Understanding Laser Spine Surgery: A Minimally Invasive Approach
For individuals who have exhausted all other treatment options for low back pain and nerve root compression, can laser spine surgery help alleviate nerve compression and provide long-lasting pain relief?

Laser Spine Surgery
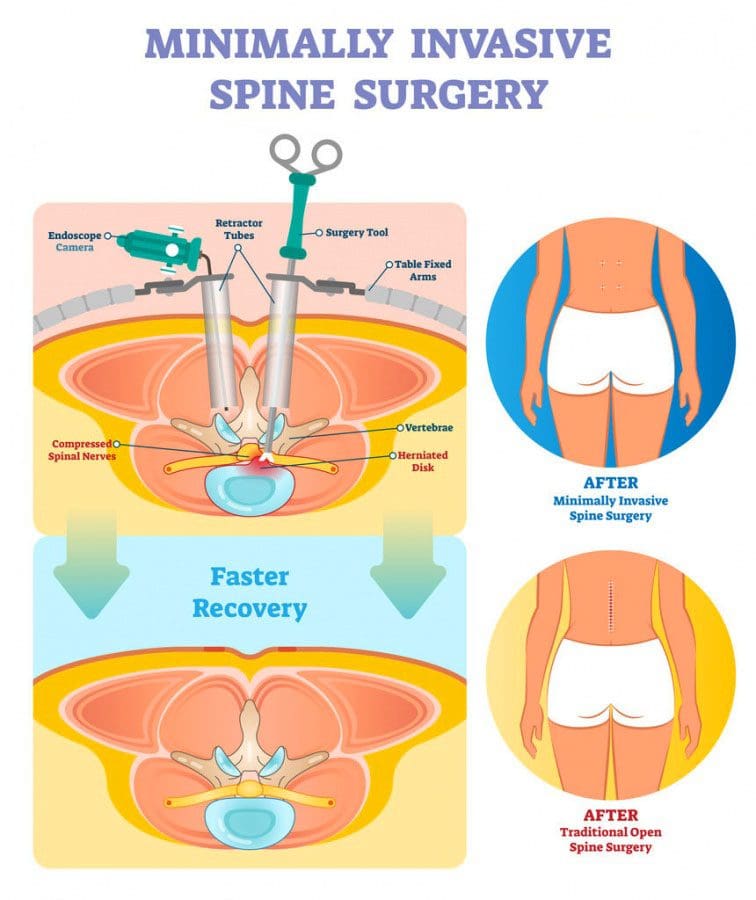
Laser spine surgery is a minimally invasive surgical procedure that uses a laser to cut through and remove spinal structures that are compressing nerves and causing intense pain. The minimally invasive procedure often results in less pain, tissue damage, and faster recovery than more extensive surgeries.
How It Works
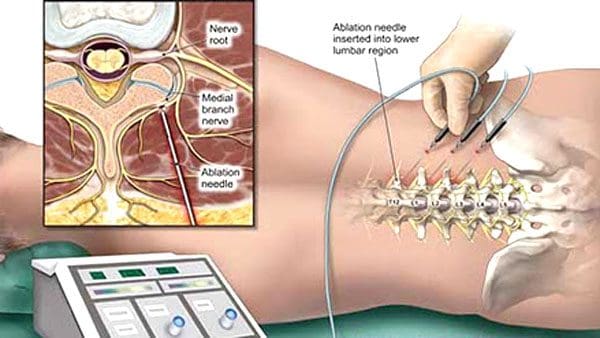
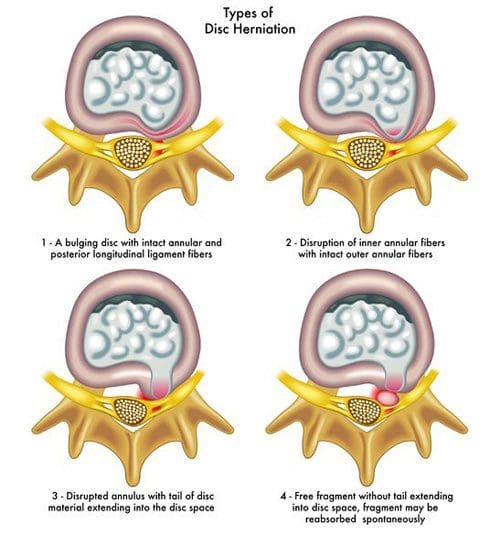
Minimally invasive procedures result in less scarring and damage to surrounding structures, often reducing pain symptoms and a shorter recovery time. (Stern, J. 2009) Small incisions are made to access spinal column structures. With open-back surgery, a large incision is made down the back to access the spine. The surgery differs from other surgeries in that a laser beam, rather than other surgical instruments, is used to cut structures in the spine. However, the initial incision through the skin is made with a surgical scalpel. Laser is an acronym for Light Amplification Stimulated by Emission of Radiation. A laser can generate intense heat to cut through soft tissues, especially those with a high water content, like spinal column discs. (Stern, J. 2009) For many spine surgeries, the laser cannot be used to cut through bone as it generates instant sparks that can damage surrounding structures. Rather, laser spine surgery is primarily used to perform a discectomy, which is a surgical technique that removes a portion of a bulging or herniated disc that is pushing against the surrounding nerve roots, causing nerve compression and sciatic pain. (Stern, J. 2009)
Surgical Risks
