by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chiropractic, Chiropractic News, Health
�Systematic Review and Meta-analysis of
Chiropractic Care and Cervical Artery
Dissection: No Evidence for Causation
Disclosures can be found in Additional Information at the end of the article
Background
Case reports and case control studies have suggested an association between chiropractic neck manipulation and cervical artery dissection (CAD), but a causal relationship has not been established. We evaluated the evidence related to this topic by performing a systematic review and meta-analysis of published data on chiropractic manipulation and CAD.
Methods
Search terms were entered into standard search engines in a systematic fashion. The articles were reviewed by study authors, graded independently for class of evidence, and combined in a meta-analysis. The total body of evidence was evaluated according to GRADE criteria.
Results
Our search yielded 253 articles. We identified two class II and four class III studies. There were no discrepancies among article ratings (i.e., kappa=1). The meta-analysis revealed a small association between chiropractic care and dissection (OR 1.74, 95% CI 1.26-2.41). The quality of the body of evidence according to GRADE criteria was “very low.”
Conclusions
The quality of the published literature on the relationship between chiropractic manipulation and CAD is very low. Our analysis shows a small association between chiropractic neck manipulation and cervical artery dissection. This relationship may be explained by the high risk of bias and confounding in the available studies, and in particular by the known association of neck pain with CAD and with chiropractic manipulation. There is no convincing evidence to support a causal link between chiropractic manipulation and CAD. Belief in a causal link may have significant negative consequences such as numerous episodes of litigation.
Categories: Neurology, Neurosurgery, Public Health
Keywords: vertebral atery dissection, cervical artery dissection, chiropractic manipulation, cervical manipulation, internal carotid artery dissection, cervical spine manipulative therapy
Introduction
� Copyright 2016
Church et al. This is an open access article distributed under the terms of the Creative Commons Attribution License CC-BY 3.0., which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
|
How to cite this article
Church E W, Sieg E P, Zalatimo O, et al. (February 16, 2016) Systematic Review and Meta-analysis of Chiropractic Care and Cervical Artery Dissection: No Evidence for Causation. Cureus 8(2): e498. DOI 10.7759/cureus.498
|
Neck pain is a common complaint in physicians� and chiropractors� offices. Data from the Centers for Disease Control and from national surveys document 10.2 million ambulatory care visits for a neck problem in 2001 and 2002. By comparison, there were 11 million office-based visits for ischemic heart disease [1]. Many patients with neck pain seek chiropractic care and undergo cervical manipulation. As many as 12% of North Americans receive chiropractic care every year, and a majority of these are treated with spinal manipulation [2].
In contrast to the frequency of neck pain and chiropractic treatments, spontaneous cervical artery dissection (CAD) is rare. The annual incidence of internal carotid artery dissection has been estimated at 2.5�3 per 100,000 patients and that of vertebral artery dissection at 1�1.5 per 100,000 [3]. Stroke occurs in a small proportion of those with CAD, and its true incidence is difficult to estimate. Overall, dissection accounts for two percent of all ischemic strokes [4].
Case reports and case series of cervical dissection following manipulation have been published. Despite their rarity, these cases are frequently publicized for several reasons. Patients are often young and otherwise in good health. Dissection accounts for 10�25% of ischemic strokes in young and middle aged patients [4]. If dissection is caused by cervical manipulation it is potentially a preventable condition. Recent reports, including case control studies, have suggested an association between chiropractic neck manipulation and cervical dissection [5- 10]. Notably, a recent study from the American Heart Association evaluated the available evidence and concluded such an association exists [11]. This report did not include a meta- analysis, nor did it seek to classify studies and grade the body of evidence. We sought to examine the strength of evidence related to this question by performing a systematic review, meta-analysis, and evaluation of the body of evidence as a whole.
Materials & Methods
Search terms �chiropract*,� �spinal manipulation,� �carotid artery dissection,� �vertebral artery dissection,� and �stroke� were included in the search. We used the Medline and Cochrane databases. We additionally reviewed references of key articles for completeness. A librarian with expertise in systematic review was consulted throughout the search process.
Two study authors independently reviewed all articles (EC, ES). They selected any applicable studies for evaluation based on pre-specified inclusion and exclusion criteria. We included only human trials examining patients with carotid or vertebrobasilar artery dissection and recent chiropractic neck manipulation. We excluded non-English language studies. The articles were independently graded using the classification of evidence scheme adopted by the American Academy of Neurology [12-14]. A third author (MG) arbitrated any discrepancies in the class- of-evidence ratings for the included studies.
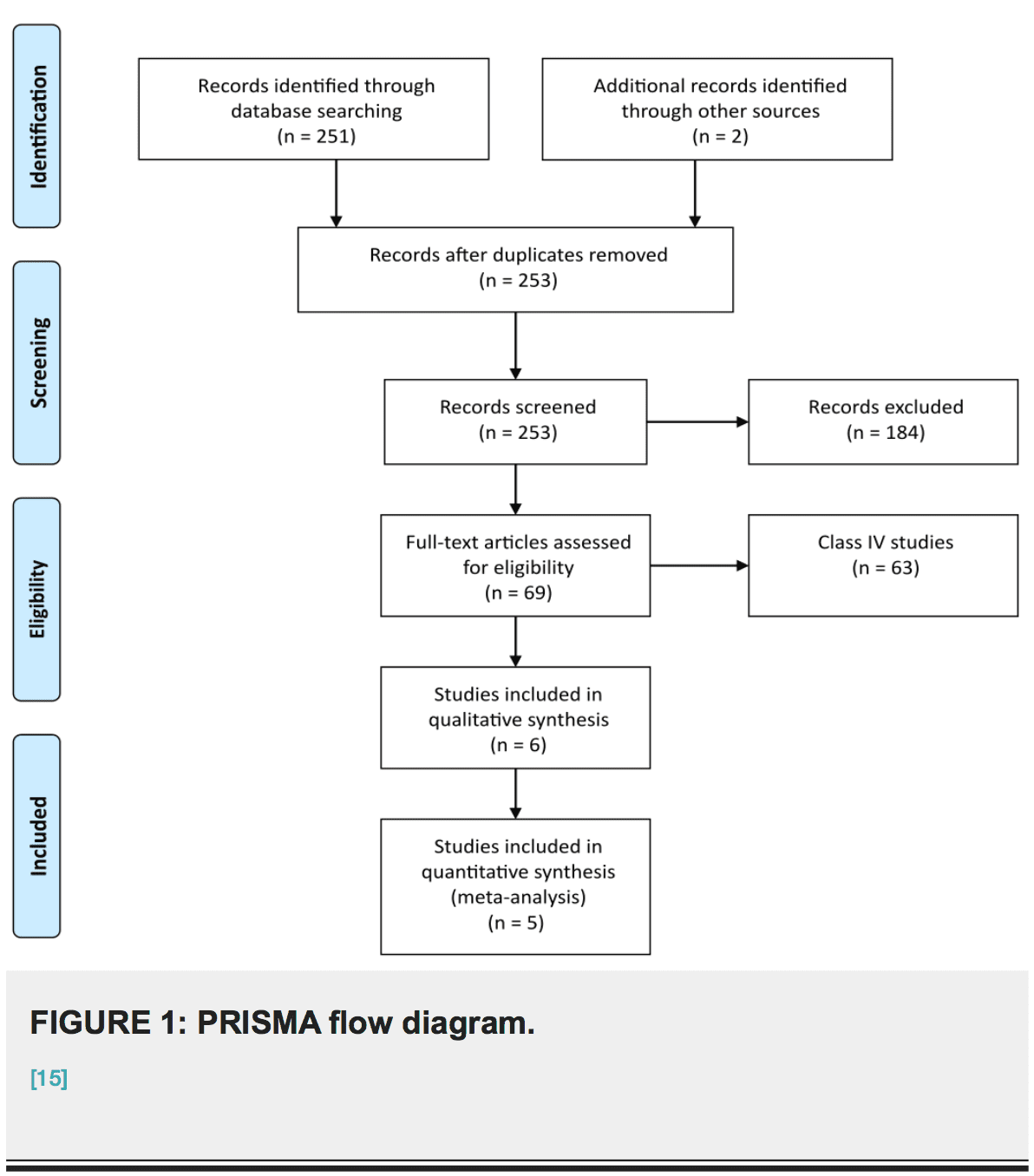
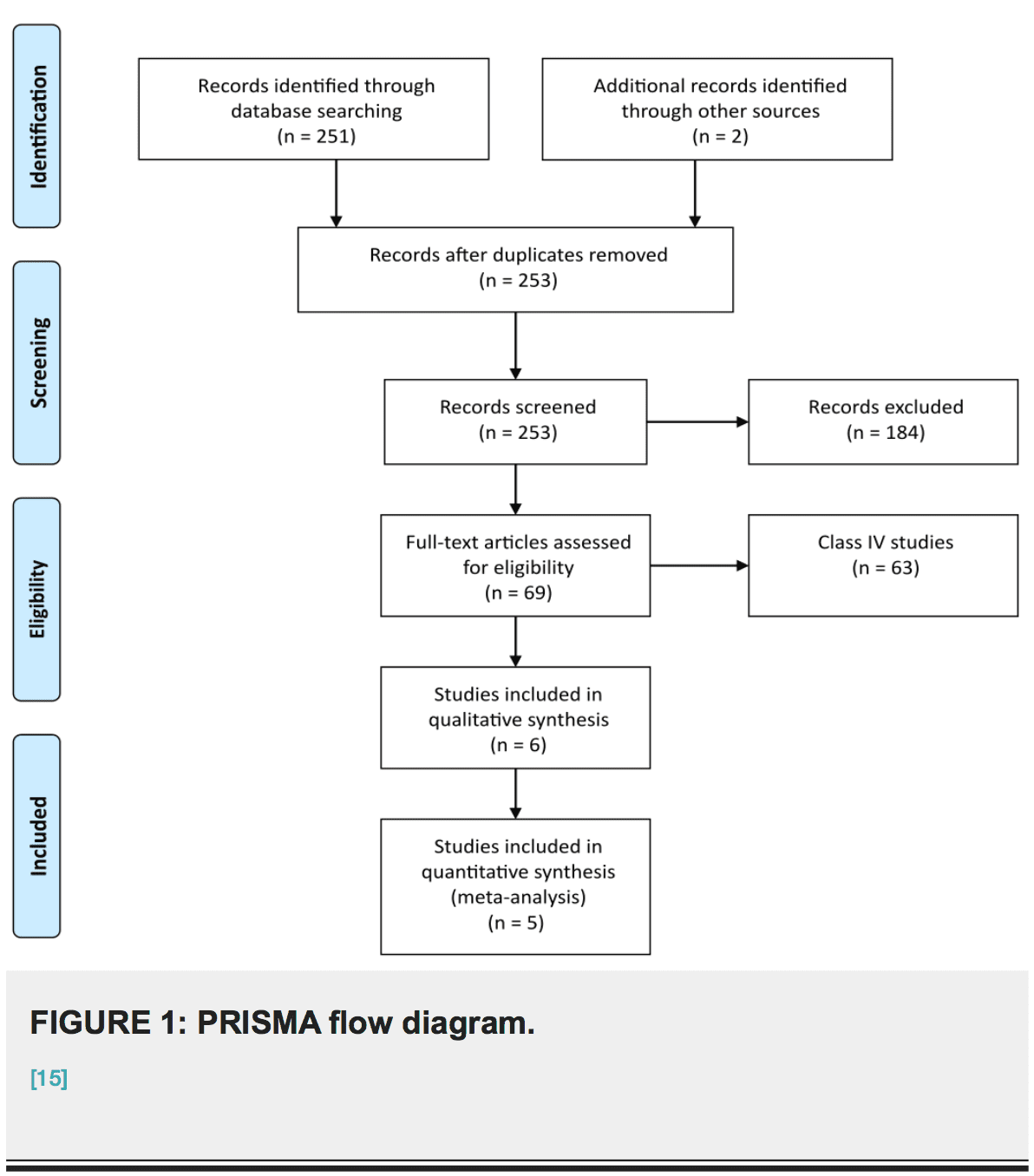
Data from all class II and III studies were included in a meta-analysis. A second meta-analysis excluding class III studies was also performed. The inverse variance method and a fixed effects model were employed. Additionally, we report results using a variable effects model. The analyses were performed using RevMan 5.3 software from the Cochrane Informatics and Knowledge Management Department. We did not compose a protocol for our review, although PRISMA and MOOSE methodologies were used throughout [15-16].
We evaluated the total body of evidence for quality using the GRADE system [17-20]. A final GRADE designation was achieved by consensus after discussions involving all study authors as recommended by GRADE guidelines. This system is designed to assess the total body of evidence rather than individual studies. The criteria include study design, risk of bias, inconsistency, indirectness, imprecision, publication bias, effect size, dose response, and all plausible residual confounding. Four possible final designations are specified: high, moderate,�low, and very low quality.
Results
Results of the systematic review
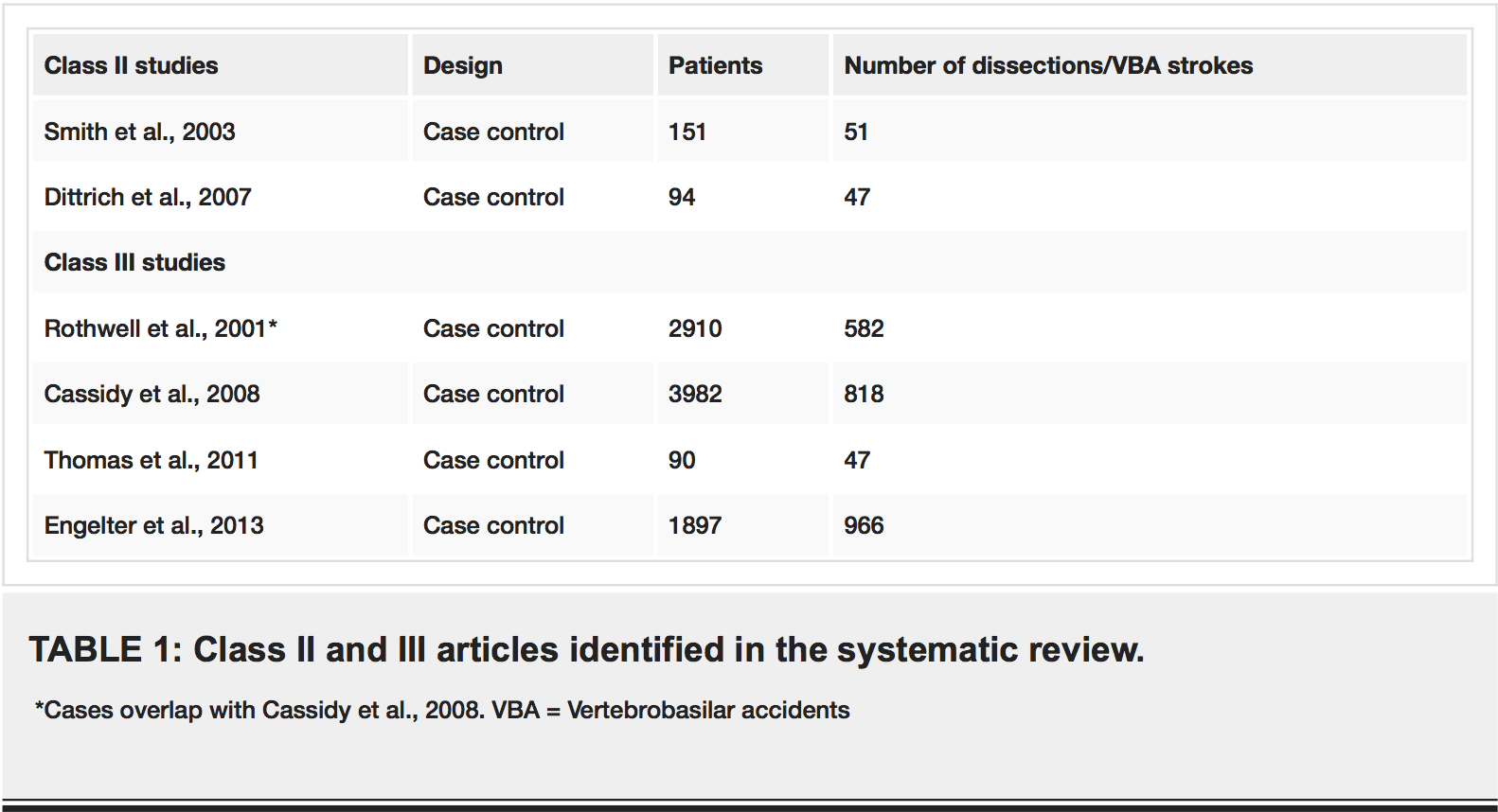
Our search strategy yielded 253 articles. Seventy-seven were judged by all reviewers to be non- relevant. Four articles were judged to be class III studies, and two were rated class II. There were no discrepancies between the independent ratings (i.e., kappa=1). Studies rated class III or higher are listed in Table 1. Figure 1 outlines our process of selecting studies for inclusion in the meta-analysis.
