Migraine Pain & Lumbar Herniated Disc Treatment in El Paso, TX
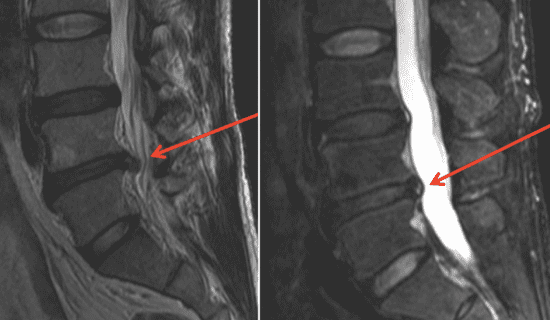
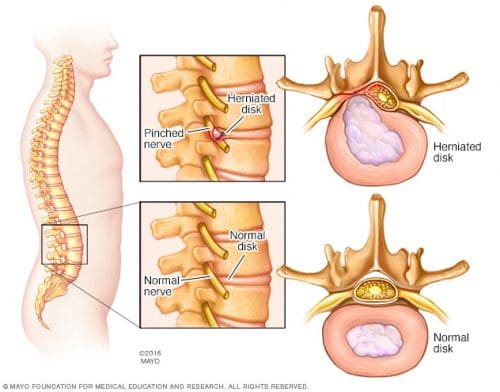
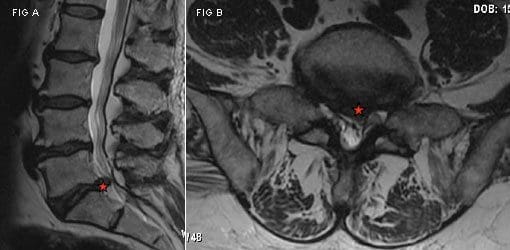
One of the most prevalent causes of lower back pain and sciatica may be due to the compression of the nerve roots in the low back from a lumbar herniated disc, or a ruptured disc in the lumbar spine. Common symptoms of lumbar herniated discs include varying intensities of pain, muscle spasms or cramping, sciatica and leg weakness as well as loss of proper leg function. While these may not appear to be closely associated with each other, a lumbar herniated disc may also affect the cervical spine, manifesting symptoms of migraine and headache. The purpose of the following articles is to educate patients and demonstrate the relation between migraine pain and lumbar herniated disc, further discussing the treatment of these two common conditions.
A Critical Review of Manual Therapy Use for Headache Disorders: Prevalence, Profiles, Motivations, Communication and Self-Reported Effectiveness
Abstract
Background
Despite the expansion of conventional medical treatments for headache, many sufferers of common recurrent headache disorders seek help outside of medical settings. The aim of this paper is to evaluate research studies on the prevalence of patient use of manual therapies for the treatment of headache and the key factors associated with this patient population.
Methods
This critical review of the peer-reviewed literature identified 35 papers reporting findings from new empirical research regarding the prevalence, profiles, motivations, communication and self-reported effectiveness of manual therapy use amongst those with headache disorders.
Results
While available data was limited and studies had considerable methodological limitations, the use of manual therapy appears to be the most common non-medical treatment utilized for the management of common recurrent headaches. The most common reason for choosing this type of treatment was seeking pain relief. While a high percentage of these patients likely continue with concurrent medical care, around half may not be disclosing the use of this treatment to their medical doctor.
Conclusions
There is a need for more rigorous public health and health services research in order to assess the role, safety, utilization and financial costs associated with manual therapy treatment for headache. Primary healthcare providers should be mindful of the use of this highly popular approach to headache management in order to help facilitate safe, effective and coordinated care.
Keywords: Headache, Migraine, Tension headache, Cervicogenic headache, Manual therapy, Physical therapy, Chiropractic, Osteopathy, Massage
Background
The co-occurrence of tension headache and migraine is very high [1]. Respectively, they are the second and third most common disorders worldwide with migraine ranking as the seventh highest specific cause of disability globally [2] and the sixteenth most commonly diagnosed condition in the US [3]. These common recurrent headache disorders place a considerable burden upon the personal health, finances and work productivity of sufferers [3�5] with migraine further complicated by an association with cardiovascular and psychiatric co-morbidities [6, 7].
Preventative migraine drug treatments include analgesics, anticonvulsants, antidepressants and beta-blockers. Preventative drug treatments for tension-type headaches can include analgesics, NSAIDs, muscle relaxants and botulinum toxin as well as anticonvulsants and antidepressants. While preventative drug treatments are successful for a significant proportion of sufferers, headache disorders are still reported as under-diagnosed and under-treated within medical settings [8�16] with other studies reporting sufferers can cease continuing with preventative headache medications long-term [9, 17].
There is a number of non-drug approaches also utilized for the prevention of headaches. These include psychological therapies such as cognitive behavioral therapy, relaxation training and EMG (electromyography) biofeedback. In addition, there is acupuncture, nutritional supplementation (including magnesium, B12, B6, and Coenzyme Q10) and physical therapies. The use of physical therapies is significant, with one recent global survey reporting physical therapy as the most frequently used �alternative or complementary treatment� for headache disorders across many countries [18]. One of the most common physical therapy interventions for headache management is manual therapy (MT), [19�21] which we define here as treatments including �spinal manipulation (as commonly performed by chiropractors, osteopaths, and physical therapists), joint and spinal mobilization, therapeutic massage, and other manipulative and body-based therapies� [22].
Positive results have been reported in many clinical trials comparing MT to controls [23�27], other physical therapies [28�30] and aspects of medical care [31�34]. More high quality research is needed however to assess the efficacy of MT as a treatment for common recurrent headaches. Recent systematic reviews of randomized clinical trials of MT for the prevention of migraine report a number of significant methodological short-comings and the need for more high quality research before any firm conclusions can be made [35, 36]. Recent reviews of MT trials for tension-type headache and cervicogenic headache are cautious in reporting positive outcomes and the strong need for further robust research [37�41]. Despite the limited clinical evidence there has been no critical review of the significant use of MT by headache populations.
Methods
The aim of this study is to report from the peer-reviewed literature; 1) the prevalence of MT use for the treatment of common recurrent headaches and 2) factors associated with this use across several key themes. The review further identifies key areas worthy of further research in order to better inform clinical practice, educators and healthcare policy within this area.
Design
A comprehensive search of peer-reviewed articles published in English between 2000 and 2015 reporting new empirical research findings of key aspects of MT use among patients with migraine and non-migraine headache disorders was undertaken. Databases searched were MEDLINE, AMED, CINAHL, EMBASE and EBSCO. The key words and phrases used were: �headache�, �migraine�, �primary headache�, �cephalgia�, �chronic headache� AND �manual therapy�, �spinal manipulation�, �manipulative therapy�, �spinal mobilization�, �chiropractic�, �osteopathy�, �massage�, �physical therapy� or �physiotherapy� AND then �prevalence�, �utilization� or �profile� was used for additional searches against the previous terms. The database search was accompanied by a hand search of prominent peer-reviewed journals. All authors accessed the reviewed literature (data) and provided input to analysis.
Due to the focus of the review, literature reporting randomized control trials and similar clinical research designs were excluded as were articles identified as letters, correspondence, editorials, case reports and commentaries. Further searches were undertaken of the bibliographies in the identified publications. All identified articles were screened and only those reporting new empirical findings on MT use for headache in adults were included in the review. Articles identified and selected for the review were research manuscripts mostly within epidemiological and health economics studies. The review includes papers reporting MT use pooled with the use of other therapies, but only where MT patients comprised a large proportion (as stated) of the included study population. Results were imported into Endnote X7 and duplicates removed.
