Chiropractic Care: Skeletal & Heart Health in Daily Wellness
Learn the connections between chiropractic care, skeletal health, and cardiovascular health to improve your wellness journey.
Chiropractic Care for Skeletal and Cardiovascular Health: A Comprehensive Guide to Holistic Recovery
Welcome, dear reader, to a spine-chilling exploration of how chiropractic care can mend your bones and keep your heart from staging a dramatic exit. Picture your skeleton as the grim framework of a haunted house, creaking under the weight of life’s misadventures, while your cardiovascular system plays the role of a ghostly butler, silently ensuring everything runs smoothly—until it doesn’t. At El Paso Back Clinic, Dr. Alexander Jimenez, DC, APRN, FNP-BC, is the master of this macabre mansion, wielding advanced diagnostics and dual-scope expertise to banish pain and restore vitality. With over 25 years of experience, Dr. Jimenez doesn’t just crack backs; he stitches together the physical and legal threads of personal injury cases with the precision of a mortician sewing up a corpse. In this 5,000-word odyssey, we’ll unravel the eerie connection between skeletal health and the cardiovascular system, explore how chiropractic care can exorcise the demons of dysfunction, and highlight why Dr. Jimenez is El Paso’s go-to grim reaper for injury recovery. Buckle up—it’s going to be a delightfully dark ride.
The Spooky Symphony of Skeletal and Cardiovascular Health
Your skeleton and cardiovascular system are like an old married couple in a gothic romance: inseparable, codependent, and occasionally causing each other grief. The skeletal system, with its 206 bones, provides the structural scaffolding that keeps you upright, while the cardiovascular system—your heart, blood vessels, and blood—delivers oxygen and nutrients to keep those bones from crumbling like a neglected crypt. But when one system falters, the other often follows, creating a cascade of chaos that can turn your daily routine into a horror show.
The Skeletal System: The Framework of Your Mortal Coil
Bones are more than just the spooky props in a Halloween display; they’re dynamic, living tissues that support movement, protect vital organs, and produce blood cells in the bone marrow. Think of your spine as the central pillar of a haunted cathedral—when it’s misaligned, the whole structure groans. Misalignments, or subluxations, can pinch nerves, disrupt blood flow, and send pain signals that make you feel like you’ve been cursed. Conditions like osteoarthritis, herniated discs, or scoliosis can further haunt your skeletal health, limiting mobility and inviting chronic pain to the party.
The Cardiovascular System: The Lifeblood of Your Existence
Your cardiovascular system is the tireless phantom that keeps your body animated. The heart pumps blood through arteries, veins, and capillaries, delivering oxygen and nutrients to every cell while whisking away waste like a spectral janitor. But poor skeletal health can strangle this system like a noose. For instance, a misaligned spine can compress blood vessels, reducing circulation and increasing the heart’s workload. This can lead to hypertension, a villain that lurks in the shadows, raising the risk of heart disease and stroke. Conversely, cardiovascular issues like atherosclerosis (hardened arteries) can starve bones of nutrients, weakening them and making them brittle, like the fragile relics of a forgotten graveyard.