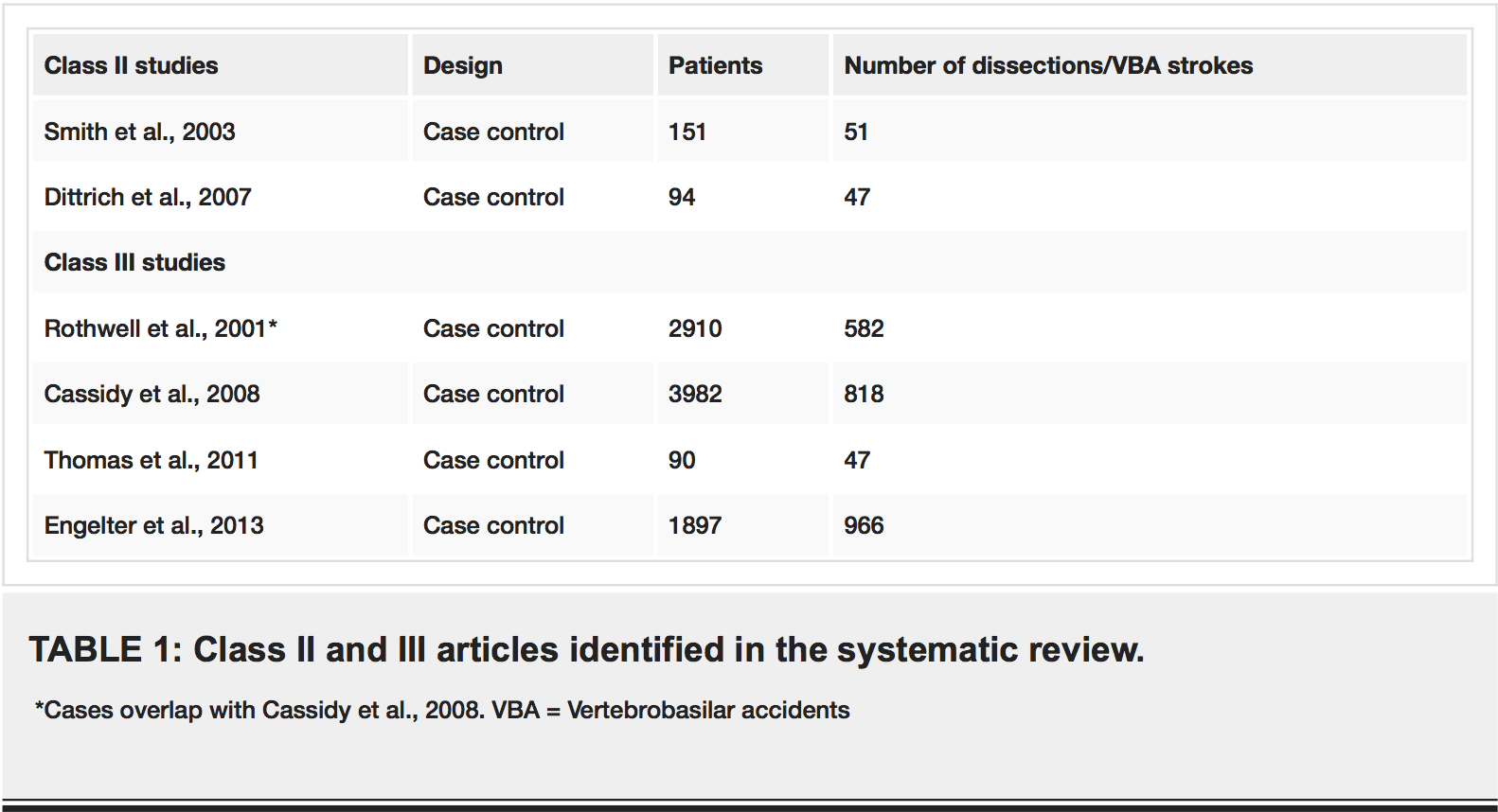
Meta-Analysis
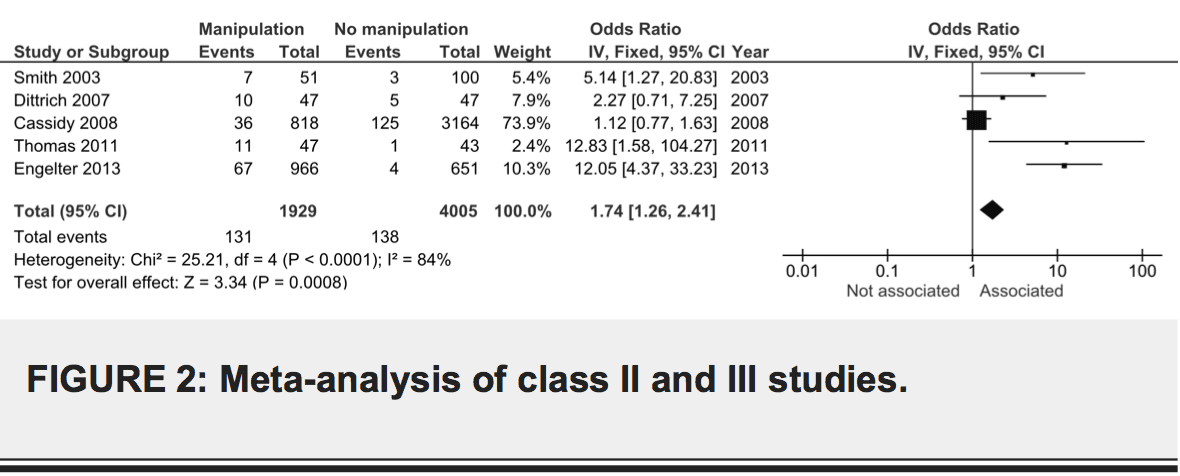
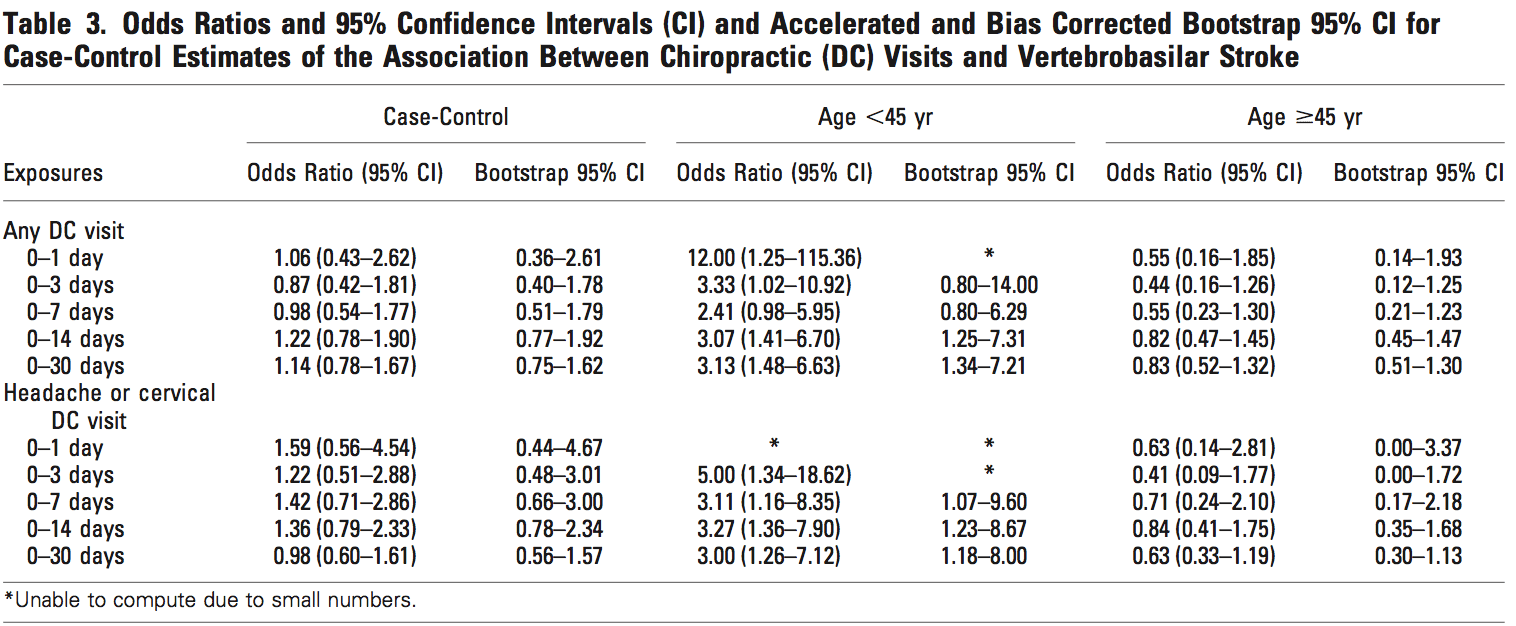
Combined data from class II and III studies suggests an association between dissection and chiropractic care, OR 1.74, 95% CI 1.26-2.41 (Figure 2). The result was similar using a random effects model, OR 4.05, 95% CI 1.27-12.91. We did not include the study by Rothwell et al. because it describes a subset of patients in the study by Cassidy et al. [5,8]. There was considerable heterogeneity among the studies (I2=84%).
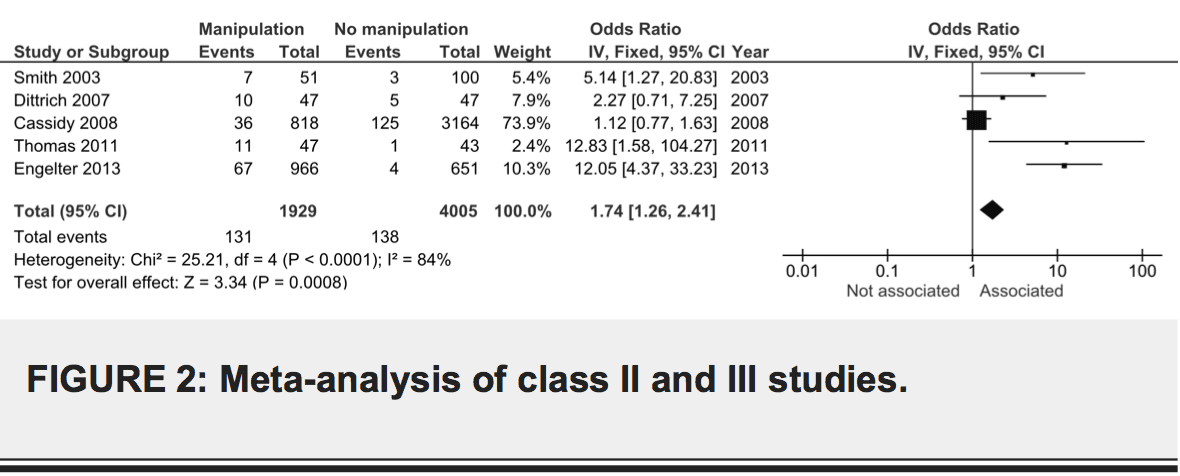
We repeated the meta-analysis excluding class III studies. The combined effect size was again indicative of a small association between dissection and chiropractic care, OR 3.17, 95% CI 1.30-7.74). The result was identical when using a random effects model.
Class II Studies
Smith et al. used a retrospective case control design, combining databases from two academic stroke centers to identify cases of arterial dissection [9]. They found 51 cases and 100 controls. Exposure to spinal manipulative therapy (SMT) was assessed by mail survey. The authors reported an association between SMT and VBA (P = .032). In multivariate analysis, chiropractor care within 30 days was associated with VBA, even when adjusting for neck pain or headache (OR 6.6, 95% CI 1.4-30). While this study controlled for possible confounders such as neck pain, there were several limitations. Head and neck pain as well as chiropractor visit were assessed in a retrospective fashion by mail survey, very possibly introducing both recall and survivor bias. The reason for reporting to the chiropractor (e.g., trauma) was not assessed. Further, there was significant variability among diagnostic procedures, which may reflect increased motivation by physicians to rule out dissection in patients with a history of SMT. Such motivation could result in interviewer bias.
Dittrich et al. compared 47 patients with CAD to a control group with stroke due to etiologies other than dissection [6]. They assessed for risk factors using a face-to-face interview with blinding. These authors found no association between any individual risk factor and CAD, including cervical manipulative therapy. They blame the small sample size for the negative result, and they point out that cumulative analysis of all mechanical risk factors <24 hours prior to symptom onset showed an association (P = .01). This study is subject to recall bias.
Class III Studies
Rothwell et al. used a retrospective case control design to test for an association between chiropractic manipulation and vertebrobasilar accidents (VBA) [8]. They reviewed Ontario hospital records for admissions for VBA from 1993�1998. There were 582 cases and 2328 matching controls. The authors report an association between VBA and visit to a chiropractor within one week (OR 5.03, 95% CI 1.32-43.87), but this was only true for young patients (<45 years). This study represented the first attempt to delineate the association between chiropractic manipulation and extremely rare VBA with controls. Limitations included requisite use of ICD-9 codes to identify cases and associated classification bias, as well as potential unmeasured confounders (e.g., neck pain).
