by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | UTEP (Local) RSS
SAN ANTONIO, Texas– The UTEP men’s golf team ended the opening day of the Lone Star Invitational in a tie for second after firing a season-low 19-under 557 (277-280). The Miners share the spot with Oklahoma, who shot rounds of 278 and 279, while Illinois leads the field with 27-under 549 (272-277).
Lone Star host UTSA trails the Miners and Sooners by two strokes with 17-under 559 (279-280). The third and final round at the Briggs Ranch Golf Course (par 72/7247 yards) in San Antonio, Texas will begin in a shotgun start at 7:30 a.m. MT.
Senior Frederik Dreier led the Miner charge, firing 8-under 136 (66-70) for sixth place and one stroke out of being apart of a three-way tie for third. Not far behind, teammate Charles Corner has a share of eighth place after a 5-under 139 (71-68) day one showing. Andreas Sorensen sits one stroke away from Corner in a tie for 12th, tallying 4-under 140 (69-71).
Aaron Terrazas fired 2-under 142 (71-71) for a share of 21st while Prescott Mann rounded out the Miners’ field with 8-over 152 (76-76) to end the two rounds in a tie for 70th.
The Lone Star Invitational will conclude tomorrow, beginning with a shotgun start at 7:30 a.m. MT. Live stats will be available via golfstat.com.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | UTEP (Local) RSS
Photo courtesy UTEP Athletics
Staff Report March 21, 2017 128 Views
SAN ANTONIO, Texas- Behind strong play, led by senior Frederik Dreier, sophomore Aaron Terrazas and junior Charles Corner, the UTEP men’s golf team finished the Lone Star Invitational in fourth place.
The Miners, who were in a tie for second place after two rounds, shot a season-low 22-under 842 (277-280-285). Oklahoma ran away with the Lone Star title after setting the tournament’s team scoring record with a 40-under 824 (278-279-267).
Dreier and Terrazas stayed at the top of the Miners’ card and were part of a five-way tie for sixth place with 7-under 209. Dreier shot rounds of 66-70-73 and recorded 37 pars while Terrazas fired 71-71-67, including 15 birdies.
Corner, who tallied 14 birdies, was one stroke behind his teammates with 6-under 210 (71-68-71), finishing in a share of 11th. Andreas Sorensen ended the invite in a tie for 37th with a even-par 216 (69-71-76) showing.
Prescott Mann finished out the Miners’ scorecard in 68th after shooting 10-over 226 (76-76-74). Due to injury, Nicklas Pihl withdrew from the tournament.
The Miners will play in their last event of the regular season April 8-9 at the Western Intercollegiate in Santa Cruz, Calif. Live stats will be available via golfstat.com.
Check Also
ALBUQUERQUE, N.M.- The UTEP women’s tennis team fell short in getting the much-needed doubles point and …
by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | UTEP (Local) RSS
The UTEP women’s tennis team will travel to Albuquerque, N.M., to meet the New Mexico Lobos in a dual match on Friday. First serve at the McKinnon Family Tennis Center is set for 11 a.m.
The Miners are coming off last week’s home loss to Iowa State. The team is 4-10 on the season with two road wins. The Lobos are 1-11 this season and will be meeting with the Miners after a 4-3 home loss to Northern Arizona.
New Mexico beat Wisconsin, 5-2, on Feb. 18 in Salt Lake City.
Representing UTEP will be Milou Pietersz, Lois Wagenvoort, Daphne Visscher, Raven Bennett and Maria Paula Medina.
The Lobos feature senior Ludivine Burguiere, who plays the No. 1 spot in singles as well as the duo of Rachana Bhat and Dominique Dulski at the No. 1 doubles position.