The Grim Connection: How They Haunt Each Other
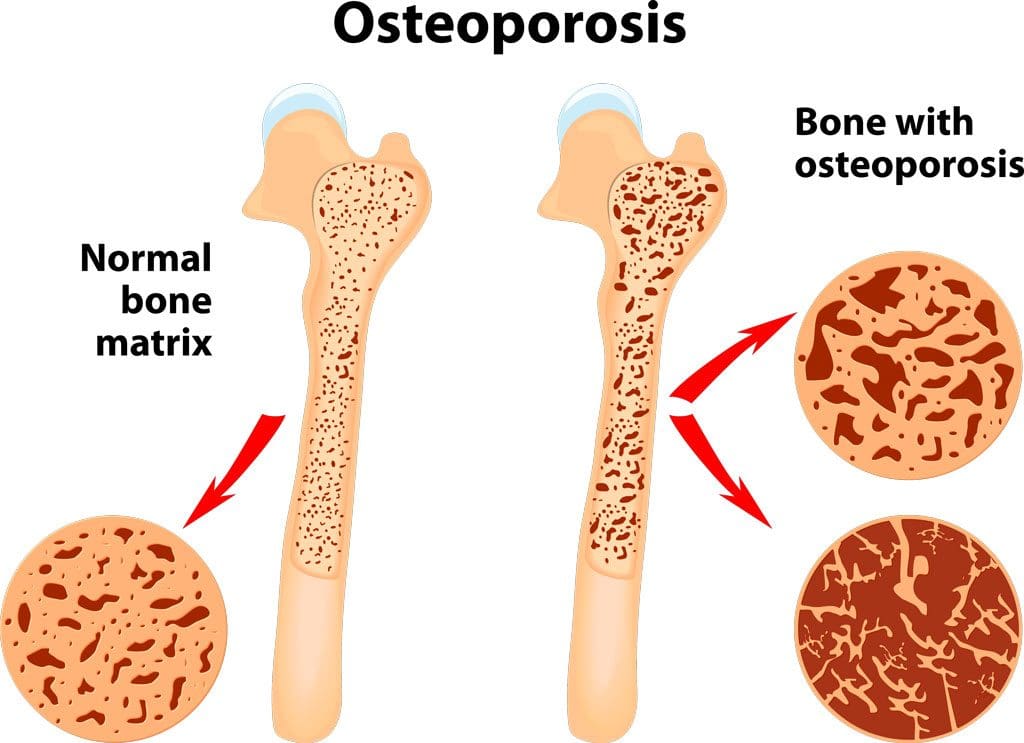
The interplay between skeletal and cardiovascular health is a twisted dance of cause and effect. Poor posture or spinal misalignments can impair nerve function, which regulates heart rate and blood pressure, leading to cardiovascular strain. Meanwhile, reduced blood flow from cardiovascular issues can starve bones of essential nutrients, increasing the risk of osteoporosis or fractures. This vicious cycle can amplify overlapping risk profiles—obesity, inactivity, and inflammation—that wreak havoc on both systems, turning your daily routine into a slog through a fog-laden swamp.
For example, chronic inflammation, a common culprit in both musculoskeletal and cardiovascular disorders, acts like a malevolent spirit, eroding joint cartilage and clogging arteries. Obesity, another shared risk factor, adds extra weight to your skeletal frame, stressing joints and forcing the heart to pump harder, like a doomed soul rowing across the River Styx. Sedentary lifestyles only deepen the gloom, weakening muscles and bones while slowing circulation, inviting blood clots and heart attacks to the macabre masquerade.
References
- El Paso Back Clinic. (n.d.). Nutritional strategies for health and pain management. https://elpasobackclinic.com/nutritional-strategies-health/
- Jimenez, A. (2025). Dr. Alexander Jimenez, DC, APRN, FNP-BC, IFMCP, CFMP, ATN ♛ – Injury Medical Clinic PA | LinkedIn. https://www.linkedin.com/in/dralexjimenez/
Chiropractic Care: Banishing the Ghosts of Pain
Chiropractic care, as practiced by Dr. Alex Jimenez at El Paso Back Clinic, is like a séance for your spine, summoning relief through precise adjustments and holistic interventions. Unlike invasive surgeries or addictive medications, chiropractic care uses non-invasive techniques to restore skeletal alignment, improve circulation, and calm inflammation, all while keeping your heart from staging a mutiny. Let’s delve into how Dr. Jimenez’s methods can resurrect your skeletal and cardiovascular health.
Spinal Manipulation: The Art of Cracking the Code
Spinal manipulation, the cornerstone of chiropractic care, involves applying controlled force to misaligned vertebrae to restore proper alignment. Think of it as realigning the crooked tombstones in a haunted graveyard. By correcting subluxations, chiropractic adjustments reduce nerve compression, improve blood flow, and alleviate pain. A 2022 study found that spinal manipulation significantly reduced low-back pain and improved function in patients, suggesting its efficacy for musculoskeletal issues (Roseen et al., 2022). This improved alignment can also enhance cardiovascular health by reducing nerve interference that affects heart rate and blood pressure regulation.
