by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chiropractic, Chronic Back Pain, Lower Back Pain
Chiropractors think that good health is decided by way of a healthy nervous system, particularly a healthy spinal column. Sometimes, vertebrae become misaligned and put pressure on the nerves exiting the spinal cord. The misalignment of a vertebra is called a chiropractic subluxation.
Chiropractors use specific methods to return the vertebrae in their proper locations or muster them to allow them to go freely when subluxations happen. These techniques are called spinal manipulations or adjustments. During an adjustment, the vertebra is freed in the misaligned location and returned to the right place in the spinal column. The adjustment permits the entire body to cure and preserve homeostasis once performed.
Chiropractors Are Trained In Many Different Adjustment Techniques

Some are done by hand; some necessitate using specialized instruments. Since each patient is different, your chiropractor will pick the best technique for the state. Nevertheless, don’t hesitate to ask the chiropractor which technique she or he will be doing and the way that it will be achieved.
Common Adjustment Techniques Employed By Chiropractors Are The Following:
- Toggle Drop – this is when the chiropractor presses down firmly on a specific part of the back. Subsequently, using a drive that is precise and rapid, the chiropractor aligns the spine. This really is accomplished to enhance mobility in the vertebral joints.
- Motion Palpation – this hand-on procedure is performed to determine in case your vertebrae are moving freely inside their normal planes of motion.
- Lumbar Spin -the chiropractor positions the patient on her or his side, then implements a thrust that is quick and precise returning it to its proper place.
- Release Work – the chiropractor applies gentle pressure using her or his fingertips to separate the vertebrae.
The chiropractor applies a quick thrust at once the table drops. The dropping of the table allows for a lighter adjustment without the twisting postures that can accompany the manual adaptation.
- Instrument adjustments – of correcting the spinal column frequently the gentlest ways. The patient lies on the table while a string is used by the chiropractor face down – filled activator instrument to do the adjustment. This technique is frequently used to perform adjustments on creatures too.
- Manipulation done under anesthesia (or twilight sedation) – this is performed by a chiropractor certified in this technique in a hospital outpatient setting when you’re unresponsive to traditional adjustments
Keep in mind that before you experience complete relief out of your symptoms you may really need to go back to the chiropractor’s office for additional adjustments.

Call Today!

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Fitness, Health, Wellness
This article originally appeared on Time.com.�
People who run marathons go through intense training before enduring the physically grueling 26.2-mile event�so it�s little wonder their health can sometimes suffer. But on marathon days, the event can also create unexpected problems for non-runners who need urgent medical care.
In a new report published in the New England Journal of Medicine, researchers found that road closures and traffic disruptions on marathon days can lead to delays in emergency care that can cost people their lives.
Dr. Anupam Jena, from the department of health care policy at Harvard Medical School and Massachusetts General Hospital, and his colleagues analyzed data from Medicare claims for hospitalizations for heart attack in 11 cities that hosted marathons from 2002 to 2012. They compared the death rates of these people on marathon days to those a few weeks before and after the marathon. People who had heart attacks on marathon days had a 13% higher rate of death than people on other days. Ambulances also took 4.4 minutes longer on days marathons were run.
�We were expecting to see there would potentially be delays in care,� says Jena, �but not necessarily increases in mortality. It�s difficult to influence mortality; you would have to have substantive delays in care.�
RELATED:�Is Running Good or Bad for Your Knees?
Road closures, detours and other changes in traffic patterns were dramatic enough to cause delays that could affect a person�s chance of surviving a heart attack, the team found. Over a year, marathons could contribute to an additional four deaths, based on the 30-day mortality rate calculations. The effect remained strong even after they adjusted for the possibility that more people visit a city hosting a marathon, and therefore statistically there may simply be more heart events. The researchers also made sure that hospitals and emergency services were not short-staffed or overburdened with the added volume of requests. All of these factors were similar on marathon and non-marathon days.
The disruption in traffic during a marathon is the primary reason for delays in care, Jena says. That�s good news because it�s a fixable problem; marathon planners can ensure that access to hospitals is not congested and affected by the race route.