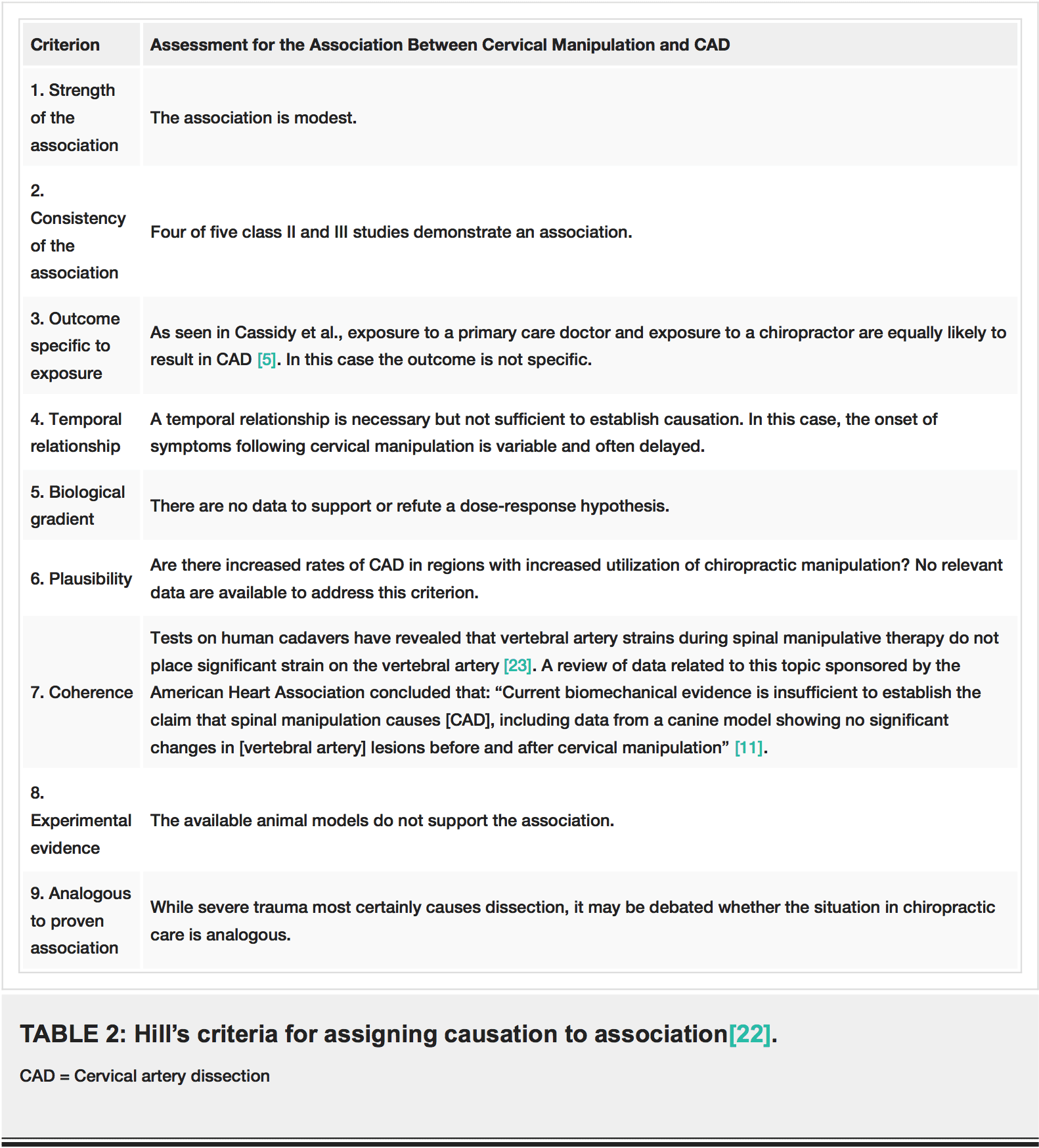
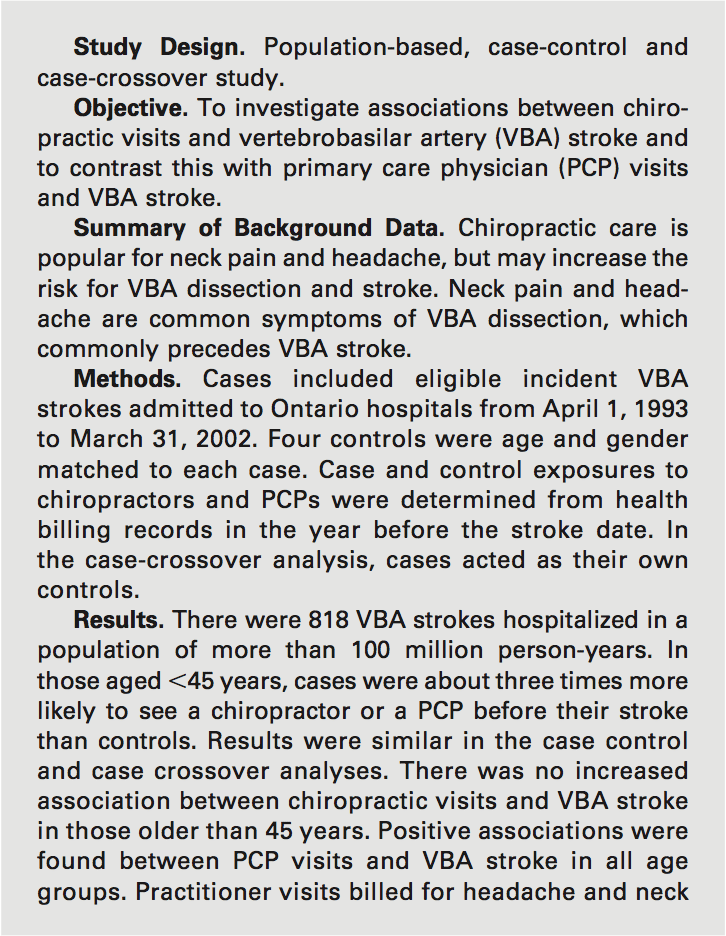
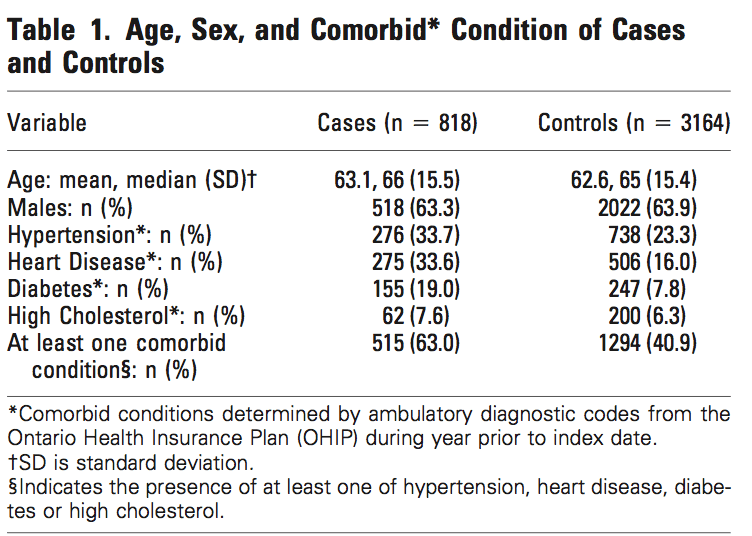
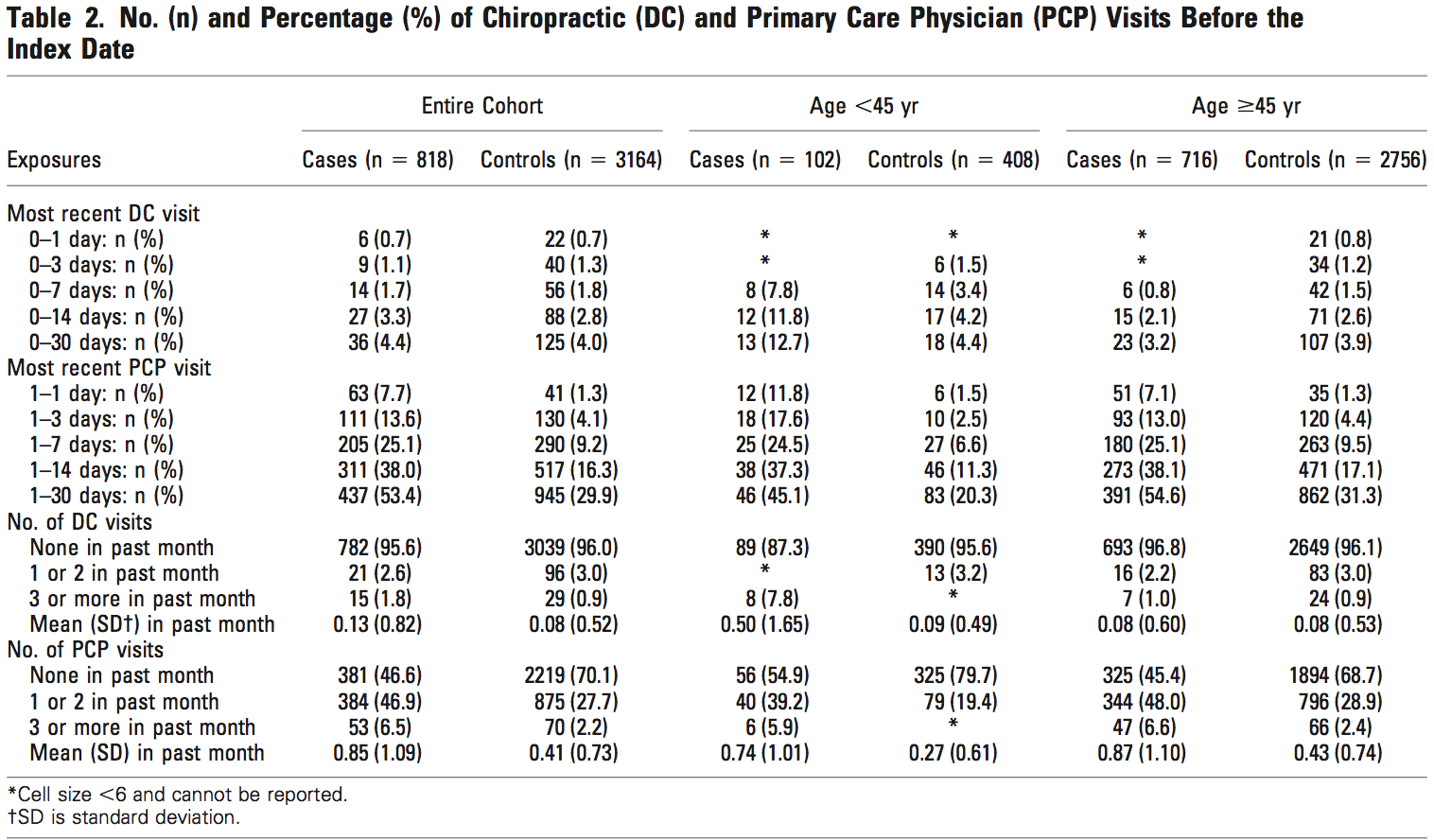
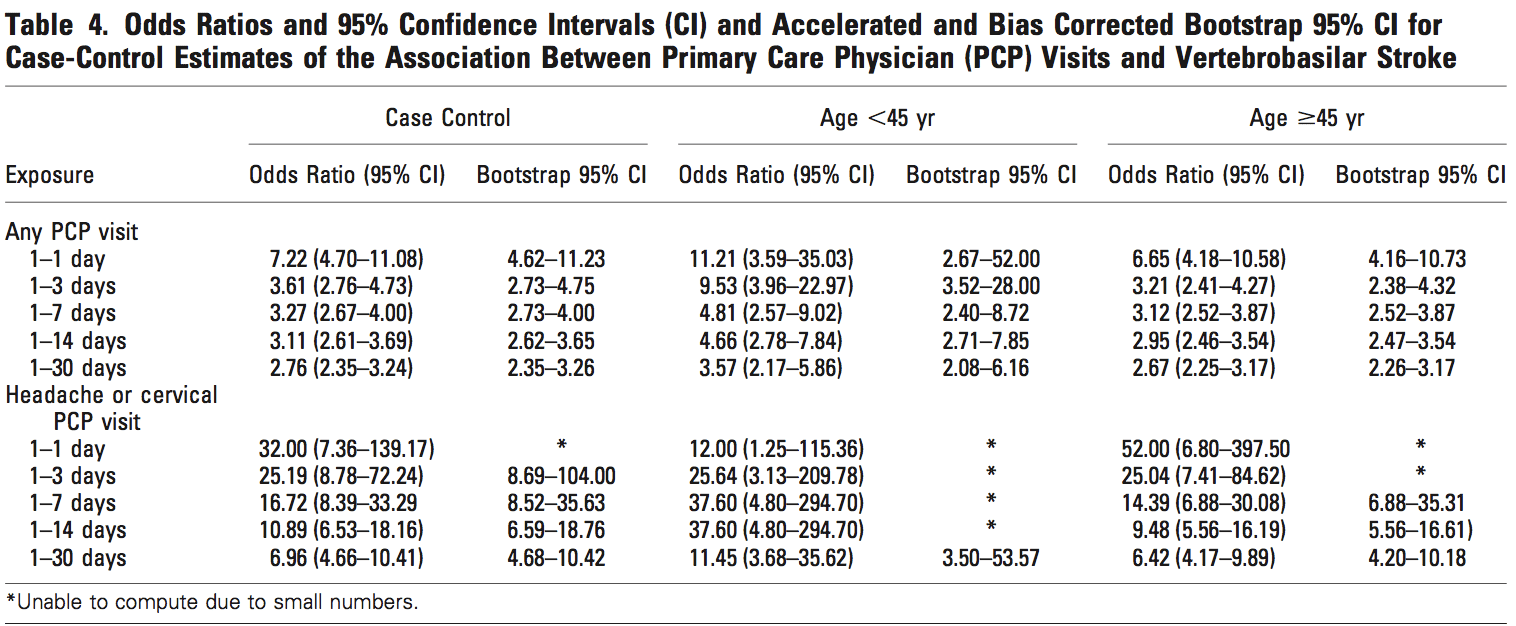
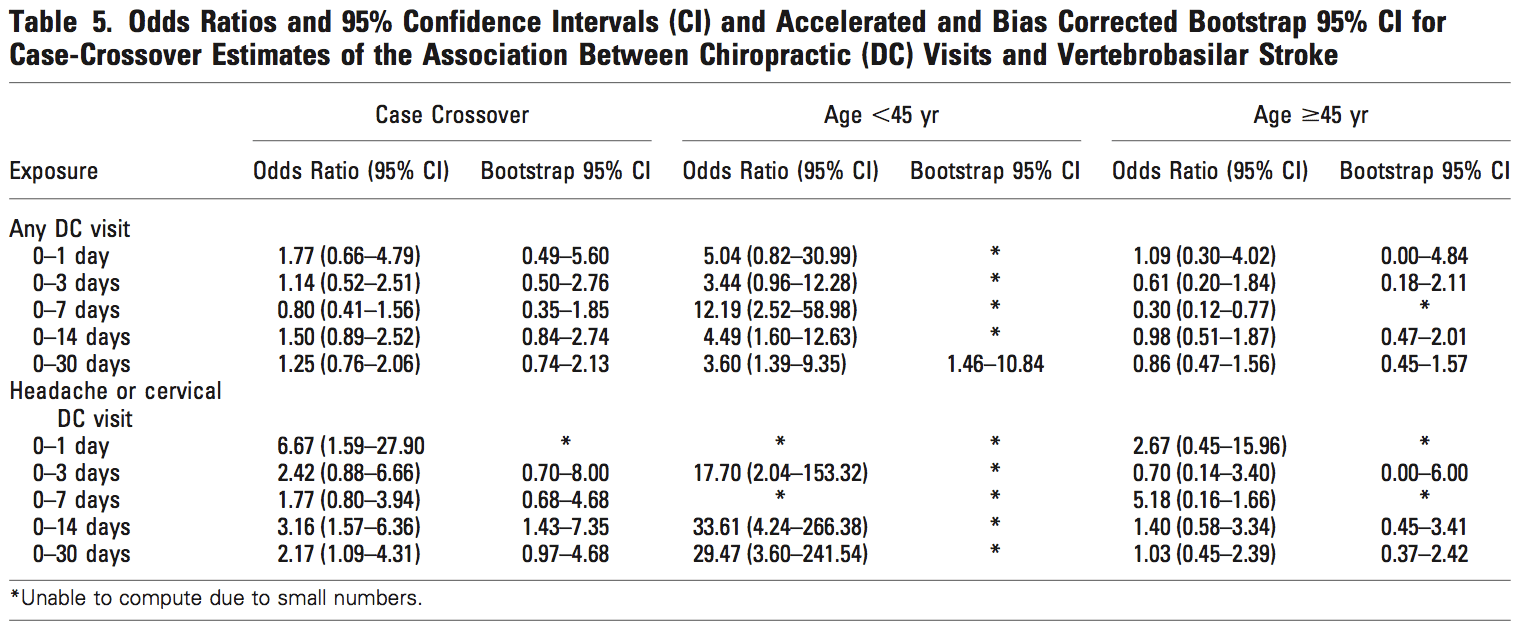
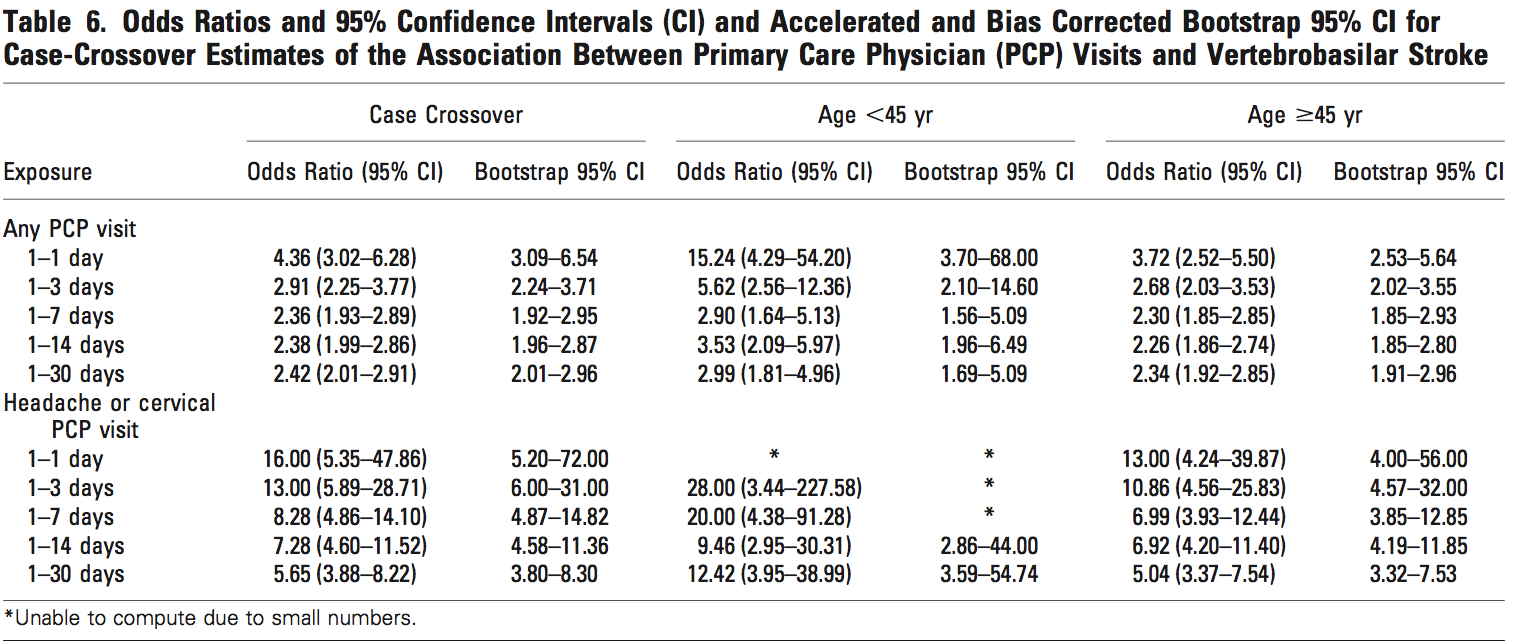
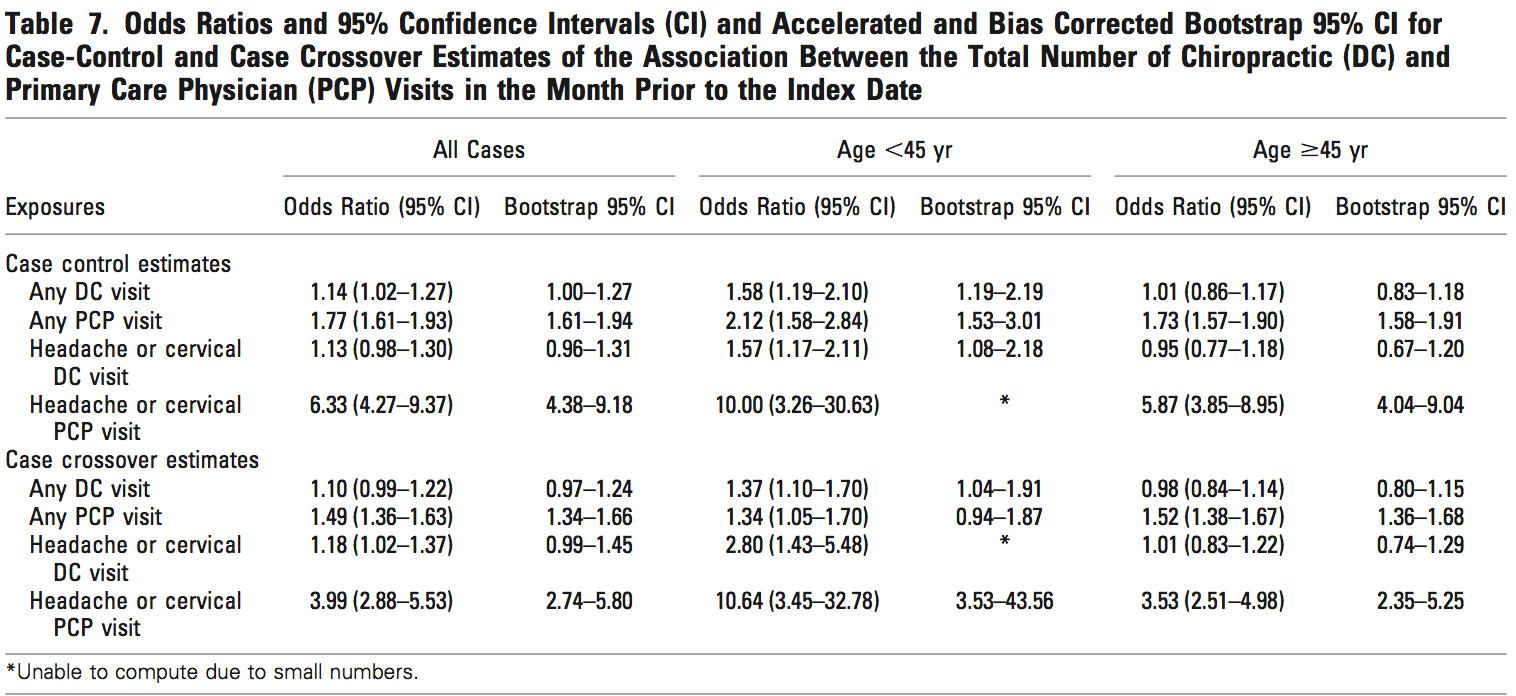
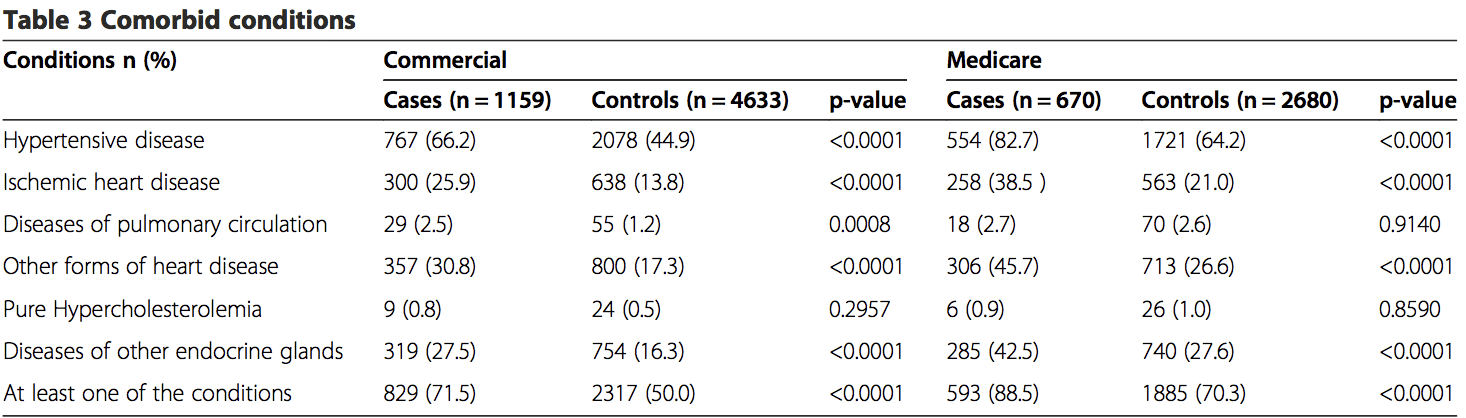
In 2008, Cassidy et al. set out to address the problem of neck pain possibly confounding the association between chiropractic care and VBA [5]. Again using a retrospective case control design, they included all residents of Ontario over a period of 9 years (1993�2002, 109,020,875 person years of observation). They identified 818 VBA strokes resulting in hospitalization and randomly selected age and sex matched controls. Next, they examined ambulatory encounters with chiropractors and primary care physicians (PCPs) in the one year preceding the stroke, limited to cervical manipulation, neck pain, and headache. Associations between chiropractor visit and VBA versus PCP visits and VBA were compared. Indeed, there were associations between both chiropractor visit and VBA (<45yrs OR 1.37, 95% CI 1.04-1.91), and PCP visit and VBA (<45 yrs OR 1.34, 95% CI .94-1.87; >45 yrs and OR 1.53, 95% CI 1.36-1.67). The association for chiropractor visit was not greater than for PCP visit. This data was interpreted as evidence that a confounder such as neck pain may account for the association between chiropractor visit and VBA. This study was subject to many of the same limitations as previous efforts. Canadian health records would not reveal whether a patient with cervical complaints underwent cervical manipulation, and the researchers could not review each chart for imaging confirming dissection. Additionally, the incidence of comorbidities (e.g., hypertension, heart disease,�diabetes) was significantly higher among cases as compared to controls, and we are concerned that these differences were non-random.
In another case control study, Thomas et al. compared the records of 47 patients with confirmed or suspected vertebral or internal carotid artery dissection with 43 controls [10]. They limited their analysis to young patients defined as <55 years. These authors report a significant association between dissection and recent head or neck trauma (OR 23.51, 95% CI 5.71-96.89) as well as neck manual therapy (OR 1.67, 95% CI 1.43-112.0). An inconsistent standard for case ascertainment (a significant number of patients lacked radiographic confirmation of dissection) and lack of blinding weaken this study.
Engelter et al. evaluated data from the Cervical Artery Dissection and Ischemic Stroke Patients (CADISP) consortium, identifying 966 patients with CAD, 651 with stroke attributable to another cause, and 280 healthy controls [7]. The CADISP study involved both prospectively and retrospectively collected data at multiple centers in several countries. They assessed for prior cervical trauma within one month using questionnaires administered during clinic visits. Cervical manipulation therapy was more common for CAD versus stroke from another cause (OR 12.1, CI 4.37-33.2). The report notes that an association between any trauma and CAD was present even when restricting the analysis to prospectively recruited patients. However, in patients to whom the questionnaire was administered after dissection, recall bias may have been at work whether or not the patient was enrolled prospectively. Indeed, the frequency of prior cervical trauma in this study was substantially higher than previous reports (40% versus 12-34%). Additional weaknesses include a highly heterogeneous standard for case definition and no clear masking procedures.
Body Of Evidence Quality (GRADE Rating)
Having performed a systematic review and rated articles according to their individual strengths and weaknesses, we graded the overall body of evidence using the system proposed by Guyatt et al. [17-20]. The GRADE approach to rating quality of evidence proposes four categories that are applied to a body of evidence: high, moderate, low, and very low. In the setting of systematic review, a particular rating reflects the extent of confidence that the estimates of effect are correct. The GRADE approach begins with study design and sequentially examines features with the potential to enhance or diminish confidence in the meta-analytic estimate of effect size.