Search Outcomes, Analyses and Quality Appraisal
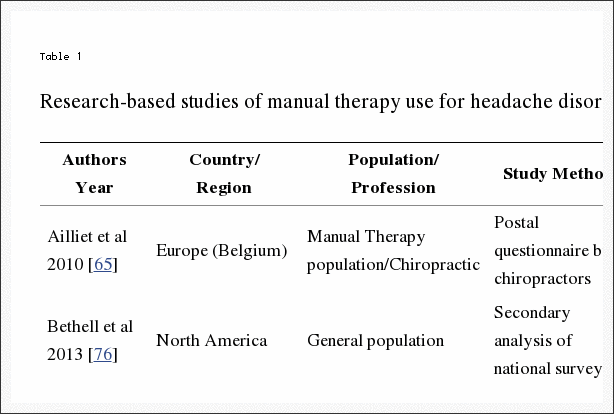
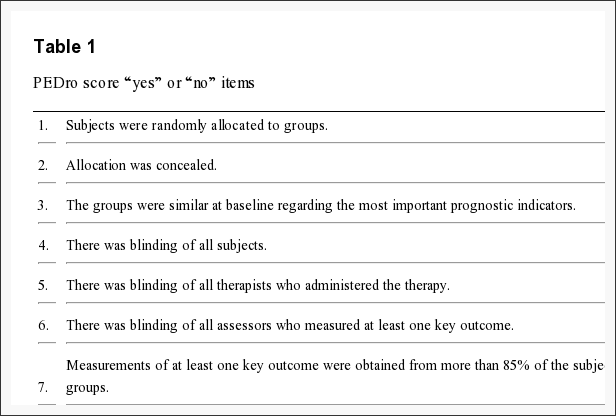
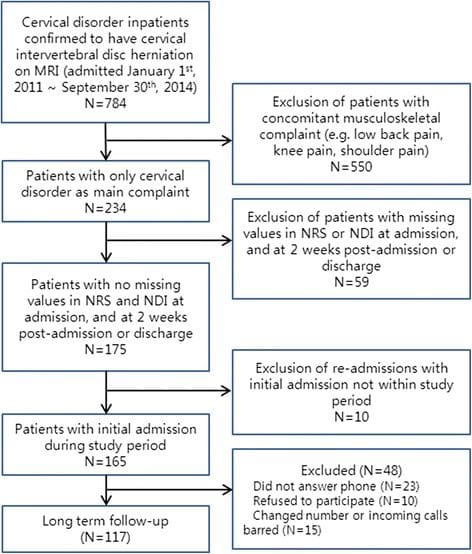
Figure 1 outlines the literature search process. The initial search identified 3286 articles, 35 of which met the inclusion criteria. Information from each article was organized into a review table (Table 1) to summarise the findings of the included papers. Information is reported under two selected headache groups and within each individual MT profession – chiropractic, physiotherapy, osteopathy and massage therapy � where sufficient detail was available.
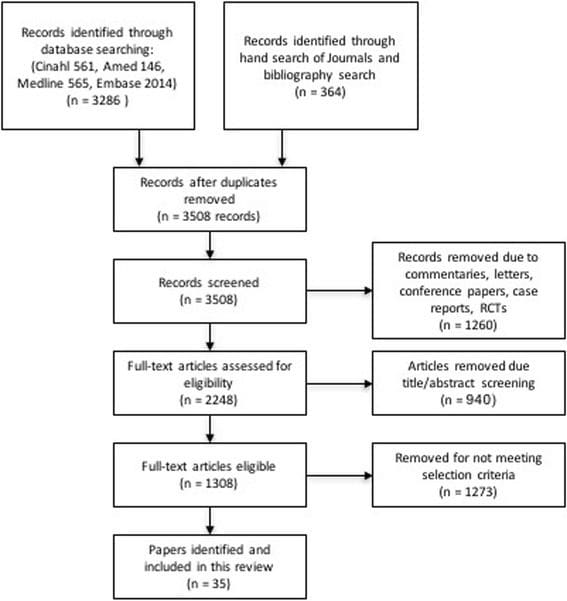
Figure 1: Flow Chart of Study Selection.
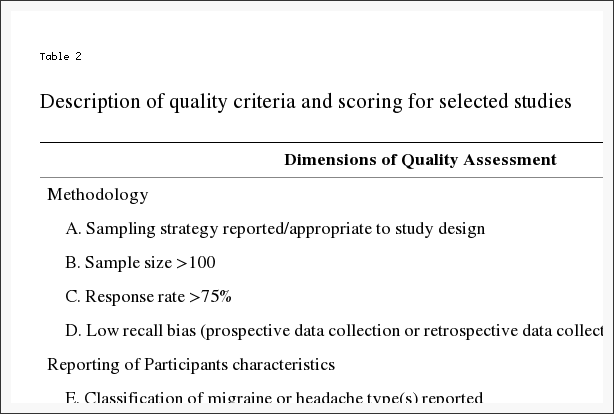
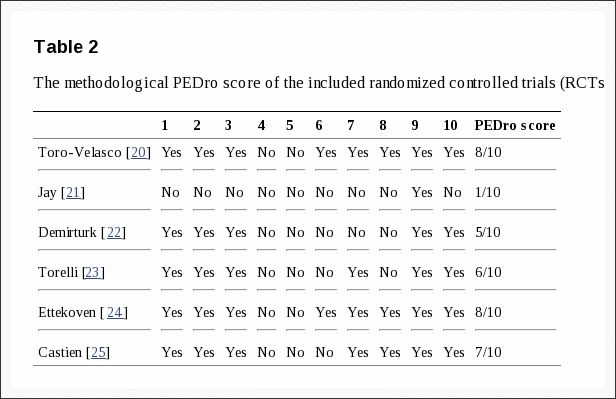
An appraisal of the quality of the articles identified for review was conducted using a quality scoring system (Table 2) developed for the critical appraisal of health literature used for prevalence and incidence of health problems [42] adapted from similar studies [43�45]. This scoring system was applicable to the majority of study designs involving surveys and survey-based structured interviews (29 of the 35 papers) but was not applicable to a small number of included studies based upon clinical records, secondary analysis or practitioner characteristics.
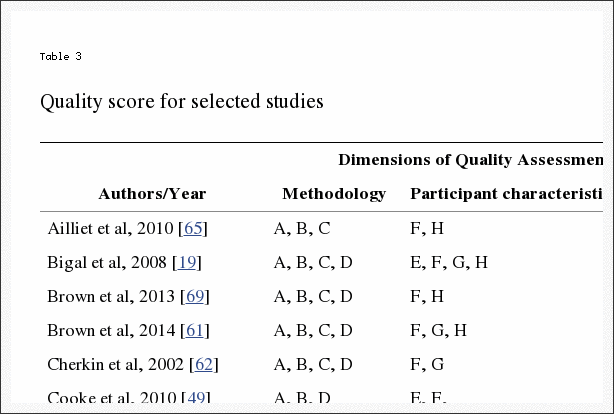
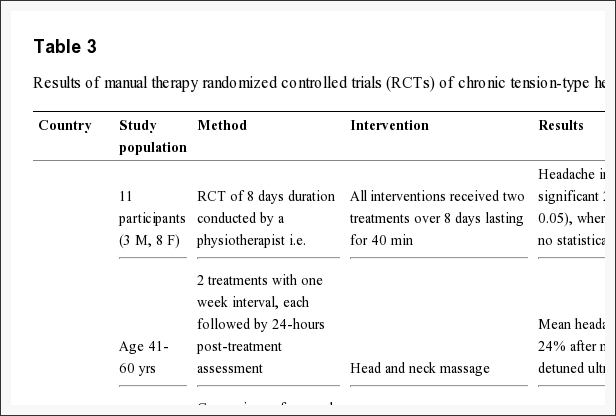
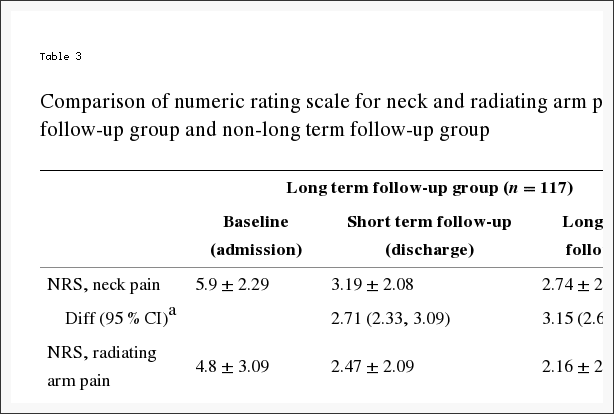
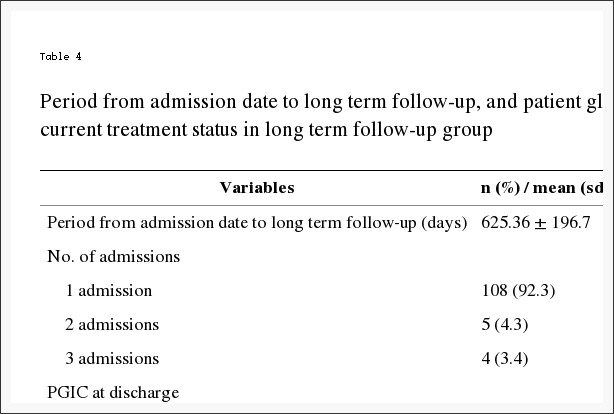
Two separate authors (CM and JA) independently searched and scored the articles. Score results were compared and any differences were further discussed and resolved by all the authors. The quality score of each relevant article is reported in Table 3.
