1 Houston MC. Treatment of hypertension with nutraceuticals, vitamins, antioxidants and minerals. Expert Rev�Cardiovasc Ther 2007; 5: 681-691 [PMID: 17605647 DOI: 10.1159/000098012]
2 Eaton SB, Eaton SB, Konner MJ. Paleolithic nutrition revisited:
a twelve-year retrospective on its nature and implications.
Eur J Clin Nutr 1997; 51: 207-216 [PMID: 9104571 DOI:
10.1038/sj.ejcn.1600389]
3 Houston MC, Harper KJ. Potassium, magnesium, and calcium:
their role in both the cause and treatment of hypertension.
J Clin Hypertens (Greenwich) 2008; 10: 3-11 [PMID:
18607145 DOI: 10.1111/j.1751-7176.2008.08575.x]
4 Layne J, Majkova Z, Smart EJ, Toborek M, Hennig B. Caveolae:
a regulatory platform for nutritional modulation of inflammatory
diseases. J Nutr Biochem 2011; 22: 807-811 [PMID:
21292468 DOI: 10.1016/j.jnutbio.2010.09.013]
5 Dandona P, Ghanim H, Chaudhuri A, Dhindsa S, Kim SS.
Macronutrient intake induces oxidative and inflammatory
stress: potential relevance to atherosclerosis and insulin
resistance. Exp Mol Med 2010; 42: 245-253 [PMID: 20200475
DOI: 10.3858/emm.2010.42.4.033]
6 Berdanier CD. Nutrient-gene interactions. In: Ziegler EE,
Filer LJ Jr, eds. Present Knowledge in Nutrition, 7th Ed.
Washington. DC: ILSI Press. 1996: 574-580
7 Talmud PJ, Waterworth DM. In-vivo and in-vitro nutrientgene
interactions. Curr Opin Lipidol 2000; 11: 31-36 [PMID:
10750691 DOI: 10.1097/00041433-200002000-00005]
8 Lundberg AM, Yan ZQ. Innate immune recognition receptors
and damage-associated molecular patterns in plaque
inflammation. Curr Opin Lipidol 2011; 22: 343-349 [PMID:
21881501 DOI: 10.1097/MOL.0b013e32834ada80]
9 Zhao L, Lee JY, Hwang DH. Inhibition of pattern recognition
receptor-mediated inflammation by bioactive phytochemicals.
Nutr Rev 2011; 69: 310-320 [PMID: 21631512 DOI:
10.1111/j.1753-4887.2011.00394.x]
10 Houston MC. The importance of potassium in managing
hypertension. Curr Hypertens Rep 2011; 13: 309-317 [PMID:
21403995 DOI: 10.1007/s11906-011-0197-8]
11 Broadhurst CL. Balanced intakes of natural triglycerides for
optimum nutrition: an evolutionary and phytochemical perspective.
Med Hypotheses 1997; 49: 247-261 [PMID: 9293470
DOI: 10.1016/S0306-9877(97)90210-3]
12 Eftekhari A, Mathiassen ON, Buus NH, Gotzsche O, Mulvany
MJ, Christensen KL. Disproportionally impaired microvascular
structure in essential hypertension. J Hypertens
2011; 29: 896-905 [PMID: 21330935 DOI: 10.1097/�HJH.0b013e
3283447a1c]
13 Touyz RM. New insights into mechanisms of hypertension.
Curr Opin Nephrol Hypertens 2012; 21: 119-121 [PMID:
22257800 DOI: 10.1097/MNH.0b013e328350a50f]
14 Xing T, Wang F, Li J, Wang N. Hypertension: an immunologic
disease? J Hypertens 2012; 30: 2440-2441 [PMID:
23151885 DOI: 10.1097/HJH.0b013e32835953f9]
15 Giannattasio C, Cattaneo BM, Mangoni AA, Carugo S, Stella
ML, Failla M, Trazzi S, Sega R, Grassi G, Mancia G. Cardiac
and vascular structural changes in normotensive subjects
with parental hypertension. J Hypertens 1995; 13: 259-264
[PMID: 7615957]
16 Goncharov A, Bloom M, Pavuk M, Birman I, Carpenter
DO. Blood pressure and hypertension in relation to levels of
serum polychlorinated biphenyls in residents of Anniston,
Alabama. J Hypertens 2010; 28: 2053-2060 [PMID: 20644494]
17 Houston MC. Role of mercury toxicity in hypertension, cardiovascular
disease, and stroke. J Clin Hypertens (Greenwich)
2011; 13: 621-627 [PMID: 21806773]
18 Al-Ghamdi A. Role of herpes simplex virus-1, cytomegalovirus
and Epstein-Barr virus in atherosclerosis. Pak J Pharm
Sci 2012; 25: 89-97 [PMID: 22186314]
19 Kotronias D, Kapranos N. Herpes simplex virus as a determinant
risk factor for coronary artery atherosclerosis
and myocardial infarction. In Vivo 2005; 19: 351-357 [PMID:
15796197]
20 Grahame-Clarke C, Chan NN, Andrew D, Ridgway GL,
Betteridge DJ, Emery V, Colhoun HM, Vallance P. Human
cytomegalovirus seropositivity is associated with impaired
vascular function. Circulation 2003; 108: 678-683 [PMID:
12900349 DOI: 10.1161/01.CIR.0000084505.54603.C7]
21 Nayak DU, Karmen C, Frishman WH, Vakili BA. Antioxidant
vitamins and enzymatic and synthetic oxygen-derived
free radical scavengers in the prevention and treatment
of cardiovascular disease. Heart Dis 2001; 3: 28-45 [PMID:
11975768 DOI: 10.1097/00132580-200101000-00006]
22 Kizhakekuttu TJ, Widlansky ME. Natural antioxidants and
hypertension: promise and challenges. Cardiovasc Ther 2010;
28: e20-e32 [PMID: 20370791 DOI: 10.1111/�j.1755-5922.2010.0
0137.x]
23 Kitiyakara C, Wilcox CS. Antioxidants for hypertension.
Curr Opin Nephrol Hypertens 1998; 7: 531-538 [PMID: 9818200
DOI: 10.1097/00041552-199809000-00008]
24 Russo C, Olivieri O, Girelli D, Faccini G, Zenari ML, Lombardi
S, Corrocher R. Anti-oxidant status and lipid peroxidation
in patients with essential hypertension. J Hypertens 1998;
16: 1267-1271 [PMID: 9746113 DOI: 10.1097/00004872-199816
090-00007]
25 Tse WY, Maxwell SR, Thomason H, Blann A, Thorpe GH,
Waite M, Holder R. Antioxidant status in controlled and
uncontrolled hypertension and its relationship to endothelial
damage. J Hum Hypertens 1994; 8: 843-849 [PMID: 7853328]
26 Mansego ML, Solar Gde M, Alonso MP, Mart�nez F, S�ez
GT, Escudero JC, Red�n J, Chaves FJ. Polymorphisms of antioxidant
enzymes, blood pressure and risk of hypertension.
J Hypertens 2011; 29: 492-500 [PMID: 21178785 DOI: 10.1097/
HJH.0b013e328341f1b2]
27 Galley HF, Thornton J, Howdle PD, Walker BE, Webster
NR. Combination oral antioxidant supplementation reduces
blood pressure. Clin Sci (Lond) 1997; 92: 361-365 [PMID:
9176034]
28 Dhalla NS, Temsah RM, Netticadan T. Role of oxidative
stress in cardiovascular diseases. J Hypertens 2000; 18: 655-673
[PMID: 10872549 DOI: 10.1097/00004872-200018060-00002]
29 Saez G, Tormos MC, Giner V, Lorano JV, Chaves FJ, Armengod
ME, Redon J. P-653: Oxidative stress and enzymatic
antioxidant mechanisms in essential hypertension. Am J Hypertens
2001; 14: 248A [DOI: 10.1016/S0895-7061(01)01983-5]
30 Nishihara M, Hirooka Y, Matsukawa R, Kishi T, Sunagawa
K. Oxidative stress in the rostral ventrolateral medulla modulates
excitatory and inhibitory inputs in spontaneously hypertensive
rats. J Hypertens 2012; 30: 97-106 [PMID: 22157590
DOI: 10.1097/HJH.0b013e32834e1df4]
31 Konno S, Hirooka Y, Kishi T, Sunagawa K. Sympathoinhibitory
effects of telmisartan through the reduction of oxidative
stress in the rostral ventrolateral medulla of obesity-induced
hypertensive rats. J Hypertens 2012; 30: 1992-1999 [PMID:
22902874 DOI: 10.1097/HJH.0b013e328357fa98]
32 Ghanem FA, Movahed A. Inflammation in high blood pressure:
a clinician perspective. J Am Soc Hypertens 2007; 1:
113-119 [PMID: 20409841 DOI: 10.1016/j.jash.2007.01.004]
33 Amer MS, Elawam AE, Khater MS, Omar OH, Mabrouk RA,
Taha HM. Association of high-sensitivity C-reactive protein
with carotid artery intima-media thickness in hypertensive
older adults. J Am Soc Hypertens 2011; 5: 395-400 [PMID:
21524639]
34 Vongpatanasin W, Thomas GD, Schwartz R, Cassis LA,
Osborne-Lawrence S, Hahner L, Gibson LL, Black S, Samols
D, Shaul PW. C-reactive protein causes downregulation of
vascular angiotensin subtype 2 receptors and systolic hypertension
in mice. Circulation 2007; 115: 1020-1028 [PMID:
17283257 DOI: 10.1161/CIRCULATIONAHA.106.664854]
35 Razzouk L, Muntner P, Bansilal S, Kini AS, Aneja A, Mozes
J, Ivan O, Jakkula M, Sharma S, Farkouh ME. C-reactive
protein predicts long-term mortality independently of lowdensity
lipoprotein cholesterol in patients undergoing percutaneous coronary intervention. Am Heart J 2009; 158: 277-283 [PMID: 19619706 DOI: 10.1016/j.ahj.2009.05.026]
36 Kvakan H, Luft FC, Muller DN. Role of the immune system
in hypertensive target organ damage. Trends Cardiovasc Med
2009; 19: 242-246 [PMID: 20382349 DOI: 10.1016/�j.�tcm.2010.02.
004]
37 Rodr�guez-Iturbe B, Franco M, Tapia E, Quiroz Y, Johnson
RJ. Renal inflammation, autoimmunity and salt-sensitive hypertension.
Clin Exp Pharmacol Physiol 2012; 39: 96-103 [PMID:
21251049 DOI: 10.1111/j.1440-1681.2011.05482.x]
38 Tian N, Penman AD, Mawson AR, Manning RD, Flessner
MF. Association between circulating specific leukocyte types
and blood pressure: the atherosclerosis risk in communities
(ARIC) study. J Am Soc Hypertens 2010; 4: 272-283 [PMID:
20980213 DOI: 10.1016/j.jash.2010.09.005]
39 Muller DN, Kvakan H, Luft FC. Immune-related effects in
hypertension and target-organ damage. Curr Opin Nephrol
Hypertens 2011; 20: 113-117 [PMID: 21245763 DOI: 10.1097/
MNH.0b013e3283436f88]
40 Marketou ME, Kontaraki JE, Zacharis EA, Kochiadakis GE,
Giaouzaki A, Chlouverakis G, Vardas PE. TLR2 and TLR4
gene expression in peripheral monocytes in nondiabetic
hypertensive patients: the effect of intensive blood pressurelowering.
J Clin Hypertens (Greenwich) 2012; 14: 330-335
[PMID: 22533660 DOI: 10.1111/j.1751-7176.2012.00620.x]
41 Luft FC. Neural regulation of the immune system modulates
hypertension-induced target-organ damage. J Am Soc Hypertens
2012; 6: 23-26 [PMID: 22047671 DOI: 10.1016/�j.�jash.2011.
09.006]
42 Herrada AA, Campino C, Amador CA, Michea LF, Fardella
CE, Kalergis AM. Aldosterone as a modulator of immunity:
implications in the organ damage. J Hypertens 2011; 29:
1684-1692 [PMID: 21826023 DOI: 10.1097/�HJH.0b013e32834a
4c75]
43 Colussi G, Catena C, Sechi LA. Spironolactone, eplerenone
and the new aldosterone blockers in endocrine and primary
hypertension. J Hypertens 2013; 31: 3-15 [PMID: 23011526
DOI: 10.1097/HJH.0b013e3283599b6a]
44 Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP,
Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM,
Lin PH, Karanja N. A clinical trial of the effects of dietary
patterns on blood pressure. DASH Collaborative Research
Group. N Engl J Med 1997; 336: 1117-1124 [PMID: 9099655]
45 Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA,
Harsha D, Obarzanek E, Conlin PR, Miller ER, SimonsMorton
DG, Karanja N, Lin PH. Effects on blood pressure
of reduced dietary sodium and the Dietary Approaches to
Stop Hypertension (DASH) diet. DASH-Sodium Collaborative
Research Group. N Engl J Med 2001; 344: 3-10 [PMID:
11136953]
46 Sun B, Williams JS, Svetkey LP, Kolatkar NS, Conlin PR.
Beta2-adrenergic receptor genotype affects the reninangiotensin-aldosterone
system response to the Dietary Approaches
to Stop Hypertension (DASH) dietary pattern. Am
J Clin Nutr 2010; 92: 444-449 [PMID: 20519561 DOI: 10.3945/
ajcn.2009.28924]
47 Chen Q, Turban S, Miller ER, Appel LJ. The effects of dietary
patterns on plasma renin activity: results from the Dietary
Approaches to Stop Hypertension trial. J Hum Hypertens
2012; 26: 664-669 [PMID: 22048714 DOI: 10.1038/jhh.2011.87]
48 Al-Solaiman Y, Jesri A, Zhao Y, Morrow JD, Egan BM. LowSodium
DASH reduces oxidative stress and improves vascular
function in salt-sensitive humans. J Hum Hypertens 2009;
23: 826-835 [PMID: 19404315 DOI: 10.1038/jhh.2009.32]
49 Lin PH, Allen JD, Li YJ, Yu M, Lien LF, Svetkey LP. Blood
Pressure-Lowering Mechanisms of the DASH Dietary Pattern.
J Nutr Metab 2012; 2012: 472396 [PMID: 22496969 DOI:
10.1155/2012/472396]
50 Kotchen TA, McCarron DA. Dietary electrolytes and blood
pressure: a statement for healthcare professionals from the
American Heart Association Nutrition Committee. Circulation
1998; 98: 613-617 [PMID: 9714124]
51 Cutler JA, Follmann D, Allender PS. Randomized trials of
sodium reduction: an overview. Am J Clin Nutr 1997; 65:
643S-651S [PMID: 9022560]
52 Svetkey LP, Sacks FM, Obarzanek E, Vollmer WM, Appel
LJ, Lin PH, Karanja NM, Harsha DW, Bray GA, Aickin M,
Proschan MA, Windhauser MM, Swain JF, McCarron PB,
Rhodes DG, Laws RL. The DASH Diet, Sodium Intake and
Blood Pressure Trial (DASH-sodium): rationale and design.
DASH-Sodium Collaborative Research Group. J Am Diet Assoc
1999; 99: S96-104 [PMID: 10450301 DOI: 10.1016/S0002-
8223(99)00423-X]
53 Kawada T, Suzuki S. Attention of salt awareness to prevent
hypertension in the young. J Clin Hypertens (Greenwich)
2011; 13: 933-934 [PMID: 22142354 DOI: 10.1111/�j.1751-7176.
2011.00555.x]
54 Weinberger MH. Salt sensitivity of blood pressure in humans.
Hypertension 1996; 27: 481-490 [PMID: 8613190 DOI:
10.1161/01.HYP.27.3.481]
55 Morimoto A, Uzu T, Fujii T, Nishimura M, Kuroda S, Nakamura
S, Inenaga T, Kimura G. Sodium sensitivity and cardiovascular
events in patients with essential hypertension.
Lancet 1997; 350: 1734-1737 [PMID: 9413464]
56 Tomonari T, Fukuda M, Miura T, Mizuno M, Wakamatsu
TY, Ichikawa T, Miyagi S, Shirasawa Y, Ito A, Yoshida A,
Omori T, Kimura G. Is salt intake an independent risk factor
of stroke mortality? Demographic analysis by regions in
Japan. J Am Soc Hypertens 2011; 5: 456-462 [PMID: 21890446
DOI: 10.1016/j.jash.2011.07.004]
57 Kanbay M, Chen Y, Solak Y, Sanders PW. Mechanisms and
consequences of salt sensitivity and dietary salt intake. Curr
Opin Nephrol Hypertens 2011; 20: 37-43 [PMID: 21088577 DOI:
10.1097/MNH.0b013e32834122f1]
58 Dubach JM, Das S, Rosenzweig A, Clark HA. Visualizing sodium
dynamics in isolated cardiomyocytes using fluorescent
nanosensors. Proc Natl Acad Sci USA 2009; 106: 16145-16150
[PMID: 19805271 DOI: 10.1073/pnas.0905909106]
59 Oberleithner H, Callies C, Kusche-Vihrog K, Schillers H,
Shahin V, Riethm�ller C, Macgregor GA, de Wardener HE.
Potassium softens vascular endothelium and increases nitric
oxide release. Proc Natl Acad Sci USA 2009; 106: 2829-2834
[PMID: 19202069 DOI: 10.1073/pnas.0813069106]
60 Oberleithner H, Riethm�ller C, Schillers H, MacGregor GA,
de Wardener HE, Hausberg M. Plasma sodium stiffens vascular
endothelium and reduces nitric oxide release. Proc Natl
Acad Sci USA 2007; 104: 16281-16286 [PMID: 17911245 DOI:
10.1073/pnas.0707791104]
61 Fels J, Oberleithner H, Kusche-Vihrog K. M�nage � trois: aldosterone,
sodium and nitric oxide in vascular endothelium.
