
by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Functional Medicine, Nutrition, Vitamins, Wellness
Mostly everyone takes their vitamins in any shape and form. It can be from the foods that we eat to the supplements and vitamins pills that we make throughout the day. We can get the boost of micronutrients in our bodies with vitamins and foods. It can help with our diets when we are trying to get a head start in our healthy lifestyle change through healthy, nutritious, whole foods. Without it, it can cause our bodies to react differently with ailments. For example, a person has a healthy lifestyle, but they are feeling out of place in their daily lives; it might be due to their low levels of the vitamins they are not taking. We will be taking a look at the micronutrition in vitamins and supplements in this two-part series for the body.
The Vitamins
Vitamins are essential for the body since we can�t produce them naturally. When we feel sluggish or horrible, it might be due to the low vitamin intake that we are missing to make us feel better. Here are some of the vitamins that can help your body if you feel a bit weak in life.
Vitamin A

Vitamin A is a fat-soluble compound that is an essential nutrient for the body. It is stored in the liver for later use and is transferred to the tissues when needed. Vitamin A helps maintain the integrity and function of all surface tissues and the eyes. Vitamin A has two forms which are retinol and retinyl esters and provitamin A carotenoids. Retinol and retinyl esters health benefits can help prevent macular degeneration to your eyes, and with the provitamin A carotenoids can have potent antioxidants to fight off free radicals in your body.
Deficiencies: Having a Vitamin A deficiency can lead to blindness in the eyes of some people. Anyone who has a deficiency in Vitamin A can have skin issues like hyperkeratosis and acne. Not only that, but it can increase any infections as well as have pregnancy complications for pregnant women.
Food Sources: Here are some of the foods that are very rich with vitamin A that are all carotenoid-rich in both animals and plants.
- Egg yolks
- Beef liver
- Cod liver oil
- Salmon
- Sweet potatoes
- Carrots
- Dandelion greens
- Cabbage
Vitamin B

All B vitamins are water-soluble, and your body can�t store them. They are used to reduce fatigue and boost your mood. There are 8 B vitamins are vital and have many essential functions for maintaining good health.
- B1 (thiamine): Thiamine helps our bodies metabolism by helping convert nutrients into energy. Some food sources include pork, sunflower seeds, and wheat germ.
- B2 (riboflavin): Riboflavin converts food into energy and acts as an antioxidant in the body. Some of the food sources that are high in riboflavin are organ meats, beef, and mushrooms.
- B3 (niacin): Niacin plays a role in cellular signaling, metabolism and DNA productions, as well as repairs it as well. Some food sources include chicken, tuna, and lentils.
- B5 (pantothenic acid): Like other B vitamins, pantothenic acid helps our bodies obtain energy from the food we eat. It also involves hormone and cholesterol production. Some food sources include liver, fish, yogurt, and avocado.
- B6 (pyridoxine): Pyridoxine helps produces red blood cells in the body. It helps create amino acid metabolism and neurotransmitters for the body. Foods that are highly rich with this vitamin are chickpeas, salmon, and potatoes.
- B7 (biotin): Biotin is highly essential for carbohydrate and fat metabolism and can regulate gene expression in the body. The best food sources that contain biotin are yeast, eggs, salmon, cheese, and liver.
- B9 (folate): Our bodies need folate for cell growth, amino acid metabolism, the formation of red and white blood cells as well as proper cell division. Folate can be found in foods like leafy greens, liver, beans and in supplements like folic acid.
- B12 (cobalamin): One of the best- known of all the B vitamins, B12 is vital for neurological function, DNA production, and red blood cell count. It can be found naturally in animal food sources like meats, eggs, seafood, and dairy.
Deficiencies: Even though taking the B vitamins are essential, there are side effects to taking a high dose of the vitamin, especially B3 and B6. Some of the side effects include vomiting, high blood sugar levels, skin lesions, nerve damage, and even liver damage.
Vitamin C

