImPACT includes modules for word recall, symbol matching, and symptom rating. It’s objective and tracks progress over time. We use it for return-to-work or play decisions (ImPACT Applications, Inc., 2023a).
Our nurse practitioners add deeper checks if needed, like repeating stories or drawing shapes. These rule out other causes.
- ImPACT features:
- Visual memory: Recall designs.
- Reaction time: Click on the colors fast.
- Symptom scale: Rate 22 items like fatigue.
- Baseline testing: Ideal for athletes before seasons.
- Retesting: Every 7-10 days to monitor healing.
Dr. Jimenez integrates ImPACT with chiropractic care, noting better results when spine health supports brain recovery.
Advanced Imaging for Clear Views of Injuries
Imaging lets us see inside. At El Paso Back Clinic®, we start with X-rays for bone alignment and fractures. They’re fast and help plan adjustments.
For deeper looks, CT scans catch bleeds quickly. MRIs show soft-tissue damage, such as bruising or tears—no radiation involved. We order these through our network for full pictures (NYU Langone Health, n.d.).
Digital Motion X-ray (DMX) is a favorite here—it films spine movement to spot instability from whiplash.
- X-ray basics: Views bones in still shots.
- CT strengths: 3D slices for emergencies.
- MRI details: Magnets reveal hidden swelling.
- DMX unique: Real-time video of neck motion.
Dr. Jimenez uses imaging to confirm diagnoses, ensuring safe, targeted care at our El Paso wellness clinic.
Non-Invasive Tools Enhancing Our Chiropractic Approach
We love tools that avoid invasives at El Paso Back Clinic®. Surface Electromyography (sEMG) measures muscle activity via skin sensors. It identifies imbalances related to nerve issues post-head injury (Injury 2 Wellness Centers, 2023a).
Our INSiGHT scanners combine scans: Thermal for inflammation, Core for posture, Pulse for stress via heart rate. These insights help us create personalized plan maps (CLA Insights, 2023a).
- sEMG benefits:
- Detects tense muscles around the neck.
- Guides gentle adjustments.
- INSiGHT scans:
- Heat patterns show hot spots.
- Muscle scans check symmetry.
- No risks: This procedure is safe for individuals of all ages.
These tools reduce the need for pokes or cuts, aligning with our wellness focus (Injury 2 Wellness Centers, 2023b). Dr. Jimenez says they boost patient involvement.
Nurse Practitioners’ Role in Comprehensive Testing
Our nurse practitioners at El Paso Back Clinic® expand options. They order blood tests for markers like inflammation or clotting risks. This rules out serious issues.
They incorporate a comprehensive approach by integrating chiropractic care into their holistic plans. If scans show problems, they coordinate referrals.
- Blood work perks:
- Checks for hidden infections.
- Monitors healing proteins.
- Team integration: NPs and chiros share findings.
- Patient plans: Include rest, nutrition, and adjustments.
Dr. Jimenez, with his NP background, ensures seamless care.
Chiropractic Perspectives on Brain Injury Diagnosis
Chiropractors at our clinic see the spine-brain connection. Head hits often shift vertebrae, worsening symptoms. We use tools like Sigma for motion analysis (Kawa, n.d.).
Vestibular tests check eyes and balance. Does the patient experience pain during head movements? The source of the pain could be either the inner ear or the brain.
- Spine focus:
- Palpate for misalignments.
- Grade Whiplash: 0-4.
- Red flags: Send to ER for severe signs.
- Recovery steps: Adjustments plus exercises.
Dr. Jimenez’s observations show that chiropractic care eases concussion symptoms more quickly.
Collaborative Care for Optimal Recovery
At El Paso Back Clinic®, teamwork rules. NPs order MRIs; chiros use them for adjustments. Shared tests like SCAT5 build complete views.
Plans cover therapy, diet, and follow-ups. Patients return stronger.
- Benefits:
- Full body healing.
- Cost-effective.
- Customized to you.
- Success stories: Less pain, better function.
Dr. Jimenez’s integrative style shines in El Paso cases.
Insights from Daily Practice at the Clinic
We adapt tests to each patient. A work injury requires X-rays and ImPACT. Follow with BESS for balance gains.
Dr. Jimenez shares how INSiGHT scans catch early nerve stress, preventing long-term woes.