Burguiere has tallied a 8-10 overall record, while Bhat and Dulski have racked up a 1-3 mark together.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | UTEP (Local) RSS
After its series win against Middle Tennessee, the UTEP softball team will host Conference USA West Division foe Southern Miss March 25-26. First pitch is set for 3 p.m. to begin Saturday’s doubleheader, while Sunday’s contest will start at 11 a.m. at the Helen of Troy Softball Complex.
The Miners (7-19, 2-4 C-USA), after a slow start in league action, rebounded last weekend as they won two of three games against Middle Tennessee at the Helen of Troy Softball Complex. It’s the second season in a row in which the Miners will host back-to-back conference weekends. Last season, UTEP split its six contests, losing three to UAB, but coming back strong with a sweep against North Texas to clinch a spot in the C-USA Tournament.
“It’s always nice to be at home no matter if it’s the beginning, middle or end of the season, we just feel more comfortable and confident playing at home,” fourth-year head coach Tobin Echo-Hawk said.
UTEP is 19-8 in C-USA contests at the Helen of Troy Softball Complex since 2015 and 24-15 since 2014.
The Golden Eagles (14-14, 1-5 C-USA) halted a four-game losing streak after edging South Alabama, 2-1, on March 22 in Hattiesburg. The Golden Eagles have lost six of the last nine games, which includes being swept against LA Tech March 18-19 and losing two of three at UAB March 11-12.
It’s a big series for both squads as each stand in the C-USA West Division. Last season, Southern Miss finished 14-10 to earn the no. 3 seed in the C-USA Tournament. UTEP was a no. 6 seed with a 13-11 league record.
“You know, it’s a big series for a lot of different reasons,” Echo-Hawk said. “If you look at our record against them last season, they kind of had our number and I think that’s a motivational factor. It’s also one of those series where the further you get into conference play, it’s nice to have those wins against teams in our division, and actually matter as far as seeding goes [for the C-USA Tournament]. We’re very similar with our records, so it’s important to win at least two of the three to win the weekend.”
Last season the two programs met four times in five days. Southern Miss won three contests in Hattiesburg, 3-0, 3-0 and 6-4 May 7-8. The two squads met again in the C-USA Tournament in Denton on May 11, with the Golden Eagles topping the Miners, 10-4.
UTEP will continue its home stretch when I-10 rival NM State heads to the Sun City for a doubleheader onMarch 28, starting at 5 p.m.
SCOUTING SOUTHERN MISS
The Golden Eagles are heading to the Helen of Troy this weekend with an overall record of 14-14. Southern Miss has tallied one conference win, which came against UAB, 10-4, on March 12. Last weekend they fell short all three games of the series to LA Tech, with game two going into 14 innings and finally ending at a 4-2 loss.
As a team, the Golden Eagles are hitting a total of .239 to rank 10th in Conference USA. Senior Lauren Holifield leading the line up with a .291 average, five home runs and 14 RBI. The pitching staff has totaled an ERA of 2.41 to rank fourth in C-USA. Junior Kim Crowson is producing the most success, as she has fashioned a 1.50 ERA to rank third in C-USA.
Crowson leads the staff in wins (six) and strikeouts (40) – ranks no. 12 in Ks in C-USA. Southern Miss ranks last in C-USA in runs (92), slugging (.328), home runs (12) and total bases (238). The Southern Miss pitching staff, however, ranks third in opposing batting average (.240) and fifth in least hits allowed (185).
ALL-TIME SERIES VS. SOUTHERN MISS
UTEP is 15-17-1 all-time versus Southern Miss. The Golden Eagles have won the last four contests, which included a sweep in Hattiesburg last season and a second-round victory at the Conference USA Tournament on May 11.
UTEP and Southern Miss have spit the last six contests at the Helen of Troy Softball Complex. The Golden Eagles took two of three contests in 2014, while the Miners returned the favor and won the series 2-1 in 2015. Southern Miss is 7-12 all-time at the Helen of Troy Softball Complex.