The other lesson from the study is useful for people in need of medical attention. A quarter of the people in the study chose not to call an ambulance and instead drove themselves to the hospital�perhaps because they thought that emergency services were tied up with the marathon�and these people seemed to account for most of the higher mortality on marathon days, says Jena. That may be because they were forced to take more circuitous routes to reach the hospital, he says. �They don�t experience the four-minute delays of ambulance transport; they�re experiencing much larger delays because they are trying to drive themselves.�
Even with the delays, ambulances were the best form of transportation to the emergency room. �Anybody thinking of driving to the hospital themselves on the day of a major public event should pick up the phone and call 911,� Jena says.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chiropractic, Mobility & Flexibility, Power & Strength
I have been travelling through Athens and now Istanbul. My 11 year old is a Percy Jackson nut and has been filling me in with the who’s who of Greek mythology and I am learning Latin words every day. Quite an education!
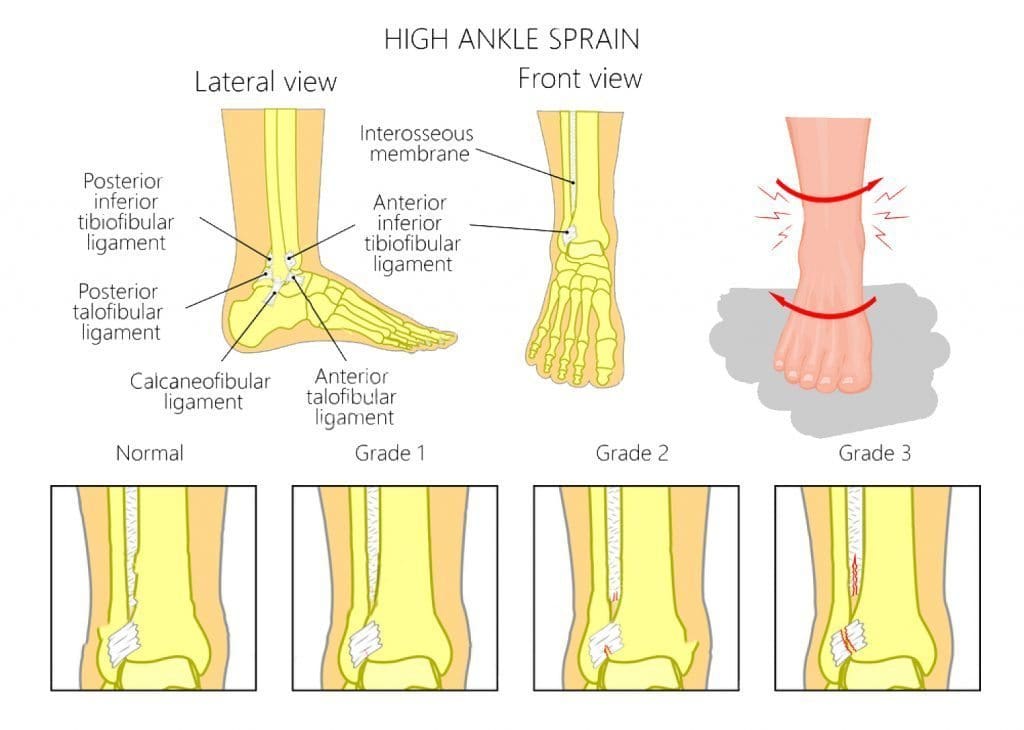
I looked up the word syndesmosis and the Latin translation is “(New Latin, from Greek sundesmos) bond, ligament, from sundein, meaning to bind together”. As sports injury professionals, we know syndesmosis to be the joint articulation between the tibia and the fibula bones around the ankle. These two bones are �bound’ together with very firm and strong ligaments.
Syndesmosis comes to mind after I saw a girl sprain a syndesmosis at the Archaeological Museum in Istanbul today. This poor girl was preoccupied by the hundreds of cats and kittens running all over the place and did not see the uneven cobblestones on which she placed her foot. At the same time, she turned to change direction. This is a common mechanism of injury for a syndesmosis – a forced dorsiflexion and rotation on a fixed foot.