Patients love visual reports—they understand and stick to plans.
Overcoming Challenges in Brain Injury Detection
Access and cost can hinder. But our clinic offers affordable options and education.
Future tools, such as blood biomarkers, promise quicker diagnoses. We stay up to date for the best care.
- Hurdles:
- Rural limits in TX.
- Insurance gaps.
- Advances: AI for scan reads, more non-invasives.
Dr. Jimenez pushes for community awareness.
Final Thoughts: Seek Care at El Paso Back Clinic®
Brain injuries need prompt attention. At El Paso Back Clinic® in El Paso, TX, we use GCS, ImPACT, scans, and more for wellness-focused recovery.
If you’ve had a head hit, visit us. Our team, led by Dr. Jimenez, is here for you.
References
Bussières, A., et al. (2022). Concussion knowledge among North American chiropractors. Journal of the Canadian Chiropractic Association, 66(1), 17–26. https://pmc.ncbi.nlm.nih.gov/articles/PMC8791549/
California State Board of Chiropractic Examiners. (n.d.). Chiropractic consumer guide. https://www.chiro.ca.gov/publications/chiro_consumer_guide.pdf
CLA Insights. (2023a). The role of neurological scanning tech in modern chiropractic care. https://insightcla.com/blog/the-role-of-neurological-scanning-tech-in-modern-chiropractic-care/
CLA Insights. (2023b). The future of non-invasive diagnostics in chiropractic practices. https://insightcla.com/blog/the-future-of-non-invasive-diagnostics-in-chiropractic-practices/
CLA Insights. (2023c). Neurological scanning technology for chiropractic diagnosis. https://insightcla.com/blog/neurological-scanning-technology-for-chiropractic-diagnosis/
Comfort Rehab & Chiropractic Center. (n.d.). Chiropractic diagnostics for auto-accident injuries. https://dallasaccidentandinjuryrehab.com/chiropractic-diagnostics-for-auto-accident-injuries-comprehensive-guide-to-chiropractic-diagnostics-for-auto-accident-injury-recovery-2/
ImPACT Applications, Inc. (2023a). Chiropractor’s role in concussion management. https://impacttest.com/chiropractors-role-in-concussion-management/
ImPACT Applications, Inc. (2023b). Chiropractors role in concussion management [PDF]. https://impacttest.com/wp-content/uploads/chiropractors-role-in-concussion-management.pdf
Injury 2 Wellness Centers. (2023a). Innovative injury assessment techniques in modern chiropractic care. https://injury2wellness.com/innovative-injury-assessment-techniques-in-modern-chiropractic-care/
Injury 2 Wellness Centers. (2023b). Revolutionizing injury diagnosis: Advanced chiropractic tools explained. https://injury2wellness.com/revolutionizing-injury-diagnosis-advanced-chiropractic-tools-explained/
Injury 2 Wellness Centers. (2023c). Transforming chiropractic care: The role of X-rays in injury diagnosis. https://injury2wellness.com/transforming-chiropractic-care-the-role-of-x-rays-in-injury-diagnosis/
Jimenez, A. (n.d.). Injury Specialists. https://dralexjimenez.com/
Jimenez, A. (n.d.). LinkedIn profile. https://www.linkedin.com/in/dralexjimenez/
Kal, D. (n.d.). Chiropractic relief for accident head injuries. https://drkal.com/chiropractic-relief-for-accident-head-injuries/
Kawa, C. (n.d.). Diagnostic tools. https://chiropractorbricknj.com/diagnostic-tools/
Modern Chiropractic Center. (n.d.). Accurate post-car crash injury diagnosis. https://modernchiropracticcenter.com/blog/accurate-post-car-crash-injury-diagnosis/
NYU Langone Health. (n.d.). Diagnosing concussion. https://nyulangone.org/conditions/concussion/diagnosis
Pickett, W., et al. (2024). Expanding concussion care in Canada: The role of chiropractors and policy implications. Journal of the Canadian Chiropractic Association, 68(2), 145–156. https://pmc.ncbi.nlm.nih.gov/articles/PMC11418793/
Sillevis, R., et al. (2018). Survey of chiropractic clinicians on self-reported knowledge and recognition of concussion injuries. Journal of the Canadian Chiropractic Association, 62(2), 84–95. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6000952/
Spine and Injury Center. (n.d.). How do chiropractors diagnose injuries. https://www.flspineandinjury.com/blog/how-do-chiropractors-diagnose-injuries
World Health Organization. (n.d.). Diagnostics. https://www.who.int/health-topics/diagnostics

Posture Recovery Exercises After TBI: A Guide
Gentle Recovery Strategies After Traumatic Brain Injury: Exercises, Chiropractic Care, and Holistic Support for Lasting Healing

Electromagnetic therapy of the back: a physiotherapist doctor works with a patient with a traumatic brain injury from an occupational accident.