Results
The key findings of the 35 articles were grouped and evaluated using a critical review approach adapted from previous research [46, 47]. Based on the limited information available for other headache types, prevalence findings are reported within one of two categories – either as �migraine� for papers reporting studies where the population was predominately or entirely made up of migraine patients or as �headache� for papers where the study population was predominately other headache types (including tension-type headaches, cluster headaches, cervicogenic headache) and/or where the headache type was not clearly stated. Ten papers reported findings examining prevalence rates for the �migraine� category alone, 18 papers reported findings examining prevalence for the �headache� category alone and 3 papers reported findings for both categories. Based on the nature of the information available, prevalence use was categorised by manual therapy providers. The extracted data was then analysed and synthesized into four thematic categories: prevalence; profile and motivations for MT use; concurrent use and order of use of headache providers; and self-reported evaluation of MT treatment outcomes.
Prevalence of MT Use
Thirty-one of the reviewed articles with a minimum sample size (>100) reported findings regarding prevalence of MT use. The prevalence of chiropractic use for those with migraine ranged from 1.0 to 36.2% (mean: 14.4%) within the general population [19�21, 48�52] and from 8.9 to 27.1% (mean: 18.0%) within headache-clinic patient populations [53, 54]. The prevalence of chiropractic use for those reported as headache ranged from 4 to 28.0% (mean: 12.9%) within the general population [20, 48, 51, 55�57]; ranged from 12.0 to 22.0% (mean: 18.6%) within headache/pain clinic patient populations [58�60] and from 1.9 to 45.5% (mean: 9.8%) within chiropractic patient populations [61�69].
The prevalence use of physiotherapy for those with migraine ranged from 9.0 to 57.0% (mean: 24.7%) within the general population [19, 20, 48, 52] and from 4.9 to 18.7% (mean: 11.8%) within headache-clinic patient populations [54, 70]. The prevalence use of physiotherapy for those reported as headache ranged from 12.2 to 52.0% (mean: 32.1%) within the general population [20, 48] and from 27.8 to 35.0%% (mean: 31.4%) within headache/pain clinic populations [60, 70].
Massage therapy use for those with migraine ranged from 2.0 to 29.7% (mean: 15.6%) within the general population [49, 50, 71] and from 10.1 to 56.4% (mean: 33.9%) within headache-clinic populations [53, 54, 72, 73]. Massage/acupressure use for those reported as headache within headache/pain clinic patient populations ranged from 12.0 to 54.0% (mean: 32.5%) [58�60, 70].
Osteopathy use for those with migraine was reported as 1% within the general population [49]; as 2.7% within a headache-clinic patient population [53] and as 1.7% within an osteopathy patient population [74]. For headache the prevalence was 9% within a headache/pain clinic population [60] and ranged from 2.7 to 10.0% (mean: 6.4%) within osteopathy patient populations [74, 75].
The combined prevalence rate of MT use across all MT professions for those with migraine ranged from 1.0 to 57.0% (mean: 15.9%) within the general population; ranged from 2.7 to 56.4% (mean: 18.4%) within headache-clinic patient populations and was reported as 1.7% in one MT patient population. The combined prevalence rate of MT use across all MT professions for those reported as headache ranged from 4.0 to 52.0% (mean: 17.7%) within the general population; ranged from 9.0 to 54.0% (mean: 32.3%) within headache-clinic patient populations and from 1.9 to 45.5% (mean: 9.25%) within MT patient populations.
Profile and Motivations for MT Use
While patient socio-demographic profiles were not reported within headache populations that were exclusively using MT, several studies report these findings where MT users made up a significant percentage of the non-medical headache treatments utilized by the study population (range 40% � 86%: mean 63%). While findings varied for level of income [58, 70] and level of education, [70, 72, 73] this patient group were more likely to be older [70, 72], female [20], have a higher rate of comorbid conditions [58, 70, 76] and a higher rate of previous medical visits [20, 58, 70] when compared to the non-user group. Overall, this group were reported to have a higher level of headache chronicity or headache disability than non-users [20, 54, 58, 70, 72, 77].
Several studies within headache-clinic populations report patient motivations for the use of complementary and alternative headache treatments where MT users made up a significant proportion of the study population (range 40% � 86%: mean 63%) [58, 70, 72, 78]. From these studies the most common motivation reported by study patients was �seeking pain relief� for headache which accounted for 45.4% � 84.0% (mean: 60.5%) of responses. The second most common motivation was patient concerns regarding the �safety or side effects� of medical headache treatment, accounting for 27.2% � 53.0% (mean: 43.8%) of responses [58, 70, 72]. �Dissatisfaction with medical care� accounted for 9.2% � 35.0% (mean: 26.1%) of responses [58, 70, 72].
A limited number of reviewed papers (all from Italy) report on the source of either the referral or recommendation to MT for headache treatment [53, 58, 59]. From these studies, referral from a GP to a chiropractor ranged from 50.0 to 60.8% (mean: 55.7%), while referral from friends/relatives ranged from 33.0 to 43.8% (mean: 38.7%) and self-recommendation ranged from 0 to 16.7% (mean: 5.6%). For massage therapy, referral from a GP ranged from 23.2 to 50.0% (mean: 36.6%), while referral from friends/relatives ranged from 38.4 to 42.3% (mean: 40.4%) and self-recommendation ranged from 7.7 to 38.4% (mean: 23.1%). For acupressure, referral from a GP ranged from 33.0 to 50.0% (mean: 41.5%), while referral from friends/relatives was reported as 50% and self-recommendation ranged from 0 to 16.6% (mean: 8.3%). One study reported findings for osteopathy where referral from both GP�s and friends/relatives was reported as 42.8% and self-recommendation was reported as 14.4%. Overall, the highest proportion of referrals within these studies was from GPs to chiropractors for chronic tension-type headache (56.2%), cluster headache (50%) and migraine (60.8%).
Concurrent Use and Order of Use of Headache Providers and Related Communication of MT Users
Several studies report on the concurrent use of medical headache management with complementary and alternative therapies. In those studies where the largest percentage of the patient population were users of MT�s (range 57.0% � 86.4%: mean 62.8%), [58, 70, 78] concurrent use of medical care ranged between 29.5% and 79.0% (mean: 60.0%) of the headache patient population.
These studies further report on the level of patient non-disclosure to medical providers regarding the use of MT for headache. Non-disclosure ranged between 25.5 and 72.0% (mean: 52.6%) of the patient population, with the most common reason for non-disclosure reported as the doctor �never asking�, ranging from 37.0 to 80.0% (mean: 58.5%). This was followed by a patient belief that �it was not important for the doctor to know� or �none of the doctor�s business�, ranging from 10.0 to 49.8% (mean: 30.0%). This was followed by a belief that either �the doctor would not understand� or �would discourage� these treatments, ranging from 10.0 to 13.0% (mean: 11.5%) [53, 77].
One large international study reported the ordering of the typical provider of headache care by comparing findings between several countries for migraine patients [21]. Primary care providers followed by neurologists were reported as the first and second providers for migraine treatment for nearly all countries examined. The only exception was Australia, where those with chronic migraine selected chiropractors as typical providers at equal frequency to neurologists (14% for both) while those with episodic migraine selected chiropractors at a greater frequency to neurologists (13% versus 5%). Comparatively, chiropractors were selected as the typical provider for those with chronic migraine by 10% in USA and Canada, 1% in Germany and 0% for UK and France. Chiropractors were selected as the typical provider for those with episodic migraine by 7% in USA, 6% in Germany, 4% in Canada and by 1% in both the UK and France.
Self-Reported Effectiveness of MT Treatment Outcomes
Several headache and pain-clinic population studies provide findings for the self-reported effectiveness of MT headache treatment. For chiropractic, patient self-reporting of partially effective or fully effective headache relief ranged from 27.0 to 82.0% (mean: 45.0%) [53, 58�60, 78]. For massage therapy, patient self-reporting of partially effective or fully effective headache relief ranged from 33.0 to 64.5% (mean: 45.2%)[53, 58, 60, 73, 78], and for acupressure this ranged from 33.4 to 50.0% (mean: 44.5%) [53, 58, 59]. For osteopathy and physiotherapy, one study reported effectiveness as 17 and 36% respectively [60].
When results are combined across all MT professions the reporting of MT as either partially or fully effective ranged from 17.0 to 82.0% (mean 42.5%) [53, 58�60, 73, 78]. In addition, one general population study provides findings for the self-reported effectiveness for chiropractic and physiotherapy at 25.6 and 25.1% respectively for those with primary chronic headache and 38 and 38% respectively for those with secondary chronic headache [79].
