Related Articles
IRVING, Texas � Anthony Rotich (Cross Country) was announced as one of the 14 recipients of the Jim Castaneda Postgraduate Scholarship Award, announced by the league office on Tuesday afternoon.
The conference annually awards the $4,000 Postgraduate Scholarships to graduates as selected by the C-USA Faculty Athletics Representatives and approved by the Board of Directors.
Rotich, a civil engineer major and mathematics minor, graduated from UTEP as a three-time C-USA All-American honoree and a four-time C-USA Commissioner�s Academic Honor Roll recipient. The Kenya native was a four-time NCAA Champion and an 11-time Mountain Region Athlete of the Year. He was named the 2014 C-USA Cross Country Athlete of the Year.
Rotich is applying to UTEP�s College of Engineering � Construction Management.
Check Also
Emmanuel Korir has been named a semifinalist for college track and field�s highest individual honor, �
Acupuncture Proves Effective ER Painkiller
Acupuncture is a safe and effective alternative to pain medications for some emergency room patients, a new study reports.
“While acupuncture is widely used by practitioners in community settings for treating pain, it is rarely used in hospital emergency departments,” said study lead investigator Marc Cohen. He is a professor in the School of Health and Biomedical Sciences at RMIT University in Melbourne, Australia.
The study — billed as the world’s largest randomized, controlled trial of acupuncture in the emergency department — included 528 patients.
The study participants were seen at four Australian emergency departments for acute low back pain, migraines or ankle sprains. Patients who said their level of pain was at least 4 on a 10-point scale received one of three treatments: acupuncture alone; acupuncture with painkillers; or painkillers alone.
One hour after treatment, less than 40 percent of all patients had significant pain reduction, meaning at least a 2-point decline on the 10-point scale. More than 80 percent still had a pain rating of at least 4, the findings showed.
But two days later, most patients were satisfied. Overall, nearly 83 percent of acupuncture-only patients said they would probably or definitely repeat their treatment, compared with about 81 percent in the combined group, and 78 percent who took painkillers alone.
“Emergency nurses and doctors need a variety of pain-relieving options when treating patients, given the concerns around opioids such as morphine, which carry the risk of addiction when used long-term,” Cohen said in a university news release.
The study results suggest acupuncture would be especially beneficial for patients who can’t use standard pain-relieving drugs because of other medical conditions, Cohen added.
But he noted that more research is needed because some patients remained in pain no matter what treatment they received.
The study was published June 18 in the Medical Journal of Australia.

Biomechanics: Hip Weakness & Shin Splints
Chiropractor, Dr. Alexander Jimenez examines the role of biomechanics in medial tibial stress syndrome…
Medial tibial stress syndrome (MTSS � commonly known as shin splints) is not medically serious, yet can suddenly side- line an otherwise healthy athlete. Roughly five percent of all athletic injuries are diagnosed as MTSS(1).