LAST WEEK
UTEP defeated Middle Tennessee twice during the March 18-19 series. The Miners won game one, 7-6, behind Kaitlin Ryder’s three-run home run and Erika Harrawood’s solid performance in the circle. Harrawood threw 6.1 innings, walked none, and struck out four batters. UTEP got tripped up in game two, but came back to win the series with a 10-7 win in weekend finale.
Middle Tennessee went up 5-0 in the first, but UTEP chipped away and scored 10 unanswered run the first four frames.
Courtney Clayton, Pamala Baber and Cortney Smith each recorded a pair of RBI in the series clinching victory. After Middle Tennessee went up 5-0 in the first frame, Devyn Cretz (4.0 IP) and Kaitlin Fifield (2.2 IP) kept the Blue Raiders’ bats in check, allowing only two runs on seven hits the next six innings. Cretz earned the win, while Fifield recorded her second save of the season.
COMEBACK KIDS
UTEP rallied from a 5-0 deficit on Sunday to defeat Middle Tennessee 10-7. The March 19 rally tied as the second-biggest come-from-behind victory in a conference game in program history, while it’s tied for fifth largest comeback in any contest in school history. UTEP rallied from 5-0 down to Colorado State after the top first to win 9-8 on Feb. 28, 2015 in Tucson, Ariz.
Earlier that season, the Miners scored eight runs in the top seventh to defeat Portland State, 8-5, in Las Vegas, Nev. on Feb. 13, 2015. The largest conference rally came against Southern Miss on March 10, 2012 in El Paso. The Miners were down 7-0 heading to the bottom first and rallied to win 13-12.
MOST RUNS, RBI & HITS COMBINED FOR IN A C-USA GAME
On March 19 UTEP and Middle Tennessee combined for the most runs (17), RBI (17) and hits (25) during a Conference USA only game up to this point of the season. The Miners banged out 13 hits during the 10-7 victory. The Miner and Blue Raiders also combined for the most stolen bases (five) during a conference only game.
GAME 3 RUNS & HITS VS. MT
UTEP clinched the series against Middle Tennessee with a 10-7 victory on March 19. The Miners tied their season highs in hits (13) and runs (10) during the victory. UTEP defeated Siena 10-2 (5) on Feb. 24, while connecting on 13 hits at New Mexico during a 7-4 triumph on March 8.
MOST RUNS/HITS DURING ECHO-HAWK ERA
During the Tobin Echo-Hawk era, the Miners’ single-game high is 17 hits on Feb. 11, 2016 against Incarnate Word, while the most runs scored was a 16-run output against Mount St. Mary’s on March 5, 2016. The hits (17) are ranked tied eighth in program history, while the runs scored is tied ninth.
OWNING MT
With UTEP’s 2-1 series win against Middle Tennessee on March 19, the Miners improved to 10-2 against the Blue Raiders all-time. UTEP is also 8-1 all-time versus MT at the Helen of Troy Softball Complex. The Miners, in 12 games played against the Blue Raiders, are hitting .394 (137-348) with 18 long balls. UTEP has outscored MT 88-51 during that span.
BAT WOMEN
After hitting .226 the first nine games of the season, the UTEP bats have caught fire, hitting .323 (153-473) during the last 17 contests. The Miners are currently ranked fifth in Conference USA with a .292 overall batting average (204-699). Marshall leads the league with a .317 batting average, while FIU (.312), UTSA (.303) and LA Tech (.299) round out the list. UTEP’s 204 hits rank sixth. FIU leads the league with 263 knocks.
DIGGING OUT TRIPLES
UTEP tallied its sixth triple of 2017 in game two against Middle Tennessee. UTEP is ranked tied fourth with Charlotte in Conference USA with six three-baggers. LA Tech leads the pack with 10, while UTSA and Marshall ranks tied second with seven apiece.