Rehab Masterclass Issue 140 Of Sports Injury Bulletin
Of all the ankle injuries, injury to the syndesmosis is the biggest pest to sports physios and the like. And unlike simple garden variety ankle sprains that heal quickly, the syndesmosis takes a LONG time to heal properly. If you deal with athletes that are susceptible to syndesmosis sprains, I’m sure you will agree that these are harder injuries to manage because of the severe consequences if done badly.
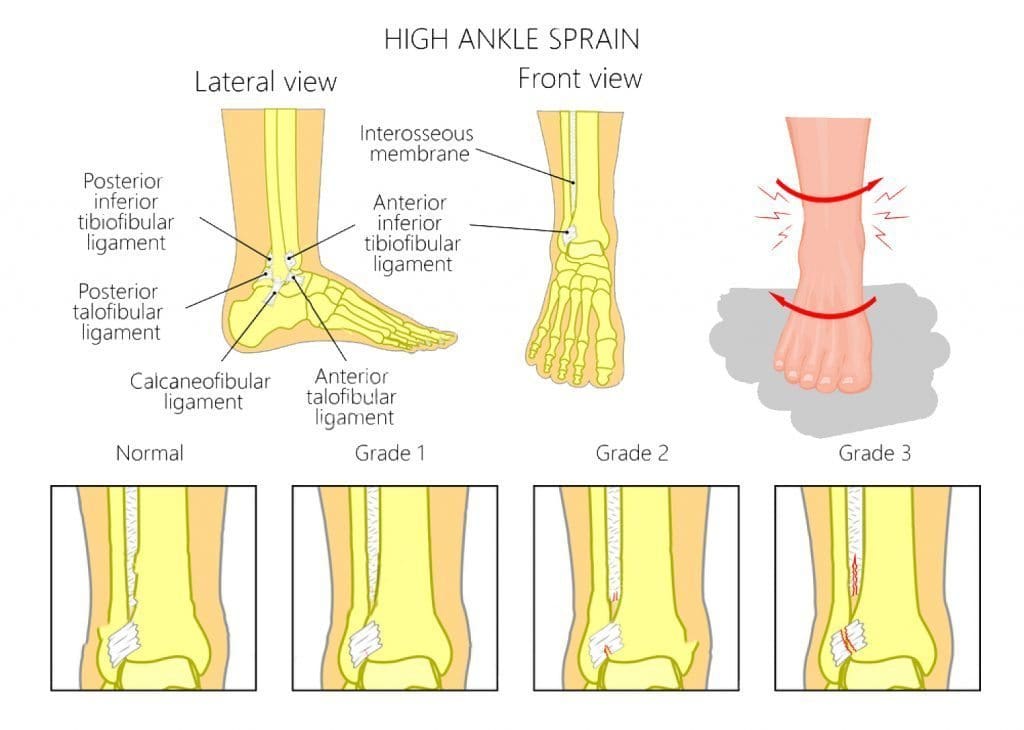
I go into a fair bit of detail in my Sports Injury Bulletin piece about syndesmosis injuries, detailing how they happen, how to identify them and then manage them. What I would like to highlight here are the implications of mismanaging a syndesmosis sprain.
In the current issue of The Journal of Sports and Physical Therapy, a group of Japanese researchers discovered that individuals who had chronic ankle instability (CAI) had a distal fibula that was positioned more lateral compared with healthy individuals with no CAI. In effect, those who had suffered serious syndesmosis injuries in the past and ended up with a wider distance between the fibula and the tibia, suffered more ongoing ankle pain than those without a tibfib separation.
Research shows that even a 1mm displacement of the talus within the mortise (due to a wider placed fibula) can reduce the contact area in the talocrural joint by 42% (Ramsey and Hamilton 1976). Mismanaged syndesmosis injuries, resulting in an excessive amount of opening, can lead to early onset arthritic changes and chronic ankle instability. The talus bone bounces around in the now wider tibfib articulation.