Our final assessment of the quality of the body of evidence using these criteria was very low. The initial rating based on study design was low (observational studies). Given the controversial nature of this topic and the legal ramifications of results, there is certainly potential for bias (-1 serious). However, blinding in the Class II studies mitigated this risk to some extent. Inconsistency and imprecision did not lower our rating. Because the body of evidence is derived from measures of association, the rating was lowered for indirectness (-1 serious). Publication bias is less likely because of the impact of a negative result in this case. The funnel plot from our meta-analysis was inconclusive with regard to possible publication bias because of the small number of studies included but suggested a deficit in the publication of small negative trials. There was not a large effect size, and currently there is no evidence for a dose response gradient. Moreover, the most worrisome potential confounder (neck pain) would increase rather than reduce the hypothesized effect.
Discussion
The results of our systematic review and meta-analysis suggest a small association between chiropractic care and CAD. There are no class I studies addressing this issue, and this conclusion is based on five class II and III studies. Scrutiny of the quality of the body of data�using the GRADE criteria revealed that it fell within the �very low� category. We found no evidence for a causal link between chiropractic care and CAD. This is a significant finding because belief in a causal link is not uncommon, and such a belief may have significant adverse effects such as numerous episodes of litigation.
The studies included in our meta-analysis share several common weaknesses. Two of the five studies used health administrative databases, and since conclusions depend on accurate ICD coding, this technique for case ascertainment may introduce misclassification bias. It is not possible to account for the type of spinal manipulation that may have been used. Retrospective collection of data is also a potential weakness and may introduce recall bias when a survey or interview was used. Moreover, patients arriving at a hospital complaining of neck pain and describing a recent visit to a chiropractor may be subject to a more rigorous evaluation for CAD (interviewer bias). Another potential source of interviewer bias was lack of blinding in the class III studies. Further, we noted substantial variability among diagnostic procedures performed. All of these weaknesses affect the reliability of the available evidence and are not �corrected� by performing a meta-analysis.
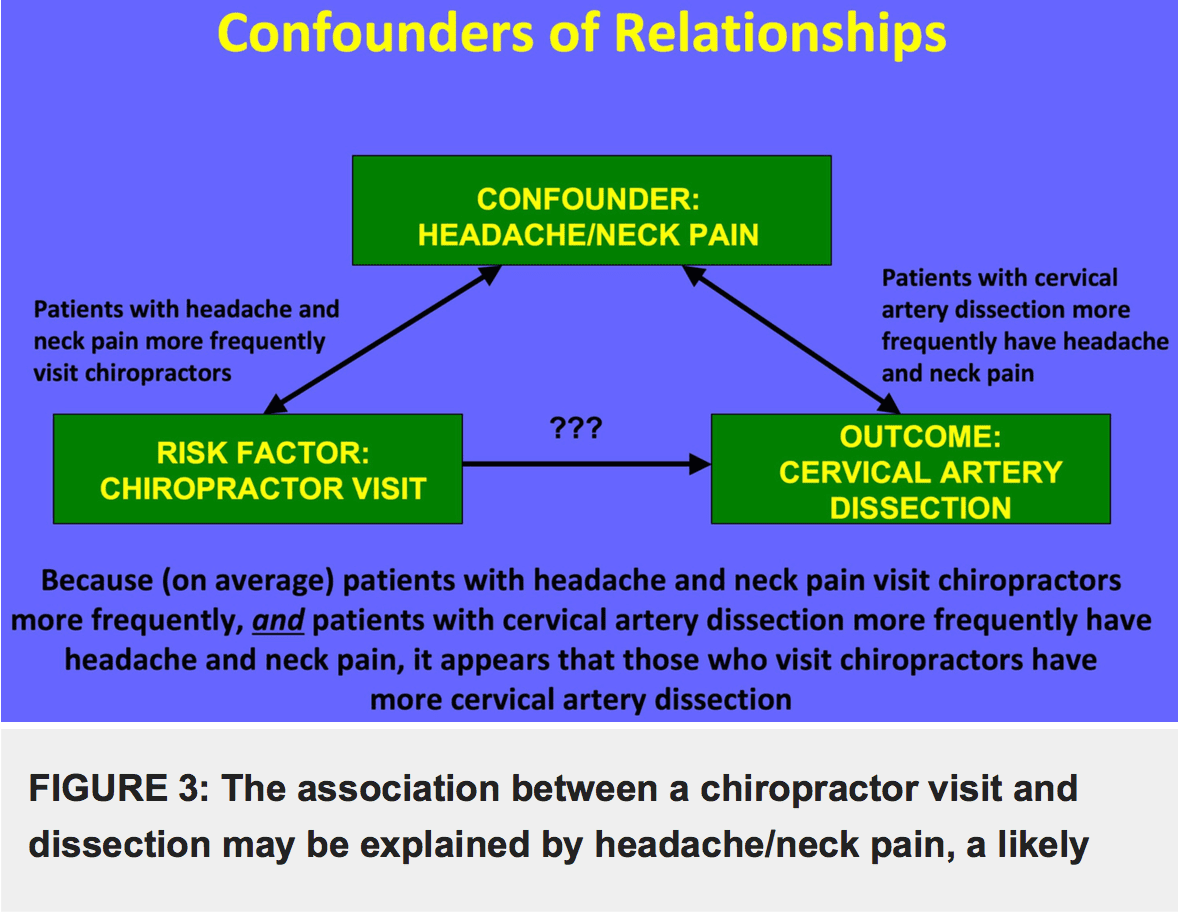
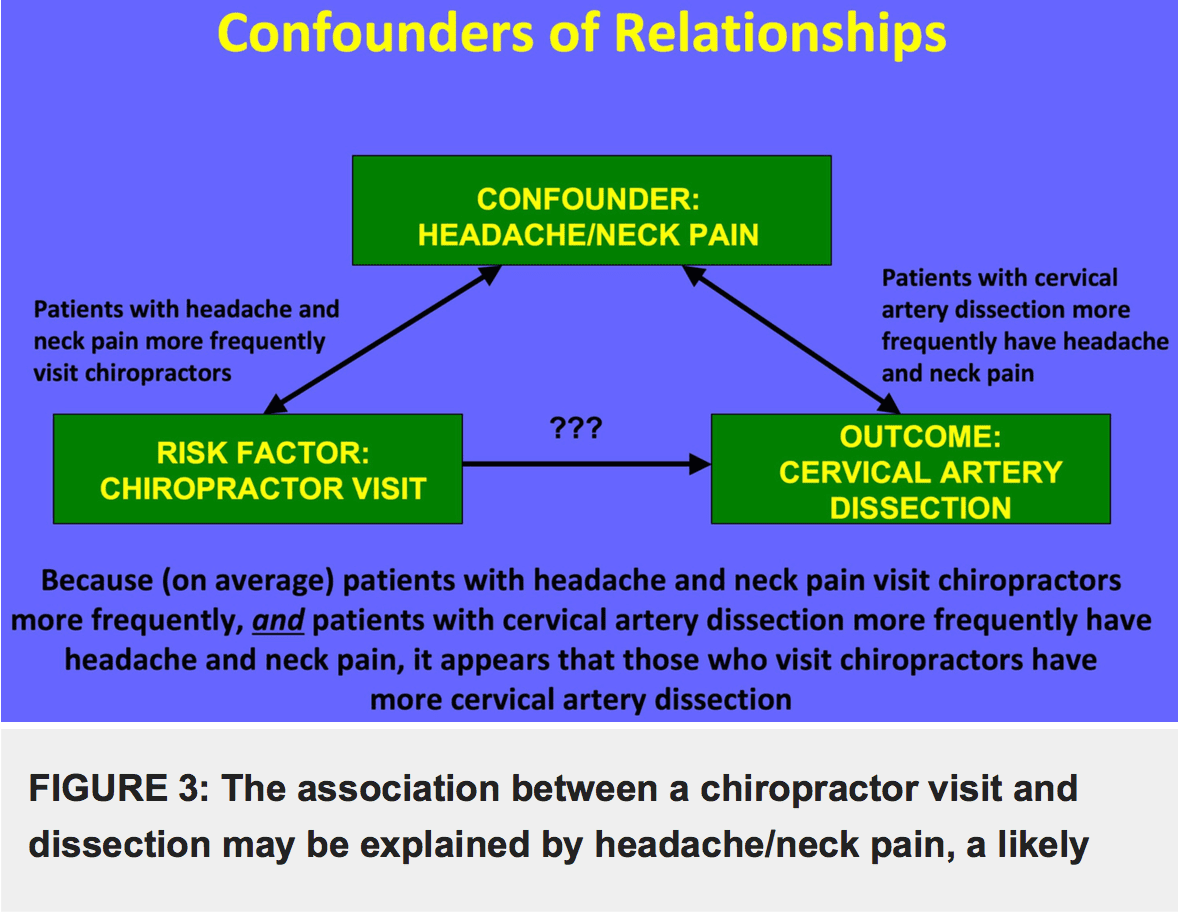
Perhaps the greatest threat to the reliability of any conclusions drawn from these data is that together they describe a correlation but not a causal relationship, and any unmeasured variable is a potential confounder. The most likely potential confounder in this case is neck pain. Patients with neck pain are more likely to have CAD (80% of patients with CAD report neck pain or headache) [21], and they are more likely to visit a chiropractor than patients without neck pain (Figure 3). Several of the studies identified in our systematic review provide suggestive evidence that neck pain is a confounder of the apparent association between chiropractic neck manipulation and CAD. For example, in Engelter et al. patients with CAD and prior cervical trauma (e.g., cervical manipulation therapy) were more likely to present with neck pain but less often with stroke than those with CAD and no prior cervical trauma (58% vs. 43% for trauma and 61% vs. 69% for stroke) [7]. If patients with CAD without neurological symptoms came to medical attention, it was probably because of pain. Patients with neck pain would also be more likely to visit a chiropractor than those without neck pain.