TOUGH OUT
UTEP has struck out 103 times in 699 at bats to rank ninth in Conference USA. Three Miners have kept their Ks low as Lindsey Sokoloski has whiffed only once in 75 at bats to rank first in C-USA and eighth nationally in toughest to strikeout. Courtney Clayton has struck out twice in 89 at bats to rank second in C-USA and 48th nationally.
Taylor Sargent has left the plate looking for swinging five times in 73 at bats to rank fifth in C-USA and tied no. 140 in the nation.
ROUGH RYDER
Kaitlin Ryder came up with a big weekend, producing six RBI and hitting .444 (4-9) during the series win against Middle Tennessee. During UTEP’s game one victory over the Blue Raiders, Ryder connected on her second home run of the season, a three-run shot over left in the second inning that put the Miners up 4-0.
Ryder is hitting .409 (9-22) with seven RBI the last seven contests. Overall, the junior is hitting .304 with two dingers and 13 RBI.
GAME SAVER
Kaitlin Fifield recorded her second save of 2017 after recording one against Middle Tennessee on March 19 in 2.2 innings of work. Fifield entered the contest with bases loaded and one out in the fifth with the Miners leading 10-5. The Blue Raiders only crossed the dish twice to get within three runs while Fifield only allowed one hit and walked no batters the next 2.0 innings.
Fifield recorded her first save of the season against Utah State on Feb. 24. Fifield is ranked tied first with five other players in Conference USA and tied no. 23 nationally. Fifield has four saves in her career to rank tied second on the program’s all-time saves’ list with four other players.
by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | UTEP (Local) RSS
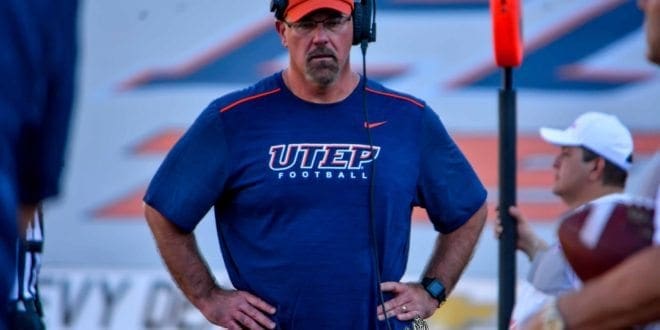
Quadraiz Wadley rushed nine times for 72 yards and two touchdowns to steal the show in the first spring scrimmage for the UTEP football team on a windy Friday morning at the Sun Bowl.
UTEP’s rushing attack accounted for six of the seven touchdowns on the day, with Kavika Johnson (17-yard TD, 5-yard TD), Walter Dawn (10-yard TD) and Terry Juniel (13-yard TD) also finding paydirt. The Miners averaged better than 5.5 yards per carry (25-141), aided by five gains of at least 10 yards.
Strong wind gusts made it tough to accomplish much through the air. Ryan Metz (4-10, 36 yards, INT), Zach Greenlee (2-9, 33 yards) and Mark Torrez (1-2, 20 yards, TD) combined to go 7-21 for 89 yards with one touchdown and one interception. The seven completions went to seven different receivers, with Richie Rodriguez hauling in a 20-yard toss from Torrez for the lone score through the air.
There were also some bright spots for the Miner defense, which produced two sacks (Dylan Parsee and Dedrick Simpson) and an interception (Lawrence Montegut). Montegut and Johnny Jones were also credited with a pass break-up.
Nik Needham finished with a team-high four tackles while Dante Lovilette (three), Justin Rogers (two), Stephen Forester (two) also had multiple stops.
But the day belonged to Wadley. After being halted for three yards on his first rush, the rising sophomore was practically unstoppable the rest of the way. Wadley scampered for at least five yards on each of his final eight rushes, including bursts of 12 and 15 yards. He also had both of his touchdowns (eight yards, five yards) in the stretch.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | UTEP (Local) RSS
ALBUQUERQUE, N.M.- The UTEP women’s tennis team fell short in getting the much-needed doubles point and ultimately fell 4-0 to New Mexico at the Estes Tennis Center in Albuquerque, N.M., on Friday. High winds moved the match indoors.