A Widening Of The Fibula Is Due To One Of The Following:
Poor initial management, whereby the athlete is allowed to weight bear too early and this weight bearing forces the fibula away from the tibia as the syndesmosis ligaments are trying to heal.
The degree of damage is so severe that proper tightening of these ligaments is not possible without surgical intervention such as a screw or similar being placed between the two bones to �force’ them together.
The key for a sports injury practitioner, is to properly identify a regular ankle sprain from a more serious syndesmosis injury. If you get this part wrong and allow the athlete to get back to weight bearing too early, then expect some complaints about a chronically painful ankle some time down the track.

Call Today!
Kobayashi et al (2014). �Fibular malalignment in individuals with chronic ankle instability.’ JOPST. 44(11); pp 841-910.
Ramsey and Hamilton (1976). J Bone and J Surgery Am. 58(3); 356-357.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Fitness, Health, Wellness
Yoga can be an effective way to prevent and ease aches and pains—but it can also cause them if you’re not careful. The key is proper alignment. Go from “ow” to “om” in seconds by making simple alignment tweaks to common poses. In this video, Yoga With Kirby founder Kirby Koo shows you quick fixes to take pressure off your knees, wrists, and neck. These basic principles can be applied throughout your practice to help prevent pain before it starts.
Warrior II
Once you’re set up in Warrior II, pay attention to the position of your front knee. Is it sticking out beyond your ankle? Is it collapsing inward? Pull your knee back into place, so it’s stacked directly above your ankle, and tracking in the same direction as the toes of your front foot. This protects the ligaments in your knee and prevents knee pain.
Related Content: Try This 15-Minute Yoga Flow for Stress Relief
Plank
Plank is a great core stabilizing exercise if you have proper alignment. But if your belly and hips sag in this pose, then your wrists are probably taking on the brunt of your body weight. In plank, engage your core muscles by imagining a zipper running up from your pubic bone to your belly button. This should help raise your hips so your body forms a continuous line from the top of your head to your heels, a more stable position that will help distribute your body weight more evenly and ease the pressure in the wrists.
Cow Pose
Cow pose can feel super satisfying, but it’s easy to go overboard and strain your neck while you’re enjoying the gentle backbend. When you’re in cow pose, it’s important to remember not to tip your head too far back, shortening the back of the neck. You’ll get a lot more out of the pose (and avoid neck strain) if you imagine your neck as an extension of the gentle curve of the spine. Lift your gaze only as far as you can without compromising the curve in your spine and the length in the back of your neck. The same concept can apply for Upward-Facing Dog, too!

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Natural Health, Wellness
The mixture of pollutants in many U.S. streams are more complicated and potentially more dangerous than previously thought, a new study suggests.
Researchers checked for 719 organic chemicals in water samples from 38 streams across the United States and found more than half of those chemicals in the different samples.
Every stream — even those in wild and uninhabited areas — had at least one of the chemicals and some had as many as 162, the study found. It was led by scientists from the U.S. Geological Survey and the Environmental Protection Agency.
The detected chemicals included: insecticides and herbicides, along with byproducts from their degradation; antibacterials such as triclosan; and medications such as antihistamines and the diabetes drug metformin.
Some of the chemicals were often detected together in streams. Further research is needed to determine the potential for complex interactions between these chemicals, to assess if they pose a threat to aquatic life, the food chain and human health, the researchers said.
The study was published April 12 in the journal Environmental Science & Technology.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Natural Health, Wellness
Your weight just might influence your risk of migraine headaches, a new review finds.
“Those with migraine and [their] doctors need to be aware that excessive weight and extreme weight loss are not good for [migraine sufferers], and that maintaining a healthy weight can decrease the risk of migraine,” said study corresponding author Dr. B. Lee Peterlin.
She is director of headache research at Johns Hopkins University School of Medicine in Baltimore.
“Healthy lifestyle choices in terms of weight management and diet and exercise are warranted,” she added.
Migraines affect about 12 percent of U.S. adults, according to background information from Johns Hopkins. These debilitating headaches are often accompanied by throbbing, nausea and sensitivity to light and sounds.
Peterlin’s team evaluated 12 previously published studies with nearly 300,000 people, a process known as a meta-analysis.