Traumatic brain injury (TBI) affects millions of people every year. A sudden blow or jolt to the head can cause headaches, dizziness, memory problems, neck pain, and poor balance. While the brain needs time and rest to heal, the body also needs gentle movement to recover fully. Early, safe exercises for the neck, core, and balance can speed healing, reduce pain, and lower the risk of falls. Integrative chiropractic care helps restore nerve signals and alignment. Nurse practitioners guide the whole recovery process. When these approaches work together, many people feel stronger and clearer months faster than with rest alone.
This 3,000-word guide uses simple language and proven steps. Every exercise and idea comes from military health guides, rehab centers, and clinical experts. Always get a doctor’s okay before starting. Stop any move that causes sharp pain or new dizziness.
Why Neck Pain Is So Common After TBI
When the head snaps forward and back—like in a car crash or sports hit—the neck takes a huge force. Doctors call this whiplash-associated disorder. Muscles tighten, joints get stiff, and nerves can become irritated. Many people also develop forward head posture, where the head sits inches in front of the shoulders. Each inch forward adds about 10 pounds of stress to the neck muscles (Healthline, 2023a).
Left alone, tight neck muscles pull on the skull base, worsening headaches. They also make balance harder because the brain receives mixed signals from the upper neck. Gentle stretches and posture exercises can effectively address this issue early on.
Common Neck Problems After TBI
- Muscle spasms and knots
- Stiffness that limits turning the head
- Headaches that start at the base of the skull
- Forward head posture from pain guarding
- Dizziness when moving the head quickly
Safe Neck Stretches to Start in the First Weeks
These four stretches appear on official military and rehab fact sheets. Have them sit in a firm chair with feet flat on the floor. Breathe slowly. Hold each stretch 15–30 seconds and repeat 3–5 times, 2–3 times a day.
- Chin Tuck – Slide your chin straight back (like making a double chin) until you feel a stretch behind the neck. Do not tilt down. This is the single best move to fight forward head posture (U.S. Department of Defense, 2020; Healthline, 2023a).
- Side Bend – Sit tall. Slowly drop one ear toward the same shoulder until you feel a stretch on the opposite side. Keep your nose pointing forward. Use the hand on top of the head for a gentle extra pull if comfortable (Achieve Brain & Spine, n.d.).
- Neck Rotation – Turn your head to look over one shoulder as far as comfortable. Hold, then switch sides. Move only the neck, not the shoulders (U.S. Department of Defense, 2020).
- Upper Trapezius Stretch – Sit and place one hand under your thigh to anchor the shoulder. With the other hand, gently pull the head away and slightly forward. You will feel the stretch along the side and back of the neck (Healix Therapy, n.d.).
Tip: Warm the neck first with a warm shower or heating pad for 10 minutes.
Core and Trunk Exercises That Protect the Neck and Brain
A weak core forces the neck muscles to work overtime to keep the head steady. Simple seated core moves wake up the deep stomach and back muscles without jarring the brain.
Do these 3–4 times a week. Start with 8–10 repetitions and build to 15–20.
- Sitting Marching – Sit tall with hands on thighs. Lift one knee toward the chest while keeping the back straight, then lower slowly. Alternate legs. This exercise turns on the lower abs and hip flexors (Flint Rehab, 2023a).
- Lateral Trunk Flexion (Side Bends) – Sit tall. Slowly slide one hand down the side of the thigh as you bend to that side. Use the opposite core muscles to pull yourself back upright. Works the obliques and reduces side-to-side sway (Illinois Department of Central Management Services, n.d.).