The incidence increases in specific populations, accounting for 13-20% of injuries in runners and up to 35% in military recruits(1,2). MTSS is defined as pain along the posterior-medial border of the lower half of the tibia, which is present during exercise and (usually) diminishes during rest. Athletes identify the lower front half of the leg or shin as the location of discomfort. Palpation along the medial tibia usually reproduces the pain.
Causes Of MTSS
There are two main hypothesized causes for MTSS. The first is that contracting leg�muscles place a repeated strain upon the medial portion of the tibia, inducing periostitis � inflammation of the periosteal outer layer of bone. While the pain of a shin splint is felt along the anterior leg, the muscles that arise from this area are the posterior calf muscles (see figure 1). The tibialis posterior, flexor digitorum longus, and the soleus all arise from the posterior- medial aspect of the proximal half of the tibia. Therefore, the traction force from these muscles on the tibia is unlikely to be the cause of the pain typically felt on the distal portion of the leg.
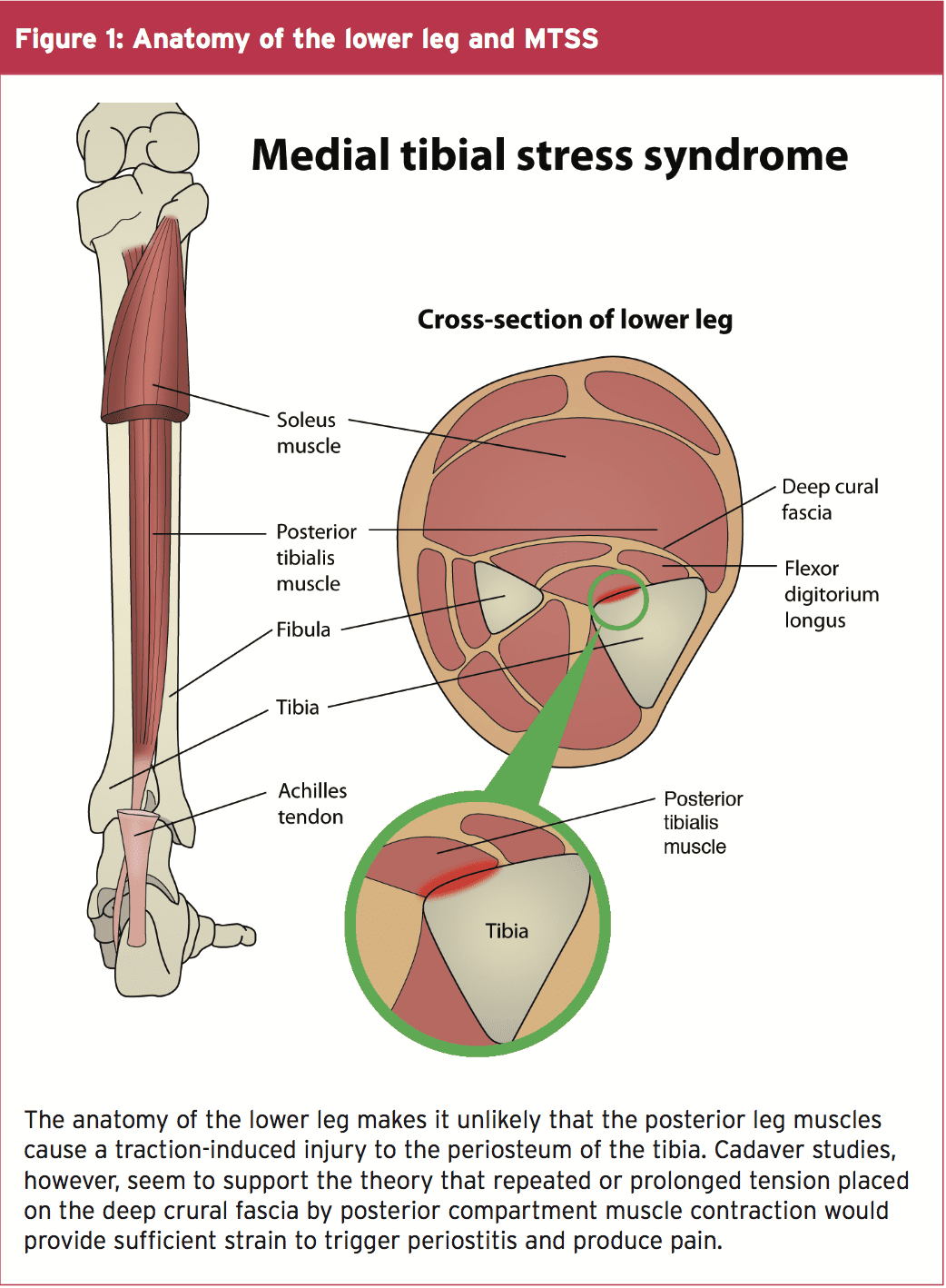
A variation of this tension theory is that the deep crural fascia (DCF) � the though- connective tissue that surrounds the deep posterior compartment muscles of the leg � pulls excessively on the tibia, again causing trauma to the bone. Researchers at�the University of Honolulu examined a single leg from five male and 11 female adult cadavers. They confirmed that in these specimens, the muscles of the posterior compartment originated above the portion of the leg that is typically painful in MTSS, and the DCF indeed attached along the entire length of the medial tibia(3).
Doctors at the Swedish Medical Centre in Seattle, Washington wondered if, given the anatomy, could the tension from the posterior calf muscles produce a related strain on the tibia at the insertion of the DCF, and thus be the mechanism of injury(4)?
In a descriptive laboratory pilot study of three fresh cadaver specimens, they found that strain at the insertion site of the DCF along the medial tibia progressed linearly as tension increased in the posterior leg muscles. This confirmed that a mechanism for a tension-induced injury at the medial tibia is plausible. However, studies of bone periosteum in MTSS patients have yet to find inflammatory markers consistently enough to confirm the periostitis theory(5).
Tibial Bowing
The second causation theory for MTSS is that repetitive or excessive loading causes a bone-stress reaction in the tibia. The tibia, unable to adequately bear the load, bends during weight bearing. The overload results in micro damage within the bone, and not just along the outer layer. When the repetitive loading outpaces the bone�s ability to repair, localized osteopenia can result. Thus, some consider a tibial stress fracture to be the result of a continuum of bone stress reactions that include MTSS(1).