On court one in doubles play, Milou Pietersz and Lois Wagenvoort were unable to close against the Lobos’ Rachana Bhat and Dominique Dulski, falling 6-2 to give the Lobos the point and lead due to a forfeit on court three due to injury. Daphne Visscher and Raven Bennett had a 3-2 lead over Emily Oliver and Diana Wong on court two before their match was called.
In singles action, Pietersz fell to Burguiere 6-0, 6-3 to give the Lobos the set and match.
The Miners will look to get healthy in the next two weeks and will be back in action to defend their home court in the first and only Conference USA match April 9 against UTSA.
First serve against the Roadrunners is 11 a.m. at the El Paso Tennis and Swim Club.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | UTEP (Local) RSS
The UTEP track and field team will open the outdoor campaign at the first of three meets at Kidd Field this Saturday.
UTEP will host the UTEP Invitational (April 22) and the Conference-USA Championships (May 11-14). The Miners will compete at the Texas Relays (March 28-April1), Mr. SAC Distance/UCLA Invitational (April 13-15), the Brutus Hamilton Open & Challenge (28-29).
The women’s team will head into the outdoor season after celebrating it’s third consecutive C-USA championship title. The Miners will look to start the outdoor season on the right foot after a fourth-place finish last year.
On the women’s side, All-American Tobi Amusan returns to her prime event in the 100m hurdles. Amusan competed at the 2016 Rio Summer Olympics placing 11th in the world. The sophomore will take the track at 2:35 p.m. MT.
Florence Uwakwe will run the 400m set for a 4:30 p.m. start. The senior holds the school second fastest time in that event.
Michael Saruni will compete in the 400m set to start at 4:55 p.m. Saruni won gold at the C-USA championships in both the 800m and the mile run. The freshman was named C-USA athlete of the week during the indoor season and was named an All-American during the indoor season.
Live results will be available at www.spato.us and follow UTEPTrack on twitter.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | UTEP (Local) RSS
UTEP sophomore hurdler Tobi Amusan clocked the fastest 100m hurdle time (12.63) in the world for 2017 on Saturday afternoon at Kidd Field in the UTEP Springtime.
Amusan exploded out of the blocks and dashed to a first-place finish, setting a school record in the process. The previous standard was held by Kim Turner (12.95, 1983) and had stood for 34 years.
Getting the day started was Fayon Gonzales in the hammer throw. The senior notched a fourth-place finish with a throw of 50.16m (164-7), followed by Adebola Akomolafe (157-1.25) in fifth place. Gonzales also captured silver in the javelin with a toss of 39.37m (129-2.25).
The Miners swept the 1,500m run with Linda Cheruiyot (4:31.81), Winny Koech (4:34.41) and Gladys Jerotich (4:51.60). Melanie Crittenden notched fourth place in the high jump with a mark of 1.53m (5-0.25).
Senior Ada Benjamin clocked the clocked the fourth-fastest time (53.16) in the nation in the 400m. She also took silver in the 200m (24.02). Lucia Mokrasova tied for second (14.00) in the 100m hurdles and secured a fourth-place finish in the 200m with a time of 24.52.
Lilian Koech notched the seventh-fastest time nationally (2:08.98) in the 800m. Samantha Hall took home gold in the discus by throwing for 52.61m (172-7.50). Israel Ramsay (5.88m, 19-3.50) and Tyler Ragin (5.79m, 19-0) took second and fourth overall in the long jump.
On the men’s side, freshman Karol Koncos won gold in the hammer throw by tossing for 61.84m (202-11), followed by Kevin Rincon with a toss of 49.70m (163-1) to finish third overall. Rincon returned in the javelin to take silver, launching for 59.31m (194-7.25).