Laser spine surgery may help resolve the cause of nerve root compression, but there is an increased risk of damage to nearby structures. Associated risks include: (Brouwer, P. A. et al., 2015)
- Infection
- Bleeding
- Blood clots
- Remaining symptoms
- Returning symptoms
- Further nerve damage
- Damage to the membrane around the spinal cord.
- Need for additional surgery
A laser beam is not precise like other surgical tools and requires practiced mastery and control to avoid damage to the spinal cord and nerve roots. (Stern, J. 2009) Because lasers cannot cut through bone, other surgical instruments are often used around corners and at different angles because they are more efficient and allow greater accuracy. (Atlantic Brain and Spine, 2022)
Purpose
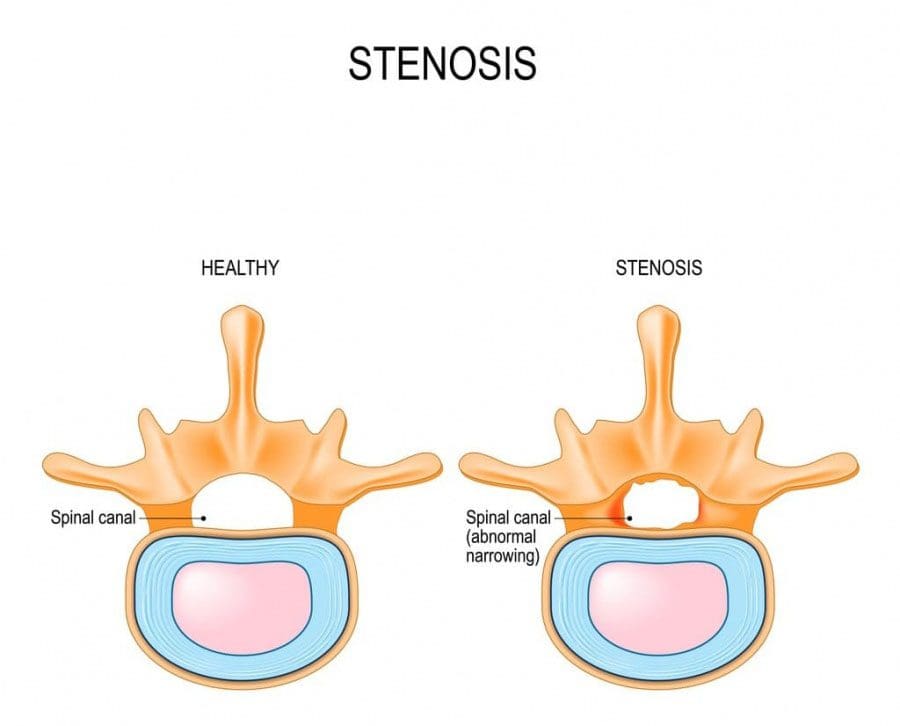
Laser spine surgery is performed to remove structures that are causing nerve root compression. Nerve root compression is associated with the following conditions (Cleveland Clinic. 2018)
- Bulging discs
- Herniated discs
- Sciatica
- Spinal stenosis
- Spinal cord tumors
Nerve roots that are injured or damaged and constantly send chronic pain signals can be ablated with laser surgery, known as nerve ablation. The laser burns and destroys the nerve fibers. (Stern, J. 2009) Because laser spine surgery is limited in treating certain spinal disorders, most minimally invasive spine procedures do not use a laser. (Atlantic Brain and Spine. 2022)
Preparation
The surgical team will provide more detailed instructions on what to do in the days and hours before surgery. To promote optimal healing and a smooth recovery, it is recommended that the patient stay active, eat a healthy diet, and stop smoking prior to the operation. Individuals may need to stop taking certain medications to prevent excess bleeding or interaction with anesthesia during the operation. Inform the healthcare provider about all prescriptions, over-the-counter drugs, and supplements being taken.