Cassidy et al. hypothesized that, although an association between chiropractor visits and vertebrobasilar artery stroke is present, it may be fully explained by neck pain and headache [5]. These authors reviewed 818 patients with vertebrobasilar artery strokes hospitalized in a population of 100 million person-years. They compared chiropractor and PCP visits in this population and reported no significant difference between these associations. For patients under 45 years of age, each chiropractor visit in the previous month increased the risk of stroke (OR 1.37, 95% CI 1.04-1.91), but each PCP visit in the previous month increased the risk in a nearly identical manner (<45 yrs OR 1.34, 95% CI .94-1.87; >45 yrs and OR 1.53, 95% CI 1.36- 1.67). The authors conclude that, since patients with vertebrobasilar stroke were as likely to visit a PCP as they were to visit a chiropractor, these visits were likely due to pain from an existing dissection.
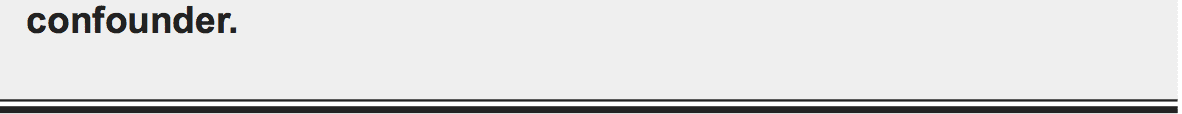
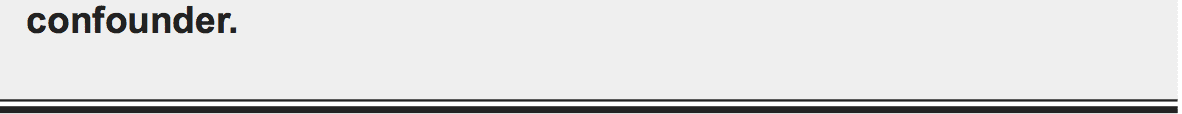
Cervical artery dissection is a rare event, creating a significant challenge for those who wish to understand it. A prospective, randomized study design is best suited to control for confounders, but given the infrequency of dissection, performing such a study would be logistically and also ethically challenging. Sir Austin Bradford Hill famously addressed the problem of assigning causation to an association with the application of nine tests [22]. These criteria include strength, consistency, specificity, temporality, biological gradient, plausibility, coherence, experimental evidence, and analogy. The specific tests and our assessment for the association between cervical manipulation and CAD are summarized in Table 2. In our appraisal, this association clearly passes only one test, it fails four, and the remaining four are equivocal due to absence of relevant data [23]. Further, a 2013 assessment of the quality of reports of cervical arterial dissection following cervical spinal manipulation similarly found lacking data to support a causal relationship [24].
In spite of the very weak data supporting an association between chiropractic neck manipulation and CAD, and even more modest data supporting a causal association, such a relationship is assumed by many clinicians. In fact, this idea seems to enjoy the status of medical dogma. Excellent peer reviewed publications frequently contain statements asserting a causal relationship between cervical manipulation and CAD [4,25,26]. We suggest that physicians should exercise caution in ascribing causation to associations in the absence of adequate and reliable data. Medical history offers many examples of relationships that were initially falsely assumed to be causal [27], and the relationship between CAD and chiropractic neck manipulation may need to be added to this list.
Conclusions
Our systematic review revealed that the quality of the published literature on the relationship between chiropractic manipulation and CAD is very low. A meta-analysis of available data shows a small association between chiropractic neck manipulation and CAD. We uncovered evidence for considerable risk of bias and confounding in the available studies. In particular, the known association of neck pain both with cervical artery dissection and with chiropractic manipulation may explain the relationship between manipulation and CAD. There is no convincing evidence to support a causal link, and unfounded belief in causation may have dire consequences.
Additional Information
Disclosures
Conflicts of interest: The authors have declared that no conflicts of interest exist.
Acknowledgements
The authors wish to thank Elaine Dean, MLS, of the Penn State Hershey Medical Center George T. Harrell Health Sciences Library, for her assistance with the systematic review.
1. Riddle DL, Schappert SM: Volume and characteristics of inpatient and ambulatory medical care for neck pain in the United States: data from three national surveys. Spine. 2007, 32:132�140.
2. Hurwitz EL, Chiang LM: A comparative analysis of chiropractic and general practitioner patients in North America: findings from the joint Canada/United States survey of health, 2002-03. BMC Health Serv Res. 2006, 6:49. 10.1186/1472-6963-6-49
3. Micheli S, Paciaroni M, Corea F, et al.: Cervical artery dissection: emerging risk factors . Open Neurol J. 2010, 4:50�55. 10.2174/1874205X01004010050
4. Schievink WI: Spontaneous dissection of the carotid and vertebral arteries . N Engl J Med. 2001, 344:898�906. 10.1056/NEJM200103223441206
5. Cassidy JD, Boyle E, C�t� PDC, et al.: Risk of vertebrobasilar stroke and chiropractic care: results of a population-based case-control and case-crossover study. Spine. 2008, 33:176�183.10.1097/BRS.0b013e3181644600
6. Dittrich R, Rohsbach D, Heidbreder A, et al.: Mild mechanical traumas are possible risk factors for cervical artery dissection. Cerebrovasc Dis. 2007, 23:275�281. 10.1159/000098327
7. Engelter ST, Grond-Ginsbach C, Metso TM, et al.: Cervical artery dissection: trauma and other potential mechanical trigger events. Neurology. 2013, 80:1950�1957.10.1212/WNL.0b013e318293e2eb
8. Rothwell DM, Bondy SJ, Williams JI: Chiropractic manipulation and stroke: a population based case-control study. Stroke. 2001, 32:1054-1060.
9. Smith WS, Johnston SC, Skalabrin EJ, et al.: Spinal manipulative therapy is an independent risk factor for vertebral artery dissection. Neurology. 2003, 60:1424-1428.10. Thomas LC, Rivett DA, Attia JR, et al.: Risk factors and clinical features of craniocervical arterial dissection. Man Ther. 2011, 16:351�356. 10.1016/j.math.2010.12.008
11. Biller J, Sacco RL, Albuquerque FC, et al.: Cervical arterial dissections and association with cervical manipulative therapy: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014, 45:3155�3174.10.1161/STR.0000000000000016
12. AAN (American Academy of Neurology): Clinical Practice Guideline Process Manual. Gronseth GS, Woodroffe LM, Getchius TSD (ed): AAN (American Academy of Neurology), St Paul, MN; 2011.
13. French J, Gronseth G: Lost in a jungle of evidence: we need a compass . Neurology. 2008, 71:1634�1638. 10.1212/01.wnl.0000336533.19610.1b 2016 Church et al. Cureus 8(2): e498. DOI 10.7759/cureus.498 10 of 11
14. Gross RA, Johnston KC: Levels of evidence: taking Neurology� to the next level . Neurology. 2009, 72:8�10. 10.1212/01.wnl.0000342200.58823.6a
15. Moher D, Liberati A, Tetzlaff J, et al.: Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009, 6:e1000097. Accessed: January 23, 2016: http://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1000097. 10.1371/journal.pmed.1000097
16. Stroup DF, Berlin JA, Morton SC, et al.: Meta-analysis of observational studies inepidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. 2000, 283:2008-2012.
17. Guyatt G, Oxman AD, Akl EA, et al.: GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011, 64:383�394. 10.1016/j.jclinepi.2010.04.026
18. Guyatt GH, Oxman AD, Kunz R, et al.: GRADE guidelines: 2. Framing the question and deciding on important outcomes. J Clin Epidemiol. 2011, 64:395�400. 10.1016/j.jclinepi.2010.09.012
19. Balshem H, Helfand M, Sch�nemann HJ, et al.: GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011, 64:401�406. 10.1016/j.jclinepi.2010.07.015
20. The Cochrane Collaboration: Cochrane Handbook for Systematic Reviews of Interventions (Version 5.1.0). Higgins JPT, Green S (ed): The Cochrane Collaboration, 2011.
21. Lee VH, Brown RD Jr, Mandrekar JN, et al.: Incidence and outcome of cervical artery dissection: a population-based study. Neurology. 2006, 67:1809-1812.
22. Hill AB: The environment and disease: association or causation?. Proc R Soc Med. 1965, 58:295�300.
23. Herzog W, Leonard TR, Symons B, et al.: Vertebral artery strains during high-speed, low amplitude cervical spinal manipulation. J Electromyogr Kinesiol. 2012, 22:740�746. 10.1016/j.jelekin.2012.03.005
24. Wynd S, Estaway M, Vohra S, Kawchuk G: The quality of reports on cervical arterial dissection following cervical spinal manipulation. PLOS ONE. 2013, 8:e59170. Accessed: February 8, 2016: http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0059170. 10.1371/journal.pone.0059170
25. Albuquerque FC, Hu YC, Dashti SR, et al.: Craniocervical arterial dissections as sequelae of chiropractic manipulation: patterns of injury and management. J Neurosurg. 2011, 115:1197�1205. 10.3171/2011.8.JNS111212
26. Debette S, Leys D: Cervical-artery dissections: predisposing factors, diagnosis, and outcome . Lancet Neurol. 2009, 8:668�678. 10.1016/S1474-4422(09)70084-5
27. Artenstein AW: The discovery of viruses: advancing science and medicine by challenging dogma. Int J Infect Dis. 2012, 16:e470�e473. 10.1016/j.ijid.2012.03.005
Ephraim W. Church 1 , Emily P. Sieg 1 , Omar Zalatimo 1 , Namath S. Hussain 1 , Michael Glantz 1 , Robert E. Harbaugh 1
1. Department of Neurosurgery, Penn State Hershey Medical Center
Corresponding author: Ephraim W. Church, [email protected]

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chiropractic, Chiropractic News, Physical Rehabilitation
How to Become A Chiropractor
A chiropractor is a doctor who specializes in musculoskeletal and nervous system problems. It is the belief of the chiropractic community that problems in these areas can cause adverse health issues, including lowered resistance to disease, illness, and injury.
Chiropractors manipulate the spine to realign spinal joints in their patients. By doing so, patients are expected to experience optimum health without the assistance of drugs or surgery. Instead, chiropractors expect the body will heal itself once the spine and spinal joints are in proper alignment. Additionally, chiropractors consider and address other lifestyle factors which are commonly recognized as significantly affecting health such as diet, rest, exercise, heredity, and environmental factors. They also make other recommendations for changes which are expected to improve the patient�s overall health.
Chiropractors perform many of the same tasks as other general and specialty doctors. Patient health histories are gathered, physical, neurological, and orthopedic examinations are performed, and various laboratory tests, x-rays, and diagnostic imaging tools are used to diagnose and analyze the patient�s condition. Other forms of treatment may be used or recommended by the chiropractor including ultrasound, massage, heat, water, acupuncture, or electric currents. Prescription drugs and surgery are not part of the services provided by chiropractors. Chiropractors may recommend patients to see other doctors or specialists to address health issues or concerns outside of their area of expertise. Some chiropractors choose to specialize in a certain type of practice, such as orthopedics, neurology, sports injuries, internal disorders, diagnostic imaging, or pediatrics.
The Bureau of Labor Statistics predicts a job growth increase of 17% in the chiropractic field over the next seven years. An increasing public interest in alternative healthcare methods is beneficial to the chiropractic field. The public is seeking healthy living options which do not include prescription medicines or surgery; instead, a substantial number of people are searching for solutions which emphasize healthy lifestyles. The non-invasive procedures provided by chiropractors in answer to their patients health issues and concerns appeals to the segment of the public looking for these types of answers.
SELECTING THE RIGHT CHIROPRACTIC COLLEGE
Chiropractor students should select a college which offers a strong science degree or pre-medical program. Some colleges may have an affiliation with chiropractic training schools, which all future chiropractors must successfully complete. Research chiropractic schools to determine which one you are most interested in attending; this will help you to determine if the school is linked to any of the colleges you are considering. Courses in biology, chemistry, and physics will be important to individuals looking to work in a medical field. Electives may be concentrated in health, fitness, and nutrition. Students should, if given the opportunity, study topics and courses related to kinesiology and sports medicine. Courses in psychology and sociology will also help students to gain a more comprehensive understanding of people and society, better preparing them to serve the public. Additionally, business courses ensure that future professionals understand how to successfully manage a business in the complex healthcare field, as medical professionals must understand finances, medical insurance processing, business laws, business practices, business ethics, and medical records maintenance.
CHIROPRACTIC SCHOOLS
Students must attend chiropractic college in order to enter the profession. Upon completion of the program, students will have earned a doctorate in chiropractic medicine. The Council on Chiropractic Education, or CCE, is the nationally recognized accrediting agency by the United States Secretary of Education which regulates the quality of the curriculum offered at chiropractic colleges. Currently there are 15 CCE accredited chiropractic institutions in the United States. These include, as listed on the CCE website:
-
- Cleveland University Kansas City: Overland Park, KS
- D�Youville College Doctor of Chiropractic: Buffalo, NY
- Life University College of Chiropractic: Marietta, GA
- Life Chiropractic College West: Hayward, CA
- Logan College of Chiropractic: Chesterfield, MO
- Southern California University of Health Sciences: Whittier, CA
- National University of Health Sciences: Lombard, IL and Pinellas Park, FL
- New York Chiropractic College: Seneca Falls, NY
- Northwestern College of Chiropractic: Bloomington, MN
- Palmer College of Chiropractic: Davenport, IA; San Jose, CA; and Port Orange, FL
- Parker College Of Chiropractic: Dallas, TX
- Sherman College Of Chiropractic: Spartanburg, SC
- Texas Chiropractic College: Pasadena, TX
- University of Bridgeport College of Chiropractic: Bridgeport, CT
- University of Western States College of Chiropractic: Portland, OR
Students attend chiropractic college for four years. During this time, students are taught the scientific and academic skills and knowledge required to become experts in the field of chiropractic medicine. The final year is spent in practice, performing the functions of a chiropractic doctor under the supervision of an experienced professional. The curriculum includes intensive study of neuromusculoskeletal conditions, nutritional and holistic health, specialized and focused curriculum in areas of acupuncture and oriental medicine, applied nutrition, and various other disciplines. Students will complete extensive course hours in diagnosis, biochemistry, anatomy, chiropractic technique, and philosophy and ancillary therapeutic procedures.