Biochim Biophys Acta 2010; 1802: 1193-1202 [PMID: 20302930
DOI: 10.1016/j.bbadis.2010.03.006]
62 Oberleithner H, Kusche-Vihrog K, Schillers H. Endothelial
cells as vascular salt sensors. Kidney Int 2010; 77: 490-494
[PMID: 20054292 DOI: 10.1038/ki.2009.490]
63 Kusche-Vihrog K, Callies C, Fels J, Oberleithner H. The
epithelial sodium channel (ENaC): Mediator of the aldosterone
response in the vascular endothelium? Steroids
2010; 75: 544-549 [PMID: 19778545 DOI: 10.1016/�j.steroids.2009.09.003]
64 Fels J, Callies C, Kusche-Vihrog K, Oberleithner H. Nitric
oxide release follows endothelial nanomechanics and not
vice versa. Pflugers Arch 2010; 460: 915-923 [PMID: 20809399
DOI: 10.1007/s00424-010-0871-8]
65 Callies C, Fels J, Liashkovich I, Kliche K, Jeggle P, KuscheVihrog
K, Oberleithner H. Membrane potential depolarization
decreases the stiffness of vascular endothelial cells. J
Cell Sci 2011; 124: 1936-1942 [PMID: 21558418 DOI: 10.1242/
jcs.084657]
66 Kusche-Vihrog K, Urbanova K, Blanqu� A, Wilhelmi M,
Schillers H, Kliche K, Pavenst�dt H, Brand E, Oberleithner
H. C-reactive protein makes human endothelium stiff and tight. Hypertension 2011; 57: 231-237 [PMID: 21149827 DOI: 10.1161/HYPERTENSIONAHA.110.163444]
67 Foulquier S, Dupuis F, Perrin-Sarrado C, Maguin Gat� K,
Merhi-Soussi F, Liminana P, Kwan YW, Capdeville-Atkinson
C, Lartaud I, Atkinson J. High salt intake abolishes AT(2)-
mediated vasodilation of pial arterioles in rats. J Hypertens
2011; 29: 1392-1399 [PMID: 21519278 DOI: 10.1097/�HJH.0b01
3e328347050e]
68 Kusche-Vihrog K, Oberleithner H. An emerging concept of
vascular salt sensitivity. F1000 Biol Rep 2012; 4: 20 [PMID:
23112808 DOI: 10.3410/B4-20]
69 Popov S, Silveira A, W�gs�ter D, Takemori H, Oguro R,
Matsumoto S, Sugimoto K, Kamide K, Hirose T, Satoh M,
Metoki H, Kikuya M, Ohkubo T, Katsuya T, Rakugi H, Imai
Y, Sanchez F, Leosdottir M, Syv�nen AC, Hamsten A, Melander
O, Bertorello AM. Salt-inducible kinase 1 influences
Na(+),K(+)-ATPase activity in vascular smooth muscle cells
and associates with variations in blood pressure. J Hypertens
2011; 29: 2395-2403 [PMID: 22045124 DOI: 10.1097/�HJH.0b01
3e32834d3d55]
70 Houston MC. Nutraceuticals, vitamins, antioxidants, and
minerals in the prevention and treatment of hypertension.
Prog Cardiovasc Dis 2005; 47: 396-449 [PMID: 16115519 DOI:
10.1016/j.pcad.2005.01.004]
71 Houston MC. Nutrition and nutraceutical supplements in
the treatment of hypertension. Expert Rev Cardiovasc Ther
2010; 8: 821-833 [PMID: 20528640 DOI: 10.1586/erc.10.63]
72 Messerli FH, Schmieder RE, Weir MR. Salt. A perpetrator of
hypertensive target organ disease? Arch Intern Med 1997; 157:
2449-2452 [PMID: 9385295 DOI: 10.1001/archinte.1997.00440
420077006]
73 Oliver WJ, Cohen EL, Neel JV. Blood pressure, sodium intake,
and sodium related hormones in the Yanomamo Indians,
a �no-salt� culture. Circulation 1975; 52: 146-151 [PMID:
1132118 DOI: 10.1161/01.CIR.52.1.146]
74 Kawasaki T, Delea CS, Bartter FC, Smith H. The effect of
high-sodium and low-sodium intakes on blood pressure and
other related variables in human subjects with idiopathic hypertension.
Am J Med 1978; 64: 193-198 [PMID: 629267 DOI:
10.1016/0002-9343(78)90045-1]
75 Toda N, Arakawa K. Salt-induced hemodynamic regulation
mediated by nitric oxide. J Hypertens 2011; 29: 415-424 [PMID:
21150639 DOI: 10.1097/HJH.0b013e328341d19e]
76 Whelton PK, He J. Potassium in preventing and treating
high blood pressure. Semin Nephrol 1999; 19: 494-499 [PMID:
10511389]
77 Gu D, He J, Wu X, Duan X, Whelton PK. Effect of potassium
supplementation on blood pressure in Chinese: a randomized,
placebo-controlled trial. J Hypertens 2001; 19: 1325-1331
[PMID: 11446724 DOI: 10.1097/00004872-200107000-00019]
78 He J, Gu D, Kelly TN, Hixson JE, Rao DC, Jaquish CE, Chen
J, Zhao Q, Gu C, Huang J, Shimmin LC, Chen JC, Mu J, Ji X,
Liu DP, Whelton PK. Genetic variants in the renin-angiotensin-aldosterone
system and blood pressure responses to
potassium intake. J Hypertens 2011; 29: 1719-1730 [PMID:
21799445 DOI: 10.1097/HJH.0b013e32834a4d1f]
79 O�Donnell MJ, Yusuf S, Mente A, Gao P, Mann JF, Teo K,
McQueen M, Sleight P, Sharma AM, Dans A, Probstfield J,
Schmieder RE. Urinary sodium and potassium excretion and
risk of cardiovascular events. JAMA 2011; 306: 2229-2238
[PMID: 22110105 DOI: 10.1001/jama.2011.1729]
80 Widman L, Wester PO, Stegmayr BK, Wirell M. The dosedependent
reduction in blood pressure through administration
of magnesium. A double blind placebo controlled crossover
study. Am J Hypertens 1993; 6: 41-45 [PMID: 8427660]
81 Laurant P, Touyz RM. Physiological and pathophysiological
role of magnesium in the cardiovascular system: implications
in hypertension. J Hypertens 2000; 18: 1177-1191 [PMID:
10994748 DOI: 10.1097/00004872-200018090-00003]
82 Houston M. The role of magnesium in hypertension and
cardiovascular disease. J Clin Hypertens (Greenwich) 2011;
13: 843-847 [PMID: 22051430 DOI: 10.1111/�j.1751-7176.2011.0
0538.x]
83 Rosanoff A, Weaver CM, Rude RK. Suboptimal magnesium
status in the United States: are the health consequences underestimated?
Nutr Rev 2012; 70: 153-164 [PMID: 22364157
DOI: 10.1111/j.1753-4887.2011.00465.x]
84 Song Y, Liu S. Magnesium for cardiovascular health: time
for intervention. Am J Clin Nutr 2012; 95: 269-270 [PMID:
22218155 DOI: 10.3945/ajcn.111.031104]
85 Kupetsky-Rincon EA, Uitto J. Magnesium: novel applications
in cardiovascular disease–a review of the literature.
Ann Nutr Metab 2012; 61: 102-110 [PMID: 22907037 DOI:
10.1159/000339380]
86 Cunha AR, Umbelino B, Correia ML, Neves MF. Magnesium
and vascular changes in hypertension. Int J Hypertens 2012;
2012: 754250 [PMID: 22518291 DOI: 10.1155/2012/754250]
87 Kass L, Weekes J, Carpenter L. Effect of magnesium supplementation
on blood pressure: a meta-analysis. Eur J Clin Nutr
2012; 66: 411-418 [PMID: 22318649 DOI: 10.1038/ejcn.2012.4]
88 McCarron DA. Role of adequate dietary calcium intake in
the prevention and management of salt-sensitive hypertension.
Am J Clin Nutr 1997; 65: 712S-716S [PMID: 9022571]
89 Resnick LM. Calcium metabolism in hypertension and allied
metabolic disorders. Diabetes Care 1991; 14: 505-520 [PMID:
1864222 DOI: 10.2337/diacare.14.6.505]
90 Garc�a Zozaya JL, Padilla Viloria M. [Alterations of calcium,
magnesium, and zinc in essential hypertension: their relation
to the renin-angiotensin-aldosterone system]. Invest Clin
1997; 38 Suppl 2: 27-40 [PMID: 9471228]
91 Carpenter WE, Lam D, Toney GM, Weintraub NL, Qin Z.
Zinc, copper, and blood pressure: Human population studies.
Med Sci Monit 2013; 19: 1-8 [PMID: 23291705 DOI: 10.12659/
MSM.883708]
92 Shahbaz AU, Sun Y, Bhattacharya SK, Ahokas RA, Gerling
IC, McGee JE, Weber KT. Fibrosis in hypertensive heart disease:
molecular pathways and cardioprotective strategies. J
Hypertens 2010; 28 Suppl 1: S25-S32 [PMID: 20823713 DOI:
10.1097/01.hjh.0000388491.35836.d2]
93 Bergomi M, Rovesti S, Vinceti M, Vivoli R, Caselgrandi E,
Vivoli G. Zinc and copper status and blood pressure. J Trace
Elem Med Biol 1997; 11: 166-169 [PMID: 9442464 DOI: 10.1016/
S0946-672X(97)80047-8]
94 Stamler J, Elliott P, Kesteloot H, Nichols R, Claeys G, Dyer
AR, Stamler R. Inverse relation of dietary protein markers
with blood pressure. Findings for 10,020 men and women in
the INTERSALT Study. INTERSALT Cooperative Research
Group. INTERnational study of SALT and blood pressure.
Circulation 1996; 94: 1629-1634 [PMID: 8840854 DOI:
10.1161/01.CIR.94.7.1629]
95 Altorf-van der Kuil W, Engberink MF, Brink EJ, van Baak
MA, Bakker SJ, Navis G, van �t Veer P, Geleijnse JM. Dietary
protein and blood pressure: a systematic review. PLoS One
2010; 5: e12102 [PMID: 20711407 DOI: 10.1371/journal.
pone.0012102]
96 Jenkins DJ, Kendall CW, Faulkner DA, Kemp T, Marchie
A, Nguyen TH, Wong JM, de Souza R, Emam A, Vidgen E,
Trautwein EA, Lapsley KG, Josse RG, Leiter LA, Singer W.
Long-term effects of a plant-based dietary portfolio of cholesterol-lowering
foods on blood pressure. Eur J Clin Nutr 2008;
62: 781-788 [PMID: 17457340 DOI: 10.1038/sj.ejcn.1602768]
97 Elliott P, Dennis B, Dyer AR. Relation of dietary protein
(total, vegetable, animal) to blood pressure: INTERMAP
epidemiologic study. Presented at the 18th Scientific Meeting
of the International Society of Hypertension, Chicago, IL,
August 20-24, 2000
98 Rebholz CM, Friedman EE, Powers LJ, Arroyave WD, He J,
Kelly TN. Dietary protein intake and blood pressure: a metaanalysis
of randomized controlled trials. Am J Epidemiol 2012;
176 Suppl 7: S27-S43 [PMID: 23035142 DOI: 10.1093/aje/
kws245]
99 Larsson SC, Virtamo J, Wolk A. Dietary protein intake and�risk of stroke in women. Atherosclerosis 2012; 224: 247-251 [PMID: 22854187]
100 He J, Wofford MR, Reynolds K, Chen J, Chen CS, Myers L,
Minor DL, Elmer PJ, Jones DW, Whelton PK. Effect of dietary
protein supplementation on blood pressure: a randomized,
controlled trial. Circulation 2011; 124: 589-595 [PMID:
21768541 DOI: 10.1161/CIRCULATIONAHA.110.009159]
101 Teunissen-Beekman KF, Dopheide J, Geleijnse JM, Bakker
SJ, Brink EJ, de Leeuw PW, van Baak MA. Protein supplementation
lowers blood pressure in overweight adults: effect
of dietary proteins on blood pressure (PROPRES), a randomized
trial. Am J Clin Nutr 2012; 95: 966-971 [PMID: 22357725
DOI: 10.3945/ajcn.111.029116]
102 FitzGerald RJ, Murray BA, Walsh DJ. Hypotensive peptides
from milk proteins. J Nutr 2004; 134: 980S-988S [PMID:
15051858]
103 Pins JJ, Keenan JM. Effects of whey peptides on cardiovascular
disease risk factors. J Clin Hypertens (Greenwich) 2006; 8:
775-782 [PMID: 17086017 DOI: 10.1111/�j.1524-6175.2006.0566
7.x]
104 Aihara K, Kajimoto O, Hirata H, Takahashi R, Nakamura
Y. Effect of powdered fermented milk with Lactobacillus
helveticus on subjects with high-normal blood pressure or
mild hypertension. J Am Coll Nutr 2005; 24: 257-265 [PMID:
16093403 DOI: 10.1080/07315724.2005.10719473]
105 Germino FW, Neutel J, Nonaka M, Hendler SS. The impact of
lactotripeptides on blood pressure response in stage 1 and stage
2 hypertensives. J Clin Hypertens (Greenwich) 2010; 12: 153-159
[PMID: 20433527 DOI: 10.1111/�j.1751-7176.2009.00250.x]
106 Geleijnse JM, Engberink MF. Lactopeptides and human
blood pressure. Curr Opin Lipidol 2010; 21: 58-63 [PMID:
19884823 DOI: 10.1097/MOL.0b013e3283333813]
107 Cicero AF, Aubin F, Azais-Braesco V, Borghi C. Do the lactotripeptides
isoleucine-proline-proline and valine-prolineproline
reduce systolic blood pressure in European subjects?
A meta-analysis of randomized controlled trials. Am J Hypertens
2013; 26: 442-449 [PMID: 23382495 DOI: 10.1093/ajh/
hps044]
108 Usinger L, Reimer C, Ibsen H. Fermented milk for hypertension.
Cochrane Database Syst Rev 2012; 4: CD008118 [PMID:
22513955 DOI: 10.1002/14651858.CD008118.pub2]
109 Ricci-Cabello I, Herrera MO, Artacho R. Possible role of
milk-derived bioactive peptides in the treatment and prevention
of metabolic syndrome. Nutr Rev 2012; 70: 241-255
[PMID: 22458697 DOI: 10.1111/j.1753-4887.2011.00448.x]
110 Jauhiainen T, Niittynen L, Ore�i? M, J�rvenp�� S, Hiltunen
TP, R�nnback M, Vapaatalo H, Korpela R. Effects of longterm
intake of lactotripeptides on cardiovascular risk factors
in hypertensive subjects. Eur J Clin Nutr 2012; 66: 843-849
[PMID: 22617279 DOI: 10.1038/ejcn.2012.44]
111 Pins JJ, Keenan JM. The antihypertensive effects of a hydrolyzed
whey protein isolate supplement. Cardiovasc Drugs
Ther 2002; 16: 68
112 Pal S, Radavelli-Bagatini S. The effects of whey protein
on cardiometabolic risk factors. Obes Rev 2013; 14: 324-343
[PMID: 23167434 DOI: 10.1111/obr.12005]
113 Zhu CF, Li GZ, Peng HB, Zhang F, Chen Y, Li Y. Therapeutic
effects of marine collagen peptides on Chinese patients
with type 2 diabetes mellitus and primary hypertension. Am
J Med Sci 2010; 340: 360-366 [PMID: 20739874 DOI: 10.1097/
MAJ.0b013e3181edfcf2]
114 De Leo F, Panarese S, Gallerani R, Ceci LR. Angiotensin converting
enzyme (ACE) inhibitory peptides: production and
implementation of functional food. Curr Pharm Des 2009; 15:
3622-3643 [PMID: 19925416 DOI: 10.2174/138161209789271834]
115 Lordan S, Ross RP, Stanton C. Marine bioactives as functional
food ingredients: potential to reduce the incidence
of chronic diseases. Mar Drugs 2011; 9: 1056-1100 [PMID:
21747748 DOI: 10.3390/md9061056]
116 Fujita H, Yoshikawa M. LKPNM: a prodrug-type ACEinhibitory
peptide derived from fish protein. Immunopharmacology
1999; 44: 123-127 [PMID: 10604535 DOI: 10.1016/�S0162
-3109(99)00118-6]
117 Kawasaki T, Seki E, Osajima K, Yoshida M, Asada K, Matsui
T, Osajima Y. Antihypertensive effect of valyl-tyrosine, a
short chain peptide derived from sardine muscle hydrolyzate,
on mild hypertensive subjects. J Hum Hypertens 2000;
14: 519-523 [PMID: 10962520 DOI: 10.1038/sj.jhh.1001065]
118 Kawasaki T, Jun CJ, Fukushima Y, Kegai K, Seki E, Osajima
K, Itoh K, Matsui T, Matsumoto K. [Antihypertensive effect
and safety evaluation of vegetable drink with peptides
derived from sardine protein hydrolysates on mild hypertensive,
high-normal and normal blood pressure subjects].