Discussion
This paper provides the first critical integrative review on the prevalence and key factors associated with the use of MT treatment for headaches within the peer-reviewed literature. While study methodological limitations and lack of data prevent making strong conclusions, these findings raise awareness of issues of importance to policy-makers, educators, headache providers and future research.
Our review found that MT use was generally higher within medical headache-clinic populations when compared to general populations. However, the use of individual MT providers does vary between different regions and this is likely due to a number of factors including variation in public access, healthcare funding and availability of MT providers. For example, the use of physiotherapy for some headache types may be relatively higher in parts of Europe [20, 60] while the use of chiropractors for some headache types may be relatively higher in Australia and the USA [19, 21]. Overall, the prevalence use of MT for headache appears to be substantial and likely to be the most common type of physical therapy utilized for headache in many countries [19�21, 49]. More high quality epidemiological studies are needed to measure the prevalence of MT use across different headache types and sub-types, both within the general population and clinical populations.
Beyond prevalence, data is more limited regarding who, how and why headache patients seek MT. From the information available however, the healthcare needs of MT headache patients may be more complex and multi-disciplinary in nature compared to those under usual medical care alone. Socio-demographic findings suggest that users of MT and other complementary and alternative therapies have a higher level of headache disability and chronicity compared to non-users. This finding may correlate with the higher prevalence of MT users within headache-clinic populations and a history of more medical appointments. This may also have implications for future MT trial designs both in terms of the selection of trial subjects from inside versus outside MT clinical settings and the decision to test singular MT interventions versus MT in combination with other interventions.
Limited information suggests that a pluralistic approach toward the use of medical and non-medical headache treatments such as MT is common. While findings suggest MT is sought most often for reasons of seeking headache relief, the evidence to support the efficacy of MT for headache relief is still limited. MT providers must remain mindful of the quality of the evidence for a given intervention for a given headache disorder and to inform patients where more effective or safer treatment interventions are available. More research is needed to assess these therapies individually and through multimodal approaches and for studies to include long-term follow-up.
Information limited to Italy, suggests referral from GPs for MT headache treatment can be common in some regions, while this is less likely to widespread given the issue of patient non-disclosure to medical doctors regarding the use of this treatment in other studies. High quality healthcare requires open and transparent communication between patients and providers and between the providers themselves. Non-disclosure may adversely influence medical management should unresponsive patients require further diagnostic investigations [80] or the implementation of more effective approaches to headache management [81] or prevents discussion in circumstances where MT may be contraindicated [82]. Primary headache providers may benefit from paying particular attention to the possibility of non-disclosure of non-medical headache treatments. Open discussion between providers and patients about the use of MT for headache and the associated outcomes may improve overall patient care.
Future Research
Despite the strong need for more high quality research to assess the efficacy of MT as a treatment for headache, the substantial use of MT brings attention to the need for more public health and health services research within this area of headache management. The need for this type of research was identified in a recent global report on the use of headache-related healthcare resources [18]. Furthering this information can lead to improvements in healthcare policy and the delivery of healthcare services.
The substantial use of physical therapies such as MT has been under-reported within many of the national surveys reporting headache-related healthcare utilization [3, 5, 83�85]. Regardless, the role of physical therapies in headache management continues to be assessed, often within mainstream and integrated headache management settings [86�89]. Continuing this research may further our understanding of the efficacy and outcomes associated with a more multidisciplinary approach to headache management.
Further to this is the need for more research to understand the healthcare utilization pathways associated with those patients who use MT in their headache management. Little is known about the sociodemographic background, types of headaches, level of headache disability and comorbidities more common to this patient population. In turn, such information can provide insights that may be valuable to provider clinical decision-making and provider education.
Limitations
The design and findings of our review has a number of limitations. The design of the review was limited by a search within English language journals only. As a result, some research on this topic may have been missed. While the quality scoring system adopted for this review requires further validation, the data we collected was limited by the low to moderate quality of available papers which averaged 6.4 out of 10 points (Table 3). The low scoring was largely due to significant methodological issues and the small sample size associated with much of the collected papers. Much of the data on this topic was heterogeneous in nature (telephone, postal surveys and face-to-face interviews). There was a lack of validated practitioner and patient questionnaires to report findings, such as for questions on prevalence, where the time frames utilized varied between �currently�, �last 12 months� and �ever�.
Data on the prevalence of MT use for headache was limited particularly within individual MT provider populations when compared to data found within the general population and headache-clinic populations. Many studies assessed the use of MT for headache without identifying headache types. Only one study inside an MT population had reported the percentage of patients attending for reasons of migraine alone (osteopathy). The prevalence of MT use for headache was reported most within chiropractic patient population studies, however information was limited on the types of headache. We found no studies reporting the prevalence of headache patients within physiotherapy or massage therapy patient populations using our search terms.
A lack of data for some themes necessitated providing findings pooled with users of other non-medical headache providers. Data within many geographical regions was very limited with the most limited data was on the source of referral to MT headache providers (three papers from Italy only). These limitations support the call for more research to be focused exclusively within MT populations and different regional areas before stronger conclusions can be drawn.
Conclusion
The needs of those with headache disorders can be complex and multi-disciplinary in nature. Beyond clinical research, more high quality public health and health services research is needed to measure and examine a number of issues of significance to the delivery and use of MT�s within headache management. With unmet needs still remaining for many who suffer recurrent headaches, clinicians should remain cognizant of the use of MT�s and remain open to discussing this approach to headache management in order to ensure greater safety, effectiveness and coordination of headache care.
Acknowledgements
Not applicable.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors while the first author on this paper receives a PhD scholarship made available by the Australian Chiropractors� Association.
Availability of Data and Materials
Not applicable (all data is reported in article).
Authors’ Contributions
CM, JA and DS designed the paper. CM carried out the literature search, data collection and selection. CM and DS provided the analysis and interpretation. CM and JA wrote the drafts. All authors contributed to the critical review and intellectual content. All authors read and approved the final manuscript.
Competing Interests
The authors declare that they have no competing interests.
Consent for Publication
Not applicable.
Ethics Approval and Consent to Participate
Not applicable.
Publisher�s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- MT Manual therapy
- EMG Electromyography
Contributor Information
Ncbi.nlm.nih.gov/pmc/articles/PMC5364599/
Dr. Alex Jimenez’s Insight
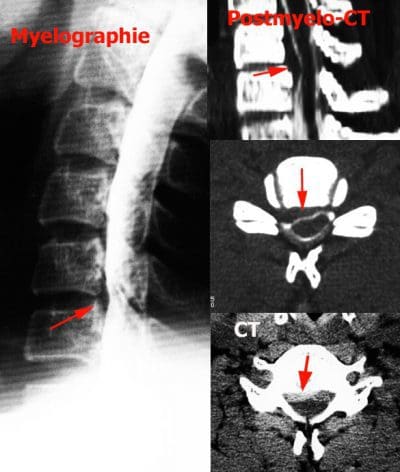
A staggering 15% of the population suffers from migraines, a debilitating condition which affects an individual’s ability to engage in everyday activities. Although widely misunderstood by researches today, I believe that migraine pain can be a symptom of a much bigger underlying health issue. Lumbar herniated discs, or ruptured discs in the lumbar spine, are a common cause of lower back pain and sciatica. When the soft, gel-like center of a lumbar herniated disc compresses the nerve roots of the low back, it can result in symptoms of pain and discomfort, numbness and weakness in the lower extremities. What’s more, a lumbar herniated disc can unbalance the structure and function of the entire spine, eliciting symptoms along the cervical spine that could ultimately trigger migraines. People who constantly experience migraine pain often have to carefully go about their day in hopes of avoiding the blaze of another painful episode. Fortunately, many migraine pain and lumbar herniated disc treatment methods are available to help improve as well as manage the symptoms. Other treatment options can also be considered before surgical interventions.
Surgical versus Non-Operative Treatment for Lumbar Disc Herniation: Eight-Year Results for the Spine Patient Outcomes Research Trial (SPORT)
Abstract
Study Design
Concurrent prospective randomized and observational cohort studies.
Objective
To assess the 8-year outcomes of surgery vs. non-operative care.
Summary of Background Data
Although randomized trials have demonstrated small short-term differences in favor of surgery, long-term outcomes comparing surgical to non-operative treatment remain controversial.
Methods
Surgical candidates with imaging-confirmed lumbar intervertebral disc herniation meeting SPORT eligibility criteria enrolled into prospective randomized (501 participants) and observational cohorts (743 participants) at 13 spine clinics in 11 US states. Interventions were standard open discectomy versus usual non-operative care. Main outcome measures were changes from baseline in the SF-36 Bodily Pain (BP) and Physical Function (PF) scales and the modified Oswestry Disability Index (ODI – AAOS/Modems version) assessed at 6 weeks, 3 and 6 months, and annually thereafter.