TAKING THE NATIONAL BOARD EXAM
The National Board Exam for chiropractors is administered by the NBCE. The test is given twice each year. The exam consists of three parts. Part one is 110 multiple choice questions relating to general anatomy, spinal anatomy, physiology, chemistry, pathology, microbiology, and public health. The second part also consists of 110 multiple choice questions, but in the areas of general diagnosis, neuromusculoskeletal diagnosis, diagnostic imaging, and principles of chiropractic, chiropractic practice, and associated clinical sciences. Part three of the test consists of another 110 multiple choice questions and 10 case vignettes covering the areas of diagnosis or clinical impression, clinical laboratory and special studies examination, chiropractic techniques, case management, physical examination, case history, and roentgenologic examination. Each part of the test is timed. Additional specialized testing is offered for applicants who choose to pursue an area of specialization.
LICENSING FOR CHIROPRACTORS
After successful completion of an accredited chiropractic program, graduates will need to obtain a license to practice in their resident state or the state in which they intend to practice. State licensure regulations may vary from state to state. It is important to research your state�s regulations prior to completion of the doctor of chiropractic program to ensure all conditions are met. The Federation of Chiropractic Licensing Boards is a nonprofit organization which provides a link to the licensure information in all states. Locate information for each state through this directory.
The information provided includes licensing fees, renewal requirements, national board testing requirements, security and criminal check requirements, additional certification requirements, continuing education, and malpractice insurance requirements. A link to each state licensing board is also provided.
CONTINUING EDUCATION FOR CHIROPRACTORS
The chiropractic field is experiencing an increase in advancements in technology and knowledge through research and academic exploration. Changing regulations are also an area in which chiropractic doctors will need to remain current. Each state maintains their own continuing education requirements upon which licensing will be contingent. Twenty-four credit hours of continuing education every two years is a common requirement. All programs must be board approved and conducted by approved colleges or chiropractic associations or organizations. Check with your state licensing board to determine if the program has been approved prior to enrollment.
PRACTICING AS A CHIROPRACTOR
After obtaining a doctorate and passing the licensing examination, a new chiropractor has many options ahead of them. Most chiropractors will end up working solo or in a group practice, with about one in three being self-employed. A small group will work in hospitals or physicians� offices. The median pay for Chiropractors in 2016 was $67,520, with the lowest 10 percent earning less than $32,380, and the highest earning more than $141,030. Chiropractors can further increase their salary by building up a strong client base and developing their own practice. Many times, chiropractors will work in the evening or on weekends to accommodate their patients.
DAY TO DAY PRACTICE
Chiropractors will spend a lot of time on their feet as they examine and treat patients. Some of the most important qualities that a chiropractor can have include decision-making, detail-oriented, dexterity, empathy, and interpersonal skills. If the chiropractor is operating his or her own practice, the ability to manage a staff of employees like secretaries and nurses is vital to the success of the practice. An understanding of the current healthcare system is also important, as that will determine what kind of payments a chiropractor may be able to receive, unless they work in a cash-only system. More information can be found in the Occupational Outlook Handbook provided by the BLS.
CHIROPRACTIC SPECIALTIES AND CERTIFICATIONS
Another way for chiropractors to increase their annual earnings or skills would be to specialize in one or more areas. Specializations can help a chiropractor better diagnose and treat chronic illnesses, sports injuries, and/or complex occupational injuries. The American Chiropractic Association and American Board of Chiropractic Specialties (ABCS) lists 14 specialties and provides guidance to maintain standards of chiropractic certification. These include, as listed on the American Chiropractic Association website:
| Certifying Body or Bodies |
Certification |
Description |
| American Chiropractic Board of RadiologyDiplomate (DACBR) |
Chiropractic Diagnostic Imaging (DACBR) Specialist |
Has additional training in interpreting diagnostic imaging results such as x-rays, CT scans, MRIs, and ultrasounds. |
| American Chiropractic Rehabilitation BoardDiplomate (DACRB) |
Chiropractic Physiotherapy and Rehabilitation (DACRB) Specialist |
Has had extensive postgraduate training in physiologic therapeutics and rehabilitation to better treat injuries that may have resulted from an accident or a sports injury. |
| American Chiropractic Rehabilitation BoardDiplomate (DACRB) |
Chiropractic Acupuncture (DABCA) Specialist |
Treats a wide variety of health conditions that include all body systems and tissues, and focuses special attention on the relationship between the spine, nervous system, and the meridian system. |
American Clinical Board of NutritionDiplomate (DACBN)
OR
Chiropractic Board of Clinical NutritionDiplomate (DCBCN) |
Chiropractic Nutrition (DACBN/CBCN) Specialist |
Is trained to encourage and promote a more advanced knowledge and use of nutrition in the practice of chiropractic for the maintenance of health and the prevention of disease. |
| American Board of Chiropractic InternistsDiplomate (DABCI) |
Chiropractic Diagnosis and Management of Internal Disorders (DABCI) Specialist |
Is trained as a holistic primary care physician specializing in modern medical diagnosis, functional medicine, and natural therapeutics. |
| Academy of Chiropractic Orthopedists Fellow (FACO) |
Chiropractic Orthopedist (DACO/DABCO) Specialist |
Has special knowledge of both the normal function and diseases of the bones, joints, capsules, discs, muscles, ligaments, and tendons, as well as their complete neurological components, referred organ systems and contiguous tissues, and is able to diagnose and treat the conditions related to them. |
American Chiropractic Neurology BoardDiplomate (DACNB) and sub-specialties:
- American Chiropractic Academy of Neurology Diplomate (DACAN)
- American Board of Chiropractic Neurology Diplomate (DABCN)
- American Board of Electrodiagnostic Specialties Fellow (FABES)
- American College of Functional Neurology Fellow (FAFCN)
- American Board of Vestibular Rehabilitation Fellow (FABVR)
- American Board of Childhood Developmental Disorders Fellow (FABCDD)
- American Board of Brain Injury & Rehabilitation Fellow (FABBIR)
- American Board of Neurochemistry & Nutrition Fellow (FABNN)
|
Chiropractic Clinical Neurologist (DACAN/DACNB) Specialist |
Is a DC specially trained in the clinical evaluation and treatment of conditions involving the central and peripheral nervous systems. |
| American Board of Forensic ProfessionalsDiplomate (DABFP) |
Diplomate of the American Board of Forensic Professionals (DABFP) |
Performs an orderly analysis, investigation, inquiry, test, inspection, and examination in an attempt to obtain the facts of a case, from which to form an expert opinion. |
American Chiropractic Board of Sports Physicians Diplomate (DACBSP)
OR
Certified Chiropractic Sports Physician (CCSP) |
Chiropractic Sports Physician (CCSP/DACBSP) Specialist |
Is trained in chiropractic sports medicine and exercise science in order to treat sports injuries, enhance athletic performance, and promote physical fitness. |
| American Chiropractic Board of Occupational Health Diplomate (DACBOH) |
Chiropractic Occupational Health (DACBOH) Specialist |
A DC trained in health care diagnosis and treatment choices for workplace neuromusculoskeletal injuries who is able to provide a broad range of work-related injury and illness prevention services for employee populations. |
| American Board of Chiropractic AcupunctureDiplomate (DABCA) |
Diplomate of the American Board of Chiropractic Acupuncture (DABCA) |
Dedicated to promoting high standards of competence and preserving the integrity of using acupuncture as an adjunct therapy to chiropractic treatment. |
| American Board of Chiropractic Pediatrics |
Diplomate in Clinical Chiropractic Pediatrics (DICCP) |
Support members who take care of children in their chiropractic practices, and to promote the acceptance and advancement of pediatric chiropractic care. |
These specialty �degrees� are given by their corresponding boards, which also maintain the level of expected qualifications and standards of excellency.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chiropractic News
Imagine a convention that mixes cutting-edge natural health seminars with a surfer dude�s attitude, a revivalist�s enthusiasm and a good measure of live rock-�n-roll. That�s the California Jam, which took place in Costa Mesa in January. Billed as �the biggest health, wellness and chiropractic event on the planet�, it�s an annual meeting of thousands of unapologetically alternative practitioners who mill about three floors of exhibitions, sampling detox juices, protein snacks, �bulletproof� coffee and vitamins.
There�s a buzz about urine tests for metabolites; people are talking cellular detoxification and energy-balancing therapies, and they�re trading spinal adjustments on a row of tables. Inside the auditorium, a roster of headliner speakers takes the stage for two days, but one of the biggest ticket draws this year was a relatively unknown figure: neurophysiologist and chiropractor Heidi Haavik, who is pioneering a whole new field of research into what happens to a person�s brain when a chiropractor adjusts their spine.
�There is so much more to chiropractic care than back and neck pain, and headaches,� enthuses Haavik, who studied neuroscience after graduating from the New Zealand College of Chiropractic and is now focusing on research.
Up to now, there�s been a gulf between the available published research and the practice. A handful of studies have shown that chiropractic works only modestly�yet substantially better than drugs�at nipping neck and back pain,1 and may help with migraine,2 and even mysteriously lower blood pressure3 which, for 40 years, has been linked to joint dysfunction in the neck.
But the research is hardly enough to support its position as the most popular alternative medical treatment for more than a century, used by 30 million people in the US alone each year.
�Haavik�s research may finally explain scientifically the amazing results chiropractors have in clinical practice,� says Ross McDonald, a practising chiropractor and President of the Scottish Chiropractic Association.
The neuroscience studies explore the underlying mechanism of those results�how the spine and central nervous system (CNS) are interconnected and �talk� to each other, and how dysfunction in the spine can affect health and well-being.

One of Haavik�s studies, published this year in the journal Brain Sciences, looked at the effect of chiropractic adjustments in 28 patients with �subclinical� pain�those with a history of intermittent back or neck ache or stiffness for which they were never treated�but who were in pain the day of the experiment. On examination, all had tender spots and restricted joint movement in their spines.
Compared with �sham� adjustments, chiropractic spinal adjustments of these people induced significantly greater brain activity, or �cortical excitability� (which has to do with neuro-electrical signals produced when brain or peripheral muscles are stimulated), as measured by transcranial magnetic stimulation (TMS), which uses magnetic fields to stimulate nerve cells in the brain, as well as arm and leg muscle strength.
Increases in muscle strength have proved to be driven by brain activity resulting from spinal manipulation, and not by any changes made to the spinal cord itself. This offers a host of possibilities for, say, recovering muscle strength after nervous-system injuries. As the study concluded, �spinal manipulation may therefore be indicated� for patients who have lost muscle tone, or are recovering from a stroke or from orthopedic surgery that affects the muscles. It may even be of interest to athletes who participate in sports.4
These findings have confirmed a 2015 study which showed that, following a full-spine chiropractic adjustment session, voluntary leg muscle strength in study participants increased by 16 per cent, while electrical activity readings from the measured muscle increased by nearly 60 per cent. But most spectacularly, the researchers (from the Centre for Chiropractic Research in New Zealand) discovered a 45 per cent increase in the reflex pathway �drive� from the brain to muscle (an indicator of the ability of the brain to activate it). By contrast, the control participants who underwent the sham adjustment actually lost strength and brain drive to the measured muscle.5
This same Auckland-based team, led by Haavik and two colleagues are now embarking on some groundbreaking research involving brain-body communication in stroke patients.6 A preliminary study had tested the effect of a single chiropractic adjustment on 12 stroke patients, and found that it increased leg muscle strength by an average of 64 per cent and brain drive to the limb by more than 50 per cent. In contrast, both measurements fell after the sham adjustments in the controls.
Ordinarily, you wouldn�t expect to see muscles gain in strength after being asked to repeatedly resist something because muscles become fatigued. Now, that we have the technology to objectively measure an increase in muscle strength after an intervention, Haavik says, these results suggest that�chiropractic care is not only preventing fatigue, but making [muscles] even more efficient at producing force�.
The potential results of the new study could have a significant impact on the role of chiropractic care in people who have reduced muscle function as a result of stroke, she says.
Injury Risk
One interesting recent study by Haavik and her colleagues looked specifically at the impact of chiropractic on the risk of falls among older people.7
Falling is a significant cause of death, injury and health decline in the elderly, with about 30-40 per cent of older adults who still live independently suffering from at least one fall each year or more as they age.
In this randomized controlled trial, half of the group of 60 community-dwelling people, aged over 65 and living in Auckland, received 12 weeks of chiropractic care (two visits per week), while the other half received the �usual care�, which didn�t include seeing a chiropractor.
The patients were tested on their proprioception (in this case, their awareness of where their ankle joint was positioned), postural stability and ability to process �multi-sensory� information�a sound-induced flash illusion test, using flashing lights and beeps. This test is used to screen for fall risk, as it measures how well people can process two different kinds of stimuli at a time.8 The participants were also given a sensorimotor function test, which measured their ability to move their feet in response to a panel that suddenly lit up on the floor, plus a questionnaire based on their self-perceived health-related quality of life.
Over the 12 weeks of the study, the group receiving chiropractic care showed significant improvement in ankle joint position sense, meaning their brains may have become more accurately aware of what was going on in their feet; they were also able to react and move their foot onto the illuminated panel on the floor more quickly than before the chiropractic care. These improvements were not seen in the control group.
The chiropractic patients were 13 per cent better able to accurately report the correct number of flashes with the corresponding number of beeps�meaning they had lowered their risk for falls.
What�s more, at the end of the study, the participants who had received the chiropractic care reported a 2.4-fold increased improvement in the quality-of-life questionnaire compared with the controls.7
Your Plastic Brain
Haavik is now trying to explain how chiropractic achieves all this, and why restoration of proper movement is able to so profoundly affect the brain and overall health.
The CNS�the brain and spinal cord�and all the nerves beyond the CNS (the peripheral nervous system, or PNS) is a complex network comprising as many as 10 billion nerve cells (also called �neurons�) and 60 trillion synapses�tiny little junctions between neurons that mediate the �talk� across highly specialized neural circuits via chemicals called �neurotransmitters�. Indeed, nerves feed out of each segment of the spine like strands of spaghetti, and facilitate communication back and forth with various regions of the body.
Everything we do�from our basic motor reflexes to our capacity to experience abstract thoughts and feelings�relies on the precision of the computational processes performed by these CNS and PNS neural circuits. They, in turn, depend on having healthy excitatory and inhibitory systems.
A neuron gets �excited� when it�s �talked to� loudly enough, or stimulated, and this sends an electrical message down one of the neuron�s extensions (called �axons�), so allowing it to talk to another nerve cell by releasing more neurotransmitters at the synapses.
Such talk happens all the time as input comes in from our external senses (eyes, ears, mouth, nose and touch), as well as through an inner �map� of the location of our muscles and joints in three-dimensional space relative to each other (proprioception), as the brain carries out its decisions and functions.
Contrary to decades of scientific dogma, a recent wave of research has shown that the brain is actually highly adaptable to its ever-changing environment throughout life. It does this by keeping an up-to-date tab on its sensory inputs and its internal map of the self. This ability to adapt is known as �neural plasticity�.
Haavik likens the plasticity of the CNS to the subtle changes in the bed in a flowing stream. �You can never really step into the same river twice; the water, stones and silt of the riverbed are constantly changing,� she says. Likewise, your brain is changing with every thought and every execution, and is in a constant state of flux.
In fact, she believes her research demonstrates that vertebral subluxations (dysfunctional spinal segments; see box, page 33) lead to a breakdown in the way the brain perceives and controls the movement of the spine. And this spinal dysfunction doesn�t just affect how the brain then perceives and controls the spine, but also how it perceives and controls other parts of the body as well.
When the brain gets even slightly wrong information, it builds a faulty map that can impede neural signaling as effectively as damped sensory input�like wearing a blindfold or losing the sense of taste. And that translates to faulty functioning.
Chronic pain and neurodegenerative disorders have been linked to these faulty perceptions by the plastic brain.9 �Pain and conditions with other symptoms don�t necessarily happen all of a sudden for no reason. They can slowly develop without your awareness, a bit like a thousand straws on a camel�s back before it breaks,� says Haavik. �Only when the last straw is added do you feel the effect.�
Haavik�s team hypothesizes that spinal adjustments that restore normal movement also restore more normal data input from the spine to the brain. This, in turn, allows the spinal cord, brain stem and brain to process any incoming information more coherently.
�We believe this to be the mechanisms by which adjustments of vertebral subluxations can improve nervous system function, as observed daily in chiropractic practices all around the world.�
While the New Zealand researchers are reluctant to speculate on immunity, an emerging body of research is demonstrating the interconnectedness of both the nervous and immune systems too. An entirely new lymphatic system in the brain was only discovered in 2015 by a team of researchers at the University of Virginia,10 which highlights how limited our understanding of the brain, and the effect of the nervous system on global health, still is. It also raises further questions about how improving one system can lead to improvement in the other�and so perhaps why some people experience benefits to their immune-mediated disease with chiropractic manipulations.
�What is becoming clear is that chiropractic care seems to impact our brain�s inner reality by restoring the proper processing and integration of sensory information, which alters the way our brain controls our body,� says Haavik.