Fukuoka Igaku Zasshi 2002; 93: 208-218 [PMID: 12471719]
119 Yang G, Shu XO, Jin F, Zhang X, Li HL, Li Q, Gao YT, Zheng
W. Longitudinal study of soy food intake and blood pressure
among middle-aged and elderly Chinese women. Am J
Clin Nutr 2005; 81: 1012-1017 [PMID: 15883423]
120 Dong JY, Tong X, Wu ZW, Xun PC, He K, Qin LQ. Effect
of soya protein on blood pressure: a meta-analysis of randomised
controlled trials. Br J Nutr 2011; 106: 317-326 [PMID:
21342608 DOI: 10.1017/S0007114511000262]
121 Teede HJ, Giannopoulos D, Dalais FS, Hodgson J, McGrath
BP. Randomised, controlled, cross-over trial of soy protein
with isoflavones on blood pressure and arterial function in
hypertensive subjects. J Am Coll Nutr 2006; 25: 533-540 [PMID:
17229901 DOI: 10.1080/07315724.2006.10719569]
122 Welty FK, Lee KS, Lew NS, Zhou JR. Effect of soy nuts on
blood pressure and lipid levels in hypertensive, prehypertensive,
and normotensive postmenopausal women. Arch
Intern Med 2007; 167: 1060-1067 [PMID: 17533209 DOI:
10.1001/archinte.167.10.1060]
123 Rosero Arenas MA, Rosero Arenas E, Portaceli Armi�ana
MA, Garc�a Garc�a MA. [Usefulness of phyto-oestrogens in
reduction of blood pressure. Systematic review and metaanalysis].
Aten Primaria 2008; 40: 177-186 [PMID: 18405582]
124 Nasca MM, Zhou JR, Welty FK. Effect of soy nuts on adhesion
molecules and markers of inflammation in hypertensive
and normotensive postmenopausal women. Am
J Cardiol 2008; 102: 84-86 [PMID: 18572041 DOI: 10.1016/
j.amjcard.2008.02.100]
125 He J, Gu D, Wu X, Chen J, Duan X, Chen J, Whelton PK.
Effect of soybean protein on blood pressure: a randomized,
controlled trial. Ann Intern Med 2005; 143: 1-9 [PMID:
15998749 DOI: 10.7326/0003-4819-143-1-200507050-00004]
126 Hasler CM, Kundrat S, Wool D. Functional foods and cardiovascular
disease. Curr Atheroscler Rep 2000; 2: 467-475
[PMID: 11122780 DOI: 10.1007/s11883-000-0045-9]
127 Tikkanen MJ, Adlercreutz H. Dietary soy-derived isoflavone
phytoestrogens. Could they have a role in coronary
heart disease prevention? Biochem Pharmacol 2000; 60: 1-5
[PMID: 10807939]
128 Begg DP, Sinclair AJ, Stahl LA, Garg ML, Jois M, Weisinger
RS. Dietary protein level interacts with omega-3 polyunsaturated
fatty acid deficiency to induce hypertension. Am J
Hypertens 2010; 23: 125-128 [PMID: 19893499 DOI: 10.1038/
ajh.2009.198]
129 Vallance P, Leone A, Calver A, Collier J, Moncada S. Endogenous
dimethylarginine as an inhibitor of nitric oxide
synthesis. J Cardiovasc Pharmacol 1992; 20 Suppl 12: S60-S62
[PMID: 1282988 DOI: 10.1097/00005344-199204002-00018]
130 Sonmez A, Celebi G, Erdem G, Tapan S, Genc H, Tasci I,
Ercin CN, Dogru T, Kilic S, Uckaya G, Yilmaz MI, Erbil MK,
Kutlu M. Plasma apelin and ADMA Levels in patients with
essential hypertension. Clin Exp Hypertens 2010; 32: 179-183
[PMID: 20504125 DOI: 10.3109/10641960903254505]
131 Michell DL, Andrews KL, Chin-Dusting JP. Endothelial
dysfunction in hypertension: the role of arginase. Front Biosci
(Schol Ed) 2011; 3: 946-960 [PMID: 21622244]
132 Rajapakse NW, Mattson DL. Role of L-arginine in nitric oxide
production in health and hypertension. Clin Exp Pharmacol
Physiol 2009; 36: 249-255 [PMID: 19076168 DOI: 10.1111/j.1440-1681.2008.05123.x]
133 Tsioufis C, Dimitriadis K, Andrikou E, Thomopoulos C,
Tsiachris D, Stefanadi E, Mihas C, Miliou A, Papademetriou
V, Stefanadis C. ADMA, C-reactive protein, and albuminuria
in untreated essential hypertension: a cross-sectional study.
Am J Kidney Dis 2010; 55: 1050-1059 [PMID: 20189274 DOI:
10.1053/j.ajkd.2009.11.024]
134 Rajapakse NW, Mattson DL. Role of cellular L-arginine
uptake and nitric oxide production on renal blood flow and
arterial pressure regulation. Curr Opin Nephrol Hypertens
2013; 22: 45-50 [PMID: 23095292 DOI: 10.1097/�MNH.0b013e
32835a6ff7]
135 Ruiz-Hurtado G, Delgado C. Nitric oxide pathway in hypertrophied
heart: new therapeutic uses of nitric oxide donors.
J Hypertens 2010; 28 Suppl 1: S56-S61 [PMID: 20823718 DOI:
10.1097/01.hjh.0000388496.66330.b8]
136 Siani A, Pagano E, Iacone R, Iacoviello L, Scopacasa F, Strazzullo
P. Blood pressure and metabolic changes during dietary
L-arginine supplementation in humans. Am J Hypertens
2000; 13: 547-551 [PMID: 10826408 DOI: 10.1016/�S0895-7061(
99)00233-2]
137 Facchinetti F, Saade GR, Neri I, Pizzi C, Longo M, Volpe
A. L-arginine supplementation in patients with gestational
hypertension: a pilot study. Hypertens Pregnancy 2007; 26:
121-130 [PMID: 17454224 DOI: 10.1080/10641950601147994]
138 Neri I, Monari F, Sgarbi L, Berardi A, Masellis G, Facchinetti
F. L-arginine supplementation in women with chronic hypertension:
impact on blood pressure and maternal and neonatal
complications. J Matern Fetal Neonatal Med 2010; 23: 1456-1460
[PMID: 20958228 DOI: 10.3109/14767051003677962]
139 Martina V, Masha A, Gigliardi VR, Brocato L, Manzato E,
Berchio A, Massarenti P, Settanni F, Della Casa L, Bergamini
S, Iannone A. Long-term N-acetylcysteine and L-arginine
administration reduces endothelial activation and systolic
blood pressure in hypertensive patients with type 2 diabetes.
Diabetes Care 2008; 31: 940-944 [PMID: 18268065 DOI:
10.2337/dc07-2251]
140 Ast J, Jablecka A, Bogdanski P, Smolarek I, Krauss H, Chmara
E. Evaluation of the antihypertensive effect of L-arginine
supplementation in patients with mild hypertension assessed
with ambulatory blood pressure monitoring. Med Sci
Monit 2010; 16: CR266-CR271 [PMID: 20424555]
141 Dong JY, Qin LQ, Zhang Z, Zhao Y, Wang J, Arigoni F,
Zhang W. Effect of oral L-arginine supplementation on
blood pressure: a meta-analysis of randomized, doubleblind,
placebo-controlled trials. Am Heart J 2011; 162: 959-965
[PMID: 22137067 DOI: 10.1016/j.ahj.2011.09.012]
142 Miller GD, Marsh AP, Dove RW, Beavers D, Presley T,
Helms C, Bechtold E, King SB, Kim-Shapiro D. Plasma nitrate
and nitrite are increased by a high-nitrate supplement but
not by high-nitrate foods in older adults. Nutr Res 2012; 32:
160-168 [PMID: 22464802 DOI: 10.1016/j.nutres.2012.02.002]
143 Schulman SP, Becker LC, Kass DA, Champion HC, Terrin
ML, Forman S, Ernst KV, Kelemen MD, Townsend SN,
Capriotti A, Hare JM, Gerstenblith G. L-arginine therapy in
acute myocardial infarction: the Vascular Interaction With
Age in Myocardial Infarction (VINTAGE MI) randomized
clinical trial. JAMA 2006; 295: 58-64 [PMID: 16391217 DOI:
10.1001/jama.295.1.58]
144 Miguel-Carrasco JL, Monserrat MT, Mate A, V�zquez CM.
Comparative effects of captopril and l-carnitine on blood
pressure and antioxidant enzyme gene expression in the heart
of spontaneously hypertensive rats. Eur J Pharmacol 2010; 632:
65-72 [PMID: 20123095 DOI: 10.1016/�j.ejphar.2010.01.017]
145 Zambrano S, Blanca AJ, Ruiz-Armenta MV, Miguel-Carrasco
JL, Ar�valo M, V�zquez MJ, Mate A, V�zquez CM. L-Carnitine
protects against arterial hypertension-related cardiac
fibrosis through modulation of PPAR-? expression. Biochem
Pharmacol 2013; 85: 937-944 [PMID: 23295156 DOI: 10.1016/
j.bcp.2012.12.021]
146 Vilskersts R, Kuka J, Svalbe B, Cirule H, Liepinsh E, Grinberga
S, Kalvinsh I, Dambrova M. Administration of L-carnitine
and mildronate improves endothelial function and
decreases mortality in hypertensive Dahl rats. Pharmacol Rep
2011; 63: 752-762 [PMID: 21857086]
147 Mate A, Miguel-Carrasco JL, Monserrat MT, V�zquez CM.
Systemic antioxidant properties of L-carnitine in two different
models of arterial hypertension. J Physiol Biochem 2010; 66:
127-136 [PMID: 20506010 DOI: 10.1007/s13105-010-0017-7]
148 Digiesi V, Cantini F, Bisi G, Guarino G, Brodbeck B. L-carnitine
adjuvant therapy in essential hypertension. Clin Ter
1994; 144: 391-395 [PMID: 7924177]
149 Ghidini O, Azzurro M, Vita G, Sartori G. Evaluation of the
therapeutic efficacy of L-carnitine in congestive heart failure.
Int J Clin Pharmacol Ther Toxicol 1988; 26: 217-220 [PMID:
3403101]
150 Digiesi V, Palchetti R, Cantini F. [The benefits of L-carnitine
therapy in essential arterial hypertension with diabetes mellitus
type II]. Minerva Med 1989; 80: 227-231 [PMID: 2654758]
151 Ruggenenti P, Cattaneo D, Loriga G, Ledda F, Motterlini N,
Gherardi G, Orisio S, Remuzzi G. Ameliorating hypertension
and insulin resistance in subjects at increased cardiovascular
risk: effects of acetyl-L-carnitine therapy. Hypertension 2009;
54: 567-574 [PMID: 19620516]
152 Mate A, Miguel-Carrasco JL, V�zquez CM. The therapeutic
prospects of using L-carnitine to manage hypertension-related
organ damage. Drug Discov Today 2010; 15: 484-492 [PMID:
20363359 DOI: 10.1016/j.drudis.2010.03.014]
153 Korkmaz S, Y?ld?z G, K?l?�l? F, Y?lmaz A, Ayd?n H, I�a?as?o?lu
S, Candan F. [Low L-carnitine levels: can it be a cause of
nocturnal blood pressure changes in patients with type 2 diabetes
mellitus?]. Anadolu Kardiyol Derg 2011; 11: 57-63 [PMID:
21220248 DOI: 10.5152/akd.2011.008]
154 Huxtable RJ. Physiological actions of taurine. Physiol Rev
1992; 72: 101-163 [PMID: 1731369]
155 Fujita T, Ando K, Noda H, Ito Y, Sato Y. Effects of increased
adrenomedullary activity and taurine in young patients with
borderline hypertension. Circulation 1987; 75: 525-532 [PMID:
3815764 DOI: 10.1161/01.CIR.75.3.525]
156 Huxtable RJ, Sebring LA. Cardiovascular actions of taurine.
Prog Clin Biol Res 1983; 125: 5-37 [PMID: 6348796]
157 Feng Y, Li J, Yang J, Yang Q, Lv Q, Gao Y, Hu J. Synergistic
effects of taurine and L-arginine on attenuating insulin resistance
hypertension. Adv Exp Med Biol 2013; 775: 427-435
[PMID: 23392951 DOI: 10.1007/978-1-4614-6130-2_32]
158 W�jcik OP, Koenig KL, Zeleniuch-Jacquotte A, Pearte C,
Costa M, Chen Y. Serum taurine and risk of coronary heart
disease: a prospective, nested case-control study. Eur J Nutr
2013; 52: 169-178 [PMID: 22322924 DOI: 10.1007/�s00394-011-
0300-6]
159 Abebe W, Mozaffari MS. Role of taurine in the vasculature:
an overview of experimental and human studies. Am J Cardiovasc
Dis 2011; 1: 293-311 [PMID: 22254206]
160 Yamori Y, Taguchi T, Hamada A, Kunimasa K, Mori H, Mori
M. Taurine in health and diseases: consistent evidence from
experimental and epidemiological studies. J Biomed Sci 2010; 17
Suppl 1: S6 [PMID: 20804626 DOI: 10.1186/1423-0127-17-S1-S6]
161 Yamori Y, Taguchi T, Mori H, Mori M. Low cardiovascular
risks in the middle aged males and females excreting greater
24-hour urinary taurine and magnesium in 41 WHO-CARDIAC
study populations in the world. J Biomed Sci 2010; 17 Suppl
1: S21 [PMID: 20804596 DOI: 10.1186/1423-0127-17-S1-S21]
162 Tanabe Y, Urata H, Kiyonaga A, Ikeda M, Tanaka H, Shindo
M, Arakawa K. Changes in serum concentrations of taurine
and other amino acids in clinical antihypertensive exercise
therapy. Clin Exp Hypertens A 1989; 11: 149-165 [PMID:
2565773]
163 Mori TA, Bao DQ, Burke V, Puddey IB, Beilin LJ. Docosahexaenoic
acid but not eicosapentaenoic acid lowers ambulatory
blood pressure and heart rate in humans. Hypertension
1999; 34: 253-260 [PMID: 10454450 DOI: 10.1161/01.
HYP.34.2.253]
164 B�naa KH, Bjerve KS, Straume B, Gram IT, Thelle D. Effect
of eicosapentaenoic and docosahexaenoic acids on blood
pressure in hypertension. A population-based intervention
trial from the Troms� study. N Engl J Med 1990; 322: 795-801
[PMID: 2137901 DOI: 10.1056/NEJM199003223221202]
165 Mori TA, Burke V, Puddey I, Irish A, Cowpland CA, Beilin
L, Dogra G, Watts GF. The effects of [omega]3 fatty acids
and coenzyme Q10 on blood pressure and heart rate in
chronic kidney disease: a randomized controlled trial. J Hypertens
2009; 27: 1863-1872 [PMID: 19705518 DOI: 10.1097/
HJH.0b013e32832e1bd9]
166 Ueshima H, Stamler J, Elliott P, Chan Q, Brown IJ, Carnethon
MR, Daviglus ML, He K, Moag-Stahlberg A, Rodriguez
BL, Steffen LM, Van Horn L, Yarnell J, Zhou B. Food
omega-3 fatty acid intake of individuals (total, linolenic acid,
long-chain) and their blood pressure: INTERMAP study. Hypertension
2007; 50: 313-319 [PMID: 17548718]
167 Mori TA. Omega-3 fatty acids and hypertension in humans.
Clin Exp Pharmacol Physiol 2006; 33: 842-846 [PMID: 16922818
DOI: 10.1111/j.1440-1681.2006.04451.x]
168 Noreen EE, Brandauer J. The effects of supplemental fish
oil on blood pressure and morning cortisol in normotensive
adults: a pilot study. J Complement Integr Med 2012; 9:
1553-3840 [PMID: 23104856 DOI: 10.1515/1553-3840.1467]
169 Bhise A, Krishnan PV, Aggarwal R, Gaiha M, Bhattacharjee
J. Effect of low-dose omega-3 fatty acids substitution
on blood pressure, hyperinsulinemia and dyslipidemia in
Indians with essential hypertension: A pilot study. Indian J
Clin Biochem 2005; 20: 4-9 [PMID: 23105526 DOI: 10.1007/
BF02867393]
170 Cabo J, Alonso R, Mata P. Omega-3 fatty acids and blood
pressure. Br J Nutr 2012; 107 Suppl 2: S195-S200 [PMID:
22591893 DOI: 10.1017/S0007114512001584]
171 Huang T, Shou T, Cai N, Wahlqvist ML, Li D. Associations
of plasma n-3 polyunsaturated fatty acids with blood pressure
and cardiovascular risk factors among Chinese. Int J
Food Sci Nutr 2012; 63: 667-673 [PMID: 22263527 DOI: 10.310
9/09637486.2011.652076]
172 Sagara M, Njelekela M, Teramoto T, Taguchi T, Mori M,
Armitage L, Birt N, Birt C, Yamori Y. Effects of docosahexaenoic
Acid supplementation on blood pressure, heart rate,
and serum lipids in Scottish men with hypertension and hypercholesterolemia.