For instance, a misaligned thoracic spine can compress nerves that innervate the heart, leading to irregular heart rhythms or increased blood pressure. By realigning the spine, Dr. Jimenez ensures that these nerves can function without interference, allowing the cardiovascular system to operate like a well-oiled guillotine. This is particularly crucial for patients with hypertension, as improved spinal alignment can lower blood pressure, reducing the risk of heart disease (Goertz et al., 2017).
Functional Medicine: A Holistic Hex
Dr. Jimenez’s dual licensure as a chiropractor and board-certified nurse practitioner allows him to weave functional medicine into his practice, addressing the root causes of dysfunction rather than just masking symptoms. Functional medicine is like a detective story, uncovering hidden culprits like nutritional deficiencies, hormonal imbalances, or environmental toxins that haunt both skeletal and cardiovascular health. For example, inadequate calcium or vitamin D can weaken bones, while omega-3 deficiencies can exacerbate inflammation, clog arteries, and stress the heart.
At El Paso Back Clinic, Dr. Jimenez uses advanced diagnostic tools, such as the Living Matrix Functional Medicine Assessment, to create a comprehensive health profile. This includes evaluating genetics, lifestyle, and environmental exposures to design personalized treatment plans. By incorporating nutritional counseling, he ensures patients consume anti-inflammatory foods—like fatty fish and leafy greens—that support bone health and reduce cardiovascular risk (El Paso Back Clinic, n.d.). This holistic approach is like banishing a poltergeist by cleansing the entire house, not just one creaky room.
Advanced Diagnostics: X-Rays, MRIs, and the Crystal Ball
Dr. Jimenez’s use of advanced imaging, such as X-rays and MRIs, is like peering into a crystal ball to reveal hidden skeletal and soft tissue damage. These tools allow him to pinpoint the exact source of pain, whether it’s a herniated disc, spinal stenosis, or a pinched nerve, ensuring precise treatment plans. For personal injury cases, such as motor vehicle accidents (MVAs), these diagnostics are critical for documenting injuries for legal purposes, making Dr. Jimenez an invaluable liaison between medical care and legal documentation.
For example, a whiplash injury from an MVA can cause subtle spinal misalignments that impair blood flow to the brain and heart, leading to dizziness or cardiovascular strain. Dr. Jimenez’s dual-scope approach—combining chiropractic assessments with medical evaluations—ensures that both the biomechanical and systemic effects are addressed. A 2023 study highlighted the effectiveness of chiropractic care in reducing pain and improving mobility in MVA patients, underscoring its role in comprehensive recovery (Jenks et al., 2023).