�It�s so exciting to see that there are other possible ways now to explain the effects of chiropractic that are actually congruent with current neuroscience,� she adds. �It�s actually more profound and powerful than we could have ever thought.�
The Many Faces Of Chiropractic
There are two schools of thought in chiropractic: the �mechanics�, who claim it should be absorbed into mainstream medicine as a standardized treatment for back and neck pain; and the �vitalists�, who believe that the treatment is much more far-reaching, as they�ve seen it help cases of fatigue, joint pain, migraines, allergies, asthma, bedwetting and even infertility.
The latter philosophy is radically different from the current medical paradigm. �The body has an innate ability to heal, provided there is no interference,� says Gilles LaMarche, vice president of professional relations at Life University in Atlanta, Georgia, the world�s largest chiropractic college. �It is self-developing, self-maintaining and self-healing.�
In this vitalistic view of chiropractic, when you get an infection or scrape your knee, the best practitioner merely assists the body in getting on with its own spontaneous and spectacular business of healing itself.
The chiropractor�s job, as vitalists see it, is to remove any interference in the body at the level of the spine, which they consider central.
�Conventional medicine doesn�t interpret symptoms as we interpret symptoms,� explains LaMarche from his end of chiropractic.
He sees fever, for instance, as one of the body�s natural mechanisms to fight infection: raising the body�s temperature kills bacteria and viruses, and facilitates other immune functions.
�Many doctors see fever as bad, as something to reduce,� he says, �and they give Tylenol [paracetamol], not considering it as a toxin that is actually going to stay in the liver and therefore interfere with healing and health.�
How Chiropractic Changes The Brain
So what�s going on in the brain after a chiropractic adjustment that could be increasing muscle strength in stroke patients? As a 2016 study from Aalborg University Hospital in Denmark demonstrated, a single chiropractic adjustment helps to improve something called �somatosensory integration� (when the brain receives accurate sensory input, so allowing it to properly organize and execute subsequent behaviors).1
Such a change mostly happens in the prefrontal cortex, that part of the brain known to be a key player in executive functions. It�s a sort of command control centre, integrating and coordinating the multiple neural inputs from a constantly changing environment to solve problems and achieve goals.
�Chiropractic care, by treating the joint dysfunction, appears to change processing by the prefrontal cortex,� the authors conclude.
So, while some chiropractors (and their patients) may have thought their adjustments were making changes locally and directly from the spine, in fact, the change is apparently effected indirectly by being sent to �central command� (the brain), then redirected back down neuronal chains to give the perception of reduced pain as well as other benefits.
�This suggests that chiropractic care may, as well, have benefits that exceed simply reducing pain or improving muscle function and may explain some claims regarding this made by chiropractors,� the study researchers say.
These claims include the ability of adjustments to increase muscle strength and core stability, improve reaction time and proprioception (your awareness of your body�s position in space), and so reduce the risk of injury.
What Is A Subluxation?
In 1895 in Iowa, the founder of chiropractic, Daniel David Palmer, claimed to have restored the hearing of deaf janitor Harvey Lillard by adjusting the part of his spine that Palmer could feel was �out of alignment�.
From this, he devised a theory that �misaligned� or �out-of-place� spinal segments interfere with proper nerve function, and that �adjusting� these segments back to their normal position relieves pressure on the nerves and restores neural function.
Chiropractors assess spines for areas where some of the small muscles that attach to the individual vertebrae have become tight due to injury, hunching over mobile phones and computers, or simply overuse. When these tight muscles cause the vertebrae�the small bones that make up the spine�to twist, certain parts of the bones can protrude and feel �misaligned� or �stuck�. Chiropractors call it a vertebral �subluxation� or �joint restriction�.
�It is more that a bone is functioning or moving in a less than ideal way�in a manner that is not �normal� for the body,� says Heidi Haavik.
And chiropractors counter this abnormality by �adjusting� it. �We don�t really put bones back in place when we adjust the spine,� she explains. The aim of the short, quick movements of chiropractic adjustments to the spine are to restore its natural range of movement.
How To Find A Good Chiropractor
All chiropractors must attend a licensed chiropractic college or university, and undergo at least four years of training in anatomy, neurology, physiology, radiology, pathology, clinical diagnostics and clinical nutrition, as well as physiotherapy and chiropractic techniques.
In the UK, chiropractors must pass a national exam to ensure competency. It is illegal to practice without first registering with the General Chiropractic Council.
Apart from these legal requirements, chiropractors have a broad range of approaches, specialities and techniques. Make sure to choose a chiropractor who:
��Meets your particular needs. Some chiropractors take a biomechanical approach, or treat a narrow range of conditions and only see people when they have a problem, like pain, while others take a �wellness� approach and treat people to prevent problems. Many chiropractors have special areas of focus: sports injuries, pregnancy, children, or even functional medicine, testing for metabolic deficiencies such as low vitamin D levels and prescribing supplements.
� Has a good reputation. It�s worth considering if other people have had good results.
� Talks with you at no cost to discuss your needs and their skills and services, and employs techniques that suit you. Some chiropractors use manual adjustments only, while others use devices like drop-tables�examination tables that move when the chiropractor adjusts so the impulse is delivered by the release-action of the table�and activators�hand-held tools that resemble a tire-pressure gauge and are spring-activated to deliver small and precisely controlled impulses to areas like the cervical (neck) spine. Some may also be trained in techniques like acupuncture, dry needling (acupuncture needles are inserted in muscle tissue to stimulate the release of �trigger points�, where muscles have gone into spasm) and active release technique (ART), which also targets contractions of muscles, ligaments and tendons to reduce joint stress.
� Carries out a thorough assessment before beginning treatment. A medical history and physical exam should be done to rule out conditions that need further referral or should not be treated by chiropractic. A chiropractor is trained to perform and read X-rays, which are sometimes required, but only if they meet standardized criteria.
� Gives you clear outcome measures to gauge improvement, such as less pain or an overall improved sense of wellbeing.
� Gives you enough time and attention. The best practitioner is also a coach or partner who can help you achieve your best state of health. Only choose someone who truly supports you.
Source: �Celeste McGovern

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chiropractic News
The importance of Magnetic Resonance Imaging to evaluate the integrity of the lumbar posterior ligament complex post trauma.
Abstract: Posterior ligamentous complex(PLC), consisting of the supraspinous ligament, interspinous ligament, ligamentum flavum, and the facet joint capsules is thought to contribute significantly to the stability of the lumbar spine. There has been much debate on whether Magnetic Resonance Imaging(MRI) is specific and sensitive in diagnosing pathology to the PLC. The objective is to determine the necessity of MRI imaging for evaluating the integrity of the lumbar posterior ligament complex post trauma.
Key Words: Magnetic Resonance Imaging(MRI), interspinous ligament, posterior ligament complex, low back pain, ligament laxity, electromyography, impairment rating
A 41-year-old male, presented to my office for an examination with complaints of low back pain with numbness, tingling and weakness into the left lower extremity after he was the restraint driver in a motor vehicle collision approximately three and a half months� post trauma.�He�rated the pain as a�3/10 on a visual analog scale with 10/10 being the worst and the pain and noted the pain as being�present most of the time.� He stated that he was on pain killers daily and this helped manage his daily activities. Without pain killers his pain levels are rated 8/10 being present most of the time. The pain killers stated by the patient are Oxycodone and Naproxen.
He�reported that the pain would be aggravated by activities which required excessive standing, repetitive bending, and lifting. He further noted that in the morning the pain was increased and his left leg would be numb and weak for about the first hour.
The patient stated that his care to date had been managed by a pain management clinic and that he had minimal improvement with treatment which has included physical therapy and massage therapy. He reported the pain clinic next recommended steroid injections which he refused. He states there has been was no imaging ordered and that an Electromyography(EMG) had been performed. He was told the test was negative for pathology.
Prior History: No significant medical history was reported.
Clinical Findings:�The patient is 6�0� and weighs 210 lbs.
Physical Exam Findings:
Cervical Spine:
Cervical spine range of motion is full and unrestricted. Maximum cervical compression is negative. Motor and other regional sensory exam are unremarkable at this time.
Thoracic Spine:
Palpation of the thoracic spine region reveals taught and tender fibers in the area of the bilateral upper and mid thoracic musculature. Thoracic spine range of motion is restricted in flexion, extension, bilateral lateral flexion, and bilateral rotation. Regional motor and sensory exam are unremarkable at this time.
Lumbar Spine:
Palpation of the lumbosacral spine region reveals taught and tender fibers in the area of the lumbar paraspinal musculature. Lumbar spine range of motion is limited in flexion, extension, bilateral lateral flexion and bilateral rotation. Extension restriction is due to pain and spasm. Straight leg raise causes pain at approximately 50 degrees when testing either side in the left low back. There is no radicular symptomatology down the leg. Kemp�s maneuver recreates pain in the L4 region on the left. No radicular symptoms are noted. The patient is able to heel and toe walk. Regional motor and sensory exam is unremarkable at this time other than L4, L5 and S1 dermatomes having decreased sensation with light touch.
Muscle testing of the upper and lower extremities was tested at a 5/5 with the exception of the left quadricep tested at a 4/5.� The patient�s deep tendon reflexes of the upper and lower extremities were tested including triceps, biceps, brachioradialis, patella, and Achilles and all were tested at 2+ bilaterally except the left patellar reflex was 1+.
RANGES OF MOTION EVALUATION
All range of motions are based on the�American Medical Association�s Guides to the Evaluation of Permanent Impairment, 5th�Edition1�and performed by a dual inclinometer for the lumbar spine.
�� Range of Motion������Normal�������� Examination�������� % Deficit
| Flexion |
60 |
48 |
|
20 |
| Extension |
25 |
12 |
|
52 |
| Left Lateral Flexion |
25 |
16 |
|
36 |
| Right Lateral Flexion |
25 |
18 |
|
28 |
An MRI was ordered to rule out gross pathology.
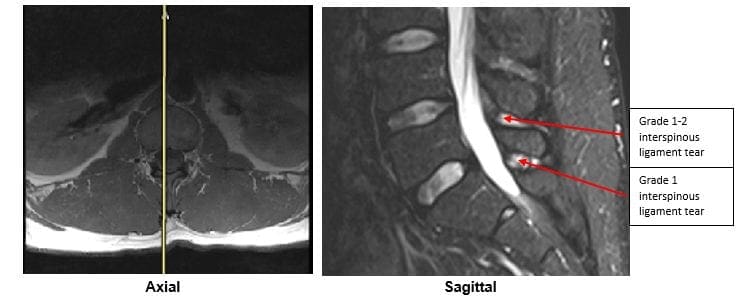
Imaging:
�
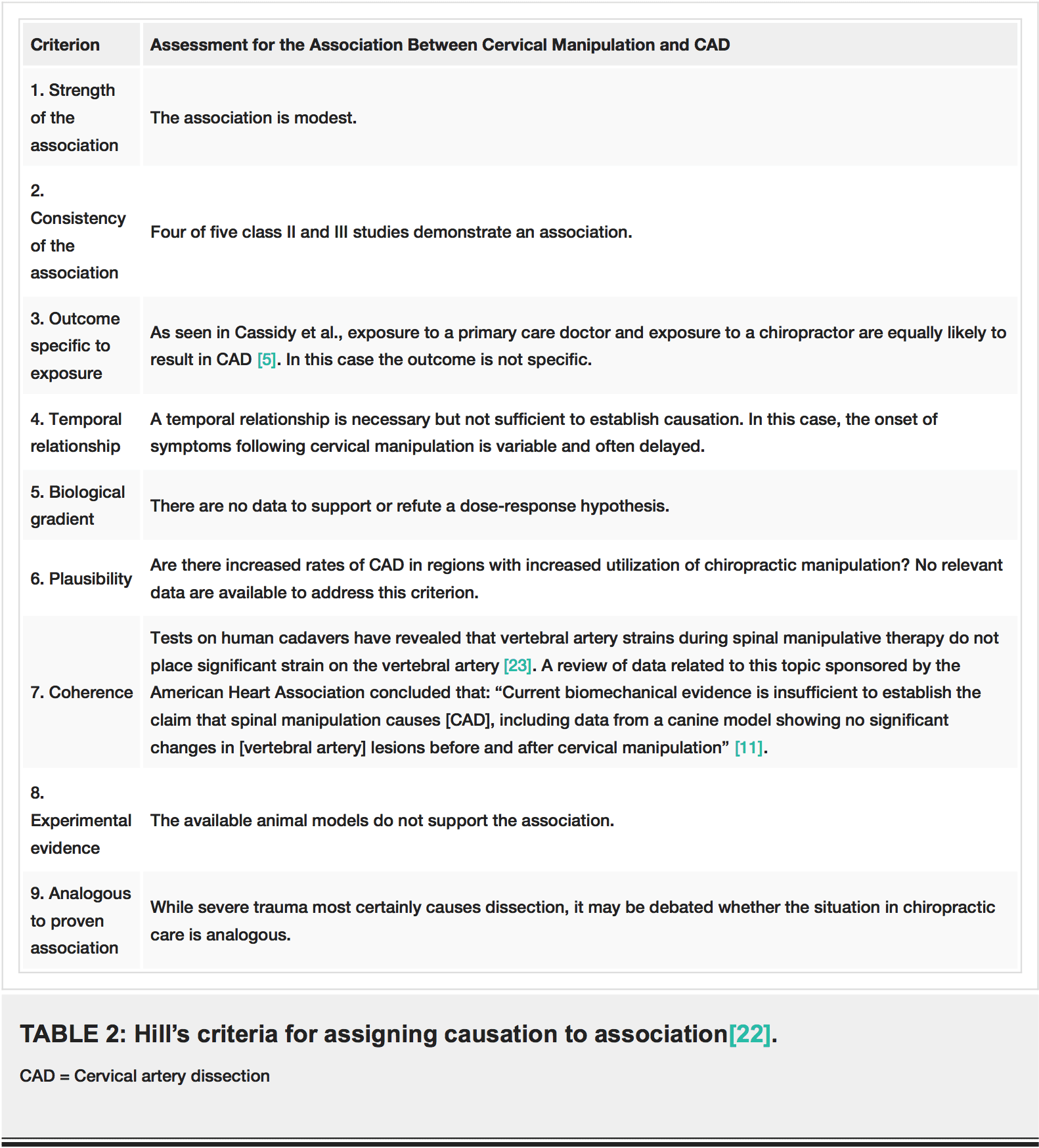
A lumbar MRI reveals;
1)��� Mild disc bulges at T11-T12, T12-L1, L1-L2 and L5-S1
2)��� Low disc signals indicative of disc desiccation at T11-T12, T12-L1, L1-L2, L2-L3, L3-L4 and L4-L5
3)��� Retrolisthesis of 2mm at L3-L4
4)��� Mild ligamentous hypertrophy at L1-L2, L2-L3, L3-L4, L4-L5 and L5-S1
5)��� L4-L5 has a Grade 1-2 tear of the interspinous ligament with mild inflammation
6)��� L5-S1 has a Grade 1 interspinous ligament tear with mild inflammation
After reviewing the MRI I ordered lumbar x-rays to rule out ligament laxity.
X-RAY STUDIES

Lumbar x-rays reveal the following:
1)��� Left lateral tilt
2)��� Retrolisthesis at L1 of 3mm
3)��� Retrolisthesis at L2 of 3mm
4)��� Combined excessive translation of 4mm of L1 during flexion-extension
5)��� Combined excessive translation of 4mm of L2 during flexion-extension
6)��� Excessive translation of L3 in extension posteriorly of 2.5mm
7)��� Decreased disc space at L5-S1
Chiropractic care was initiated. The patient was placed on an initial care plan of 2-3x/week for 3 months and then a recommended break in care for one month so the patient could be evaluated for permanency while he was not care dependent.
At maximum medical improvement, he had continued low back pain rated 4/10, continued numbness and tingling into his left leg and left quadricep weakness rated 4/5. He does not need pain killers for pain management anymore. He continues chiropractic care every two weeks to manage his symptoms.
Conclusion:
In this specific case, pathology to the posterior ligament complex diagnosed on MRI lead to the x-ray finding of excessive translation at L1-L2 and L2-L3. The patient was given a permanent impairment rating of 22% based on my interpretation of the American Medical Association�s Guides to the Evaluation of Permanent Impairment, 5th�Edition1. The interspinous ligament tears at the L4-L5 and L5-S1 level would not have been diagnosed without the MRI.