Results
Advantages were seen for surgery in intent-to-treat analyses for the randomized cohort for all primary and secondary outcomes other than work status; however, with extensive non-adherence to treatment assignment (49% patients assigned to non-operative therapy receiving surgery versus 60% of patients assigned to surgery) these observed effects were relatively small and not statistically significant for primary outcomes (BP, PF, ODI). Importantly, the overall comparison of secondary outcomes was significantly greater with surgery in the intent-to-treat analysis (sciatica bothersomeness [p > 0.005], satisfaction with symptoms [p > 0.013], and self-rated improvement [p > 0.013]) in long-term follow-up. An as-treated analysis showed clinically meaningful surgical treatment effects for primary outcome measures (mean change Surgery vs. Non-operative; treatment effect; 95% CI): BP (45.3 vs. 34.4; 10.9; 7.7 to 14); PF (42.2 vs. 31.5; 10.6; 7.7 to 13.5) and ODI (?36.2 vs. ?24.8; ?11.2; ?13.6 to ?9.1).
Conclusion
Carefully selected patients who underwent surgery for a lumbar disc herniation achieved greater improvement than non-operatively treated patients; there was little to no degradation of outcomes in either group (operative and non-operative) from 4 to 8 years.
Keywords: SPORT, intervertebral disc herniation, surgery, non-operative care, outcomes
Introduction
Lumbar discectomy for relief of sciatica in patients with intervertebral disc herniation (IDH) is a well-researched and common indication for spine surgery, yet rates of this surgery exhibit considerable geographic variation.[1] Several randomized trials and large prospective cohorts have demonstrated that surgery provides faster pain relief and perceived recovery in patients with herniated disc.[2�6] The effect of surgery on longer term outcomes remains less clear.
In a classic RCT evaluating surgery versus non-operative treatment for lumbar IDH, Weber et al. showed a greater improvement in the surgery group at 1 year that was statistically significant; there was also greater improvement for surgery at 4 years, although not statistically significant, but no apparent difference in outcomes at 10 years.[2] However, a number of patients in the non-operative group eventually underwent surgery over that time, complicating the interpretation of the long-term results. The Maine Lumbar Spine Study, a prospective observational cohort, found greater improvement at one year in the surgery group that narrowed over time, but remained significantly greater in the surgical group for sciatica bothersomeness, physical function, and satisfaction, but no different for work or disability outcomes.[3] This paper reports 8-year results from the Spine Patient Outcomes Research Trial (SPORT) based on the continued follow-up of the herniated disc randomized and observational cohorts.
Methods
Study Design
SPORT is a randomized trial with a concurrent observation cohort conducted in 11 US states at 13 medical centers with multidisciplinary spine practices. The human subjects committees at each participating institution approved a standardized protocol for both the observational and the randomized cohorts. Patient inclusion and exclusion criteria, study interventions, outcome measures, and follow-up procedures have been reported previously.[5�8]
Patient Population
Men and women were eligible if they had symptoms and confirmatory signs of lumbar radiculopathy persisting for at least six weeks, disc herniation at a corresponding level and side on imaging, and were considered surgical candidates. The content of pre-enrollment non-operative care was not pre-specified in the protocol.[5�7] Specific enrollment and exclusion criteria are reported elsewhere.[6,7]
A research nurse at each site identified potential participants, verified eligibility and used a shared decision making video for uniformity of enrollment. Participants were offered enrollment in either the randomized trial or the observational cohort. Enrollment began in March of 2000 and ended in November of 2004.
Study Interventions
The surgery was a standard open discectomy with examination of the involved nerve root.[7,9] The non-operative protocol was �usual care� recommended to include at least: active physical therapy, education/counseling with home exercise instruction, and non-steroidal anti-inflammatory drugs if tolerated. Non-operative treatments were individualized for each patient and tracked prospectively.[5�8]
Study Measures
Primary endpoints were the Bodily Pain (BP) and Physical Function (PF) scales of the SF-36 Health Survey[10] and the AAOS/Modems version of the Oswestry Disability Index (ODI)[11] as measured at 6 weeks, 3 and 6 months, and annually thereafter. If surgery was delayed beyond six weeks, additional follow-up data was obtained 6 weeks and 3 months post-operatively. Secondary outcomes included patient self-reported improvement; work status; satisfaction with current symptoms and care;[12] and sciatica severity as measured by the sciatica bothersomeness index.[13,14] Treatment effect was defined as the difference in the mean changes from baseline between the surgical and non-operative groups.
Statistical Considerations
Initial analyses compared means and proportions for baseline patient characteristics between the randomized and observational cohorts and between the initial treatment arms of the individual and combined cohorts. The extent of missing data and the percentage of patients undergoing surgery were calculated by treatment arm for each scheduled follow-up. Baseline predictors of time until surgical treatment (including treatment crossovers) in both cohorts were determined via a stepwise proportional hazards regression model with an inclusion criterion of p < 0.1 to enter and p > 0.05 to exit. Predictors of missing follow-up visits at yearly intervals up to 8 years were separately determined via stepwise logistic regression. Baseline characteristics that predicted surgery or a missed visit at any time-point were then entered into longitudinal models of primary outcomes. Those that remained significant in the longitudinal models of outcome were included as adjusting covariates in all subsequent longitudinal regression models to adjust for potential confounding due to treatment selection bias and missing data patterns.[15] In addition, baseline outcome, center, age and gender were included in all longitudinal outcome models.
Primary analyses compared surgical and non-operative treatments using changes from baseline at each follow-up, with a mixed effects longitudinal regression model including a random individual effect to account for correlation between repeated measurements within individuals. The randomized cohort was initially analyzed on an intent-to-treat basis.[6] Because of cross-over, additional analyses were performed based on treatments actually received. In these as-treated analyses, the treatment indicator was a time-varying covariate, allowing for variable times of surgery. Follow-up times were measured from enrollment for the intent-to-treat analyses, whereas for the as-treated analysis the follow-up times were measured from the beginning of treatment (i.e. the time of surgery for the surgical group and the time of enrollment for the non-operative group), and baseline covariates were updated to the follow-up immediately preceding the time of surgery. This procedure has the effect of including all changes from baseline prior to surgery in the estimates of the non-operative treatment effect and all changes after surgery in the estimates of the surgical effect. The six-point sciatica scales and binary outcomes were analyzed via longitudinal models based on generalized estimating equations[16] with linear and logit link functions respectively, using the same intent-to-treat and adjusted as-treated analysis definitions as the primary outcomes. The randomized and observational cohorts were each analyzed to produce separate as-treated estimates of treatment effect. These results were compared using a Wald test to simultaneously test all follow-up visit times for differences in estimated treatment effects between the two cohorts.[15] Final analyses combined the cohorts.
To evaluate the two treatment arms across all time-periods, the time-weighted average of the outcomes (area under the curve) for each treatment group was computed using the estimates at each time period from the longitudinal regression models and compared using a Wald test.[15]
Kaplan-Meier estimates of re-operation rates at 8 years were computed for the randomized and observational cohorts and compared via the log-rank test.[17,18]
Computations were done using SAS procedures PROC MIXED for continuous data and PROC GENMOD for binary and non-normal secondary outcomes (SAS version 9.1 Windows XP Pro, Cary, NC). Statistical significance was defined as p < 0.05 based on a two-sided hypothesis test with no adjustments made for multiple comparisons. Data for these analyses were collected through February 4, 2013.
