Musculoskeletal Disorders
Musculoskeletal Disorders, or MSDs, are injuries, conditions, and disorders that affect the body’s musculoskeletal system. It includes the muscles, tendons, ligaments, nerves, discs, blood vessels, bones, and joints. MSDs are common, and the risk of developing them increases with age. The severity of an MSD can vary. They cause discomfort, recurrent pain, stiffness, swelling, and aching that interfere with everyday activities. Early diagnosis and treatment can alleviate symptoms and improve long-term health. Common disorders include:
- Tendonitis
- Tendon Strain
- Epicondylitis
- Carpal Tunnel Syndrome
- Trigger Finger
- Radial Tunnel Syndrome
- DeQuervain’s Syndrome
- Rotator Cuff Tendonitis
- Muscle strain
- Ligament Sprain
- Rheumatoid arthritis – RA
- Osteoarthritis
- Tension Neck Syndrome
- Thoracic Outlet Compression
- Mechanical Back Syndrome
- Degenerative Disc Disease
- Ruptured Disc
- Herniated Disc
- Fibromyalgia
- Digital Neuritis
- Bone Fractures
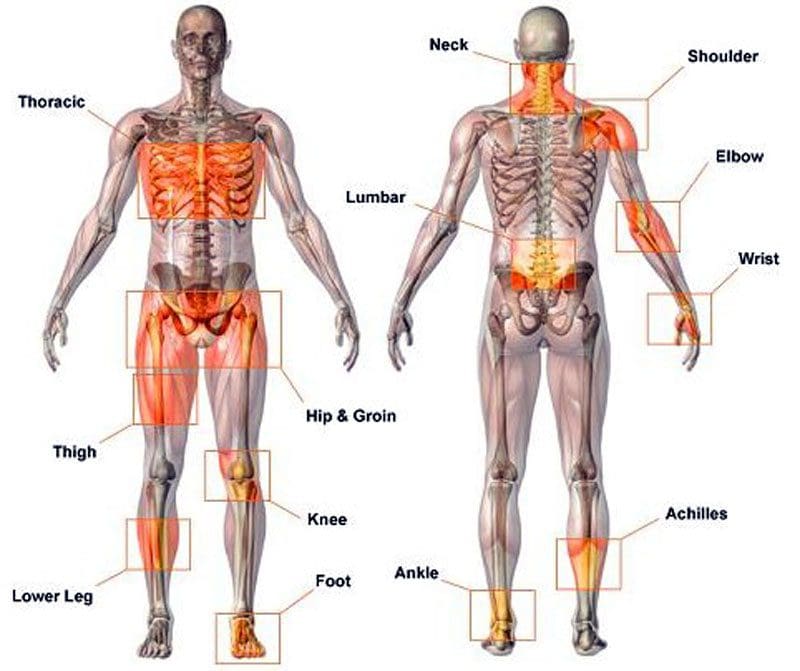
Musculoskeletal Disorders Discomfort and Pain
The term musculoskeletal disorder is used as it accurately describes the injury or condition. Other terms used are repetitive motion injury, repetitive stress injury, and overuse injury. When individuals are exposed to MSD risk factors, they begin to fatigue. This can start a musculoskeletal imbalance. With time, fatigue completely overtakes recovery/healing, and the musculoskeletal imbalance continues, a musculoskeletal disorder develops. The risk factors are broken into two categories: work-related/ergonomic risk factors and individual-related risk factors.
Ergonomic Factors:
- Force
- Repetition
- Posture
High Task Repetition
- Many work tasks and cycles are repetitive and are typically controlled by hourly or daily production targets and work processes.
- High task repetition combined with other risks factors like high force and/or awkward postures can contribute to the formation of MSD.
- A job is considered highly repetitive if the cycle time is 30 seconds or less.
Forceful Exertions
- Many job tasks require high force loads on the body.
- Muscle effort increases in response to high force requirements. This increases associated fatigue.
Repetitive or Sustained Awkward Postures
- Awkward postures place excessive force on joints, overload the muscles and tendons around affected joints.
- The joints of the body are most efficient when they operate close to the mid-range motion of the joint.
- The risk of MSD is increased when the joints are worked outside of this mid-range repetitively for sustained periods without a proper amount of recovery time.