The investigators found that obese people were 27 percent more likely to have migraines than people who were at a normal weight.
And those who were underweight were 13 percent more likely to have migraines.
The researchers used the standard definitions of both obesity — a body mass index (BMI) of 30 or higher — and underweight, a BMI of less than 18.5. A person who is 5 feet 4 inches tall and weighs 175 pounds has a BMI of 30, while someone of the same height who weighs 105 has a BMI of 18.
In previous research, Peterlin’s team found that the link between obesity and migraines was greater for women and for those under the age of 55. This new study reaffirmed those findings.
The new review found that the link between obesity and migraines is a moderate one, Peterlin said. It’s similar to the link between migraines and ischemic heart disease, in which the heart doesn’t get enough blood, she added.
Peterlin said she can’t explain with certainty how body composition affects migraine risk. But, she speculated that fat tissue “is an endocrine organ and like other endocrine organs, such as the thyroid, too much and too little cause problems.”
The change in fat tissue that occurs with weight gain or extreme weight loss alters the function and production of several proteins and hormones, Peterlin explained, changing the inflammatory environment in the body. This could make a person more prone to a migraine or it could trigger a migraine, she said.
However, the study only found an association, and not a cause-and-effect relationship, between weight and migraine risk.
The review was published April 12 in the journal Neurology.
Would weight loss or gain help? It’s not certain, Peterlin said.
“Limited data in humans show that in both episodic and chronic [migraine sufferers] who are extremely obese and undergo bariatric surgery for other health reasons also have a reduction in headache frequency by over 50 percent,” she said. Aerobic exercise has also been shown to decrease headaches.
“What is not yet clear is if it is the weight loss per se or other factors related to exercise that result in the improvement,” Peterlin said.
One headache specialist who wasn’t involved with the study lauded the findings.
The new analysis is “a valuable addition to the growing body of literature on migraine and body mass index,” said Dawn Buse, director of behavioral medicine at the Montefiore Headache Center in New York City.
With her patients, Buse said, she has seen migraine frequency increase with weight gain. And she has also seen improvement in migraines after weight loss, she said.
Buse acknowledged that, while weight loss appears to help, losing weight can be challenging. Health care professionals should discuss with their patients the relationship with migraines, and help them by providing education and referrals for treatments that may help weight loss.
by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Anti Aging
You should be adding a magnesium supplement to your daily vitamin regimen in middle age to prevent fractures later, says a new study.
Bone fractures, which are often caused by osteoporosis, are one of the leading causes of disability in the elderly. Calcium and vitamin D are known to play a role in bone health, and while magnesium is a vital nutrient and an important component of bone, no studies have shown that supplements might have a beneficial effect on bone health.
Researchers at the Universities of Bristol and Eastern Finland followed 2,245 middle-aged men for 20 years. They found that men with lower blood levels of magnesium had an increased risk of fractures, particularly fractures of the hip.
Men who had higher blood levels of magnesium lowered their risk by 44 percent. None of the men who had very high magnesium levels suffered a fracture during the 20-year follow-up.
However, dietary magnesium intake was not found to be linked with fractures. Only supplements were shown to be beneficial.
“The findings do suggest that avoiding low serum concentrations of magnesium may be a promising though unproven strategy for risk prevention of fractures,” said Dr. Setor Kunutsor of the University of Bristol.
Low blood levels of magnesium are common among the middle-aged and elderly, since the mineral becomes harder for the body to absorb as it ages, but the majority of people have no symptoms. Since blood magnesium isn’t measured routinely in the hospital, those with low levels are usually not diagnosed. The researchers believe their findings could help trigger initiatives to include blood magnesium screening in routine blood panels, especially for the elderly.
Magnesium may also help solve another problem faced by seniors — getting a good night’s sleep. British researchers found that magnesium helps cells keep track of the natural cycles of day and night.
Other studies show that magnesium provides a wide range of health benefits, including boosting the immune system and lowering the risk of heart attacks. Studies have also shown that people who have migraines tend to have lower levels of magnesium than those who are headache free.