There has been much debate on whether MRI imaging has a role in evaluating lumbar PLC. MRI is a powerful diagnostic tool that can provide important clinical information regarding the condition of the PLC. Useful sequences for spinal MRI in trauma include sagittal and axial T1-weighted images, T2-weighted FSE, fat-saturated T2-weighted FSE, and STIR sequences to highlight bone edema.2�Ligamentous injuries are best identified on T2-weighted images with fat saturation because the ligaments are thin and bonded on either side by fat, which can appear as hyperintense on both T1 and T2 images.3�T1-weighted images are inadequate in isolation for identifying ligamentous injuries.4�
The diagnostic accuracy for MRI was reported for both supraspinous ligament and interspinous ligament injury with a sensitivity of 89.4% and 98.5%, respectively, and a specificity of 92.3% and 87.2% in 35 patients.5
For patients with persistent symptoms after trauma an MRI may be indicated to evaluate posterior ligamentous complex integrity.
Competing Interests:� There are no competing interests in the writing of this case report.
De-Identification: All of the patient�s data has been removed from this case.
References:
1. Cocchiarella L., Anderson G. Guides to the Evaluation of Permanent Impairment, 5th Edition, Chicago IL, 2001 AMA Press.
2. Cohen, W.A., Giauque, A.P., Hallam, D.K., Linnau, K.F. and Mann, F.A., 2003. Evidence-based approach to use of MR imaging in acute spinal trauma.�European journal of radiology,�48(1), pp.49-60.
3. Terk, M.R., Hume-Neal, M., Fraipont, M., Ahmadi, J. and Colletti, P.M., 1997. Injury of the posterior ligament complex in patients with acute spinal trauma: evaluation by MR imaging.�AJR. American journal of roentgenology,�168(6), pp.1481-1486.
4. Saifuddin, A., Green, R. and White, J., 2003. Magnetic resonance imaging of the cervical ligaments in the absence of trauma.�Spine,�28(15), pp.1686-1691.
5. Haba H, Taneichi H, Kotani Y, et al. Diagnostic accuracy of magnetic resonance imaging for detecting posterior ligamentous complex injury associated with thoracic and lumbar fractures.�J Neurosurg. 2003; 99(1 Suppl):20-26.
SaveSave




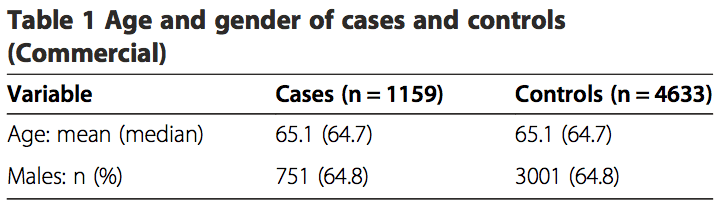
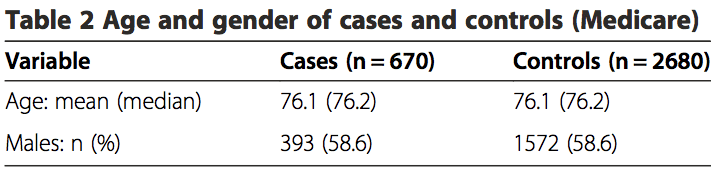
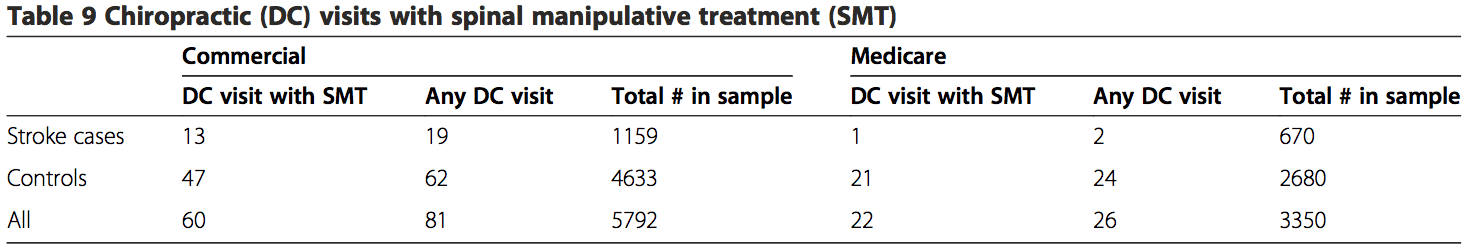
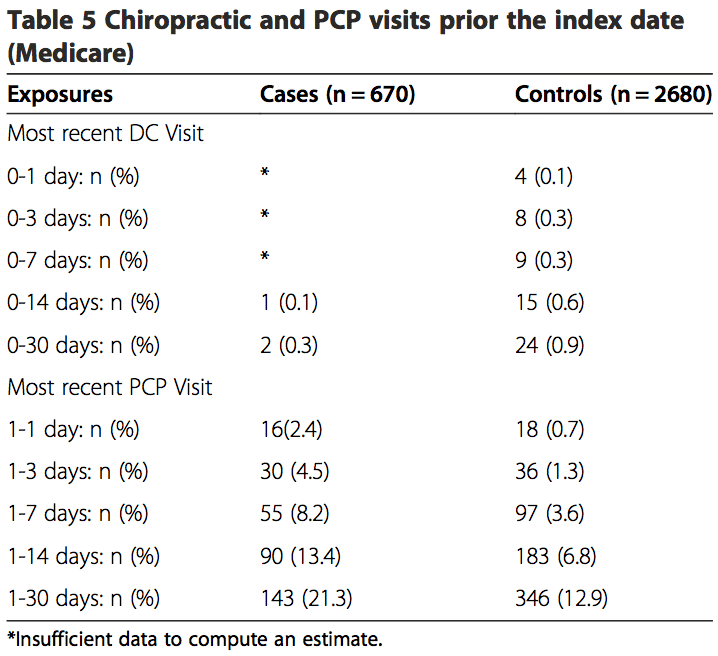
 Among the commercially insured, 1.6% of stroke cases had visited chiropractors within 30 days of being admit- ted to the hospital, as compared to 1.3% of controls visit- ing chiropractors within 30 days prior to their index date. Of the stroke cases, 18.9% had visited a PCP within 30 days prior to their index date, while only 6.8% of controls had visited a PCP (Table 4). The proportion of exposures for chiropractic visits was lower in the MA sample within the 30-day hazard period (cases = 0.3%; controls = 0.9%). However, the proportion of exposures for PCP visits was higher, with 21.3% of cases having PCP visits as compared to12.9% for controls (Table 5).
Among the commercially insured, 1.6% of stroke cases had visited chiropractors within 30 days of being admit- ted to the hospital, as compared to 1.3% of controls visit- ing chiropractors within 30 days prior to their index date. Of the stroke cases, 18.9% had visited a PCP within 30 days prior to their index date, while only 6.8% of controls had visited a PCP (Table 4). The proportion of exposures for chiropractic visits was lower in the MA sample within the 30-day hazard period (cases = 0.3%; controls = 0.9%). However, the proportion of exposures for PCP visits was higher, with 21.3% of cases having PCP visits as compared to12.9% for controls (Table 5).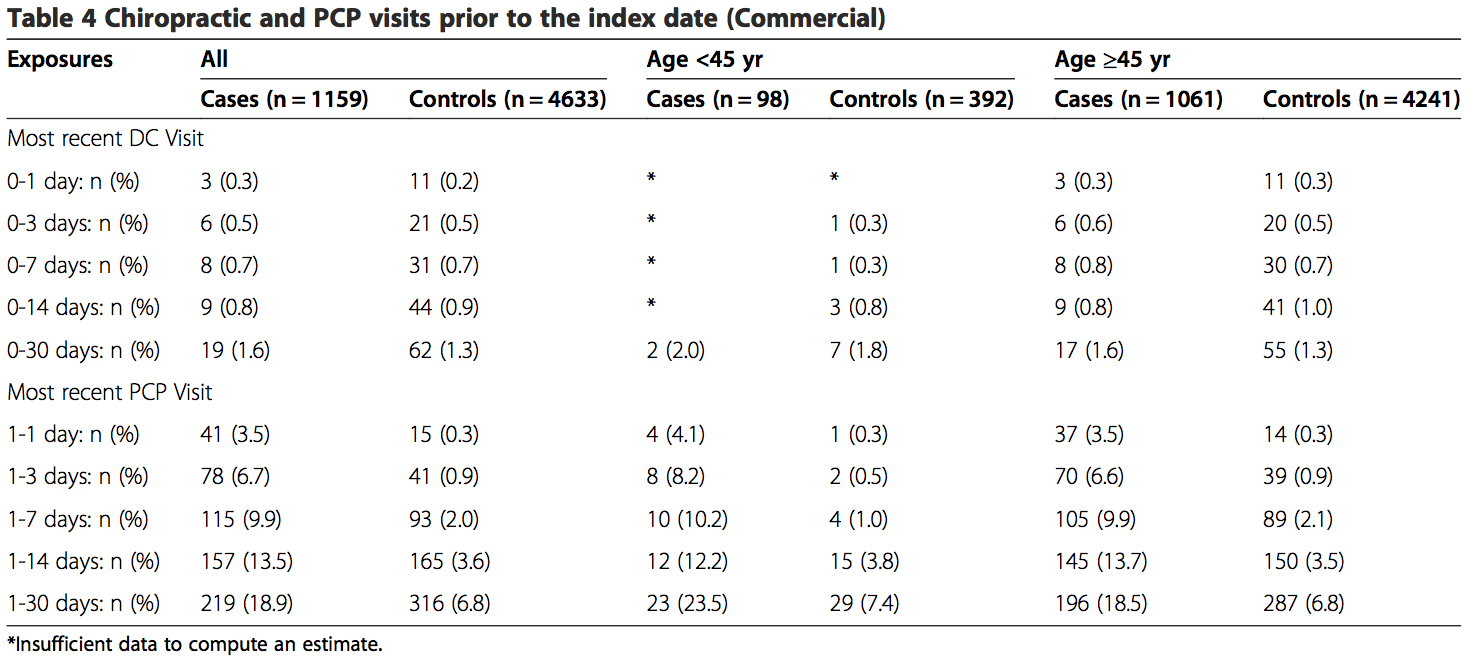
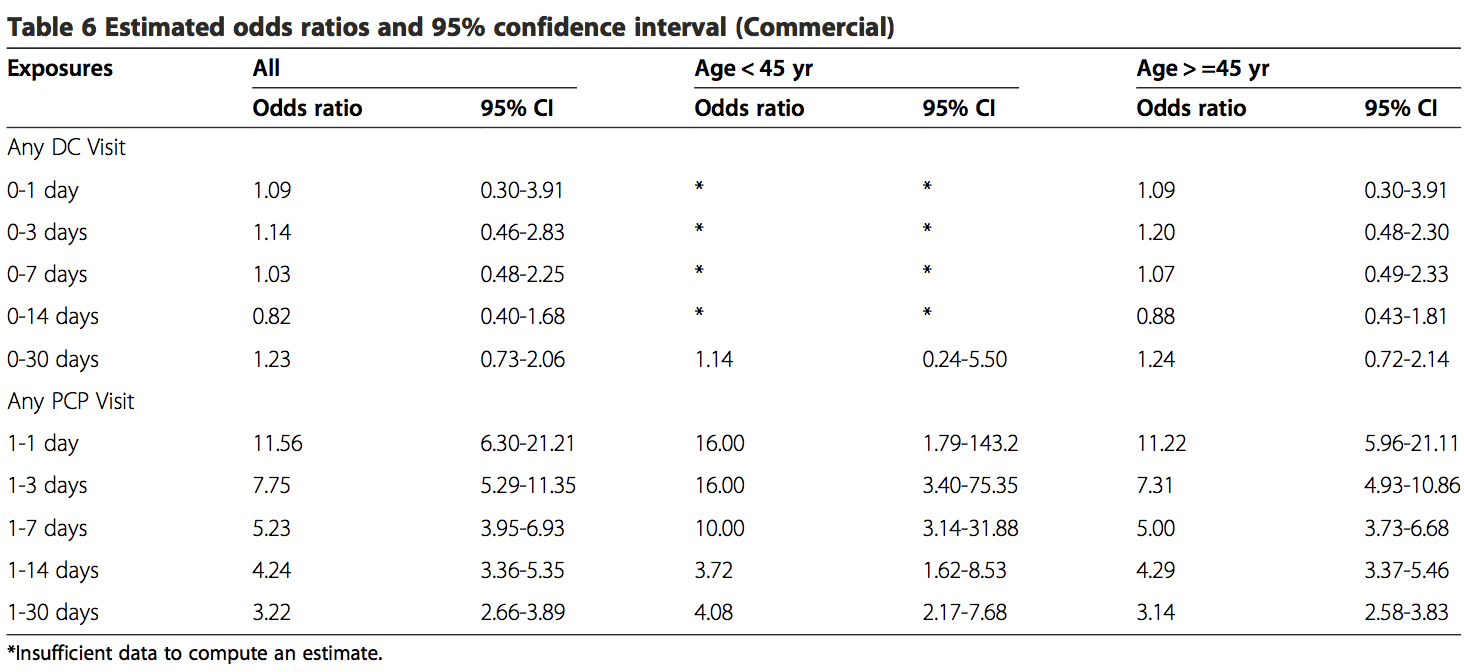
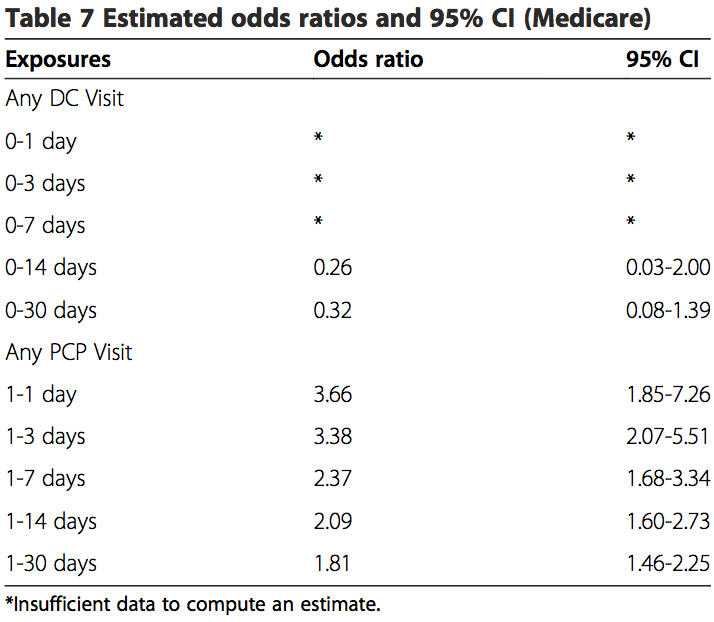
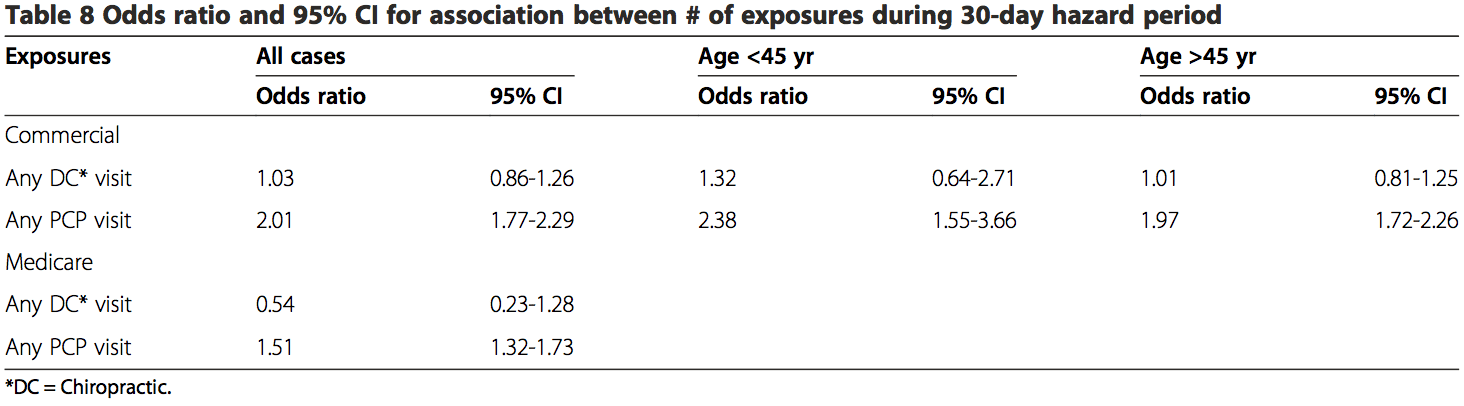
 The results from the analyses of both the commercial population and the MA population were similar (Tables 6, 7 and 8). There was no association between chiropractic visits and VBA stroke found for the�
The results from the analyses of both the commercial population and the MA population were similar (Tables 6, 7 and 8). There was no association between chiropractic visits and VBA stroke found for the