Results
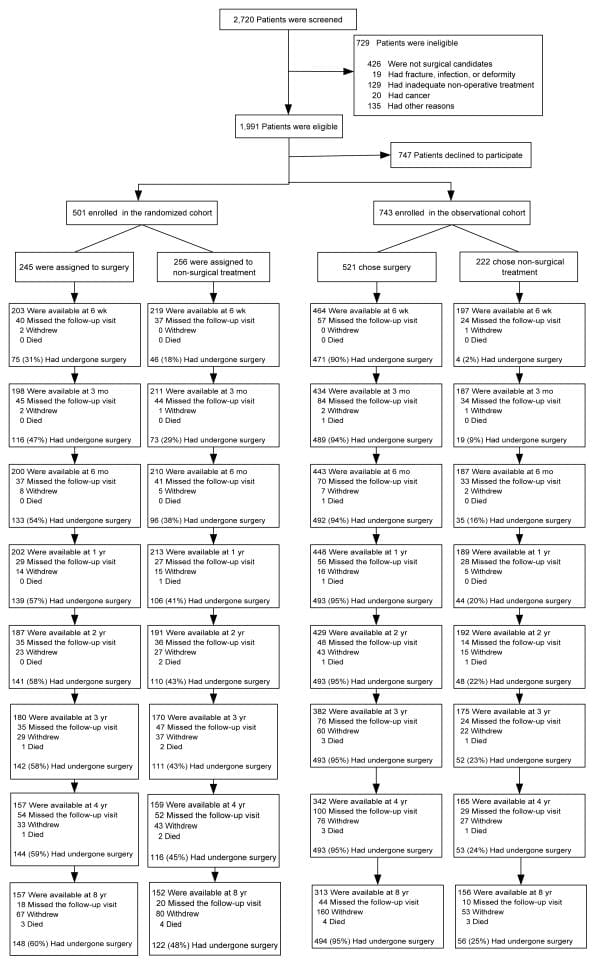
Overall, 1,244 SPORT participants with lumbar intervertebral disc herniation were enrolled (501 in the randomized cohort, and 743 in the observational cohort) (Figure 1). In the randomized cohort, 245 were assigned to surgical treatment and 256 to non-operative treatment. Of those randomized to surgery, 57% had surgery by 1 year and 60% by 8 years. In the group randomized to non-operative care, 41% of patients had surgery by 1 year and 48% by 8 years. In the observational cohort, 521 patients initially chose surgery and 222 patients initially chose non-operative care. Of those initially choosing surgery, 95% received surgery by 1 year; at 8 years 12 additional patients had undergone primary surgery. Of those choosing non-operative treatment, 20% had surgery by 1 year and 25% by 8 years. In both cohorts combined, 820 patients received surgery at some point during the first 8 years; 424 (34%) remained non-operative. Over the 8 years, 1,192 (96%) of the original enrollees completed at least 1 follow-up visit and were included in the analysis (randomized cohort: 94% and observational cohort 97%); 63% of initial enrollees supplied data at 8 years with losses due to dropouts, missed visits, or deaths (Figure 1).
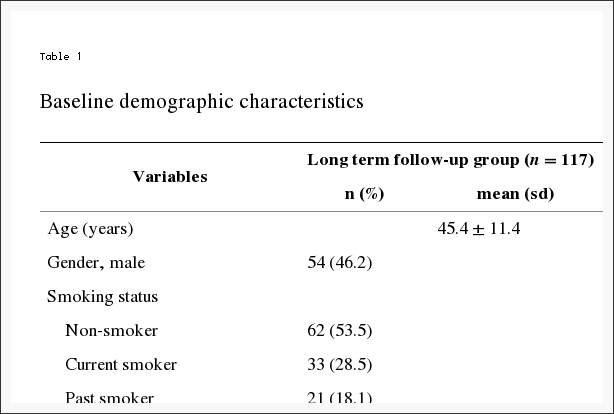
Patient Characteristics
Baseline characteristics have been previously reported and are summarized in Table 1.[5,6,8] The combined cohorts had an overall mean age of 41.7 with slightly more men than women. Overall, the randomized and observational cohorts were similar. However, patients in the observational cohort had more baseline disability (higher ODI scores), were more likely to prefer surgery, more often rated their problem as worsening, and were slightly more likely to have a sensory deficit. Subjects receiving surgery over the course of the study were: younger; less likely to be working; more likely to report being on worker�s compensation; had more severe baseline pain and functional limitations; fewer joint and other co-morbidities; greater dissatisfaction with their symptoms; more often rated their condition as getting worse at enrollment; and were more likely to prefer surgery. Subjects receiving surgery were also more likely to have a positive straight leg test, as well as more frequent neurologic, sensory, and motor deficits. Radiographically, their herniations were more likely to be at the L4�5 and L5-S1 levels and to be posterolateral in location.
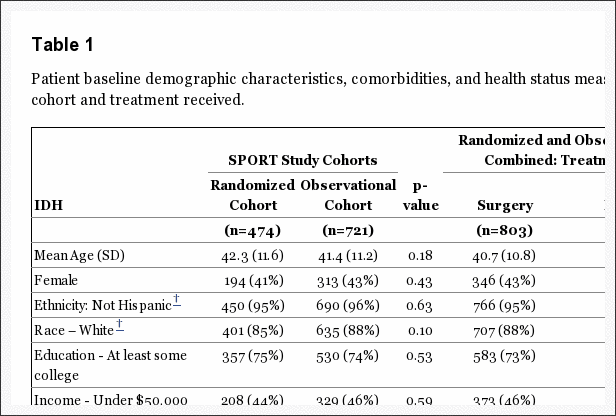
Table 1: Patient baseline demographic characteristics, comorbidities and health status measures according to study cohort and treatment received.
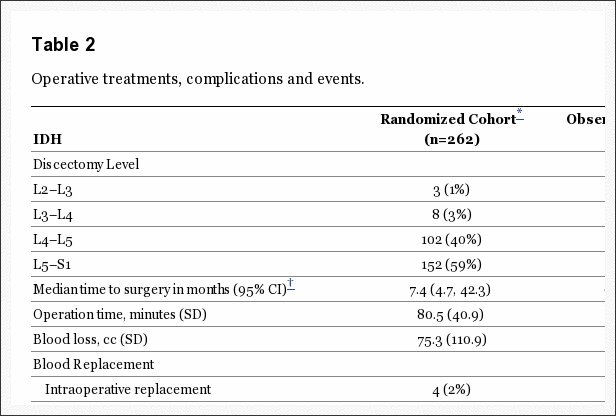
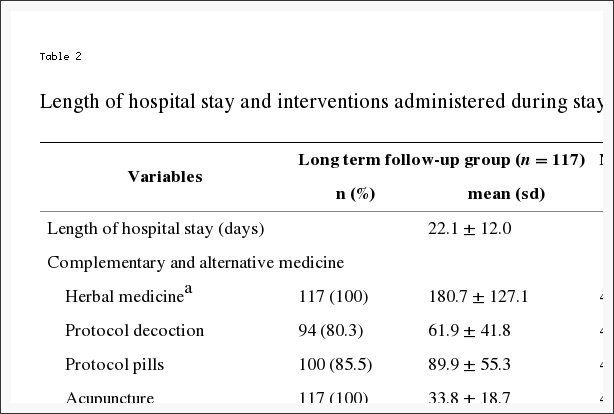
Surgical Treatment and Complications
Overall surgical treatment and complications were similar between the two cohorts (Table 2). The average surgical time was slightly longer in the randomized cohort (80.5 minutes randomized vs. 74.9 minutes observational, p=0.049). The average blood loss was 75.3cc in the randomized cohort vs. 63.2cc in the observational, p=0.13. Only 6 patients total required intra-operative transfusions. There were no perioperative mortalities. The most common surgical complication was dural tear (combined 3% of cases). Re-operation occurred in a combined 11% of cases by 5 years, 12% by 6 years, 14% by 7 years, and 15% by 8 years post-surgery. The rates of reoperation were not significantly different between the randomized and observational cohorts. Eighty-seven of the 119 re-operations noted the type of re-operation; approximately 85% of these (74/87) were listed as recurrent herniations at the same level. One death occurred within 90 days post-surgery related to heart surgery at another institution; the death was judged to be unrelated and was reported to the Institutional Review Board and the Data and Safety Monitoring Board.
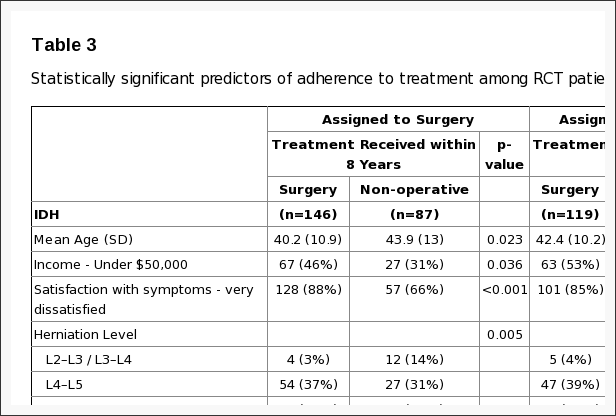
Cross-Over
Non-adherence to treatment assignment affected both treatment arms: patients chose to delay or decline surgery in the surgical arm and crossed over to surgery in the non-operative arm. (Figure 1) Statistically significant differences of patients crossing over to non-operative care within 8 years of enrollment were that they were older, had higher incomes, less dissatisfaction with their symptoms, more likely to have a disc herniation at an upper lumbar level, more likely to express a baseline preference for non-operative care, less likely to perceive their symptoms as getting worse at baseline, and had less baseline pain and disability (Table 3). Patients crossing over to surgery within 8 years were more dissatisfied with their symptoms at baseline; were more likely to perceive they were getting worse at baseline; more likely to express a baseline preference for surgery; and had worse baseline physical function and more self-rated disability.