Int J Hypertens 2011; 2011: 809198 [PMID:
21423683 DOI: 10.4061/2011/809198]
173 Passfall J, Philipp T, Woermann F, Quass P, Thiede M,
Haller H. Different effects of eicosapentaenoic acid and olive
oil on blood pressure, intracellular free platelet calcium, and
plasma lipids in patients with essential hypertension. Clin
Investig 1993; 71: 628-633 [PMID: 8219660]
174 Liu JC, Conklin SM, Manuck SB, Yao JK, Muldoon MF.
Long-chain omega-3 fatty acids and blood pressure. Am J
Hypertens 2011; 24: 1121-1126 [PMID: 21753804 DOI: 10.1038/
ajh.2011.120]
175 Engler MM, Schambelan M, Engler MB, Ball DL, Goodfriend
TL. Effects of dietary gamma-linolenic acid on blood pressure
and adrenal angiotensin receptors in hypertensive rats.
Proc Soc Exp Biol Med 1998; 218: 234-237 [PMID: 9648942]
176 Chin JP. Marine oils and cardiovascular reactivity. Prostaglandins
Leukot Essent Fatty Acids 1994; 50: 211-222 [PMID:
8066094 DOI: 10.1016/0952-3278(94)90156-2]
177 Saravanan P, Davidson NC, Schmidt EB, Calder PC. Cardiovascular
effects of marine omega-3 fatty acids. Lancet
2010; 376: 540-550 [PMID: 20638121 DOI: 10.1016/S0140-
6736(10)60445-X]
178 Ferrara LA, Raimondi AS, d�Episcopo L, Guida L, Dello
Russo A, Marotta T. Olive oil and reduced need for antihypertensive
medications. Arch Intern Med 2000; 160: 837-842
[PMID: 10737284 DOI: 10.1001/archinte.160.6.837]
179 Alonso A, Ruiz-Gutierrez V, Mart�nez-Gonz�lez MA. Monounsaturated
fatty acids, olive oil and blood pressure: epidemiological,
clinical and experimental evidence. Public Health
Nutr 2006; 9: 251-257 [PMID: 16571180]
180 Ter�s S, Barcel�-Coblijn G, Benet M, Alvarez R, Bressani R,
Halver JE, Escrib� PV. Oleic acid content is responsible for
the reduction in blood pressure induced by olive oil. Proc
Natl Acad Sci USA 2008; 105: 13811-13816 [PMID: 18772370
DOI: 10.1073/pnas.0807500105]
181 Cherif S, Rahal N, Haouala M, Hizaoui B, Dargouth F,
Gueddiche M, Kallel Z, Balansard G, Boukef K. [A clinical
trial of a titrated Olea extract in the treatment of essential
arterial hypertension]. J Pharm Belg 1996; 51: 69-71 [PMID:
8786521]
182 Psaltopoulou T, Naska A, Orfanos P, Trichopoulos D,
Mountokalakis T, Trichopoulou A. Olive oil, the Mediterranean
diet, and arterial blood pressure: the Greek European
Prospective Investigation into Cancer and Nutrition (EPIC)
study. Am J Clin Nutr 2004; 80: 1012-1018 [PMID: 15447913]
183 Alonso A, Mart�nez-Gonz�lez MA. Olive oil consumption
and reduced incidence of hypertension: the SUN study. Lipids
2004; 39: 1233-1238 [PMID: 15736920 DOI: 10.1007/�s11745
-004-1352-x]
184 Perrinjaquet-Moccetti T, Busjahn A, Schmidlin C, Schmidt
A, Bradl B, Aydogan C. Food supplementation with an olive
(Olea europaea L.) leaf extract reduces blood pressure in borderline
hypertensive monozygotic twins. Phytother Res 2008;
22: 1239-1242 [PMID: 18729245 DOI: 10.1002/ptr.2455]
185 Moreno-Luna R, Mu�oz-Hernandez R, Miranda ML, Costa
AF, Jimenez-Jimenez L, Vallejo-Vaz AJ, Muriana FJ, Villar J,
Stiefel P. Olive oil polyphenols decrease blood pressure and
improve endothelial function in young women with mild
hypertension. Am J Hypertens 2012; 25: 1299-1304 [PMID:
22914255 DOI: 10.1038/ajh.2012.128]
186 Thomsen C, Rasmussen OW, Hansen KW, Vesterlund M,
Hermansen K. Comparison of the effects on the diurnal
blood pressure, glucose, and lipid levels of a diet rich in
monounsaturated fatty acids with a diet rich in polyunsaturated
fatty acids in type 2 diabetic subjects. Diabet Med 1995;
12: 600-606 [PMID: 7554782 DOI: 10.1111/j.1464-5491.1995.
tb00549.x]
187 Perona JS, Ca�izares J, Montero E, S�nchez-Dom�nguez JM,
Catal� A, Ruiz-Guti�rrez V. Virgin olive oil reduces blood
pressure in hypertensive elderly subjects. Clin Nutr 2004; 23:
1113-1121 [PMID: 15380903 DOI: 10.1016/j.clnu.2004.02.004]
188 Perona JS, Montero E, S�nchez-Dom�nguez JM, Ca�izares
J, Garcia M, Ruiz-Guti�rrez V. Evaluation of the effect of
dietary virgin olive oil on blood pressure and lipid composition
of serum and low-density lipoprotein in elderly type
2 diabetic subjects. J Agric Food Chem 2009; 57: 11427-11433
[PMID: 19902947 DOI: 10.1021/jf902321x]
189 Susalit E, Agus N, Effendi I, Tjandrawinata RR, Nofiarny
D, Perrinjaquet-Moccetti T, Verbruggen M. Olive (Olea europaea)
leaf extract effective in patients with stage-1 hypertension:
comparison with Captopril. Phytomedicine 2011; 18:
251-258 [PMID: 21036583 DOI: 10.1016/�j.phymed.2010.08.016]
190 L�pez-Miranda J, P�rez-Jim�nez F, Ros E, De Caterina R,
Badim�n L, Covas MI, Escrich E, Ordov�s JM, Soriguer F,
Abi� R, de la Lastra CA, Battino M, Corella D, ChamorroQuir�s
J, Delgado-Lista J, Giugliano D, Esposito K, Estruch
R, Fernandez-Real JM, Gaforio JJ, La Vecchia C, Lairon D,
L�pez-Segura F, Mata P, Men�ndez JA, Muriana FJ, Osada
J, Panagiotakos DB, Paniagua JA, P�rez-Martinez P, Perona
J, Peinado MA, Pineda-Priego M, Poulsen HE, Quiles JL,
Ram�rez-Tortosa MC, Ruano J, Serra-Majem L, Sol� R, Solanas
M, Solfrizzi V, de la Torre-Fornell R, Trichopoulou
A, Uceda M, Villalba-Montoro JM, Villar-Ortiz JR, Visioli
F, Yiannakouris N. Olive oil and health: summary of the II
international conference on olive oil and health consensus
report, Ja�n and C�rdoba (Spain) 2008. Nutr Metab Cardiovasc
Dis 2010; 20: 284-294 [PMID: 20303720 DOI: 10.1016/
j.numecd.2009.12.007]
191 Zhang J, Villacorta L, Chang L, Fan Z, Hamblin M, Zhu T,
Chen CS, Cole MP, Schopfer FJ, Deng CX, Garcia-Barrio MT,�Feng YH, Freeman BA, Chen YE. Nitro-oleic acid inhibits angiotensin II-induced hypertension. Circ Res 2010; 107: 540-548 [PMID: 20558825 DOI: 10.1161/CIRCRESAHA.110.218404]
192 Scheffler A, Rauwald HW, Kampa B, Mann U, Mohr FW,
Dhein S. Olea europaea leaf extract exerts L-type Ca(2+)
channel antagonistic effects. J Ethnopharmacol 2008; 120:
233-240 [PMID: 18790040 DOI: 10.1016/j.jep.2008.08.018]
193 Papamichael CM, Karatzi KN, Papaioannou TG, Karatzis
EN, Katsichti P, Sideris V, Zakopoulos N, Zampelas A,
Lekakis JP. Acute combined effects of olive oil and wine on
pressure wave reflections: another beneficial influence of
the Mediterranean diet antioxidants? J Hypertens 2008; 26:
223-229 [PMID: 18192835 DOI: 10.1097/�HJH.0b013e3282f25b
80]
194 He J, Whelton PK. Effect of dietary fiber and protein intake
on blood pressure: a review of epidemiologic evidence. Clin
Exp Hypertens 1999; 21: 785-796 [PMID: 10423101 DOI: 10.310
9/10641969909061008]
195 Pruijm M, Wuerzer G, Forni V, Bochud M, Pech�re-Bertschi
A, Burnier M. [Nutrition and hypertension: more than table
salt]. Rev Med Suisse 2010; 6: 1715-1716, 1718-1720, [PMID:
21294306]
196 Sherman DL, Keaney JF, Biegelsen ES, Duffy SJ, Coffman
JD, Vita JA. Pharmacological concentrations of ascorbic acid
are required for the beneficial effect on endothelial vasomotor
function in hypertension. Hypertension 2000; 35: 936-941
[PMID: 10775565]
197 Ness AR, Khaw KT, Bingham S, Day NE. Vitamin C status
and blood pressure. J Hypertens 1996; 14: 503-508 [PMID:
8761901]
198 Duffy SJ, Gokce N, Holbrook M, Huang A, Frei B, Keaney
JF, Vita JA. Treatment of hypertension with ascorbic acid.
Lancet 1999; 354: 2048-2049 [PMID: 10636373 DOI: 10.1016/
S0140-6736(99)04410-4]
199 Enstrom JE, Kanim LE, Klein MA. Vitamin C intake and
mortality among a sample of the United States population.
Epidemiology 1992; 3: 194-202 [PMID: 1591317 DOI: 10.1097/0
0001648-199205000-00003]
200 Block G, Jensen CD, Norkus EP, Hudes M, Crawford PB. Vitamin
C in plasma is inversely related to blood pressure and
change in blood pressure during the previous year in young
Black and White women. Nutr J 2008; 7: 35 [PMID: 19091068
DOI: 10.1186/1475-2891-7-35]
201 Hatzitolios A, Iliadis F, Katsiki N, Baltatzi M. Is the antihypertensive
effect of dietary supplements via aldehydes
reduction evidence based? A systematic review. Clin Exp
Hypertens 2008; 30: 628-639 [PMID: 18855266 DOI: 10.1080/1
0641960802443274]
202 Mahajan AS, Babbar R, Kansal N, Agarwal SK, Ray PC. Antihypertensive
and antioxidant action of amlodipine and vitamin
C in patients of essential hypertension. J Clin Biochem Nutr
2007; 40: 141-147 [PMID: 18188416 DOI: 10.3164/�jcbn.40.141]
203 Leclerc PC, Proulx CD, Arguin G, B�langer S, Gobeil F, Escher
E, Leduc R, Guillemette G. Ascorbic acid decreases the binding
affinity of the AT1 receptor for angiotensin II. Am J Hypertens
2008; 21: 67-71 [PMID: 18091746 DOI: 10.1038/�ajh.2007.1]
204 Plantinga Y, Ghiadoni L, Magagna A, Giannarelli C, Franzoni
F, Taddei S, Salvetti A. Supplementation with vitamins
C and E improves arterial stiffness and endothelial
function in essential hypertensive patients. Am J Hypertens
2007; 20: 392-397 [PMID: 17386345 DOI: 10.1016/�j.amjhyper.2006.09.021]
205 Sato K, Dohi Y, Kojima M, Miyagawa K, Takase H, Katada
E, Suzuki S. Effects of ascorbic acid on ambulatory blood
pressure in elderly patients with refractory hypertension.
Arzneimittelforschung 2006; 56: 535-540 [PMID: 16927536]
206 Block G, Mangels AR, Norkus EP, Patterson BH, Levander
OA, Taylor PR. Ascorbic acid status and subsequent diastolic
and systolic blood pressure. Hypertension 2001; 37: 261-267
[PMID: 11230282 DOI: 10.1161/01.HYP.37.2.261]
207 McRae MP. Is vitamin C an effective antihypertensive supplement?
A review and analysis of the literature. J Chiropr
Med 2006; 5: 60-64 [PMID: 19674673 DOI: 10.1016/�S0899-346
7(07)60134-7]
208 Simon JA. Vitamin C and cardiovascular disease: a review. J
Am Coll Nutr 1992; 11: 107-125 [PMID: 1578086]
209 Ness AR, Chee D, Elliott P. Vitamin C and blood pressure-an
overview. J Hum Hypertens 1997; 11: 343-350 [PMID:
9249227 DOI: 10.1038/sj.jhh.1000423]
210 Trout DL. Vitamin C and cardiovascular risk factors. Am J
Clin Nutr 1991; 53: 322S-325S [PMID: 1985405]
211 Fulwood R, Johnson CL, Bryner JD; National Center for
Health Statistics. Hematological and Nutritional Biochemistry
Reference Data for Persons 6 Months-74 Years of Age:
United States, 1976-1980. Washington, DC; US Public Health
Service; 1982 Vital and Health Statistics series 11, No. 232,
DHHS publication No. (PHS) 83-1682
212 Ward NC, Wu JH, Clarke MW, Puddey IB, Burke V, Croft
KD, Hodgson JM. The effect of vitamin E on blood pressure
in individuals with type 2 diabetes: a randomized, doubleblind,
placebo-controlled trial. J Hypertens 2007; 25: 227-234
[PMID: 17143195]
213 Murray ED, Wechter WJ, Kantoci D, Wang WH, Pham T,
Quiggle DD, Gibson KM, Leipold D, Anner BM. Endogenous
natriuretic factors 7: biospecificity of a natriuretic gammatocopherol
metabolite LLU-alpha. J Pharmacol Exp Ther 1997;
282: 657-662 [PMID: 9262327]
214 Gray B, Swick J, Ronnenberg AG. Vitamin E and adiponectin:
proposed mechanism for vitamin E-induced improvement
in insulin sensitivity. Nutr Rev 2011; 69: 155-161 [PMID:
21348879 DOI: 10.1111/j.1753-4887.2011.00377.x]
215 Lind L, H�nni A, Lithell H, Hvarfner A, S�rensen OH,
Ljunghall S. Vitamin D is related to blood pressure and other
cardiovascular risk factors in middle-aged men. Am J Hypertens
1995; 8: 894-901 [PMID: 8541004 DOI: 10.1016/0895-7061
(95)00154-H]
216 Bednarski R, Donderski R, Manitius J. [Role of vitamin D3
in arterial blood pressure control]. Pol Merkur Lekarski 2007;
23: 307-310 [PMID: 18293857]
217 Ngo DT, Sverdlov AL, McNeil JJ, Horowitz JD. Does vitamin
D modulate asymmetric dimethylarginine and C-reactive
protein concentrations? Am J Med 2010; 123: 335-341 [PMID:
20362753 DOI: 10.1016/j.amjmed.2009.09.024]
218 Rosen CJ. Clinical practice. Vitamin D insufficiency. N Engl
J Med 2011; 364: 248-254 [PMID: 21247315 DOI: 10.1056/
NEJMcp1009570]
219 Pittas AG, Chung M, Trikalinos T, Mitri J, Brendel M, Patel K,
Lichtenstein AH, Lau J, Balk EM. Systematic review: Vitamin
D and cardiometabolic outcomes. Ann Intern Med 2010; 152:
307-314 [PMID: 20194237 DOI: 10.7326/0003-4819-152-5-2010
03020-00009]
220 Motiwala SR, Wang TJ. Vitamin D and cardiovascular disease.
Curr Opin Nephrol Hypertens 2011; 20: 345-353 [PMID:
21519252 DOI: 10.1097/MNH.0b013e3283474985]
221 Bhandari SK, Pashayan S, Liu IL, Rasgon SA, Kujubu DA,
Tom TY, Sim JJ. 25-hydroxyvitamin D levels and hypertension
rates. J Clin Hypertens (Greenwich) 2011; 13: 170-177
[PMID: 21366848 DOI: 10.1111/j.1751-7176.2010.00408.x]
222 Kienreich K, Tomaschitz A, Verheyen N, Pieber TR, Pilz S.
Vitamin D and arterial hypertension: treat the deficiency!