Laser spine surgery is an outpatient procedure at a hospital or outpatient surgical center. The patient will likely go home on the same day of the operation. (Cleveland Clinic. 2018) Patients cannot drive to or from the hospital before or after their surgery, so arrange for family or friends to provide transportation. Minimizing stress and prioritizing healthy mental and emotional well-being is important to lowering inflammation and aiding recovery. The healthier the patient goes into surgery, the easier the recovery and rehabilitation will be.
Expectations
The surgery will be decided by the patient and healthcare provider and scheduled at a hospital or outpatient surgical center. Arrange for a friend or family member to drive to the surgery and home.
Before Surgery
- The patient will be taken to a pre-operative room and asked to change into a gown.
- The patient will undergo a brief physical examination and answer questions about medical history.
- The patient lies on a hospital bed, and a nurse inserts an IV to deliver medication and fluids.
- The surgical team will use the hospital bed to transport the patient in and out of the operating room.
- The surgical team will assist the patient in getting onto the operating table, and the patient will be administered anesthesia.
- The patient may receive general anesthesia, which will cause the patient to sleep for the surgery, or regional anesthesia, injected into the spine to numb the affected area. (Cleveland Clinic. 2018)
- The surgical team will sterilize the skin where the incision will be made.
- An antiseptic solution will be used to kill bacteria and prevent the risk of infection.
- Once sanitized, the body will be covered with sterilized linens to keep the surgical site clean.
During Surgery
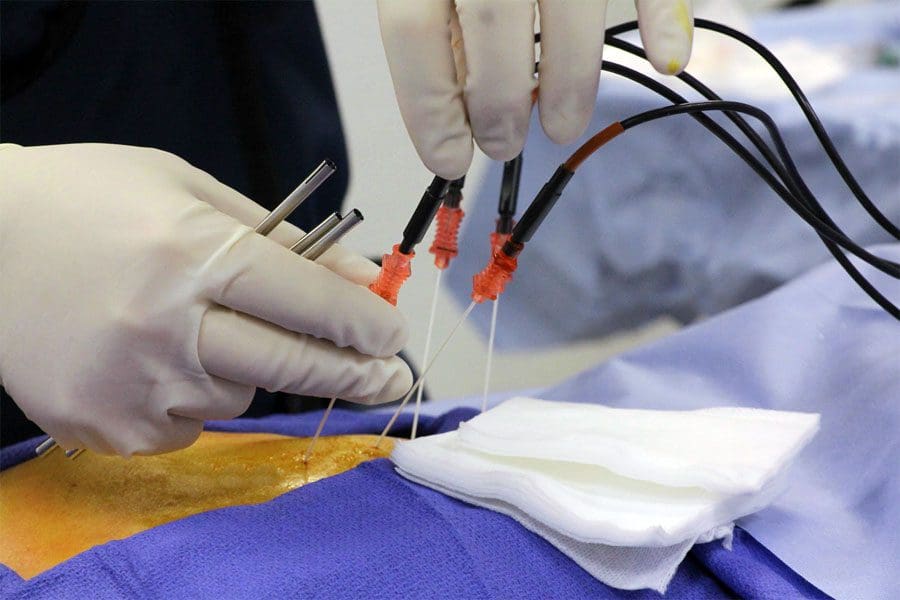
- For a discectomy, the surgeon will make a small incision less than one inch in length with a scalpel along the spine to access the nerve roots.