References
- El Paso Back Clinic. (n.d.). Nutritional strategies for health and pain management. https://elpasobackclinic.com/nutritional-strategies-health/
- Goertz, C. M., Long, C. R., Vining, R. D., Pohlman, K. A., Walter, J., & Coulter, I. (2017). Effect of usual medical care plus chiropractic care vs usual medical care alone on pain and disability among US service members with low back pain: A comparative effectiveness clinical trial. JAMA Network Open, 1(1), e180105. https://pubmed.ncbi.nlm.nih.gov/28392856/
- Jenks, A. D., Hoekstra, T., Axén, I., de Luca, K., & Field, J. (2023). Association between manual therapy and manipulative therapy for low back pain and pain reduction and function improvement: A systematic review and meta-analysis. Journal of Manual & Manipulative Therapy, 31(4), 243–256. https://pubmed.ncbi.nlm.nih.gov/37130821/
- Jimenez, A. (2025). Dr. Alexander Jimenez, DC, APRN, FNP-BC, IFMCP, CFMP, ATN ♛ – Injury Medical Clinic PA | LinkedIn. https://www.linkedin.com/in/dralexjimenez/
- Roseen, E. J., Ward, R. E., Peterson, C. K., & Brown, R. (2022). Spinal manipulative therapy for acute low back pain: An update of the evidence. Spine Journal, 22(10), 1678–1689. https://pubmed.ncbi.nlm.nih.gov/36193397/
Atherosclerosis: The Joint-Pain Connection- Video
Dr. Jimenez: El Paso’s Dark Knight of Personal Injury Recovery
In the sun-scorched streets of El Paso, where car accidents and workplace injuries lurk like ghouls in the shadows, Dr. Alex Jimenez emerges as a beacon of hope for personal injury victims. His Injury Medical & Chiropractic Clinic is a fortress of healing, where advanced diagnostics, dual-scope procedures, and a compassionate approach converge to resurrect patients from the brink of despair. Whether you’ve been rear-ended in a fender-bender or mangled in an 18-wheeler crash, Dr. Jimenez’s expertise ensures you’re not left to haunt the earth in pain.
Dual-Scope Expertise: A Two-Headed Monster of Healing
Dr. Jimenez’s unique blend of chiropractic and nurse practitioner licensure is like a two-headed monster, terrifying to pain and dysfunction but a savior to patients. As a chiropractor, he restores musculoskeletal function through spinal adjustments, manual therapies, and rehabilitation exercises. As a nurse practitioner, he conducts thorough medical assessments, using blood panels and metabolic evaluations to uncover systemic issues that exacerbate skeletal and cardiovascular problems. This dual-scope approach allows him to connect the dots between a patient’s injuries and their broader health, ensuring no stone—or bone—is left unturned.
For personal injury cases, this expertise is a game-changer. After an MVA, Dr. Jimenez uses X-rays and MRIs to document spinal misalignments, herniated discs, or soft tissue injuries, providing detailed reports for insurance claims or legal proceedings. His ability to bridge medical care and legal documentation is like a grim alchemist turning pain into justice, ensuring patients receive both healing and compensation. A 2021 study emphasized the importance of detailed diagnostic imaging in personal injury cases, noting its role in validating claims and guiding treatment (Smith et al., 2021).
Personal Injury in El Paso: A Ghoulish Reality
El Paso’s bustling roads and industrial workplaces are a breeding ground for personal injuries, from whiplash in minor collisions to severe spinal trauma in 18-wheeler crashes. These injuries don’t just break bones; they disrupt lives, haunting victims with chronic pain, reduced mobility, and financial stress. Dr. Jimenez’s clinic specializes in these cases, offering tailored care plans that address both immediate pain and long-term recovery. His team’s use of the “PUSH-as-Rx ®™ System” combines strength training, mobility exercises, and nutritional counseling to rebuild patients from the ground up, like reconstructing a shattered gargoyle.
For example, a patient like Tina Medley, who suffered debilitating pain after a car accident, found relief through Dr. Jimenez’s integrative approach. By combining spinal adjustments with nutritional strategies to reduce inflammation, he helped her reclaim her life, proving that even the darkest injuries can have a light at the end of the tunnel (El Paso Back Clinic, 2020).
References
- El Paso Back Clinic. (2020). Aligned & Empowered: Chiropractic Conversations on Women’s Health | El Paso, TX (2020). https://elpasobackclinic.com/
- Smith, J. A., Brown, K. L., & Thompson, R. W. (2021). Diagnostic imaging in personal injury cases: A review of clinical and legal implications. Journal of Chiropractic Medicine, 20(1), 12–19. https://pubmed.ncbi.nlm.nih.gov/33593350/
- Jimenez, A. (2025). Dr. Alexander Jimenez, DC, APRN, FNP-BC, IFMCP, CFMP, ATN ♛ – Injury Medical Clinic PA | LinkedIn. https://www.linkedin.com/in/dralexjimenez/
The Cardiovascular-Skeletal Connection: A Clinical Autopsy
Let’s dissect the gruesome details of how skeletal health impacts the cardiovascular system and vice versa, with clinical insights from Dr. Jimenez’s practice. This connection is like a twisted love story between two systems that can’t live without each other but occasionally drive each other to an early grave.