Austin Ondijo took second in the high jump leaping over 1.97m (6-5.50). The 1,500m run featured the most Miners in one event. Cosmas Boit (3:49.46) took home silver, Antony Kosgei (3:56.28) finished fifth, Daniel Cheruiyot (3:57.44) finished sixth and Evans Kiprono (3:59.90) finished seventh overall.
In the 200m Asa Guevara took the number one spot running 21.06, followed by James Bias (21.50) to finish fourth overall.
UTEP has a short rest before returning to the track, this time in Austin, Texas, for the Texas Relays March 28-April 1. Be sure to follow @UTEPTrack on Twitter for live updates.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | UTEP (Local) RSS
Kaitlin Ryder and Erika Harrawood were game one heroes for a second consecutive week as UTEP took care of Southern Miss, 12-2 (5) in the first game of a Saturday doubleheader at the Helen of Troy Softball Complex.
Ryder registered a career-high five RBI, while Harrawood (3-7) chalked up her first complete-game victory in her career and second triumph in her hometown. Harrawood won her first game in El Paso last Saturday against Middle Tennessee.
“[Harrawood] has done a tremendous job this year,” fourth-year head coach Tobin Echo-Hawk said. “I know we haven’t necessarily got the wins that she deserved, but all year she’s just kept improving. She’s been solid and just her presence on the mound is exactly want you want in a pitcher. She’s calm, collective and knows what she has to do. It’s not flashy, but she does her job.”
The Orange and Blue also tallied season highs in runs (12) and hits (15).
“We had a lot of clutch hits from a lot of different people,” Echo-Hawk said. “Even that pinch hit from Macey Brown was big; she’s been kind of clutch for us lately. It’s nice to know that they can handle that pressure.”
The Golden Eagles (15-15, 2-6 Conference USA) rebounded to win game two, 6-2. But the Miners (8-20, 3-5 C-USA) still hold a one-game lead in the C-USA West Division.
The series finale is Sunday with the first pitch slated for 11 a.m.
UTEP 12, Southern Miss 2 (5)
The Miners jumped on the Golden Eagles in the second inning, crossing the dish four times. Courtney Clayton put her squad on the board first with a RBI single to left. Cortney Smith scored run after she singled to left with one out. Ryder, with bases juiced, was hit by a pitch to earn a RBI the hard way, plating Mallorie Cross, who walked to reach base. Kiki Pepi put the Miners up 4-0 with a two-run single through the right side that scored Ariel Blair and Clayton.
Southern Miss answered with a pair of runs in the third, but Harrawood kept its bats in check the rest of the way.
Harrawood started strong, as she retired eight of the first nine batters. The tenth batter, Lauren Holifield, put her team on the board with a two-run single. Harrawood only allowed three hits the rest of the way. Harrawood threw all 5.0 frames, allowing only five hits and striking out three.
More run support came Harrawood’s way as the Miners tacked on five more runs in the third, led by two RBI from Ryder and one each from Brown, Cross and Pepi. Brown delivered her fourth RBI in her third pinch-hit situation (3-for-3) the last few weeks.
With UTEP up 9-2 in the fourth, Cross singled in Smith for the run-rule to come into effect. Ryder then punched in a few insurance runs on a double to left center, paving the way for Blair and Lindsey Sokoloski to cross the dish.
Chase Nelson led off the fifth by reaching on an error and Samantha Reynolds reached on an infield single, but Harrawood struck out Arille Pollock on a full-count pitch for the first out. Holifield reached on a fielder’s choice as Nelson rounded second only to be called out on an unassisted out by third baseman Pepi. Tori Dew ended the contest by flying out to center.
Clayton went 2-for-3 for her 10th multi-hit game of the season and no. 52 for her career. Three Miners tied their career highs in hits as Ryder went 3-for-3, Pepi notched a 3-for-4 outing and tallied three RBI, and Smith was a perfect 3-for-3 while setting her career high with three runs. Cross finished with a career high in RBI (two) and runs scored (two).