Am J Hypertens 2013; 26: 158 [PMID: 23382398 DOI: 10.1093/
ajh/hps058]
223 Tamez H, Kalim S, Thadhani RI. Does vitamin D modulate
blood pressure? Curr Opin Nephrol Hypertens 2013; 22: 204-209
[PMID: 23299053 DOI: 10.1097/MNH.0b013e32835d919b]
224 Wang L, Ma J, Manson JE, Buring JE, Gaziano JM, Sesso HD.
A prospective study of plasma vitamin D metabolites, vitamin
D receptor gene polymorphisms, and risk of hypertension
in men. Eur J Nutr 2013; 52: 1771-1779 [PMID: 23262750
DOI: 10.1007/s00394-012-0480-8]
225 Pfeifer M, Begerow B, Minne HW, Nachtigall D, Hansen C.
Effects of a short-term vitamin D(3) and calcium supplementation on blood pressure and parathyroid hormone levels in elderly women. J Clin Endocrinol Metab 2001; 86: 1633-1637 [PMID: 11297596 DOI: 10.1210/jc.86.4.1633]
226 Keniston R, Enriquez J Sr. Relationship between blood pressure
and Plasma Vitamin B6 Levels in Healthy Middle-Aged
Adults. Ann N Y Acad Sci 1990; 585: 499-501 [DOI: 10.1111/
j.1749-6632.1990.tb28087.x]
227 Aybak M, Sermet A, Ayyildiz MO, Karakil�ik AZ. Effect of
oral pyridoxine hydrochloride supplementation on arterial
blood pressure in patients with essential hypertension. Arzneimittelforschung
1995; 45: 1271-1273 [PMID: 8595083]
228 Paulose CS, Dakshinamurti K, Packer S, Stephens NL. Sympathetic
stimulation and hypertension in the pyridoxinedeficient
adult rat. Hypertension 1988; 11: 387-391 [PMID:
3356457 DOI: 10.1161/01.HYP.11.4.387]
229 Dakshinamurti K, Lal KJ, Ganguly PK. Hypertension, calcium
channel and pyridoxine (vitamin B6). Mol Cell Biochem
1998; 188: 137-148 [PMID: 9823019]
230 Moline J, Bukharovich IF, Wolff MS, Phillips R. Dietary
flavonoids and hypertension: is there a link? Med
Hypotheses 2000; 55: 306-309 [PMID: 11000057 DOI:
10.1054/�mehy.2000.1057]
231 Knekt P, Reunanen A, J�rvinen R, Sepp�nen R, Heli�vaara
M, Aromaa A. Antioxidant vitamin intake and coronary
mortality in a longitudinal population study. Am J Epidemiol
1994; 139: 1180-1189 [PMID: 8209876]
232 Karatzi KN, Papamichael CM, Karatzis EN, Papaioannou
TG, Aznaouridis KA, Katsichti PP, Stamatelopoulos KS,
Zampelas A, Lekakis JP, Mavrikakis ME. Red wine acutely
induces favorable effects on wave reflections and central
pressures in coronary artery disease patients. Am J Hypertens
2005; 18: 1161-1167 [PMID: 16182104 DOI: 10.1016/�j.amjhyper.2005.03.744]
233 Biala A, Tauriainen E, Siltanen A, Shi J, Merasto S, Louhelainen
M, Martonen E, Finckenberg P, Muller DN, Mervaala
E. Resveratrol induces mitochondrial biogenesis and ameliorates
Ang II-induced cardiac remodeling in transgenic rats
harboring human renin and angiotensinogen genes. Blood
Press 2010; 19: 196-205 [PMID: 20429690 DOI: 10.3109/08037
051.2010.481808]
234 Wong RH, Howe PR, Buckley JD, Coates AM, Kunz I,
Berry NM. Acute resveratrol supplementation improves
flow-mediated dilatation in overweight/obese individuals
with mildly elevated blood pressure. Nutr Metab Cardiovasc
Dis 2011; 21: 851-856 [PMID: 20674311 DOI: 10.1016/
j.numecd.2010.03.003]
235 Bhatt SR, Lokhandwala MF, Banday AA. Resveratrol prevents
endothelial nitric oxide synthase uncoupling and
attenuates development of hypertension in spontaneously
hypertensive rats. Eur J Pharmacol 2011; 667: 258-264 [PMID:
21640096 DOI: 10.1016/j.ejphar.2011.05.026]
236 Rivera L, Mor�n R, Zarzuelo A, Galisteo M. Long-term resveratrol
administration reduces metabolic disturbances and
lowers blood pressure in obese Zucker rats. Biochem Pharmacol
2009; 77: 1053-1063 [PMID: 19100718 DOI: 10.1016/
j.bcp.2008.11.027]
237 Paran E, Engelhard YN. Effect of lycopene, an oral natural
antioxidant on blood pressure. J Hypertens 2001; 19: S74. Abstract
P 1.204
238 Engelhard YN, Gazer B, Paran E. Natural antioxidants
from tomato extract reduce blood pressure in patients with
grade-1 hypertension: a double-blind, placebo-controlled
pilot study. Am Heart J 2006; 151: 100 [PMID: 16368299]
239 Paran E, Novack V, Engelhard YN, Hazan-Halevy I. The effects
of natural antioxidants from tomato extract in treated
but uncontrolled hypertensive patients. Cardiovasc Drugs
Ther 2009; 23: 145-151 [PMID: 19052855 DOI: 10.1007/�s10557
-008-6155-2]
240 Ried K, Frank OR, Stocks NP. Dark chocolate or tomato
extract for prehypertension: a randomised controlled trial.
BMC Complement Altern Med 2009; 9: 22 [PMID: 19583878
DOI: 10.1186/1472-6882-9-22]
241 Paran E, Engelhard Y. P-333: Effect of tomato�s lycopene on
blood pressure, serum lipoproteins, plasma homocysteine
and oxidative stress markers in grade I hypertensive patients.
Am J Hypertens 2001; 14: 141A. Abstract P-333 [DOI:
10.1016/S0895-7061(01)01854-4]
242 Xaplanteris P, Vlachopoulos C, Pietri P, Terentes-Printzios D,
Kardara D, Alexopoulos N, Aznaouridis K, Miliou A, Stefanadis
C. Tomato paste supplementation improves endothelial
dynamics and reduces plasma total oxidative status in
healthy subjects. Nutr Res 2012; 32: 390-394 [PMID: 22652379
DOI: 10.1016/j.nutres.2012.03.011]
243 Hosseini S, Lee J, Sepulveda RT, Rohdewaldc P, Watson
RR. A randomized, double-blind, placebo-controlled, prospective
16 week crossover study to determine the role of
pycnogenol in modifying blood pressure in mildly hypertensive
patients. Nutr Res 2001; 21: 1251-1260 [DOI: 10.1016/
S0271-5317(01)00342-6]
244 Zibadi S, Rohdewald PJ, Park D, Watson RR. Reduction of
cardiovascular risk factors in subjects with type 2 diabetes
by Pycnogenol supplementation. Nutr Res 2008; 28: 315-320
[PMID: 19083426 DOI: 10.1016/j.nutres.2008.03.003]
245 Liu X, Wei J, Tan F, Zhou S, W�rthwein G, Rohdewald P.
Pycnogenol, French maritime pine bark extract, improves
endothelial function of hypertensive patients. Life Sci 2004;
74: 855-862 [PMID: 14659974 DOI: 10.1016/j.lfs.2003.07.037]
246 van der Zwan LP, Scheffer PG, Teerlink T. Reduction of
myeloperoxidase activity by melatonin and pycnogenol may
contribute to their blood pressure lowering effect. Hypertension
2010; 56: e34; author reply e35 [PMID: 20696986 DOI:
10.1161/HYPERTENSIONAHA.110.158170]
247 Cesarone MR, Belcaro G, Stuard S, Sch�nlau F, Di Renzo
A, Grossi MG, Dugall M, Cornelli U, Cacchio M, Gizzi G,
Pellegrini L. Kidney flow and function in hypertension: protective
effects of pycnogenol in hypertensive participants–a
controlled study. J Cardiovasc Pharmacol Ther 2010; 15: 41-46
[PMID: 20097689 DOI: 10.1177/1074248409356063]
248 Simons S, Wollersheim H, Thien T. A systematic review on
the influence of trial quality on the effect of garlic on blood
pressure. Neth J Med 2009; 67: 212-219 [PMID: 19749390]
249 Reinhart KM, Coleman CI, Teevan C, Vachhani P, White
CM. Effects of garlic on blood pressure in patients with and
without systolic hypertension: a meta-analysis. Ann Pharmacother
2008; 42: 1766-1771 [PMID: 19017826 DOI: 10.1345/
aph.1L319]
250 Ried K, Frank OR, Stocks NP. Aged garlic extract lowers
blood pressure in patients with treated but uncontrolled
hypertension: a randomised controlled trial. Maturitas
2010; 67: 144-150 [PMID: 20594781 DOI: 10.1016/�j.maturitas.2010.06.001]
251 Suetsuna K, Nakano T. Identification of an antihypertensive
peptide from peptic digest of wakame (Undaria pinnatifida).
J Nutr Biochem 2000; 11: 450-454 [PMID: 11091100 DOI:
10.1016/S0955-2863(00)00110-8]
252 Nakano T, Hidaka H, Uchida J, Nakajima K, Hata Y. Hypotensive
effects of wakame. J Jpn Soc Clin Nutr 1998; 20: 92
253 Krotkiewski M, Aurell M, Holm G, Grimby G, Szczepanik
J. Effects of a sodium-potassium ion-exchanging seaweed
preparation in mild hypertension. Am J Hypertens 1991; 4:
483-488 [PMID: 1873002 DOI: 10.1093/ajh/4.6.483]
254 Sato M, Oba T, Yamaguchi T, Nakano T, Kahara T, Funayama
K, Kobayashi A, Nakano T. Antihypertensive effects
of hydrolysates of wakame (Undaria pinnatifida) and
their angiotensin-I-converting enzyme inhibitory activity.
Ann Nutr Metab 2002; 46: 259-267 [PMID: 12464726 DOI:
10.1159/000066495]
255 Sato M, Hosokawa T, Yamaguchi T, Nakano T, Muramoto
K, Kahara T, Funayama K, Kobayashi A, Nakano T. Angiotensin
I-converting enzyme inhibitory peptides derived from
wakame (Undaria pinnatifida) and their antihypertensive
effect in spontaneously hypertensive rats. J Agric Food Chem2002; 50: 6245-6252 [PMID: 12358510 DOI: 10.1021/jf020482t]
256 Sankar D, Sambandam G, Ramakrishna Rao M, Pugalendi
KV. Modulation of blood pressure, lipid profiles and redox
status in hypertensive patients taking different edible oils.
Clin Chim Acta 2005; 355: 97-104 [PMID: 15820483 DOI:
10.1016/j.cccn.2004.12.009]
257 Sankar D, Rao MR, Sambandam G, Pugalendi KV. Effect of
sesame oil on diuretics or Beta-blockers in the modulation
of blood pressure, anthropometry, lipid profile, and redox
status. Yale J Biol Med 2006; 79: 19-26 [PMID: 17876372]
258 Miyawaki T, Aono H, Toyoda-Ono Y, Maeda H, Kiso Y,
Moriyama K. Antihypertensive effects of sesamin in humans.
J Nutr Sci Vitaminol (Tokyo) 2009; 55: 87-91 [PMID: 19352068]
259 Wichitsranoi J, Weerapreeyakul N, Boonsiri P, Settasatian
C, Settasatian N, Komanasin N, Sirijaichingkul S, Teerajetgul
Y, Rangkadilok N, Leelayuwat N. Antihypertensive
and antioxidant effects of dietary black sesame meal in prehypertensive
humans. Nutr J 2011; 10: 82 [PMID: 21827664
DOI: 10.1186/1475-2891-10-82]
260 Sudhakar B, Kalaiarasi P, Al-Numair KS, Chandramohan G,
Rao RK, Pugalendi KV. Effect of combination of edible oils
on blood pressure, lipid profile, lipid peroxidative markers,
antioxidant status, and electrolytes in patients with hypertension
on nifedipine treatment. Saudi Med J 2011; 32: 379-385
[PMID: 21483997]
261 Sankar D, Rao MR, Sambandam G, Pugalendi KV. A pilot
study of open label sesame oil in hypertensive diabetics. J
Med Food 2006; 9: 408-412 [PMID: 17004907 DOI: 10.1089/
jmf.2006.9.408]
262 Harikumar KB, Sung B, Tharakan ST, Pandey MK, Joy B,
Guha S, Krishnan S, Aggarwal BB. Sesamin manifests chemopreventive
effects through the suppression of NF-kappa
B-regulated cell survival, proliferation, invasion, and angiogenic
gene products. Mol Cancer Res 2010; 8: 751-761 [PMID:
20460401 DOI: 10.1158/1541-7786.MCR-09-0565]
263 Nakano D, Ogura K, Miyakoshi M, Ishii F, Kawanishi H, Kurumazuka
D, Kwak CJ, Ikemura K, Takaoka M, Moriguchi S,
Iino T, Kusumoto A, Asami S, Shibata H, Kiso Y, Matsumura
Y. Antihypertensive effect of angiotensin I-converting enzyme
inhibitory peptides from a sesame protein hydrolysate
in spontaneously hypertensive rats. Biosci Biotechnol Biochem
2006; 70: 1118-1126 [PMID: 16717411]
264 Karatzi K, Stamatelopoulos K, Lykka M, Mantzouratou
P, Skalidi S, Manios E, Georgiopoulos G, Zakopoulos N,
Papamichael C, Sidossis LS. Acute and long-term hemodynamic
effects of sesame oil consumption in hypertensive
men. J Clin Hypertens (Greenwich) 2012; 14: 630-636 [PMID:
22947362 DOI: 10.1111/j.1751-7176.2012.00649.x]
265 Hodgson JM, Puddey IB, Burke V, Beilin LJ, Jordan N. Effects
on blood pressure of drinking green and black tea. J
Hypertens 1999; 17: 457-463 [PMID: 10404946 DOI: 10.1097/0
0004872-199917040-00002]
266 Kurita I, Maeda-Yamamoto M, Tachibana H, Kamei M.
Antihypertensive effect of Benifuuki tea containing O-methylated
EGCG. J Agric Food Chem 2010; 58: 1903-1908 [PMID:
20078079 DOI: 10.1021/jf904335g]
267 McKay DL, Chen CY, Saltzman E, Blumberg JB. Hibiscus
sabdariffa L. tea (tisane) lowers blood pressure in prehypertensive
and mildly hypertensive adults. J Nutr 2010; 140:
298-303 [PMID: 20018807 DOI: 10.3945/jn.109.115097]
268 Bogdanski P, Suliburska J, Szulinska M, Stepien M, PupekMusialik
D, Jablecka A. Green tea extract reduces blood
pressure, inflammatory biomarkers, and oxidative stress
and improves parameters associated with insulin resistance
in obese, hypertensive patients. Nutr Res 2012; 32: 421-427
[PMID: 22749178 DOI: 10.1016/j.nutres.2012.05.007]
269 Hodgson JM, Woodman RJ, Puddey IB, Mulder T, Fuchs
D, Croft KD. Short-term effects of polyphenol-rich black tea
on blood pressure in men and women. Food Funct 2013; 4:
111-115 [PMID: 23038021 DOI: 10.1039/c2fo30186e]
270 Medina-Rem�n A, Estruch R, Tresserra-Rimbau A, Vallverd�-Queralt A, Lamuela-Raventos RM. The effect of polyphenol
consumption on blood pressure. Mini Rev Med Chem
2013; 13: 1137-1149 [PMID: 22931531]
271 Jim�nez R, Duarte J, Perez-Vizcaino F. Epicatechin: endothelial
function and blood pressure. J Agric Food Chem 2012; 60:
8823-8830 [PMID: 22440087 DOI: 10.1021/jf205370q]
272 Taubert D, Roesen R, Sch�mig E. Effect of cocoa and tea
intake on blood pressure: a meta-analysis. Arch Intern Med
2007; 167: 626-634 [PMID: 17420419 DOI: 10.1001/�archinte.16
7.7.626]
273 Grassi D, Lippi C, Necozione S, Desideri G, Ferri C. Shortterm
administration of dark chocolate is followed by a
significant increase in insulin sensitivity and a decrease in
blood pressure in healthy persons. Am J Clin Nutr 2005; 81:
611-614 [PMID: 15755830]
274 Taubert D, Roesen R, Lehmann C, Jung N, Sch�mig E. Effects
of low habitual cocoa intake on blood pressure and bioactive
nitric oxide: a randomized controlled trial. JAMA 2007;
298: 49-60 [PMID: 17609490 DOI: 10.1001/jama.298.1.49]
275 Cohen DL, Townsend RR. Cocoa ingestion and hypertension-another
cup please? J Clin Hypertens (Greenwich)
2007; 9: 647-648 [PMID: 17673887 DOI: 10.1111/
j.1524-6175.2007.07291.x]
276 Ried K, Sullivan T, Fakler P, Frank OR, Stocks NP. Does
chocolate reduce blood pressure? A meta-analysis. BMC Med
2010; 8: 39 [PMID: 20584271 DOI: 10.1186/1741-7015-8-39]
277 Egan BM, Laken MA, Donovan JL, Woolson RF. Does dark
chocolate have a role in the prevention and management of
hypertension?: commentary on the evidence. Hypertension
2010; 55: 1289-1295 [PMID: 20404213 DOI: 10.1161/HYPERTENSIONAHA.110.151522]
278 Desch S, Kobler D, Schmidt J, Sonnabend M, Adams V,
Sareban M, Eitel I, Bl�her M, Schuler G, Thiele H. Low vs.
higher-dose dark chocolate and blood pressure in cardiovascular
high-risk patients. Am J Hypertens 2010; 23: 694-700
[PMID: 20203627 DOI: 10.1038/ajh.2010.29]
279 Desch S, Schmidt J, Kobler D, Sonnabend M, Eitel I, Sareban
M, Rahimi K, Schuler G, Thiele H. Effect of cocoa products
on blood pressure: systematic review and meta-analysis. Am
J Hypertens 2010; 23: 97-103 [PMID: 19910929 DOI: 10.1038/
ajh.2009.213]
280 Grassi D, Desideri G, Necozione S, Lippi C, Casale R,
Properzi G, Blumberg JB, Ferri C. Blood pressure is reduced
and insulin sensitivity increased in glucose-intolerant, hypertensive
subjects after 15 days of consuming high-polyphenol
dark chocolate. J Nutr 2008; 138: 1671-1676 [PMID: 18716168]
281 Grassi D, Necozione S, Lippi C, Croce G, Valeri L, Pasqualetti
P, Desideri G, Blumberg JB, Ferri C. Cocoa reduces blood
pressure and insulin resistance and improves endotheliumdependent
vasodilation in hypertensives. Hypertension
2005; 46: 398-405 [PMID: 16027246 DOI: 10.1161/01.
HYP.0000174990.46027.70]
282 Ellinger S, Reusch A, Stehle P, Helfrich HP. Epicatechin
ingested via cocoa products reduces blood pressure in
humans: a nonlinear regression model with a Bayesian approach.