- A surgical tool called an endoscope is a camera inserted into the incision to view the spine. (Brouwer, P. A. et al., 2015)
- Once the problematic disc portion causing the compression is located, the laser is inserted to cut through it.
- The cut disc portion is removed, and the incision site is sutured.
After Surgery
- After surgery, the patient is brought to a recovery room, where vital signs are monitored as the effects of the anesthesia wear off.
- Once stabilized, the patient can usually go home one or two hours after the operation.
- The surgeon will determine when the individual is clear to resume driving.
Recovery
Following a discectomy, the individual can return to work within a few days to a few weeks, depending on the severity, but it can take up to three months to return to normal activities. Length of recovery can range from two to four weeks or less to resume a sedentary job or eight to 12 weeks for a more physically demanding job that requires heavy lifting. (University of Wisconsin School of Medicine and Public Health, 2021) During the first two weeks, the patient will be given restrictions to facilitate the spine’s healing until it becomes more stable. Restrictions can include: (University of Wisconsin School of Medicine and Public Health, 2021)
- No bending, twisting, or lifting.
- No strenuous physical activity, including exercise, housework, yard work, and sex.
- No alcohol in the initial stage of recovery or while taking narcotic pain medications.
- No driving or operating a motor vehicle until discussed with the surgeon.
The healthcare provider may recommend physical therapy to relax, strengthen, and maintain musculoskeletal health. Physical therapy may be two to three times weekly for four to six weeks.
Process
Optimal recovery recommendations include:
- Getting enough sleep, at least seven to eight hours.
- Maintaining a positive attitude and learning how to cope and manage stress.
- Maintaining body hydration.
- Following the exercise program as prescribed by the physical therapist.
- Practicing healthy posture with sitting, standing, walking, and sleeping.
- Staying active and limiting the amount of time spent sitting. Try to get up and walk every one to two hours during the day to stay active and prevent blood clots. Gradually increase the amount of time or distance as recovery progresses.