Main Treatment Effects
Intent-to-Treat Analysis In the intention-to-treat analysis of the randomized cohort, all measures over 8 years favored surgery but there were no statistically significant treatment effects in the primary outcome measures (Table 4 and Figure 2). In the overall intention-to-treat comparison between the two treatment groups over time (area-under the curve), secondary outcomes were significantly greater with surgery in the intention-to-treat analysis (sciatica bothersomeness (p=0.005), satisfaction with symptoms (p=0.013), and self-rated improvement (p=0.013)) (Figure 3) Improvement in sciatica bothersomeness index was also statistically significant in favor of surgery at most individual time point comparisons (although non-significant in years 6 and 7) (Table 4).
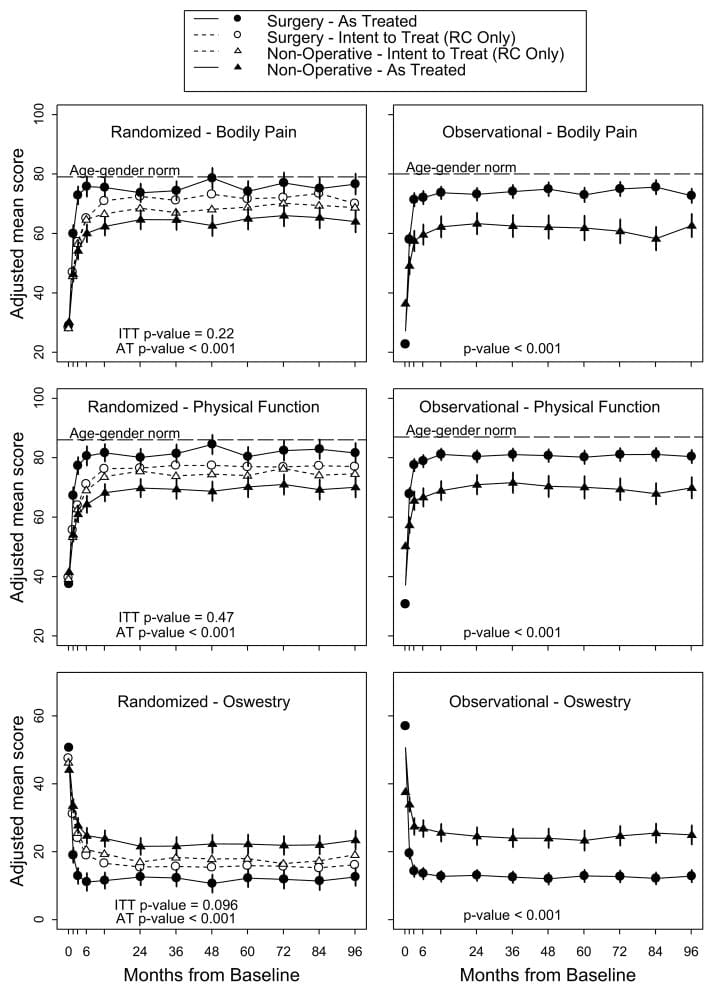
Figure 2: Primary outcomes (SF-36 Bodily Pain and Physical Function, and Oswestry Disability Index) in the randomized and observational cohorts during 8 years of follow-up.
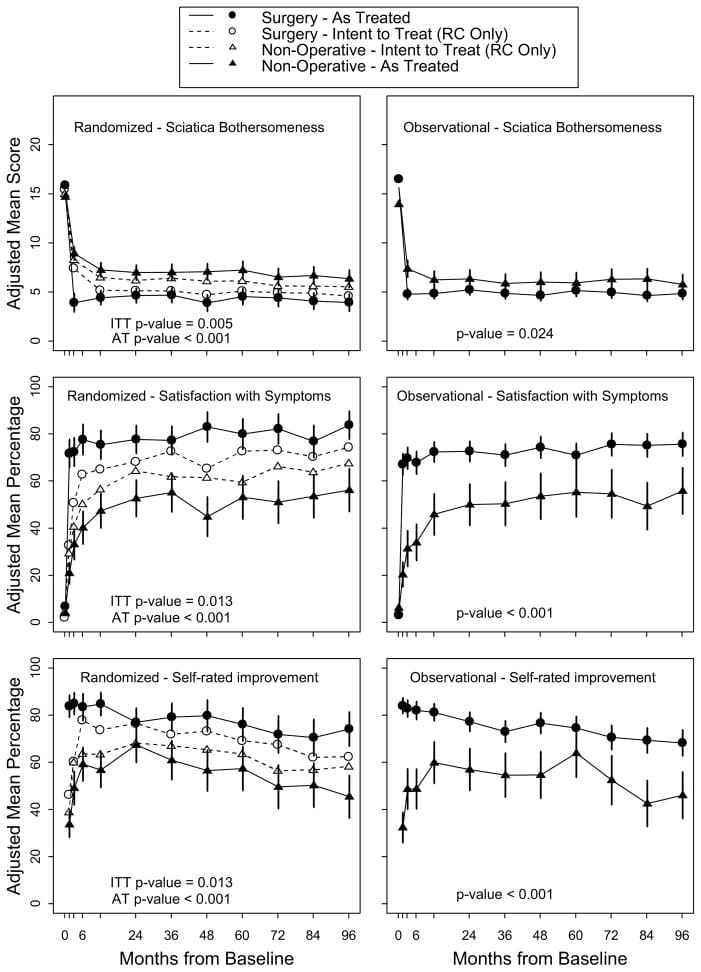
Figure 3: secondary outcomes (Sciatica Bothersomeness, Satisfaction with Symptoms, and Self-rated Global Improvement) in the randomized and observational cohorts during 8 years of follow-up.
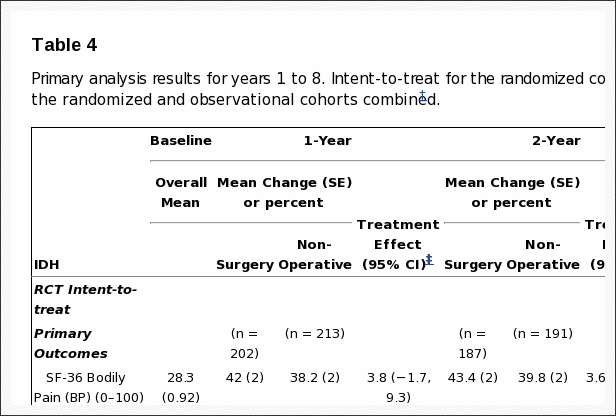
Table 4: Primary analysis results for years 1 to 8. Intent-to-treat for the randomized cohort and adjusted* analyses according to treatment received for the randomized and observational cohorts combined.
As-Treated Analysis The adjusted as-treated effects seen in the randomized and observational were similar. Accordingly, the cohorts were combined for the final analyses. Treatment effects for the primary outcomes in the combined as-treated analysis were clinically meaningful and statistically significant out to 8 years: SF-36 BP 10.9 p < 0.001 (95% CI 7.7 to 14); SF-36 PF 10.6 p<0.001 (95% CI 7.7 to 13.5); ODI ?11.3 p<0.001 (95% CI ?13.6 to ?9.1) (Table 4). The footnote for Table 4 describes the adjusting covariates selected for the final model.
Results from the intent-to-treat and as-treated analyses of the two cohorts are compared in Figure 2. In the combined analysis, treatment effects were statistically significant in favor of surgery for all primary and secondary outcome measures (with the exception of work status which did not differ between treatment groups) at each time point (Table 4 and Figure 3).
Loss-to-Follow-Up
At the 8-year follow-up, 63% of initial enrollees supplied data, with losses due to dropouts, missed visits, or deaths. Table 5 summarized the baseline characteristics of those lost to follow-up compared to those retained in the study at 8-years. Those who remained in the study at 8 years were – somewhat older; more likely to be female, white, college educated, and working at baseline; less likely to be disabled, receiving compensation, or a smoker; less symptomatic at baseline with somewhat less bodily pain, better physical function, less disability on the ODI, better mental health, and less sciatica bothersomeness. These differences were small but statistically significant. Table 6 summarizes the short-term outcomes during the first 2 years for those retained in the study at 8 years compared to those lost to follow-up. Those lost to follow-up had worse outcomes on average; however this was true in both the surgical and non-operative groups with non-significant differences in treatment effects. The long-term outcomes are therefore likely to be somewhat over-optimistic on average in both groups, but the comparison between surgical and non-operative outcomes appear likely to be un-biased despite the long-term loss to follow-up.