- Seated Trunk Extension – Cross arms over chest. Lean forward 10–15 degrees, then slowly sit back tall using the back muscles. Keep the chin tucked to protect the neck (Flint Rehab, 2023a).
- Seated Weight Shifts – Scoot forward on the chair so feet are flat and knees are at 90 degrees. Shift weight side to side or front to back while keeping the trunk tall. This exercise is particularly beneficial for promoting early balance (Flint Rehab, 2023a).
Balance Exercises That Are Safe After TBI
Poor balance is one of the biggest fall risks after brain injury. Start every balance exercise seated or holding onto a sturdy surface.
Beginner Level (Weeks 1–4)
- Reach in different directions while seated
- Heel raises and toe raises while holding a counter
- March in place, holding onto a chair
Intermediate Level (Weeks 4–8)
- Stand with feet together, eyes open, then eyes closed for 10–20 seconds
- Single-leg stance holding a chair (5–10 seconds each leg)
- Stand on a firm cushion or folded towel (Neofect, n.d.)
Advanced Level
- Tandem stance (heel-to-toe) with arms out
- Walk heel-to-toe in a straight line
- Step over small objects while watching your feet
Do balance work for 5–10 minutes daily. Progress only when the easier level feels straightforward.
Gentle Yoga and Breathing for Brain and Body Recovery
Modified yoga poses calm the nervous system and safely stretch the entire spine.
- Seated Cat-Cow – Hands on knees. Inhale and arch the back while lifting the chest and chin slightly. Exhale and round the back while tucking the chin. Move slowly with the breath (Flint Rehab, 2023b).
- Seated Side Stretch – Inhale arms overhead. Exhale and lean to one side, keeping both sit bones on the chair. Hold 3–5 breaths on each side.
- Chair Warrior II – Sit sideways on the chair. Extend one leg back and bend the front knee. Reach arms out for a gentle chest and hip opener.
Yoga improves balance by 36% and reduces anxiety in brain-injury patients (Flint Rehab, 2023b).
How Integrative Chiropractic Care Helps TBI Recovery
Chiropractic care is not just about “cracking” the back. Doctors of chiropractic trained in brain-injury care use gentle techniques to:
- Remove pressure on nerves, leaving the spine
- Restore normal motion to stiff neck joints
- Reduce muscle spasms with soft-tissue therapy
- Improve blood flow and oxygen to the brain
- Correct forward head posture that slows healing
Studies and clinical reports show that spinal adjustments can reduce headache frequency, improve sleep, and speed return to work after concussion (Calibration Mansfield, n.d.; Northwest Florida Physicians Group, n.d.; Pinnacle Health Chiropractic, n.d.).
Dr. Alexander Jimenez, DC, APRN, FNP-BC, a dual-credentialed chiropractor and family nurse practitioner in El Paso, Texas, has treated thousands of patients with TBI, including veterans. He combines precise cervical adjustments, soft-tissue work, and functional neurology exercises. “The upper neck houses sensors that tell the brain where the head is in space. When those joints are stuck, the brain gets fuzzy signals, and balance suffers,” Dr. Jimenez explains in his clinical teaching (Jimenez, 2025). His patients often report clearer thinking and less dizziness within weeks of starting care.
The Important Role of Nurse Practitioners in TBI Care
Nurse practitioners (NPs) are trained to manage complex patients from head to toe. In TBI recovery, they:
- Watch for worsening symptoms (increased swelling, seizures, mood changes)
- Coordinate physical therapy, chiropractic, counseling, and medications
- Teach patients and families what is normal and what needs quick attention
- Adjust care plans as healing progresses
- Provide follow-up visits to catch problems early (Ackerman, 2012; Mayo Clinic, 2024; Nursing Center, 2023)
Because NPs spend more time with patients than many doctors, they often spot small improvements or setbacks first. Dr. Jimenez, who also holds APRN and FNP-BC credentials, uses this whole-person view in his clinic every day.