- Do not push to do too much too soon. Overexertion can increase pain and delay recovery.
- Learning correct lifting techniques to utilize the core and leg muscles to prevent increased pressure on the spine.
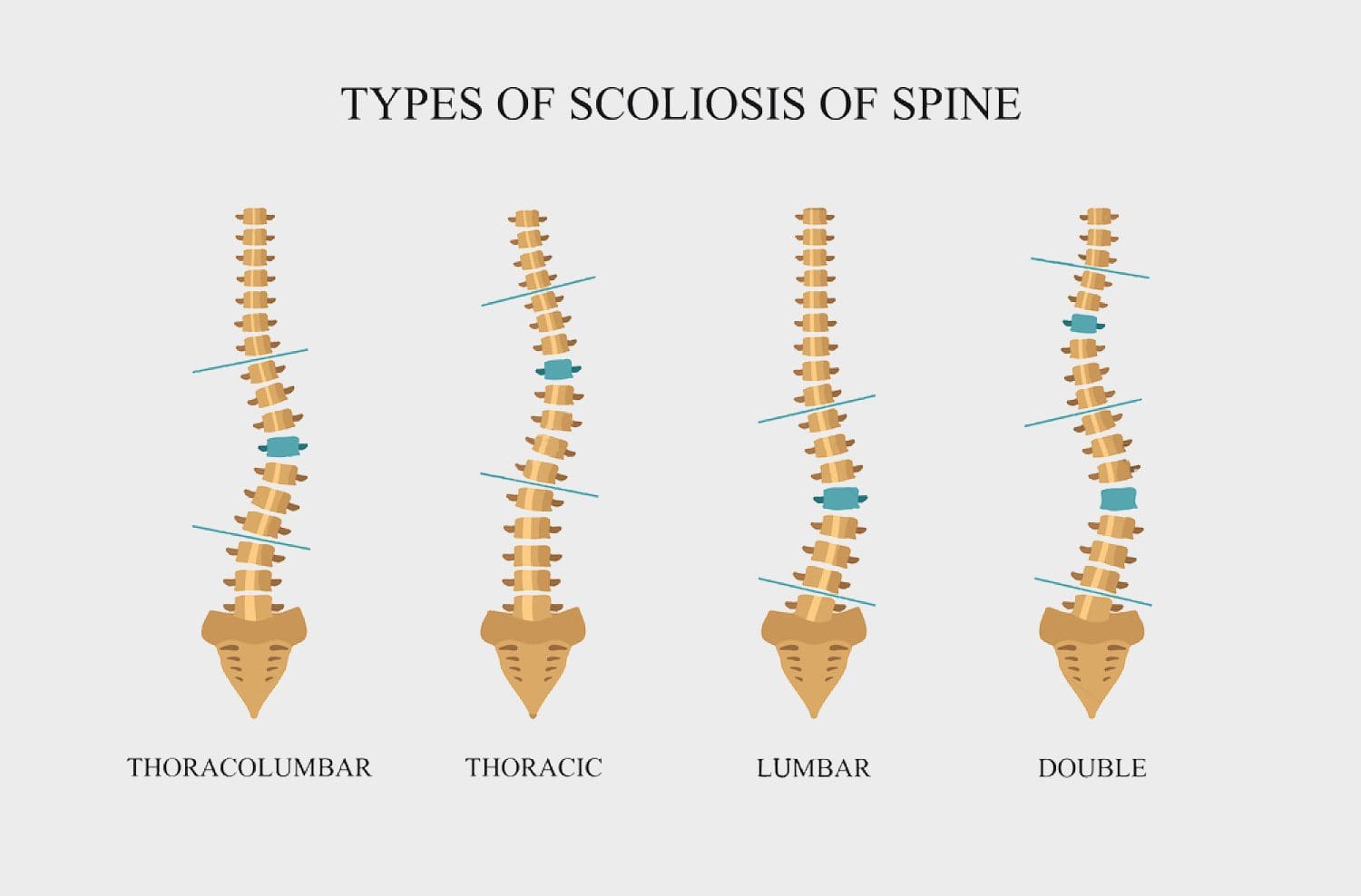
Discuss treatment options for managing symptoms with a healthcare provider or specialist to determine if laser spine surgery is appropriate. Injury Medical Chiropractic and Functional Medicine Clinic care plans and clinical services are specialized and focused on injuries and the complete recovery process. Dr. Jimenez has teamed with the top surgeons, clinical specialists, medical researchers, therapists, trainers, and premiere rehabilitation providers. We focus on restoring normal body functions after trauma and soft tissue injuries using Specialized Chiropractic Protocols, Wellness Programs, Functional and integrative Nutrition, Agility and mobility Fitness Training, and Rehabilitation Systems for all ages. Our areas of practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
The Non-Surgical Approach
References
Stern, J. SpineLine. (2009). Lasers in Spine Surgery: A Review. Current Concepts, 17-23. www.spine.org/Portals/0/assets/downloads/KnowYourBack/LaserSurgery.pdf
Brouwer, P. A., Brand, R., van den Akker-van Marle, M. E., Jacobs, W. C., Schenk, B., van den Berg-Huijsmans, A. A., Koes, B. W., van Buchem, M. A., Arts, M. P., & Peul, W. C. (2015). Percutaneous laser disc decompression versus conventional microdiscectomy in sciatica: a randomized controlled trial. The spine journal : official journal of the North American Spine Society, 15(5), 857–865. doi.org/10.1016/j.spinee.2015.01.020
Atlantic Brain and Spine. (2022). The Truth About Laser Spine Surgery [2022 Update]. Atlantic Brain and Spine Blog. www.brainspinesurgery.com/blog/the-truth-about-laser-spine-surgery-2022-update?rq=Laser%20Spine%20Surgery
Cleveland Clinic. (2018). Can Laser Spine Surgery Fix Your Back Pain? health.clevelandclinic.org/can-laser-spine-surgery-fix-your-back-pain/
University of Wisconsin School of Medicine and Public Health. (2021). Home Care Instructions after Lumbar Laminectomy, Decompression or Discectomy Surgery. patient.uwhealth.org/healthfacts/4466