UTEP 2, Southern Miss 6
UTEP’s nemesis Samantha Robles pitched a complete game, while defeating the Miners for the fourth time in four starts. Robles tallied three wins against UTEP in 2016 (two in the regular season and one in the C-USA Tournament), while earning a save in game one of the regular season series in Hattiesburg.
The Miners took an early 1-0 advantage on Robles in the second on a Cross sacrifice fly to left that plated Hope Moreno.
But the Golden Eagles scored a trio of runs the next frame as Eva Scott led off with a walk and Nelson singled to third, advancing Scott to third base. Both runners would steal bases while Scott’s base snag tied the game 1-1. Holifield gave Southern Miss the go-ahead lead on a sac-fly to center and Dew reached first on an error by Clayton, also paving the way for Ciarra Cherry to score, who walked earlier in the inning.
UTEP got within a run in the third on a Pepi RBI double that scored Ryder. But the Golden Eagles put up two runs in the sixth and another run in the seventh to seal the victory.
Devyn Cretz (5-6) started the game, throwing 3.0 frames with two earned runs, while Kaitlin Fifield hurled 4.0 innings with one earned run.
Clayton, Ryder, Pepi, Moreno, Smith and Sokoloski registered all six hits for the Miners.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Fitness, Health News El Paso, Sleep Hygiene, UTEP (Local) RSS
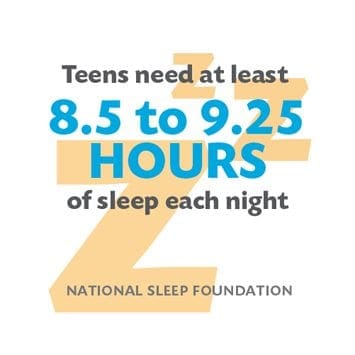
Getting more sleep will likely help middle and high school students in Nevada and across the country do better in school, be healthier and make healthier choices, according to a study from the Centers for Disease Control and Prevention.
Epidemiologist Anne Wheaton with the CDC says only one in eight students in Nevada gets the recommended amount of sleep, between eight-and-a-half and nine-and-a-half hours per night. She says sleep deprivation is linked to drinking alcohol, smoking tobacco and using drugs as well as poor academic performance.
�If you haven�t had enough sleep and you�re sitting in the first period of school, you have a harder time paying attention and your memory doesn�t work quite as well,� she says. �If you don�t get enough sleep.�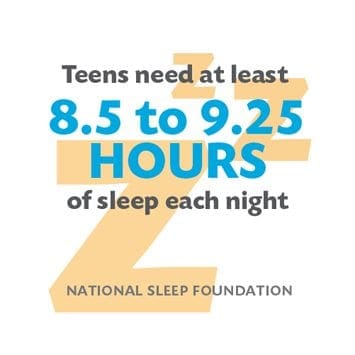
Wheaton says a major cause of the sleep problem is 87 percent of middle and high schools in Nevada start school before 8:30 a.m., which does not give students enough time to get the recommended amount of sleep. She says puberty delays sleep, which means teenagers need more time to get going in the morning because their bodies are keeping them up later at night.
Wheaton points out the American Academy of Pediatrics issued a policy statement last year urging middle and high schools to modify start times to no earlier than 8:30 a.m. to aid students in getting sufficient sleep to improve their overall health.
�Not getting enough sleep tends to affect your appetite so you eat more, you�re more fatigued, so you�re less likely to exercise,� says Wheaton. �It can impact your blood sugar, so further down the road after years of not getting enough sleep, you�re more likely to develop diabetes for instance.�
There are other factors involved, but Wheaton says some school districts are resistant to later start times because they say it would increase costs for busing students. She says parents can also help their children practice good sleep habits by maintaining a consistent bedtime and rise time, including on weekends.