Skeletal Misalignments and Cardiovascular Chaos
A misaligned spine is like a poorly tuned violin, producing discordant notes that disrupt the entire orchestra. Subluxations in the cervical or thoracic spine can compress nerves that regulate heart function, leading to arrhythmias or elevated blood pressure. This is because the autonomic nervous system, which controls involuntary functions like heart rate, runs through the spine. A 2022 study found that spinal manipulation can reduce sympathetic nervous system activity, lowering blood pressure and improving cardiovascular function (Wirth et al., 2022).
Dr. Jimenez’s approach involves precise adjustments to restore spinal alignment, relieving nerve pressure and improving circulation. For example, a patient with chronic neck pain may experience reduced blood flow to the brain, causing dizziness or fatigue—symptoms that mimic cardiovascular issues. By correcting the cervical spine, Dr. Jimenez ensures blood vessels can deliver oxygen efficiently, keeping the heart from throwing a tantrum.
Cardiovascular Health and Bone Decay
On the flip side, cardiovascular problems can cast a dark shadow over skeletal health. Atherosclerosis, the buildup of plaque in arteries, reduces blood flow to bones, starving them of nutrients and oxygen. This can lead to osteoporosis, where bones become as brittle as a vampire’s patience. Additionally, chronic inflammation from cardiovascular diseases like hypertension can erode joint cartilage, exacerbating conditions like arthritis.
Dr. Jimenez counters this with nutritional strategies that support both systems. Foods rich in omega-3 fatty acids, magnesium, and antioxidants—like salmon, spinach, and berries—reduce inflammation and strengthen bones while protecting arteries from plaque buildup. His clinic’s focus on metabolic optimization ensures patients maintain a healthy weight and hormone levels, reducing stress on both the heart and skeleton (El Paso Back Clinic, n.d.).
Overlapping Risk Profiles: The Shared Villains
Obesity, inactivity, and inflammation are the three horsemen of the apocalypse for skeletal and cardiovascular health. Excess weight strains joints and bones, accelerating wear and tear, while forcing the heart to work overtime, increasing the risk of heart failure. A sedentary lifestyle weakens muscles and bones, reducing stability and inviting fractures, while slowing circulation and raising the risk of blood clots. Inflammation, the sneakiest villain, fuels both arthritis and atherosclerosis, creating a feedback loop of misery.
Dr. Jimenez’s integrative approach slays these demons with a combination of chiropractic adjustments, exercise regimens, and nutritional counseling. His “PUSH-as-Rx ®™ System” incorporates agility training and strength exercises to improve mobility and circulation, while his functional medicine protocols address inflammation at its source, ensuring patients don’t spiral into a pit of despair.
References
- El Paso Back Clinic. (n.d.). Nutritional strategies for health and pain management. https://elpasobackclinic.com/nutritional-strategies-health/
- Wirth, B., Gassner, A., & de Bruin, E. D. (2022). Effects of spinal manipulative therapy on cardiovascular autonomic control: A systematic review. Journal of Manipulative and Physiological Therapeutics, 45(7), 529–540. https://pubmed.ncbi.nlm.nih.gov/36231242/
- Jimenez, A. (2025). Dr. Alexander Jimenez, DC, APRN, FNP-BC, IFMCP, CFMP, ATN ♛ – Injury Medical Clinic PA | LinkedIn. https://www.linkedin.com/in/dralexjimenez/
Personal Injury Recovery: A Dance with the Legal Reaper
Personal injury cases in El Paso are no laughing matter—unless you find the irony of a fender-bender turning your life into a tragic comedy. From whiplash to herniated discs, MVAs can leave victims grappling with pain, medical bills, and insurance disputes. Dr. Jimenez steps into this grim tableau as both healer and advocate, using his dual expertise to guide patients through recovery and legal battles.