Magnetic resonance imaging (MRI) of the symptomatic leg often shows bone�marrow edema, periosteal lifting, and areas of increased bony resorption in patients with MTSS(1,5). This supports the bone- stress reaction theory. Magnetic resonance imaging of an athlete with a clinical presentation of MTSS can also help rule out other causes of lower leg pain such as tibial stress fracture, deep posterior compartment syndrome, and popliteal artery entrapment syndrome.
Risk Factors For MTSS
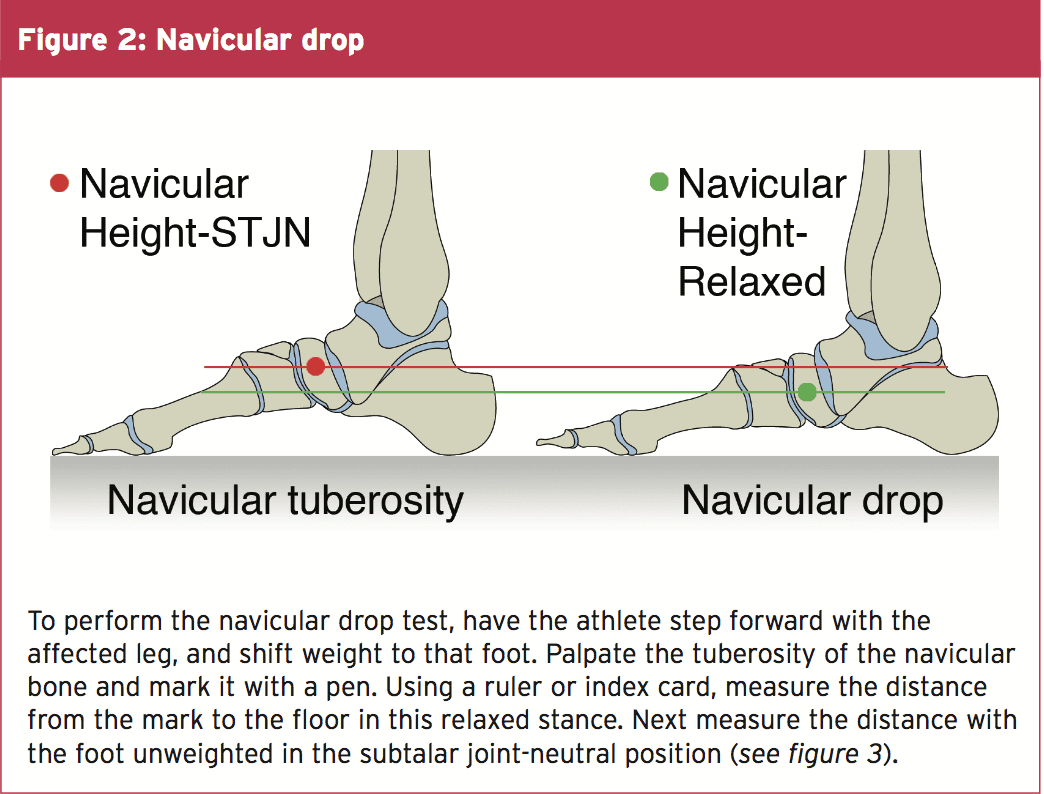
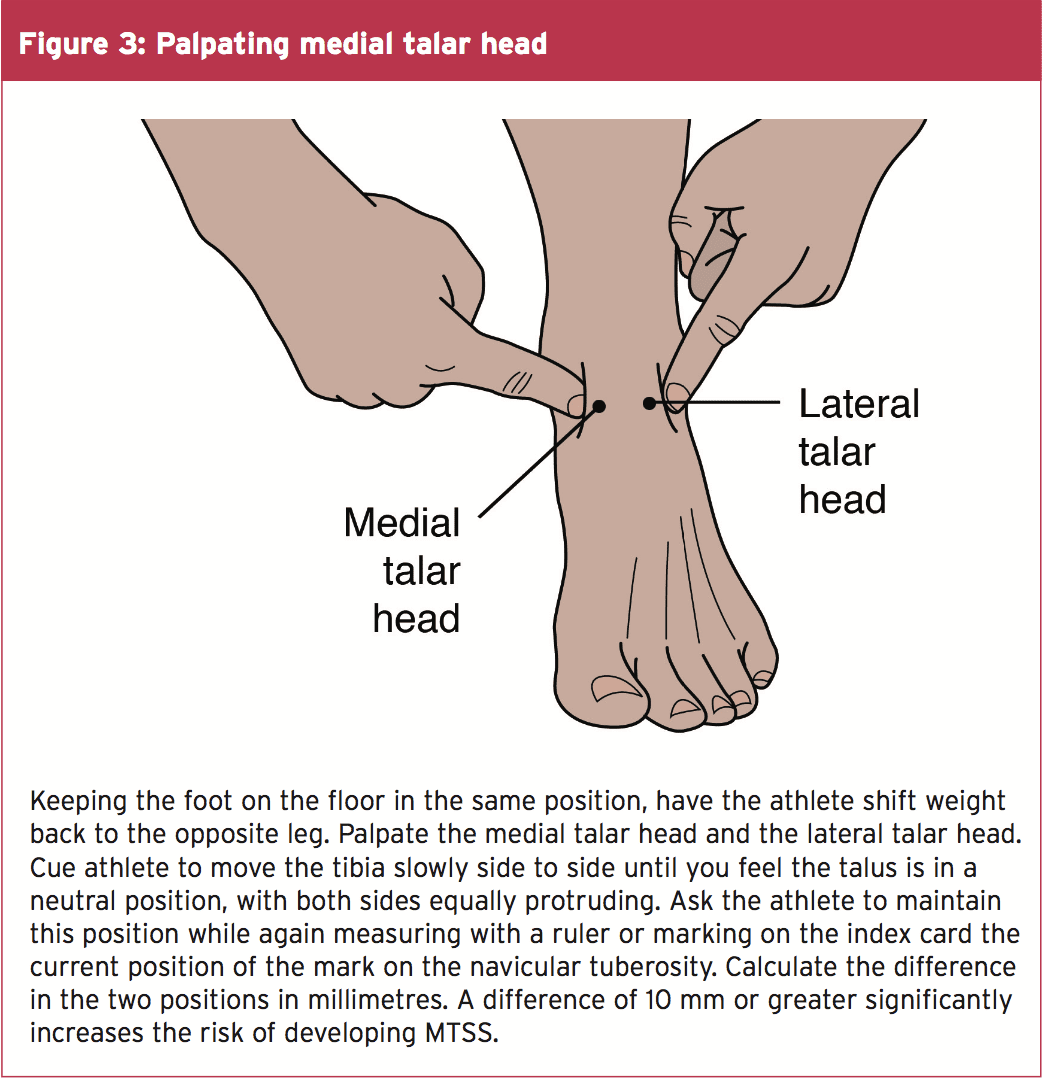
While the aetiology of MTSS is still theoretical, the risk factors for athletes developing it are well determined. A large navicular drop, as determined by the navicular drop test (NDT), significantly correlates with a diagnosis of MTSS(2,5). The NDT measures the difference in height position of the navicular bone, from a neutral subtalar joint position in supported non-weight bearing, to full weight bearing (see figures 2 and 3). The NDT is an indication of the degree of arch collapse during weight bearing. An excursion of more than 10 mm is considered excessive and a significant risk factor for the development of MTSS(5).
Research suggests that athletes with MTSS are found more likely to be female, have a higher BMI, less running experience, and a previous history of MTSS(2,5). Running kinematics for females can differ from males and fit a pattern that is known to leave them vulnerable to anterior cruciate ligament tears and patellofemoral pain syndrome(5). This same biomechanical pattern may also predispose females to MTSS. Hormonal considerations and low bone density are possibly contributing factors in increasing the risk of MTSS in the female athlete as well.
A higher BMI in an athlete likely indicates they have more muscle mass rather than they are overweight. The end result, however, is the same in that the legs bear a significantly heavy load. It is thought that in these instances, the bone growth�stimulated by the tibial bowing may not progress rapidly enough, and injury to the bone occurs. Therefore, those with a higher BMI may need to progress their training programs more slowly, to allow for adaptation.
Those with less running experience are more likely to make training errors (often identified by the athlete) as the catalyst for MTSS. These include increasing distance�too rapidly, changing terrain, overtraining, poor equipment (shoes), etc. Inexperience may also lead the athlete to return to activity too soon, thus accounting for the higher prevalence of MTSS in those who had suffered MTSS previously. Full recovery from MTSS can take anywhere from six to ten months, and if the cause of injury was not rectified or the athlete returns to training too soon, the chances are good the pain will return(5).
Biomechanical Considerations
The NDT is used as a measurable indication of foot pronation. Pronation is a tri-planar movement comprised of eversion at the hind foot, abduction of the forefoot, and dorsiflexion of the ankle. Pronation is a normal movement, and essential in walking and running. When the foot strikes the ground at the initial contact phase of running, the foot begins to pronate and the joints of the foot assume a loose-packed position. This flexibility helps the foot absorb ground reaction forces (see figure 4).