Am J Clin Nutr 2012; 95: 1365-1377 [PMID: 22552030
DOI: 10.3945/ajcn.111.029330]
283 Hooper L, Kay C, Abdelhamid A, Kroon PA, Cohn JS, Rimm
EB, Cassidy A. Effects of chocolate, cocoa, and flavan-3-ols
on cardiovascular health: a systematic review and meta-analysis
of randomized trials. Am J Clin Nutr 2012; 95: 740-751
[PMID: 22301923 DOI: 10.3945/ajcn.111.023457]
284 Yamaguchi T, Chikama A, Mori K, Watanabe T, Shioya Y,
Katsuragi Y, Tokimitsu I. Hydroxyhydroquinone-free coffee:
a double-blind, randomized controlled dose-response study
of blood pressure. Nutr Metab Cardiovasc Dis 2008; 18: 408-414
[PMID: 17951035 DOI: 10.1016/j.numecd.2007.03.004]
285 Chen ZY, Peng C, Jiao R, Wong YM, Yang N, Huang Y.
Anti-hypertensive nutraceuticals and functional foods. J
Agric Food Chem 2009; 57: 4485-4499 [PMID: 19422223 DOI:
10.1021/jf900803r]
286 Ochiai R, Chikama A, Kataoka K, Tokimitsu I, Maekawa Y,
Ohishi M, Rakugi H, Mikami H. Effects of hydroxyhydroquinone-reduced
coffee on vasoreactivity and blood pressure.
Hypertens Res 2009; 32: 969-974 [PMID: 19713967 DOI:
10.1038/hr.2009.132]
287 Kozuma K, Tsuchiya S, Kohori J, Hase T, Tokimitsu I. Antihypertensive
effect of green coffee bean extract on mildly
hypertensive subjects. Hypertens Res 2005; 28: 711-718 [PMID:
16419643 DOI: 10.1291/hypres.28.711]
288 Palatini P, Ceolotto G, Ragazzo F, Dorigatti F, Saladini F,
Papparella I, Mos L, Zanata G, Santonastaso M. CYP1A2
genotype modifies the association between coffee intake
and the risk of hypertension. J Hypertens 2009; 27: 1594-1601
[PMID: 19451835 DOI: 10.1097/HJH.0b013e32832ba850]
289 Scheer FA, Van Montfrans GA, van Someren EJ, Mairuhu
G, Buijs RM. Daily nighttime melatonin reduces blood pressure
in male patients with essential hypertension. Hypertension
2004; 43: 192-197 [PMID: 14732734 DOI: 10.1161/01.
HYP.0000113293.15186.3b]
290 Cavallo A, Daniels SR, Dolan LM, Khoury JC, Bean JA.
Blood pressure response to melatonin in type 1 diabetes.
Pediatr Diabetes 2004; 5: 26-31 [PMID: 15043687 DOI: 10.1111
/�j.1399-543X.2004.00031.x]
291 Cavallo A, Daniels SR, Dolan LM, Bean JA, Khoury JC.
Blood pressure-lowering effect of melatonin in type 1 diabetes.
J Pineal Res 2004; 36: 262-266 [PMID: 15066051 DOI:
10.1111/j.1600-079X.2004.00126.x]
292 Cagnacci A, Cannoletta M, Renzi A, Baldassari F, Arangino
S, Volpe A. Prolonged melatonin administration decreases
nocturnal blood pressure in women. Am J Hypertens 2005; 18:
1614-1618 [PMID: 16364834]
293 Grossman E, Laudon M, Yalcin R, Zengil H, Peleg E, Sharabi
Y, Kamari Y, Shen-Orr Z, Zisapel N. Melatonin reduces night
blood pressure in patients with nocturnal hypertension. Am
J Med 2006; 119: 898-902 [PMID: 17000226 DOI: 10.1016/
j.amjmed.2006.02.002]
294 Rechci?ski T, Kurpesa M, Trzos E, Krzeminska-Paku?a M.
[The influence of melatonin supplementation on circadian
pattern of blood pressure in patients with coronary artery
disease–preliminary report]. Pol Arch Med Wewn 2006; 115:
520-528 [PMID: 17263223]
295 Merkur�eva GA, Ryzhak GA. [Effect of the pineal gland peptide
preparation on the diurnal profile of arterial pressure in
middle-aged and elderly women with ischemic heart disease
and arterial hypertension]. Adv Gerontol 2008; 21: 132-142
[PMID: 18546838]
296 Zaslavskaia RM, Shcherban� EA, Logvinenko SI. [Melatonin
in combined therapy of patients with stable angina and arterial
hypertension]. Klin Med (Mosk) 2008; 86: 64-67 [PMID:
19048842]
297 Zamotaev IuN, Enikeev AKh, Kolomoets NM. [The use of
melaxen in combined therapy of arterial hypertension in
subjects occupied in assembly line production]. Klin Med
(Mosk) 2009; 87: 46-49 [PMID: 19670717]
298 Rechci?ski T, Trzos E, Wierzbowska-Drabik K, Krzemi?skaPaku?a
M, Kurpesa M. Melatonin for nondippers with coronary
artery disease: assessment of blood pressure profile and
heart rate variability. Hypertens Res 2010; 33: 56-61 [PMID:
19876062 DOI: 10.1038/hr.2009.174]
299 Kozir�g M, Poliwczak AR, Duchnowicz P, Koter-Michalak
M, Sikora J, Broncel M. Melatonin treatment improves
blood pressure, lipid profile, and parameters of oxidative
stress in patients with metabolic syndrome. J Pineal Res
2011; 50: 261-266 [PMID: 21138476 DOI: 10.1111/j.1600-
079X.2010.00835.x]
300 De Leersnyder H, de Blois MC, Vekemans M, Sidi D, Villain
E, Kindermans C, Munnich A. beta(1)-adrenergic antagonists
improve sleep and behavioural disturbances in a circadian
disorder, Smith-Magenis syndrome. J Med Genet 2001; 38:
586-590 [PMID: 11546826]
301 Morand C, Dubray C, Milenkovic D, Lioger D, Martin JF,
Scalbert A, Mazur A. Hesperidin contributes to the vascular
protective effects of orange juice: a randomized crossover
study in healthy volunteers. Am J Clin Nutr 2011; 93: 73-80
[PMID: 21068346 DOI: 10.3945/ajcn.110.004945]
302 Basu A, Penugonda K. Pomegranate juice: a heart-healthy
fruit juice. Nutr Rev 2009; 67: 49-56 [PMID: 19146506 DOI:
10.1111/j.1753-4887.2008.00133.x]
303 Aviram M, Rosenblat M, Gaitini D, Nitecki S, Hoffman A,
Dornfeld L, Volkova N, Presser D, Attias J, Liker H, Hayek
T. Pomegranate juice consumption for 3 years by patients
with carotid artery stenosis reduces common carotid intimamedia
thickness, blood pressure and LDL oxidation. Clin
Nutr 2004; 23: 423-433 [PMID: 15158307 DOI: 10.1016/�j.
clnu.2003.10.002]
304 Aviram M, Dornfeld L. Pomegranate juice consumption
inhibits serum angiotensin converting enzyme activity and
reduces systolic blood pressure. Atherosclerosis 2001; 158:
195-198 [PMID: 11500191]
305 Feringa HH, Laskey DA, Dickson JE, Coleman CI. The effect
of grape seed extract on cardiovascular risk markers:
a meta-analysis of randomized controlled trials. J Am Diet
Assoc 2011; 111: 1173-1181 [PMID: 21802563 DOI: 10.1016/�j.
jada.2011.05.015]
306 Sivaprakasapillai B, Edirisinghe I, Randolph J, Steinberg
F, Kappagoda T. Effect of grape seed extract on blood pressure
in subjects with the metabolic syndrome. Metabolism
2009; 58: 1743-1746 [PMID: 19608210 DOI: 10.1016/�j.metabol.2009.05.030]
307 Edirisinghe I, Burton-Freeman B, Tissa Kappagoda C. Mechanism
of the endothelium-dependent relaxation evoked by a
grape seed extract. Clin Sci (Lond) 2008; 114: 331-337 [PMID:
17927567 DOI: 10.1042/CS20070264]
308 Rosenfeldt FL, Haas SJ, Krum H, Hadj A, Ng K, Leong JY,
Watts GF. Coenzyme Q10 in the treatment of hypertension: a
meta-analysis of the clinical trials. J Hum Hypertens 2007; 21:
297-306 [PMID: 17287847]
309 Burke BE, Neuenschwander R, Olson RD. Randomized,
double-blind, placebo-controlled trial of coenzyme Q10
in isolated systolic hypertension. South Med J 2001; 94:
1112-1117 [PMID: 11780680 DOI: 10.1097/00007611-20011100
0-00015]
310 Mikhin VP, Kharchenko AV, Rosliakova EA, Cherniatina
MA. [Application of coenzyme Q(10) in combination therapy
of arterial hypertension]. Kardiologiia 2011; 51: 26-31 [PMID:
21878067]
311 Tsai KL, Huang YH, Kao CL, Yang DM, Lee HC, Chou HY,
Chen YC, Chiou GY, Chen LH, Yang YP, Chiu TH, Tsai CS,
Ou HC, Chiou SH. A novel mechanism of coenzyme Q10
protects against human endothelial cells from oxidative
stress-induced injury by modulating NO-related pathways.
J Nutr Biochem 2012; 23: 458-468 [PMID: 21684136 DOI:
10.1016/j.jnutbio.2011.01.011]
312 Sohet FM, Delzenne NM. Is there a place for coenzyme Q
in the management of metabolic disorders associated with
obesity? Nutr Rev 2012; 70: 631-641 [PMID: 23110642 DOI:
10.1111/j.1753-4887.2012.00526.x]
313 Digiesi V, Cantini F, Oradei A, Bisi G, Guarino GC, Brocchi
A, Bellandi F, Mancini M, Littarru GP. Coenzyme Q10
in essential hypertension. Mol Aspects Med 1994; 15 Suppl:
s257-s263 [PMID: 7752838]
314 Langsjoen P, Langsjoen P, Willis R, Folkers K. Treatment of
essential hypertension with coenzyme Q10. Mol Aspects Med
1994; 15 Suppl: S265-S272 [PMID: 7752851 DOI: 10.1016/009
8-2997(94)90037-X]
315 Ankola DD, Viswanad B, Bhardwaj V, Ramarao P, Kumar
MN. Development of potent oral nanoparticulate formulation
of coenzyme Q10 for treatment of hypertension: can
the simple nutritional supplements be used as first line
therapeutic agents for prophylaxis/therapy? Eur J Pharm
Biopharm 2007; 67: 361-369 [PMID: 17452099 DOI: 10.1016/
j.ejpb.2007.03.010]
316 Trimarco V, Cimmino CS, Santoro M, Pagnano G, Manzi
MV, Piglia A, Giudice CA, De Luca N, Izzo R. Nutraceuticals
for blood pressure control in patients with high-normal or
grade 1 hypertension. High Blood Press Cardiovasc Prev 2012;
19: 117-122 [PMID: 22994579 DOI: 10.2165/11632160-0000000
00-00000]
317 Young JM, Florkowski CM, Molyneux SL, McEwan RG,
Frampton CM, Nicholls MG, Scott RS, George PM. A randomized,
double-blind, placebo-controlled crossover study
of coenzyme Q10 therapy in hypertensive patients with the
metabolic syndrome. Am J Hypertens 2012; 25: 261-270 [PMID:
22113168 DOI: 10.1038/ajh.2011.209]
318 McMackin CJ, Widlansky ME, Hamburg NM, Huang AL,
Weller S, Holbrook M, Gokce N, Hagen TM, Keaney JF, Vita
JA. Effect of combined treatment with alpha-Lipoic acid and
acetyl-L-carnitine on vascular function and blood pressure
in patients with coronary artery disease. J Clin Hypertens
(Greenwich) 2007; 9: 249-255 [PMID: 17396066 DOI: 10.1111/
j.1524-6175.2007.06052.x]
319 Salinthone S, Schillace RV, Tsang C, Regan JW, Bourdette
DN, Carr DW. Lipoic acid stimulates cAMP production
via G protein-coupled receptor-dependent and -independent
mechanisms. J Nutr Biochem 2011; 22: 681-690 [PMID:
21036588 DOI: 10.1016/j.jnutbio.2010.05.008]
320 Rahman ST, Merchant N, Haque T, Wahi J, Bhaheetharan S,
Ferdinand KC, Khan BV. The impact of lipoic acid on endothelial
function and proteinuria in quinapril-treated diabetic
patients with stage I hypertension: results from the QUALITY
study. J Cardiovasc Pharmacol Ther 2012; 17: 139-145 [PMID:
21750253 DOI: 10.1177/1074248411413282]
321 Morcos M, Borcea V, Isermann B, Gehrke S, Ehret T, Henkels
M, Schiekofer S, Hofmann M, Amiral J, Tritschler H,
Ziegler R, Wahl P, Nawroth PP. Effect of alpha-lipoic acid on
the progression of endothelial cell damage and albuminuria
in patients with diabetes mellitus: an exploratory study. Diabetes
Res Clin Pract 2001; 52: 175-183 [PMID: 11323087]
322 Jiang B, Haverty M, Brecher P. N-acetyl-L-cysteine enhances
interleukin-1beta-induced nitric oxide synthase expression.
Hypertension 1999; 34: 574-579 [PMID: 10523329]
323 Vasdev S, Singal P, Gill V. The antihypertensive effect of
cysteine. Int J Angiol 2009; 18: 7-21 [PMID: 22477470 DOI:
10.1055/s-0031-1278316]
324 Meister A, Anderson ME, Hwang O. Intracellular cysteine
and glutathione delivery systems. J Am Coll Nutr 1986; 5:
137-151 [PMID: 3722629 DOI: 10.1080/07315724.1986.107201
21]
325 Asher GN, Viera AJ, Weaver MA, Dominik R, Caughey M,
Hinderliter AL. Effect of hawthorn standardized extract on
flow mediated dilation in prehypertensive and mildly hypertensive
adults: a randomized, controlled cross-over trial.
BMC Complement Altern Med 2012; 12: 26 [PMID: 22458601
DOI: 10.1186/1472-6882-12-26]
326 Ko�yildiz ZC, Birman H, Olga� V, Akg�n-Dar K, Meliko?lu
G, Meri�li AH. Crataegus tanacetifolia leaf extract prevents
L-NAME-induced hypertension in rats: a morphological
study. Phytother Res 2006; 20: 66-70 [PMID: 16397846 DOI:
10.1002/ptr.1808]
327 Schr�der D, Weiser M, Klein P. Efficacy of a homeopathic
Crataegus preparation compared with usual therapy for
mild (NYHA II) cardiac insufficiency: results of an observational
cohort study. Eur J Heart Fail 2003; 5: 319-326 [PMID:
12798830 DOI: 10.1016/S1388-9842(02)00237-4]
328 Walker AF, Marakis G, Simpson E, Hope JL, Robinson PA,
Hassanein M, Simpson HC. Hypotensive effects of hawthorn
for patients with diabetes taking prescription drugs: a
randomised controlled trial. Br J Gen Pract 2006; 56: 437-443
[PMID: 16762125]
329 Walker AF, Marakis G, Morris AP, Robinson PA. Promising
hypotensive effect of hawthorn extract: a randomized double-blind
pilot study of mild, essential hypertension. Phytother
Res 2002; 16: 48-54 [PMID: 11807965 DOI: 10.1002/�ptr.947]
330 Larson A, Witman MA, Guo Y, Ives S, Richardson RS, Bruno
RS, Jalili T, Symons JD. Acute, quercetin-induced reductions
in blood pressure in hypertensive individuals are not secondary
to lower plasma angiotensin-converting enzyme activity
or endothelin-1: nitric oxide. Nutr Res 2012; 32: 557-564
[PMID: 22935338 DOI: 10.1016/j.nutres.2012.06.018]
331 Edwards RL, Lyon T, Litwin SE, Rabovsky A, Symons JD,
Jalili T. Quercetin reduces blood pressure in hypertensive
subjects. J Nutr 2007; 137: 2405-2411 [PMID: 17951477]
332 Egert S, Bosy-Westphal A, Seiberl J, K�rbitz C, Settler U,
Plachta-Danielzik S, Wagner AE, Frank J, Schrezenmeir J,
Rimbach G, Wolffram S, M�ller MJ. Quercetin reduces systolic
blood pressure and plasma oxidised low-density lipoprotein
concentrations in overweight subjects with a high-cardiovascular
disease risk phenotype: a double-blinded, placebocontrolled
cross-over study. Br J Nutr 2009; 102: 1065-1074
[PMID: 19402938 DOI: 10.1017/�S0007114509359127]