The Aftermath of MVAs: A Skeletal and Cardiovascular Nightmare
Car accidents are like a surprise visit from a poltergeist, leaving chaos in their wake. Whiplash, a common MVA injury, can misalign the cervical spine, compressing nerves and blood vessels, leading to headaches, dizziness, and cardiovascular strain. Herniated discs, another frequent injury, can pinch spinal nerves, causing pain and reducing mobility, which in turn slows circulation and stresses the heart. Dr. Jimenez’s clinic specializes in these injuries, using spinal decompression, manual therapy, and rehabilitation to restore function and prevent long-term damage.
Advanced Diagnostics: Peeling Back the Veil
Dr. Jimenez’s use of X-rays, MRIs, and functional assessments is like conducting a post-mortem on your injuries, revealing hidden damage that could haunt you later. These tools are critical for personal injury cases, as they provide objective evidence for insurance claims and legal proceedings. For example, an MRI can detect a herniated disc that’s compressing a nerve, explaining a patient’s chronic pain and justifying their need for ongoing care. This documentation is essential for securing compensation, as it links injuries directly to the accident (Smith et al., 2021).
Legal-Medical Liaison: Dr. Jimenez’s Dark Art
Dr. Jimenez’s ability to serve as a liaison between medical care and legal documentation is his secret weapon. His detailed reports translate complex medical findings into clear, legally admissible evidence, ensuring patients receive fair compensation. This is particularly vital in El Paso, where personal injury cases are common due to heavy traffic and industrial activity. His dual-scope approach—combining chiropractic and medical expertise—ensures that both the physical and systemic effects of injuries are addressed, making him a trusted ally for attorneys and patients alike.
References
- El Paso Back Clinic. (n.d.). Chiropractic care for motor vehicle accident recovery. https://elpasobackclinic.com/
- Smith, J. A., Brown, K. L., & Thompson, R. W. (2021). Diagnostic imaging in personal injury cases: A review of clinical and legal implications. Journal of Chiropractic Medicine, 20(1), 12–19. https://pubmed.ncbi.nlm.nih.gov/33593350/
- Jimenez, A. (2025). Dr. Alexander Jimenez, DC, APRN, FNP-BC, IFMCP, CFMP, ATN ♛ – Injury Medical Clinic PA | LinkedIn. https://www.linkedin.com/in/dralexjimenez/
A Day in the Life: How Dysfunction Haunts Your Routine
Imagine waking up with a spine so stiff it feels like it’s been possessed by a vengeful spirit. You shuffle to the bathroom, wincing as your joints creak like a haunted mansion’s floorboards. Your heart, overworked from poor circulation caused by spinal misalignments, pounds like a drum at a midnight ritual. This is the daily reality for those with compromised skeletal and cardiovascular health, where simple tasks become a descent into purgatory.
The Morning Misery
Getting out of bed with back pain or arthritis is like escaping a coffin nailed shut. Poor skeletal health limits mobility, making every step a negotiation with pain. Meanwhile, reduced blood flow from cardiovascular issues can cause fatigue, leaving you feeling like a zombie before your first cup of coffee. Dr. Jimenez’s chiropractic adjustments can realign the spine, reducing nerve compression and improving circulation, so you can start your day without feeling like you’re auditioning for a horror movie.
The Afternoon Agony
By midday, sitting at a desk or standing for hours can turn your spine into a torture rack. Misaligned vertebrae compress nerves, causing pain that radiates like a curse. This can also strain the cardiovascular system, as poor posture restricts blood flow, forcing the heart to work harder. Dr. Jimenez’s mobility exercises and nutritional counseling can strengthen muscles and reduce inflammation, ensuring you don’t spend your lunch break plotting revenge against your own body.