Individual Factors
- Unhealthy work practices
- Lack of physical activity/fitness
- Unhealthy habits
- Poor diet
Unhealthy Work Practices
- Individuals that engage in poor work practices, body mechanics, and lifting techniques are introducing unnecessary risk factors.
- These poor practices create unnecessary stress on the body that increases fatigue and decreases the body’s ability to recover properly.
Poor Health Habits
- Individuals who smoke, drink excessively, are obese, or exhibit numerous other poor health habits put themselves at risk for musculoskeletal disorders and other chronic diseases.
Insufficient Rest and Recovery
- Individuals that do not get adequate rest and recovery put themselves at higher risk.
- MSDs develop when fatigue outruns the individual’s recovery system, causing a musculoskeletal imbalance.
Poor Diet, Fitness, and Hydration
- Individuals who eat unhealthily are dehydrated, at a poor level of physical fitness, and do not take care of their bodies are putting themselves at a higher risk of developing musculoskeletal and chronic health problems.
Causes
The causes of musculoskeletal disorders are varied. Muscle tissue can be damaged with the wear and tear of daily work, school, and physical activities. Trauma to the body can come from:
- Postural strain
- Repetitive movements
- Overuse
- Prolonged immobilization
- Jerking movements
- Sprains
- Dislocations
- Falling injuries
- Auto accident injuries
- Fractures
- Direct trauma to the muscle/s
Poor body mechanics can cause spinal alignment problems and muscle shortening, causing other muscles to be strained, causing problems and pain.
Treatment Rehabilitation
A doctor will recommend a treatment plan based on the diagnosis and severity of the symptoms. They may recommend moderate exercise and over-the-counter medications like ibuprofen or acetaminophen to address occasional discomfort or pain. They often recommend chiropractic and physical therapy rehabilitation to learn how to manage pain and discomfort, maintain strength, range of motion, and adjust everyday activities. Different types of manual therapy, or mobilization, can treat body alignment problems. A doctor may prescribe medications like nonsteroidal anti-inflammatories NSAIDs to reduce inflammation and pain for more severe symptoms. For individuals with musculoskeletal disorders like fibromyalgia, medications to increase the body’s level of serotonin and norepinephrine may be prescribed in low doses to modulate sleep, pain, and immune system function.
Body Composition
Types of Pain
Pain can be grouped into three categories:
Early Warning Pain
- This is most recognizable after having just touched a pan, and the hand jerks away before realizing how hot the pan is, also known as the withdrawal reflex.
- This is a protective mechanism that helps avoid danger and is vital for survival.
Inflammatory Pain
- This type of pain happens after an injury or surgery while the body is healing and recovering.
- Inflammation prevents the body from performing movements to prevent and avoid re-injury.
Pathological Pain
- This type of pain can happen after the body has healed, but the nervous system has been damaged.
- This is often the case with individuals who sustain an injury and inform doctors that the injured area is never the same.
- If the rehabilitation does not correctly heal the nervous system, protective pain measures can generate a false alarm causing pain signals to fire off.
References
Asada, Fuminari, and Kenichiro Takano. Nihon eiseigaku zasshi. Japanese journal of hygiene vol. 71,2 (2016): 111-8. doi:10.1265/jjh.71.111
da Costa, Bruno R, and Edgar Ramos Vieira. “Risk factors for work-related musculoskeletal disorders: A systematic review of recent longitudinal studies.” American journal of industrial medicine vol. 53,3 (2010): 285-323. doi:10.1002/ajim.20750
Malińska, Marzena. “Dolegliwości układu mięśniowo-szkieletowego u operatorów komputerowych” [Musculoskeletal disorders among computer operators]. Medycyna pracy vol. 70,4 (2019): 511-521. doi:10.13075/mp.5893.00810
Musculoskeletal system diseases. (n.d.). dmu.edu/medterms/musculoskeletal-system/musculoskeletal-system-diseases/
Roquelaure, Yves et al. “Troubles musculo-squelettiques liés au travail” [Work-related musculoskeletal disorders]. La Revue du praticien vol. 68,1 (2018): 84-90.
Villa-Forte A. (n.d.). Diagnosis of musculoskeletal disorders. merckmanuals.com/home/bone,-joint,-and-muscle-disorders/diagnosis-of-musculoskeletal-disorders/introduction
Work-related musculoskeletal disorders (WMSDs). (2014). ccohs.ca/oshanswers/diseases/rmirsi.html