333 Trovato A, Nuhlicek DN, Midtling JE. Drug-nutrient interactions.
Am Fam Physician 1991; 44: 1651-1658 [PMID: 1950962]

 #4: Beware Of Little Critters
#4: Beware Of Little Critters

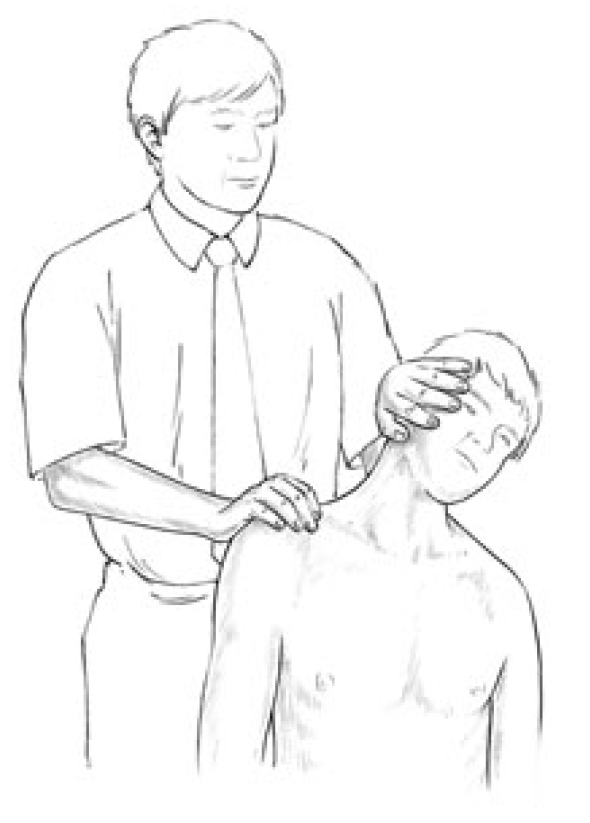
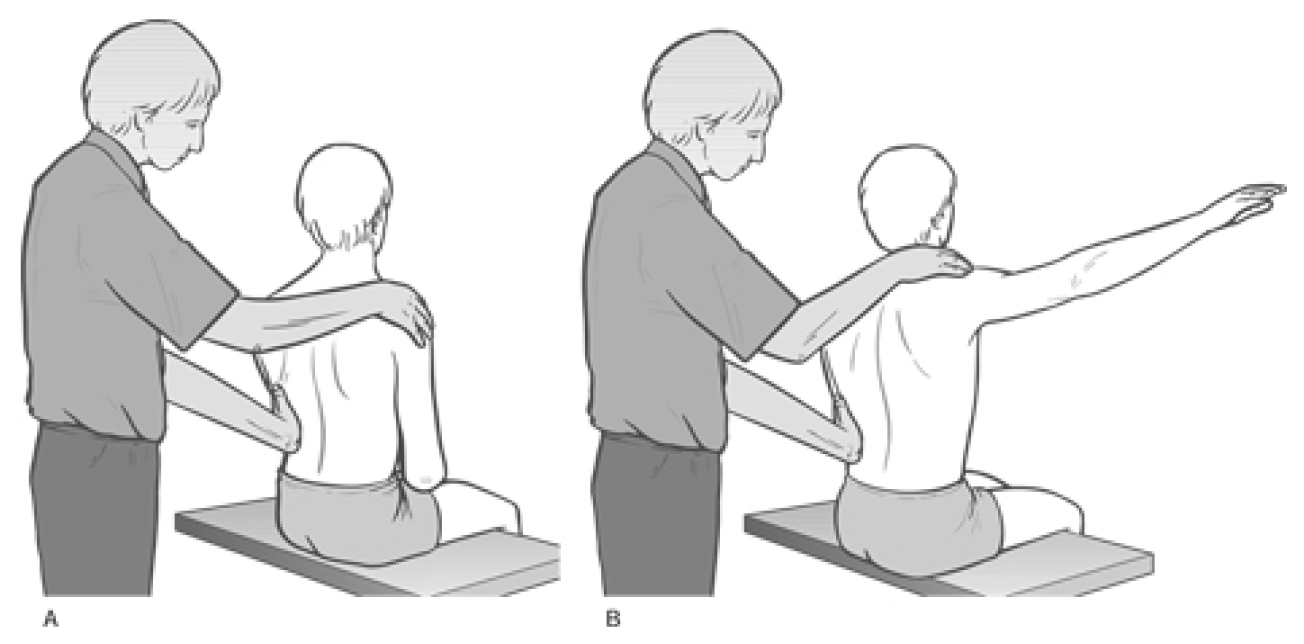
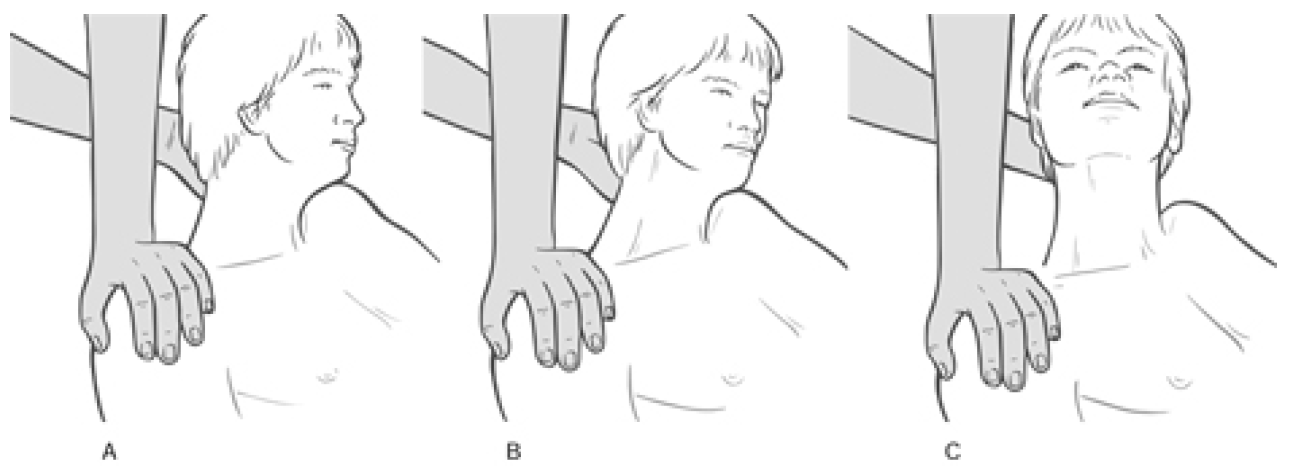


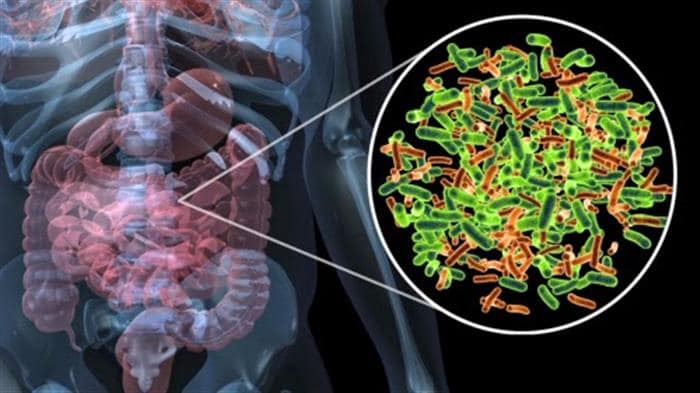
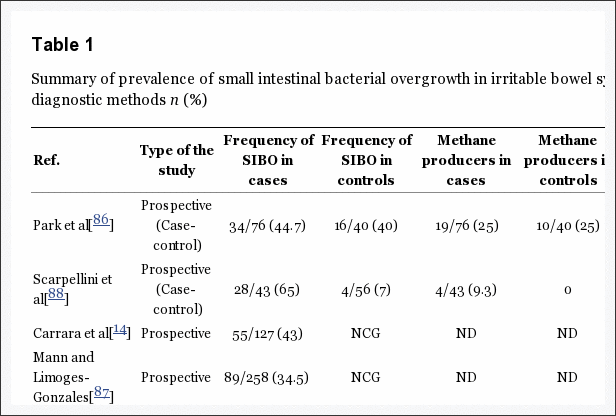
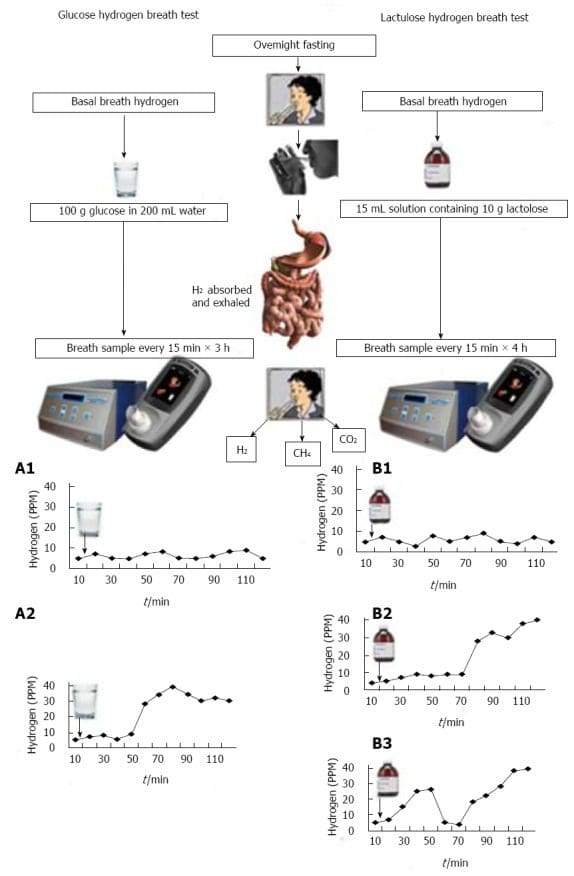
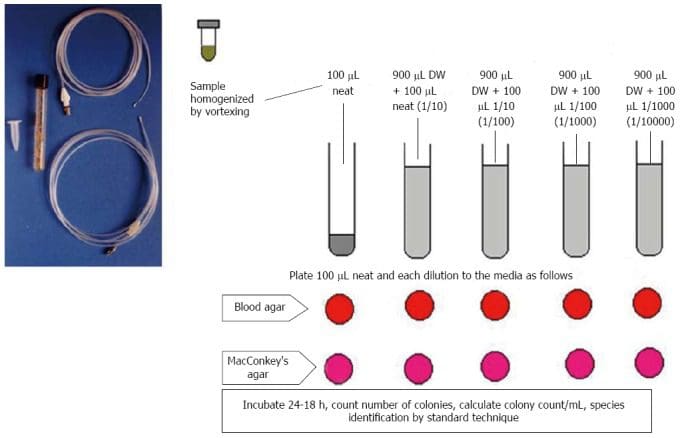
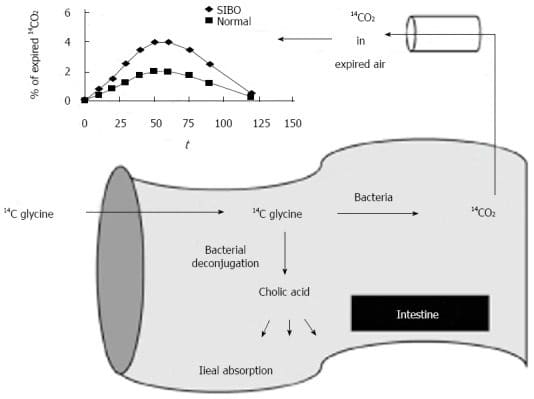

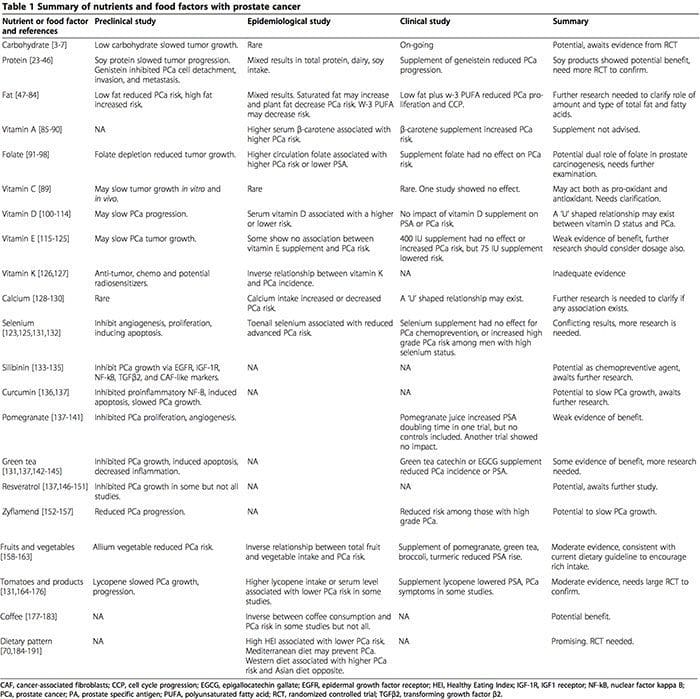

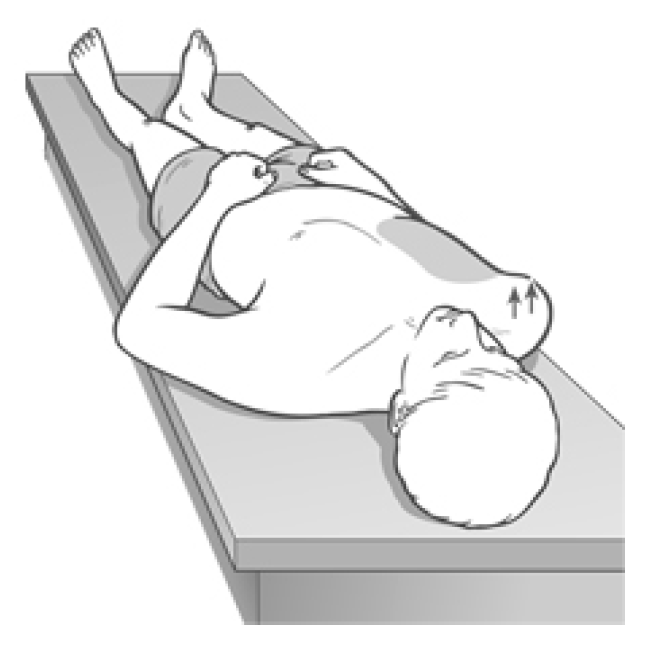


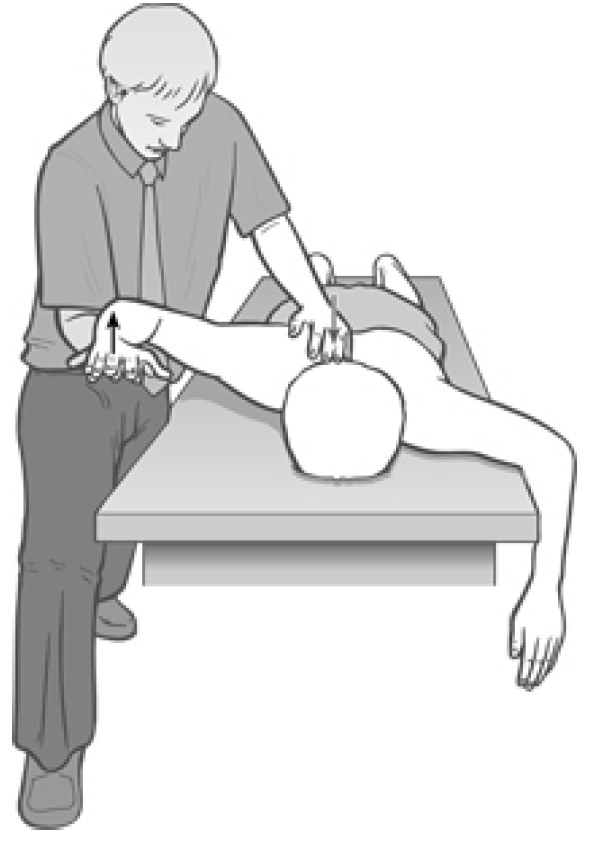
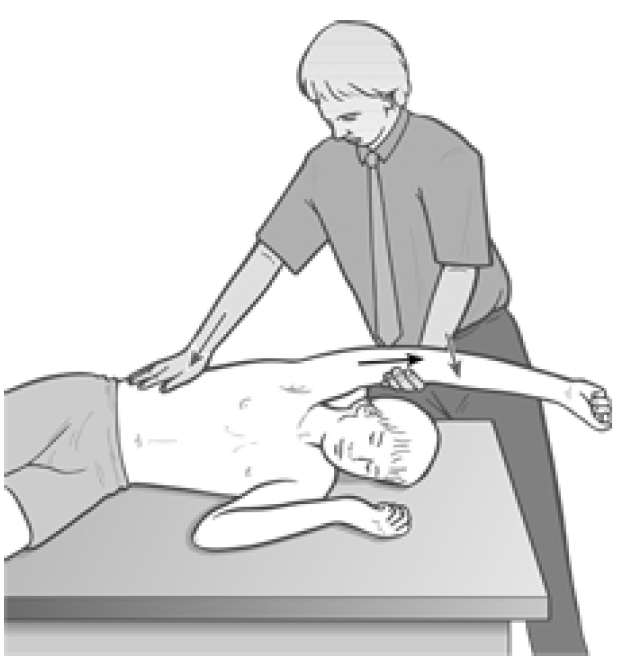


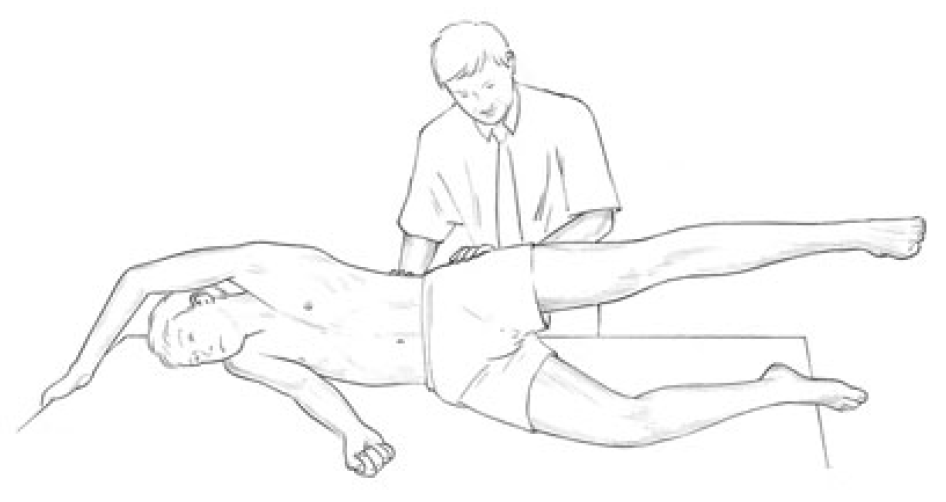

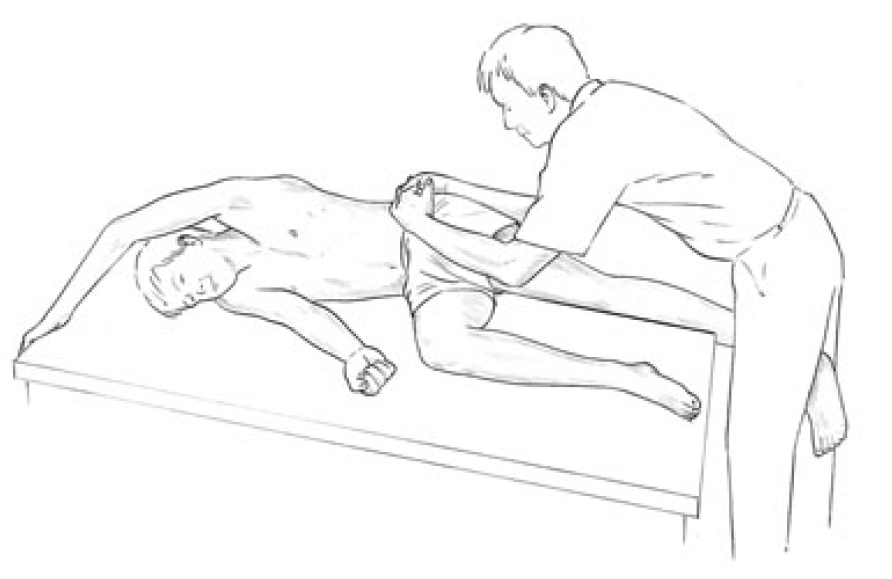


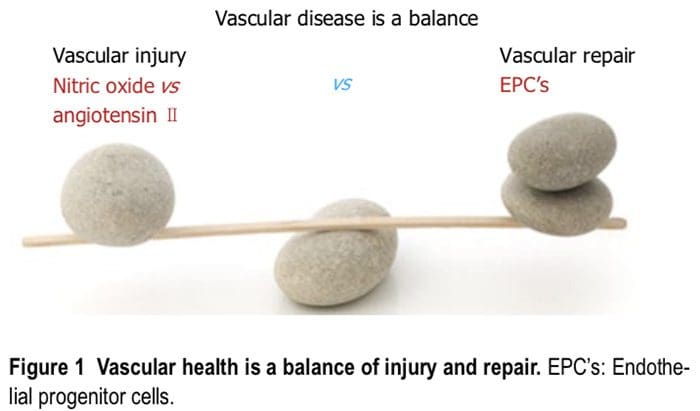
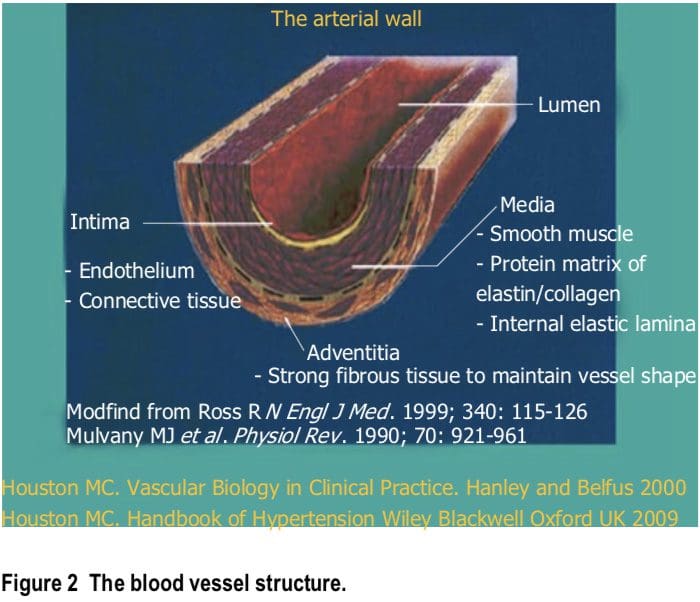
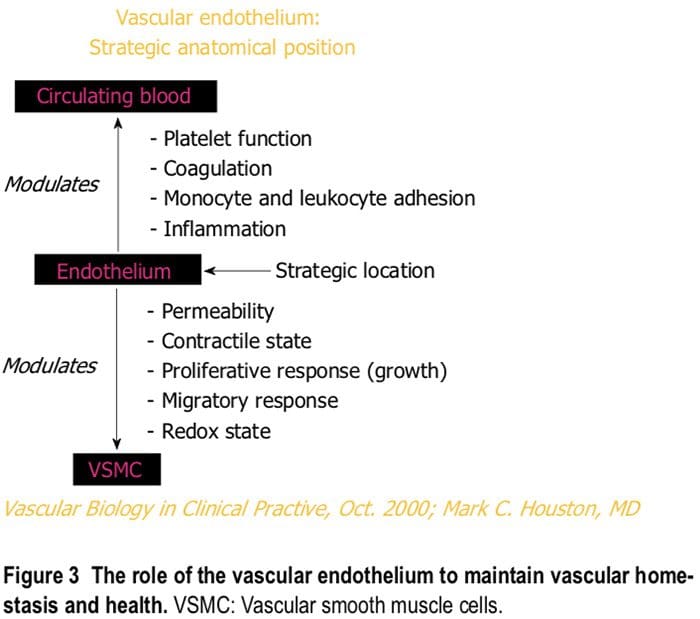 Macronutrient and micronutrient deficiencies are very common in the general population and may be even more common in patients with hypertension and cardiovascular
Macronutrient and micronutrient deficiencies are very common in the general population and may be even more common in patients with hypertension and cardiovascular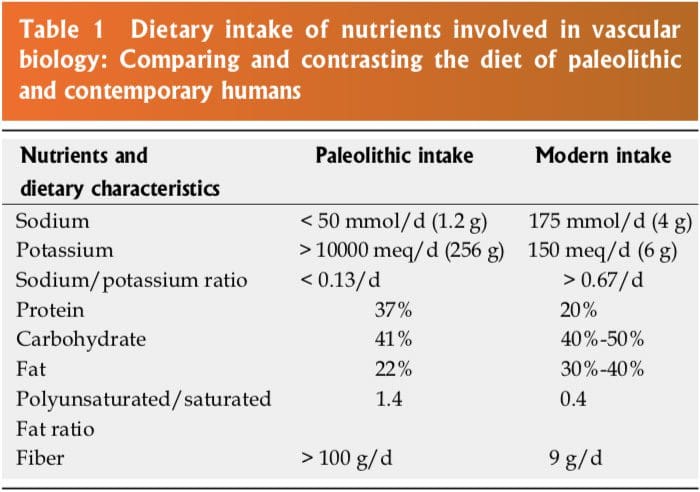 The human genetic makeup is 99.9% that of our Paleolithic ancestors, yet our nutritional, vitamin and mineral intakes are vastly different[3]. The macronutrient and micronutrient variations, oxidative stress from radical oxygen species (ROS) and radical nitrogen species (RNS) and inflammatory mediators such as cell adhesion molecules (CAMs), cytokines, signaling molecules and autoimmune vascular dysfunction of T cells and B cells, contribute
The human genetic makeup is 99.9% that of our Paleolithic ancestors, yet our nutritional, vitamin and mineral intakes are vastly different[3]. The macronutrient and micronutrient variations, oxidative stress from radical oxygen species (ROS) and radical nitrogen species (RNS) and inflammatory mediators such as cell adhesion molecules (CAMs), cytokines, signaling molecules and autoimmune vascular dysfunction of T cells and B cells, contribute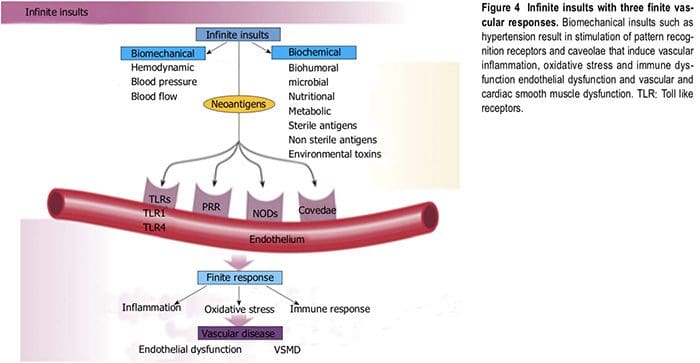 PATHOPHYSIOLOGY
PATHOPHYSIOLOGY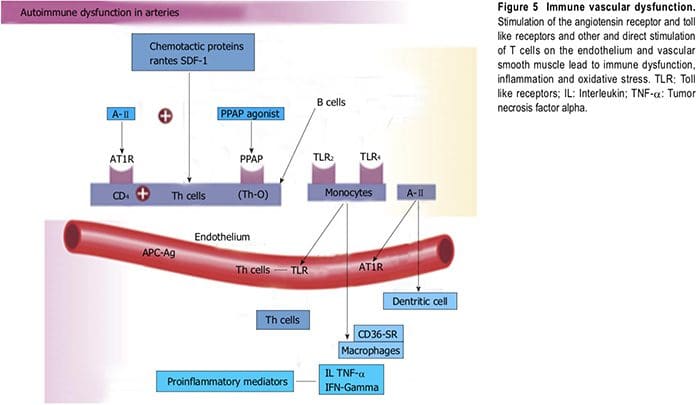