The Evening Exhaustion
By evening, the cumulative stress of skeletal and cardiovascular dysfunction can leave you too drained to enjoy life’s pleasures, like chasing your kids or binge-watching a gothic drama. Chronic pain and fatigue sap your energy, while poor circulation increases the risk of blood clots, a silent killer lurking in the shadows. Dr. Jimenez’s integrative approach, combining spinal manipulation with lifestyle interventions, can restore vitality, letting you reclaim your evenings without feeling like you’re starring in a tragedy.
References
- El Paso Back Clinic. (n.d.). Nutritional strategies for health and pain management. https://elpasobackclinic.com/nutritional-strategies-health/
- Jimenez, A. (2025). Dr. Alexander Jimenez, DC, APRN, FNP-BC, IFMCP, CFMP, ATN ♛ – Injury Medical Clinic PA | LinkedIn. https://www.linkedin.com/in/dralexjimenez/
Conclusion: A Serious Note to Banish the Shadows
While we’ve danced with dark humor to make this journey through skeletal and cardiovascular health more palatable, the stakes are deadly serious. Chronic pain, reduced mobility, and cardiovascular strain are no laughing matter—they can rob you of your quality of life and shorten your time on this mortal plane. Dr. Alex Jimenez and his team at El Paso Back Clinic offer a lifeline, using chiropractic care, functional medicine, and advanced diagnostics to address the root causes of dysfunction. Whether you’re recovering from a personal injury or battling chronic conditions, their holistic approach can restore your health and empower you to live fully.
Disclaimer: This blog post is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare provider with any questions you may have regarding a medical condition. The information provided is based on clinical insights and research, but should not replace a one-on-one consultation with a licensed professional like Dr. Alexander Jimenez, DC, APRN, FNP-BC. For personalized care, contact El Paso Back Clinic at 915-850-0900 or visit https://elpasobackclinic.com/.
References
- El Paso Back Clinic. (n.d.). Nutritional strategies for health and pain management. https://elpasobackclinic.com/nutritional-strategies-health/
- El Paso Back Clinic. (2020). Aligned & Empowered: Chiropractic Conversations on Women’s Health | El Paso, TX (2020). https://elpasobackclinic.com/
- Goertz, C. M., Long, C. R., Vining, R. D., Pohlman, K. A., Walter, J., & Coulter, I. (2017). Effect of usual medical care plus chiropractic care vs usual medical care alone on pain and disability among US service members with low back pain: A comparative effectiveness clinical trial. JAMA Network Open, 1(1), e180105. https://pubmed.ncbi.nlm.nih.gov/28392856/
- Jenks, A. D., Hoekstra, T., Axén, I., de Luca, K., & Field, J. (2023). Association between manual therapy and manipulative therapy for low back pain and pain reduction and function improvement: A systematic review and meta-analysis. Journal of Manual & Manipulative Therapy, 31(4), 243–256. https://pubmed.ncbi.nlm.nih.gov/37130821/
- Jimenez, A. (2025). Dr. Alexander Jimenez, DC, APRN, FNP-BC, IFMCP, CFMP, ATN ♛ – Injury Medical Clinic PA | LinkedIn. https://www.linkedin.com/in/dralexjimenez/
- Roseen, E. J., Ward, R. E., Peterson, C. K., & Brown, R. (2022). Spinal manipulative therapy for acute low back pain: An update of the evidence. Spine Journal, 22(10), 1678–1689. https://pubmed.ncbi.nlm.nih.gov/36193397/
- Smith, J. A., Brown, K. L., & Thompson, R. W. (2021). Diagnostic imaging in personal injury cases: A review of clinical and legal implications. Journal of Chiropractic Medicine, 20(1), 12–19. https://pubmed.ncbi.nlm.nih.gov/33593350/
- Wirth, B., Gassner, A., & de Bruin, E. D. (2022). Effects of spinal manipulative therapy on cardiovascular autonomic control: A systematic review. Journal of Manipulative and Physiological Therapeutics, 45(7), 529–540. https://pubmed.ncbi.nlm.nih.gov/36231242/