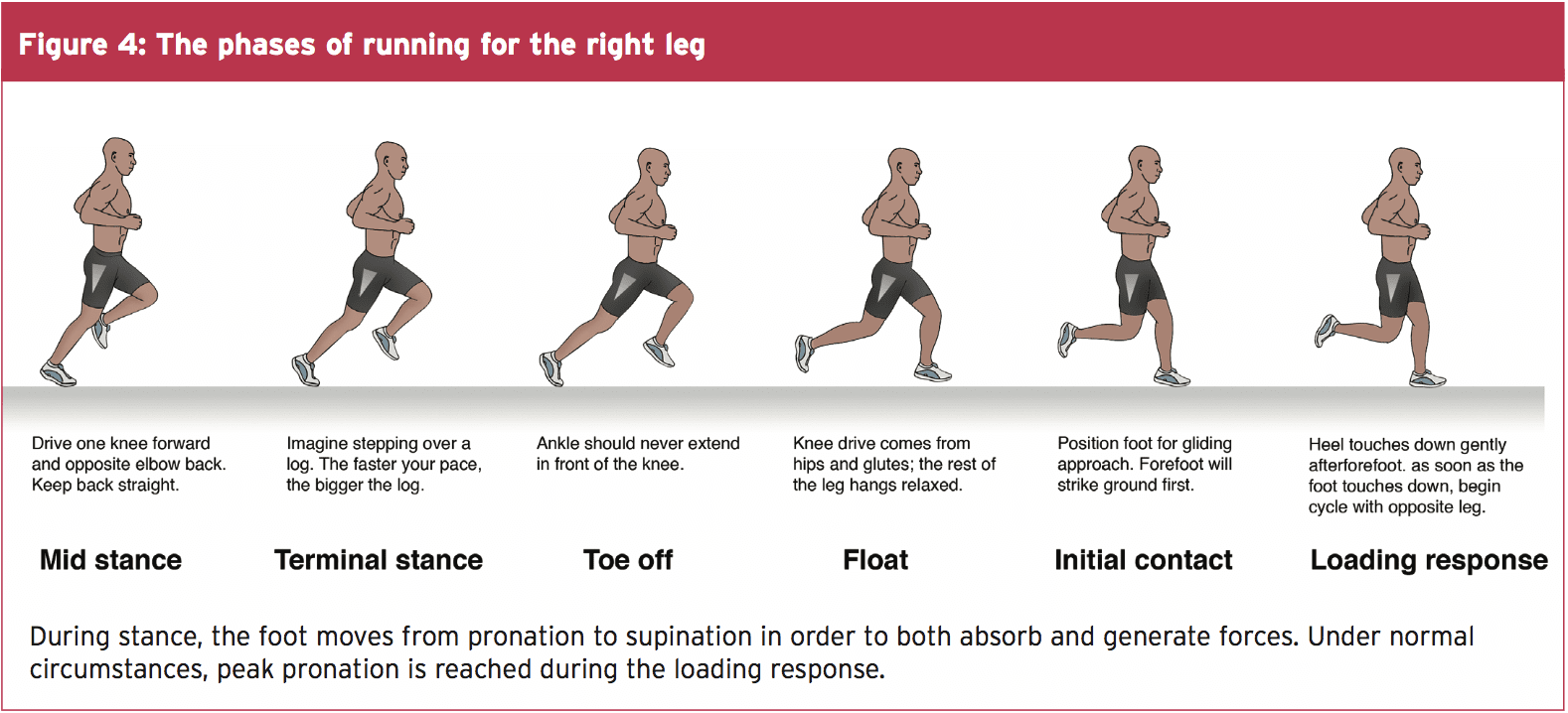
During the loading response phase, the foot further pronates, reaching peak pronation by around 40% of stance phase(6). In mid stance, the foot moves out of pronation and back to a neutral position. During terminal stance, the foot supinates, moving the joints into a closed packed position and creating a rigid lever arm from which to generate the forces for toe off.
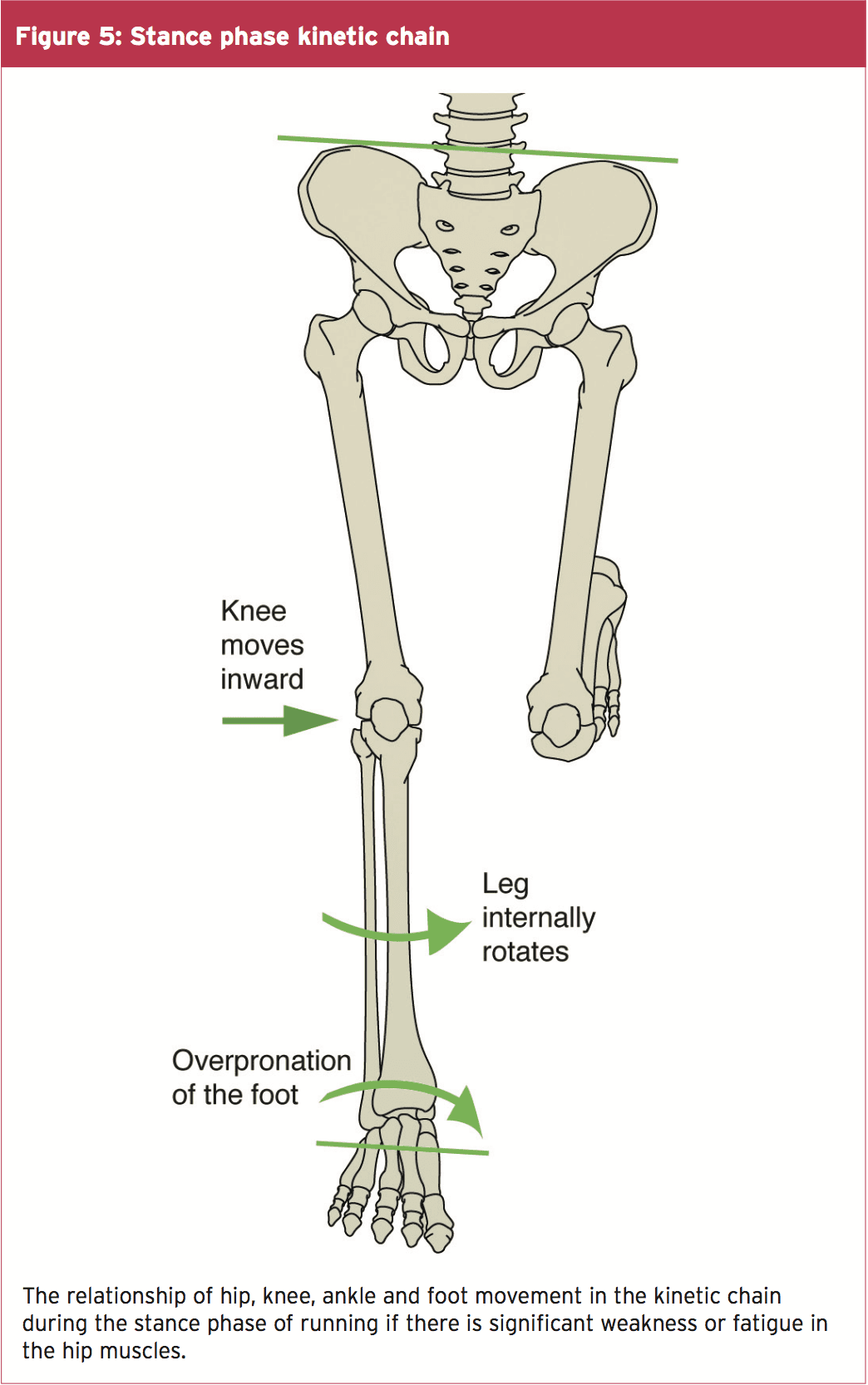
Beginning with the loading response phase and throughout the remainder of the single leg stance phase of running, the hip is stabilized, extended, abducted and externally rotated by the concentric contraction of the hip muscles of the stance�leg (the gluteals, piriformis, obturator internus, superior gemellus and inferior gemellus). Weakness or fatigue in any of these muscles can result in internal rotation of the femur, adduction of the knee, internal rotation of the tibia, and over-pronation (see figure 5). Overpronation therefore, can be a result of muscle weakness or fatigue. If this is the case, the athlete may have a quite normal NDT, and yet when the hip muscles don�t function as needed, can overpronate.