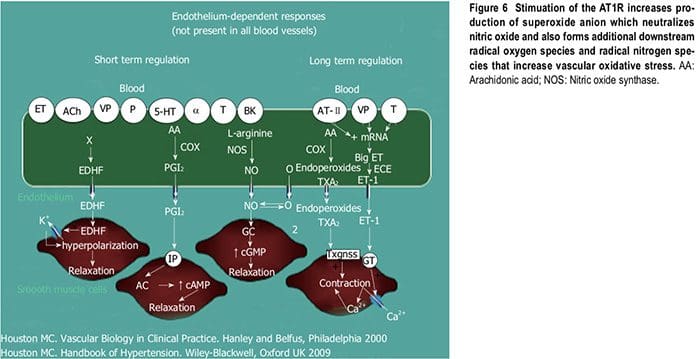 Numerous microbial organisms have been implicated in hypertension and CHD[18-20]. All of these insults lead to impaired microvascular structure and function which manifests clinically as hypertension[12-14]. The level of BP may not give an accurate indication of the microvascular involvement and impairment in hypertension. Hypertensive patients have abnormal microvasculature in the form of inward eutrophic remodeling of the small resistance arteries leading to impaired vasodilatory capacity, increased vascular resistance, increased media to lumen ratio, decreased maximal organ perfusion and reduced flow reserve, especially in the heart with decreased coronary flow reserve[12-14]. Significant functional then structural microvascular impairment occurs even before the BP begins to rise in normotensive offspring of hypertensive parents evidenced by ED, impaired vasodilation, forearm vascular resistance, diastolic dysfunction, increased left ventricular mass index, increased septal and posterior wall thickness and left ventricular hypertrophy[12,15]. Thus, the cellular processes underlying the vascular perturbations constitute a vascular phenotype of hypertension that may be determined by early life
Numerous microbial organisms have been implicated in hypertension and CHD[18-20]. All of these insults lead to impaired microvascular structure and function which manifests clinically as hypertension[12-14]. The level of BP may not give an accurate indication of the microvascular involvement and impairment in hypertension. Hypertensive patients have abnormal microvasculature in the form of inward eutrophic remodeling of the small resistance arteries leading to impaired vasodilatory capacity, increased vascular resistance, increased media to lumen ratio, decreased maximal organ perfusion and reduced flow reserve, especially in the heart with decreased coronary flow reserve[12-14]. Significant functional then structural microvascular impairment occurs even before the BP begins to rise in normotensive offspring of hypertensive parents evidenced by ED, impaired vasodilation, forearm vascular resistance, diastolic dysfunction, increased left ventricular mass index, increased septal and posterior wall thickness and left ventricular hypertrophy[12,15]. Thus, the cellular processes underlying the vascular perturbations constitute a vascular phenotype of hypertension that may be determined by early life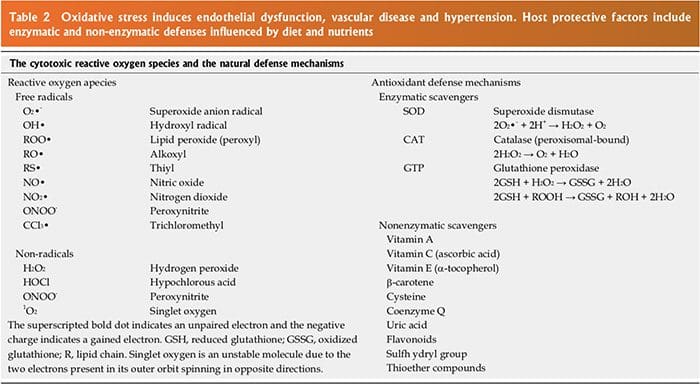
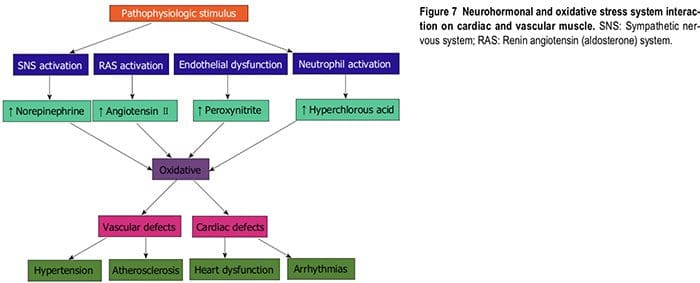 Inflammation
Inflammation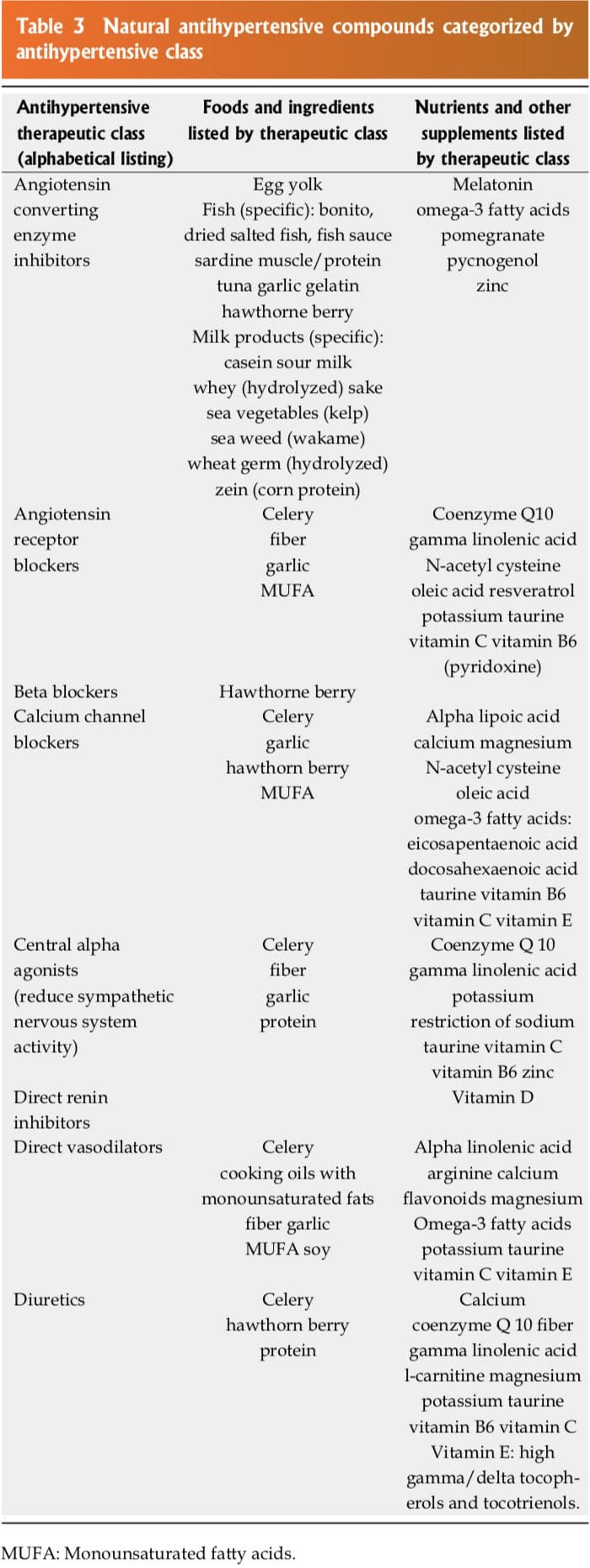 Dietary Approaches To Stop Hypertension Diets
Dietary Approaches To Stop Hypertension Diets