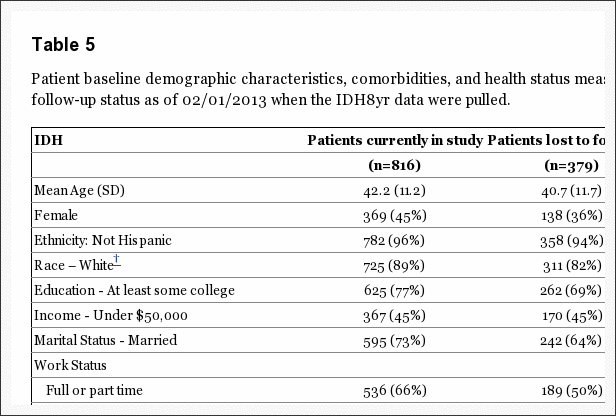
Table 5: Patient baseline demographic characteristics, comorbidities, and health status measures according to patient follow-up status as of 02/01/2013 when the IDH8yr data were pulled.
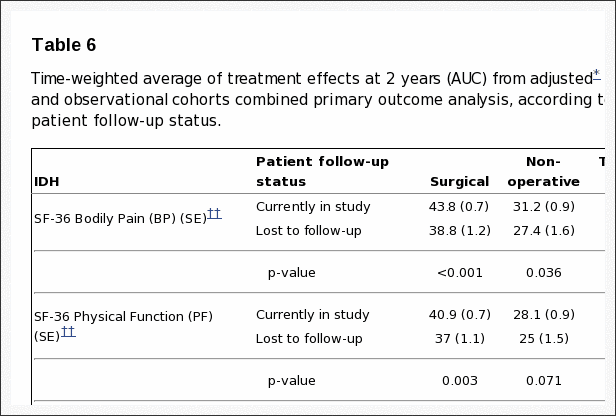
Table 6: Time-weighted average of treatment effects at 2 years (AUC) from adjusted* as-treated randomized and observational cohorts combined primary outcome analysis, according to treatment received and patient follow-up status.
Discussion
In patients with a herniated disc confirmed by imaging and leg symptoms persisting for at least 6 weeks, surgery was superior to non-operative treatment in relieving symptoms and improving function. In the as-treated analysis, the treatment effect for surgery was seen as early as 6 weeks, appeared to reach a maximum by 6 months and persisted over 8 years; it is notable that the non-operative group also improved significantly and this improvement persisted with little to no degradation of outcomes in either group (operative and non-operative) between 4 and 8 years. In the longitudinal intention-to-treat analysis, all the outcomes showed small advantages for surgery, but only the secondary outcomes of sciatica bothersomeness, satisfaction with symptoms, and self-rated improvement were statistically significant. The persistent small benefit in the surgery group over time has made the overall intention-to-treat comparison more statistically significant over time despite high levels of cross-over. The large effects seen in the as-treated analysis after adjustments for characteristics of the crossover patients suggest that the intent-to-treat analysis may underestimate the true effect of surgery since the mixing of treatments due to crossover can be expected to create a bias toward the null in the intent-to-treat analyses.[4,19] Loss to follow-up among patients who were somewhat worse at baseline and with worse short-term outcomes probably leads to overly-optimistic estimated long-term outcomes in both surgery and non-operative groups but unbiased estimates of surgical treatment effects.
Comparisons to Other Studies
There are no other long-term randomized studies reporting the same primary outcome measures as SPORT. The results of SPORT primary outcomes at 2 years were quite similar to those of Peul et al but longer follow up for the Peul study is necessary for further comparison.[4,20] In contrast to the Weber study, the differences in the outcomes in SPORT between treatment groups remained relatively constant between 1 and 8 years of follow-up. One of the factors in this difference may be the sensitivity of the outcome measures � for example, sciatica bothersomeness, which was significantly different out to 8 years in the intention-to-treat, may be a more sensitive marker of treatment success than the general outcome measure used by Weber et al.[2]
The long-term results of SPORT are similar to the Maine Lumbar Spine Study (MLSS).[21] The MLSS reported statistically significantly greater improvements at 10 years in sciatica bothersomeness for the surgery group (?11.9) compared to the nonsurgical groups (?5.8) with a treatment effect of ?6.1 p=0.004; in SPORT the improvement in sciatica bothersomeness in the surgical group at 8 years was similar to the 10 year result in MLSS (?11) though the non-operative cohort in SPORT did better than their MLSS counterparts (?9.1) however the treatment effect in SPORT, while smaller, remained statistically significant (?1.5; p<0.001) due to the much larger sample size. Greater improvements in the non-operative cohorts between SPORT and MLSS may be related to differences in non-operative treatments over time, differences between the two cohorts since the MLSS and did not require imaging confirmation of IDH.
Over the 8 years there was little evidence of harm from either treatment. The 8-year rate of re-operation was 14.7%, which is lower than the 25% reported by MLSS at 10 years.[22]
Limitations
Although our results are adjusted for characteristics of cross over patients and control for important baseline covariates, the as-treated analyses presented do not share the strong protection from confounding that exists for an intent-to-treat analysis.[4�6] However, However, intent-to-treat analyses are known to be biased in the presence of noncompliance at the level observed in SPORT, and our adjusted as-treated analyses have been shown to produce accurate results under reasonable assumptions about the dependence of compliance on longitudinal outcomes.[23] Another potential limitation is the heterogeneity, of the non-operative treatment interventions, as discussed in our prior papers.[5,6,8] Finally, attrition in this long-term follow-up study meant that only 63% of initial enrollees supplied data at 8 years with losses due to dropouts, missed visits, or deaths; based on analyses at baseline and at short-term follow-up, this likely leads to somewhat overly-optimistic estimated long-term outcomes in both treatment groups but an unbiased estimation of surgical treatment effect.
Conclusions
In the intention-to-treat analysis, small, statistically insignificant surgical treatment effects were seen for the primary outcomes but statistically significant advantages for sciatica bothersomeness, satisfaction with symptoms, and self-rated improvement were seen out to 8 years despite high levels of treatment cross-over. The as-treated analysis combining the randomized and observational cohorts, which carefully controlled for potentially confounding baseline factors, showed significantly greater improvement in pain, function, satisfaction, and self-rated progress over 8 years compared to patients treated non-operatively. The non-operative group, however, also showed substantial improvements over time, with 54% reporting being satisfied with their symptoms and 73% satisfied with their care after 8 years.
Acknowledgments
The National Institute of Arthritis and Musculoskeletal and Skin Diseases (U01-AR45444; P60-AR062799) and the Office of Research on Women�s Health, the National Institutes of Health, and the National Institute of Occupational Safety and Health, the Centers for Disease Control and Prevention grant funds were received in support of this work. Relevant financial activities outside the submitted work: consultancy, grants, stocks.
This study is dedicated to the memories of Brieanna Weinstein and Harry Herkowitz, leaders in their own rights, who simply made the world a better place.
Footnotes
Other comorbidities include: stroke, diabetes, osteoporosis, cancer, fibromyalgia, cfs, PTSD, alcohol, drug dependency, heart, lung, liver, kidney, blood vessel, nervous system, hypertension, migraine, anxiety, stomach, bowel
In conclusion, individuals who suffer from migraine pain require the most effective type of treatment in order to help improve as well as manage their symptoms, particularly if their migraines were elicited from a lumbar herniated disc. The purpose of the following articles was to associate the two conditions with each other and demonstrate the results of the research above. Various treatment options can be considered before surgery for migraine pain and lumbar herniated disc treatment. Information referenced from the National Center for Biotechnology Information (NCBI). The scope of our information is limited to chiropractic as well as to spinal injuries and conditions. To discuss the subject matter, please feel free to ask Dr. Jimenez or contact us at 915-850-0900 .
Curated by Dr. Alex Jimenez

Additional Topics: Neck Pain
Neck pain is a common complaint which can result due to a variety of injuries and/or conditions. According to statistics, automobile accident injuries and whiplash injuries are some of the most prevalent causes for neck pain among the general population. During an auto accident, the sudden impact from the incident can cause the head and neck to jolt abruptly back-and-forth in any direction, damaging the complex structures surrounding the cervical spine. Trauma to the tendons and ligaments, as well as that of other tissues in the neck, can cause neck pain and radiating symptoms throughout the human body.

IMPORTANT TOPIC: EXTRA EXTRA: A Healthier You!
OTHER IMPORTANT TOPICS: EXTRA: Sports Injuries? | Vincent Garcia | Patient | El Paso, TX Chiropractor