In a runner who has significant over pronation, the foot may continue to pronate into mid stance, resulting in a�delayed supination response, and thus less power generation at toe off. The athlete may attempt two biomechanical fixes here that could contribute to the development of MTSS. Firstly, the tibialis posterior will strain to prevent the over pronation. This can add tension to the DCF and strain the medial tibia. Secondly, the gastroc-soleus complex will contract more forcefully at toe off to improve the power generation. Again, the increased force within these muscle groups can theoretically add tension to the medial tibia through the DCF and possibly irritate the periosteum.
Evaluating The Injured Athlete
Knowing that over pronation is one of the leading risk factors for MTSS, start your evaluation at the ground and work your way up. First, perform the NDT, noting if the difference is more than 10mm. Analyze the athlete�s running gait on a treadmill, preferably when the muscles are fatigued, as at the end of a training run. Even with a normal NDT, you may see evidence of over pronation in running (see figure 6).
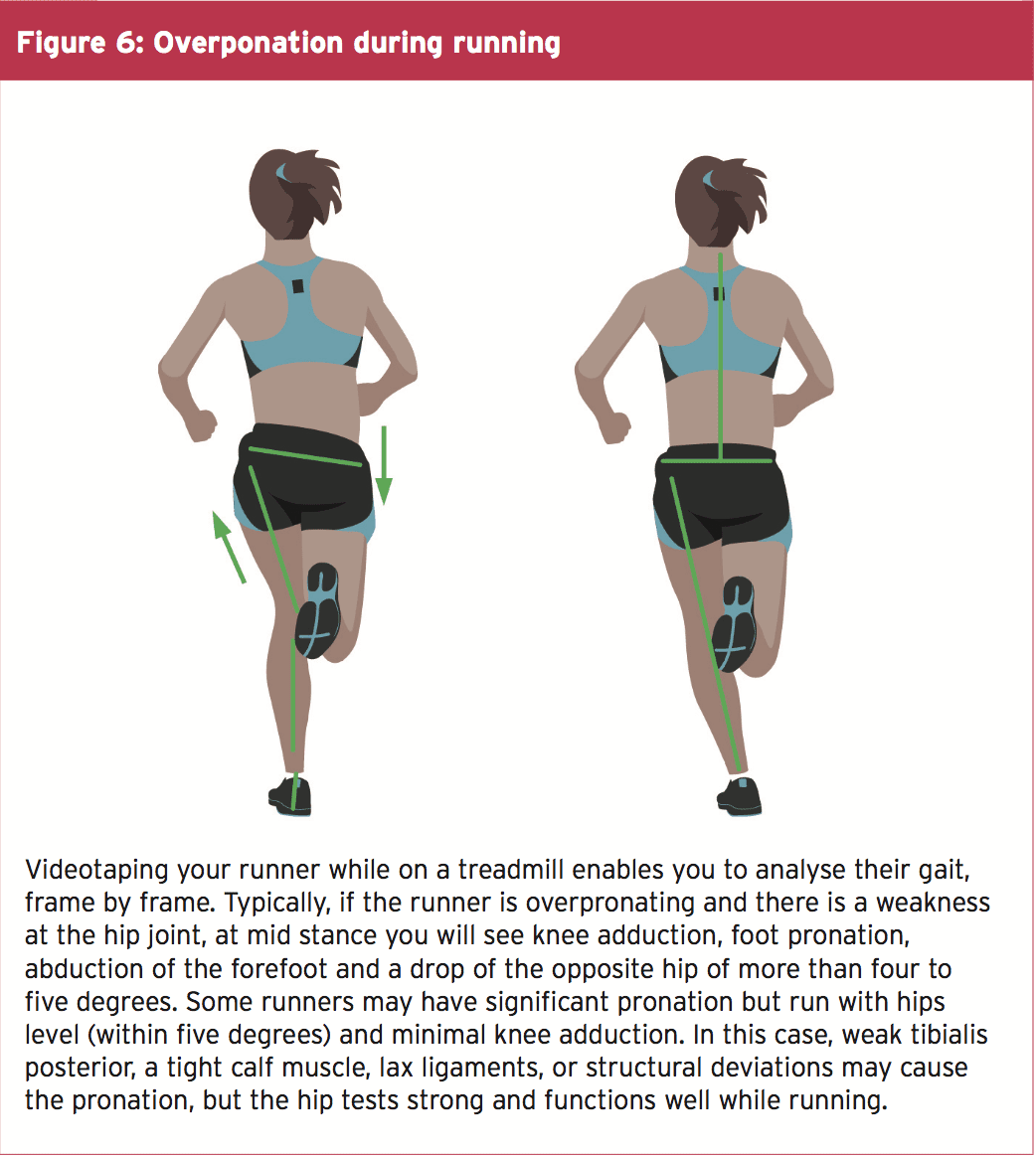
Next evaluate the knee. Is it adducted? Notice if the hip is level or if either hip is more than 5 degrees from level. These are indications that there is likely weakness at the hip. Traditional muscle testing may not reveal the weakness; therefore, functional muscle testing is required.