Sample 6-Week Gentle Recovery Plan
Week 1–2 (Very Gentle Phase)
- 5–10 minutes of chin tucks and side bends twice daily
- Sitting, marching 2 sets of 10 each leg
- Deep breathing for 3 minutes
- Short walks with a partner
Week 3–4 (Add Core and Balance)
- Add lateral trunk flexion and seated trunk extension
- Begin seated weight shifts and reaching
- One chiropractic visit for evaluation and gentle adjustment
Week 5–6 (Build Strength and Confidence)
- Add standing balance drills with support
- Try modified cat-cow and seated yoga stretches
- Increase reps to 15–20
- Weekly chiropractic care and NP follow-up
Rest for at least one full day between harder sessions. Keep a simple journal: note pain level (0–10), dizziness, and energy. Share it with your team.
Extra Self-Care Tips That Speed Healing
- Sleep 8–9 hours in a dark, quiet room
- Drink water all day (half your body weight in ounces)
- Eat protein and colorful vegetables at every meal
- Limit screen time in the first weeks—use blue-light glasses if needed
- Join an online TBI support group for encouragement
- Walk outside in nature when symptoms allow
When to Call the Doctor Right Away
Stop exercising and seek help if you have:
- Sudden severe headache
- Vomiting or vision changes
- Worsening confusion or slurred speech
- Seizure or loss of consciousness
Final Thoughts: Healing Is Possible and Often Faster Than You Think
A traumatic brain injury feels overwhelming at first, but the brain and body are built to heal. Gentle neck stretches, core work, balance drills, chiropractic adjustments, and strong nurse practitioner guidance give your recovery the best chance. Start small, stay consistent, and celebrate every tiny win.
Thousands of people—including veterans treated by Dr. Alexander Jimenez—return to work, sports, and family life after TBI by using exactly these safe, evidence-based steps. You can too.
References
Ackerman, L. L. (2012). Neurotrauma—The role of the nurse practitioner in traumatic brain injury. The Journal for Nurse Practitioners, 8(2), 104–109. https://www.npjournal.org/article/S1555-4155(11)00482-X/abstract
Achieve Brain & Spine. (n.d.). Patient exercises. https://www.achievebrainandspine.com/resources/patient-exercises/
Calibration Mansfield. (n.d.). How can integrative chiropractic care help with traumatic brain injuries? https://calibrationmansfield.com/how-can-integrative-chiropractic-care-help-with-traumatic-brain-injuries/
Flint Rehab. (2023a). Exercises for brain injury recovery. https://www.flintrehab.com/exercises-for-brain-injury-recovery/
Flint Rehab. (2023b). Yoga poses for brain injury. https://www.flintrehab.com/yoga-poses-for-brain-injury/
Healthline. (2023a). Forward head posture: Exercises and stretches to try. https://www.healthline.com/health/bone-health/forward-head-posture
Healix Therapy. (n.d.). Neck exercises for TMJ pain relief. https://healixtherapy.com/neck-exercises-tmj-pain-relief/
Illinois Department of Central Management Services. (n.d.). Traumatic brain injury recovery. https://cms.illinois.gov/benefits/stateemployee/bewell/getmoving/traumatic-brain-injury-recovery.html
Jimenez, A. (2025). Functional medicine and injury care clinical observations. https://dralexjimenez.com/
Mayo Clinic. (2024). Traumatic brain injury – Diagnosis & treatment. https://www.mayoclinic.org/diseases-conditions/traumatic-brain-injury/diagnosis-treatment/drc-20378561
Neofect. (n.d.). Balance exercise after brain injury. https://www.neofect.com/blog/balance-exercise-after-brain-injury
Northwest Florida Physicians Group. (n.d.). Using chiropractic care to treat traumatic brain injuries. https://northwestfloridaphysiciansgroup.com/using-chiropractic-care-to-treat-traumatic-brain-injuries/
Nursing Center. (2023). Neurotrauma—The role of the nurse practitioner in traumatic brain injury. https://www.nursingcenter.com/journalarticle?Article_ID=527301&Journal_ID=420955&Issue_ID=527288
Pinnacle Health Chiropractic. (n.d.). Six ways chiropractic care supports healing after TBI. https://www.pinnaclehealthchiro.com/blog/six-ways-chiropractic-care-supports-healing-after-tbi
U.S. Department of Defense. (2020, July 30). Neck pain following concussion/mTBI fact sheet. https://health.mil/Reference-Center/Fact-Sheets/2020/07/30/Neck-Pain-Following-ConcussionmTBI-Fact-Sheet