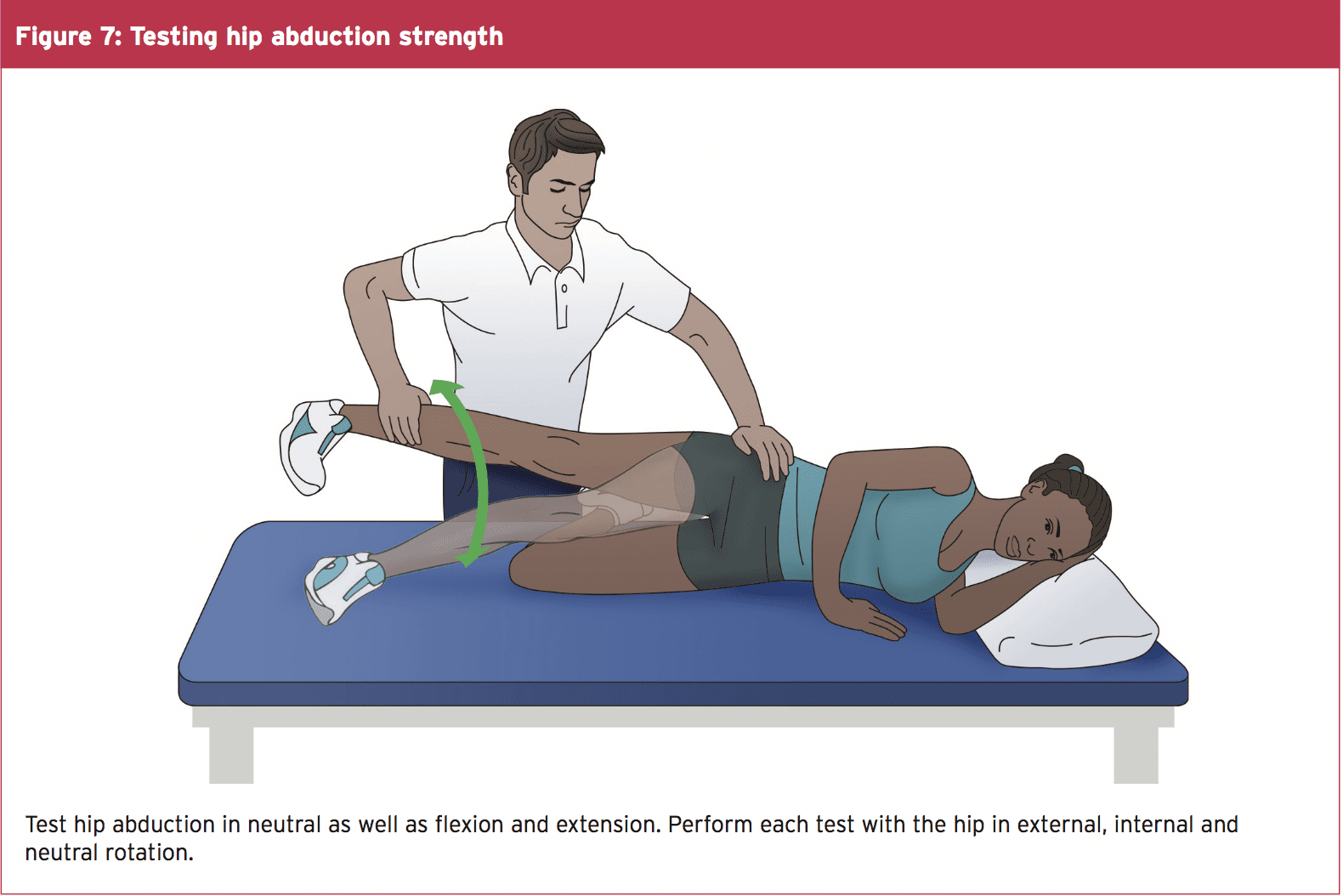
Observe the athlete perform a one-legged squat with arms in and arms overhead. Does the hip drop, the knee adduct and the foot pronate? Test the strength of hip abductors in side lying, with hip in neutral, extended, and flexed, keeping the knee straight (see figure 7). Test all three positions with hip rotated in neutral, and at end ranges of external and internal rotation. Test hip extension in prone with the knee straight and bent, in all three positions of hip rotation: external, neutral and internal. The position where you find the weakness is where you should begin strengthening activities.
Treat The kinetic Chain
If there is weakness in the hip, begin by having the athlete perform isometric exercises in the position of weakness. For instance, if you find weakness in hip abduction with extension, then begin isolated isometrics in this position. Not until the muscles consistently fire isometrically in this position for three to five sets of 10 to 20 seconds should you add movement. Once the athlete achieves this level, begin concentric contractions, in that same position, against gravity. Some examples are unilateral bridging and side lying abduction. Eccentric contractions should follow, and then sport specific drills.
Keep in mind if there are other biomechanical compensations, they must also be addressed. If the tibialis posterior is also weak, begin strengthening there. If the calf muscles are tight, initiate a stretching program. Utilise whatever modalities might be helpful. Lastly, consider a stabilising shoe if the ligaments in the foot are over stretched. Using a stabilising shoe for a short time during rehabilitation can�be helpful in cuing the athlete to adopt new movement patterns.
Conclusion
The best way to prevent shin pain from MTSS is to decrease the athlete�s risk factors. Ideally, each athlete should have a basic running gait analysis and proper shoe fitting. Include hip strengthening in functional positions such as unilateral stance as part of the strengthening program. Pair inexperienced athletes with a more experienced mentor to ensure proper training, use of equipment, and investigation of pain at onset. They may be more likely to tell a teammate they are feeling pain than a coach or trainer. Progress the running schedule of heavier athletes more slowly to allow adaptation of the bone. Ensure that athletes fully rehabilitate before returning to play because the chances of recurrence of MTSS are high.
References
1. Am J Sports Med. 2015 Jun;43(6):1538-47
2. Br J Sports Med. 2015 Mar;49(6):362-9
3. Med Sci Sports Exerc. 2009;41(11):1991-1996
4. J Am Podiatr Med Assoc. 2007 Jan;97(1):31-6
5. J Sports Med. 2013;4:229-41
6. Gait and Posture. 1998;7:77�95

Chiropractic for the Management of Mechanical Spine Pain
Title: The Utilization of Long Term Care for Herniated Lumbar Discs with Chiropractic for the Management of Mechanical Spine Pain.
Dr. Alex Jimenez, doctor of chiropractic, focuses on the diagnosis, treatment and prevention of a variety of injuries and conditions associated with the musculoskeletal and nervous systems, utilizing several chiropractic methods and techniques. The following procedures may be similar to his own but can differ according to the specific issue and complications by which the individual is diagnosed.
Abstract: To explore the utilization of chiropractic treatment consisting of spinal adjusting, axial traction, electrical muscle stimulation, and core stabilization exercise for the management of mechanical spine pain. Diagnostic studies included physical examination, orthopedic and neurological examinations, and lumbar spine MRI. The patient reports long-term success in reducing pain levels and increasing functionality by having the ability to perform activities of daily living (ADL�s) without frequent flare-ups which he reported of prior to undergoing chiropractic treatment.
Introduction: On 2/6/2015, a 49 year old male certified nursing assistant, presented for consultation and examination due to a work injury which occurred on 11/12/2001. The patient stated he sustained a lifting injury that resulted in severe low back pain. He stated that he was under the care of a pain management interventionist receiving epidural injections in his lumbar spine on an ongoing basis since the injury occurred. He added that the injections helped him to cope with the elevated pain levels he experienced on a frequent basis. The patient had previously received chiropractic and physical therapy for his injury and reported that the therapies did help him when he was actively treating. He informed it had been over 3 years since he last treated with chiropractic or physical therapy.
Chiropractic Back Pain Management
The patient presented to my office on 2/6/2015 with a chief complaint of lumbar pain. He rated the discomfort as a 7 on a visual analog scale of 10 with 10 being the worst and the pain was noted as being constant (76-100% of the time). The onset of pain was a result of the work injury described above. He reported that the pain would aggravate by activities which required excessive or repetitive bending, lifting, and pulling. He stated he experienced flare-up episodes 4-6 times a month depending on the type of activities he was involved with. The quality of the discomfort was described as aching, gnawing, sharp, shooting, and painful and was noted as being the worst at the end of the day. He stated that when his pain levels were elevated, it would limit his ability of getting a good night sleep. The patient further noted he was experiencing numbness and tingling in both legs and his right foot.
Prior History:
The patient denied any prior or subsequent low back injuries and/or traumas.
Clinical Findings:
The patient was 5 feet 10 inches and weighed 230 pounds. His sitting blood pressure was 132/86 and his radial pulse was 74 BPM. The patient�s Review of Systems and Family History were unremarkable.
An evaluation and management exam was performed. The exam consisted of visual assessment of range of motion, manual muscle tests, deep tendon reflexes, digital and motion palpation, and other neurological and orthopedic tests. Palpation revealed areas of spasm, hypertonicity, asymmetry, and end point tenderness indicative of subluxation at T12, L2, and L4. Palpation of the lumbar muscles revealed moderate to severe muscle spasms in the left piriformis, right piriformis, right sacrospinalis, right gluteus maximus, right erector spinae, right quadratus lumborum and right iliacus. He presented with postural deviations that were found using a plumb line assessment showing short right leg (pelvic deficiency), head tilted to the left, high left shoulder and high right hip. Point tenderness was notably present along the midline of the spine at the L4 and L5 level.
Manual, subjectively rated strength tests were performed on some of the major muscle groups of the lower extremities, based on the AMA Guides to the Evaluation of Permanent Impairment, 4th Ed., 1993/5th ed., 2001. A rating scale of five to zero was used, with five representing normal muscle strength. A muscle strength loss of the lower extremities indicates a neurological facilitation resulting from dysfunction in the lumbar spine. Grade 4 muscle weakness was noted on the right extensor hallicus longus.
Dermatomal sensation was decreased at L4 on the right and decreased at L5 on the right.
Reflex testing was completed and was diminished: 0/+2 on the right patella and +1/+2 on the left patella. The following lumbar orthopedic examinations were performed and found to be positive: Ely’s on the right, Hibb’s on the right, Iliac compression test and Bragard’s on the right.
Lumbar Range of Motion tested with Dual Inclinometers:
Range of Motion Normal Examination % Deficit
| Flexion | 90 | 40 | 56 | |
| Extension | 25 | 10 | 60 | |
| Left Lateral Flexion | 40 | 20 | 50 | |
| Right Lateral Flexion | 40 | 15 | 62 | |
| Left Rotation | 35 | 25 | 29 | |
| Right Rotation | 35 | 20 | 43 |
Flexion and left lateral bending were painful at end range. The patient�s limitation to bend is corroborated by the persistent spasticity of lack of motion eliciting pain upon exertion in the lumbar spine.
MRI Results
The MRI images were personally reviewed. The lumbar MRI performed on 9/29/2014 revealed anterior positioning of the L4 vertebral body with respect to L5 with a right L4-L5 protrusion compromising the right neural foramen. There is a central herniation at the L5-S1 disc.
Fig. 1, (A), (B), (C) shows in T2 MRI images (A) is Sagittal and (B) is Axial at L4-L5 and (C) is Axial at L5-S1
Fig. 1 (A) Sagital

Fig. 1 (B) T2 Axial at L4-L5

Fig. 1 (C) T2 Axial at L5-S1

After reviewing the history, physical and neurological examination, and MRI�s it was determined that chiropractic treatment was medically indicated and warranted. Frequency of treatment was determined 1 time a week.
The patient was placed on a treatment plan consisting of high velocity low amplitude chiropractic adjustments, axial traction, electrical muscle stimulation, and core stabilization exercise. The patient responded in favorable fashion to the chiropractic treatment over a 6 month period. The patient demonstrated subjective and objective improvement and his care plan was reduced to one time every two weeks to manage and modulate pain levels associated with his permanent condition.
On follow-up re-evaluation approximately 9 months after starting supportive treatment the patient showed improvement in range of motion testing.
Lumbar Range of Motion was tested with Dual Inclinometers:
Range of Motion Normal Examination % Deficit
| Flexion | 90 | 70 | 13 | |
| Extension | 25 | 20 | 20 | |
| Left Lateral Flexion | 40 | 35 | 12 | |
| Right Lateral Flexion | 40 | 30 | 25 | |
| Left Rotation | 35 | 30 | 15 | |
| Right Rotation | 35 | 25 | 29 |
The patient also reported a reduction in pain levels rating the low back discomfort as a4 on a scale of 10 with 10 being the worst and the pain was noted as beingintermittent 25 to 50% of the time. Decreased muscle spasm in the lumbar paraspinal muscles was noted as well as better symmetry and tonicity. The patient reported the ability of getting a better night sleep and waking up in the morning with less rigidity and achiness. He stated he was able to perform his work duties and activities of daily living with less flare-ups and exacerbations occurring only 1-2 times a month. The core training exercises we worked on have helped stabilize the patient�s spine and protected it from reinjuring the already injured tissues.
Conclusion of Research Study
Chiropractic care has been shown to be both safe and effective in treating patients with disc herniation and accompanying radicular symptoms1-4. Spinal chiropractic adjustive therapy has been proven to modulate pain6. This patient presented with chronic low back pain sequela to an injury that occurred over 13 years ago. The patient had prior success in reduction of pain when he was treating with chiropractic in the past then discontinued treatment. The patient has been treating with pain management intervention since the injury occurred and it has helped him reduce his pain but has done minimal for him from a functional and mechanical standpoint. The history and exam indicated the presence of 2 herniated discs in the lumbar spine. Lumbar MRI�s were ordered prior to being evaluated and the images were viewed to establish an accurate diagnosis, prognosis, and treatment plan. Long term chiropractic treatment has been utilized successfully in this case study to reduce pain levels and restore the patient�s functional capacity of performing activities of daily living and work duties with less flare ups and exacerbations of low back pain.
Competing Interests: There are no competing interests in the writing of this case report.
De-Identification: All of the patient�s data has been removed from this case.
The scope of our information is limited to chiropractic and spinal injuries and conditions. To discuss options on the subject matter, please feel free to ask Dr. Jimenez or contact us at 915-850-0900 . 
- Leeman S., Peterson C., Schmid C., Anklin B., Humphryes B., (2014) Outcomes of Acute and Chronic Patients with Magnetic Resonance Imaging-Confirmed Symptomatic Lumbar Disc Herniation Receiving High-Velocity, Low Amplitude, Spinal Manipulative Therapy: A Prospective Observational Cohort Study With One-Year Follow Up, Journal of Manipulative and Physiological Therapeutics, 37 (3) 155-163
- Hahne AJ, Ford JJ, McMeeken JM, “Conservative management of lumbar disc herniation with associated radiculopathy: a systematic review,”Spine35 (11): E488�504 (2010).
- Rubinstein SM, van Middelkoop M, et. al, “Spinal manipulative therapy for chronic low-back pain,”Cochrane Database Syst Rev(2): CD008112. doi:10.1002/14651858.CD008112.pub2. PMID 21328304.
- Hoiriis, K. T., Pfleger, B., McDuffie, F. C., Cotsonis, G., Elsangak, O., Hinson, R. & Verzosa, G. T. (2004). A randomized clinical trial comparing chiropractic adjustments to muscle relaxants for subacute low back pain. Journal of Manipulative and Physiological Therapeutics, 27(6), 388-398.
- Coronado, R. A., Gay, C. W., Bialosky, J. E., Carnaby, G. D., Bishop, M. D., & George, S. Z. (2012).Changes in pain sensitivity following spinal manipulation: A systematic review and meta-analysis. Manuscript in preparation.
- Whedon, J. M., Mackenzie, T.A., Phillips, R.B., & Lurie, J.D. (2014). Risk of traumatic injury associated with chiropractic spinal manipulation in Medicare Part B beneficiaries aged 66-69. Spine, (Epub ahead of print) 1-33.
Additional Topics: Recovering from Auto Injuries
After being involved in an automobile accident, many victims frequently report neck or back pain due to damage, injury or aggravated conditions resulting from the incident. There’s a variety of treatments available to treat some of the most common auto injuries, including alternative treatment options. Conservative care, for instance, is a treatment approach which doesn’t involve surgical interventions. Chiropractic care is a safe and effective treatment options which focuses on naturally restoring the original dignity of the spine after an individual suffered an automobile accident injury.

TRENDING TOPIC: EXTRA EXTRA: New PUSH 24/7�? Fitness Center