Vitamin C is one of the most essential vitamins since it can�t be produced by the body. It has so many roles and has been linked to many impressive health benefits. It can help boost antioxidant levels, reduce high blood pressure, and heart disease risk. It can protect your body against any gout attacks and reduce your risk of dementia while improving your iron absorption and boosting your immunity.
Deficiencies: When you don�t take enough vitamin C, it can raise up your blood sugar. Without it, you can develop scurvy if you don�t have enough of vitamin C in your system. You can get really sick, and your immune system will be shot if you don�t take vitamin C.
Food Sources: The most common way to get vitamin C in your body is through citrus fruit. There are lots of foods that contain vitamin C and are very delicious.
- Red and green peppers
- Oranges and orange juice
- Kiwi
- Guava
- Broccoli
- Strawberries
- Brussel sprouts
- Tomato juice
- Cantaloupe
Vitamin D3

Also known as the sunshine vitamin, vitamin D3 is essential for maintaining healthy bones and teeth. It can support the immune system, brain, and nervous system by keeping it healthy. It will even regulate insulin levels and help managing diabetes. However, vitamin D3 can be synthesized to our body whenever sunlight hits our skin.
Deficiencies: Even though the body can create vitamin D, there many reasons that vitamin D deficiency can occur. If a person has a darker skin color and uses sunscreen to reduce the absorption of UVB (ultraviolet radiation B) rays from the sun. They can stop the production of vitamin D. Some of the symptoms of vitamin D deficiency include getting sick more, fatigue, muscle pain, and depression. And if it continues for long periods, it can lead to obesity, diabetes, hypertension, chronic fatigue syndrome, fibromyalgia, and osteoporosis, just to name a few.
Food Sources: There are a few foods that contain vitamin D naturally. And for vitamin D3 it is mostly animal produced.
- Salmon
- Sardines
- Egg yolk
- Shrimp
- Milk (fortified)
- Cereal (fortified)
- Yogurt (fortified)
Vitamin E

Vitamin E is one of the most essential nutrients that is available as a dietary supplement and can occur naturally in foods. It is an antioxidant that can help protect your cells damage and is fat-soluble. Researchers have investigated that vitamin E can be used as a treatment for various degenerative diseases, including high blood pressure, heart disease, and cancer. It is a rare case for a vitamin E deficiency; however, it is a rare condition that is being researched.
Since Vitamin E is the most common nutrient found in most foods, here are some of the foods, including cooking oils that are exceptional.
- Wheat Germ Oil
- Sunflower seeds
- Almonds
- Hazelnut Oil
- Goose meat
- Peanuts
- Mango
Conclusion
So with these vitamins, it can help your body feel so much better in the long run. Without them, our bodies will have various health problems that can hurt us in the long haul. When we take these vitamins, our bodies began to heal properly, and we can see that our moods are a bit better. We can have normal functions without the vitamins because we eat the food that contains them, but when we need that extra boost of energy, vitamins are the way to go.
Cites:
Basavaraj, K H, et al. �Diet in Dermatology: Present Perspectives.� Indian Journal of Dermatology, Medknow Publications, 2010, www.ncbi.nlm.nih.gov/pmc/articles/PMC2965901/.
Chiu, Zelia K, et al. �Patterns of Vitamin D Levels and Exposures in Active and Inactive Noninfectious Uveitis�Patients.� Ophthalmology, U.S. National Library of Medicine, 11 July 2019, www.ncbi.nlm.nih.gov/pubmed/31519386.
Choi, Hyon K, et al. �Vitamin C Intake and the Risk of Gout in Men: a Prospective Study.� Archives of Internal Medicine, U.S. National Library of Medicine, 9 Mar. 2009, www.ncbi.nlm.nih.gov/pubmed/19273781.
Ettarh, R R, et al. �Vitamin C Lowers Blood Pressure and Alters Vascular Responsiveness in Salt-Induced Hypertension.� Canadian Journal of Physiology and Pharmacology, U.S. National Library of Medicine, Dec. 2002, www.ncbi.nlm.nih.gov/pubmed/12564647.
Institute of Medicine (US) Panel on Micronutrients, Unknown. �Vitamin A.� Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc., U.S. National Library of Medicine, 1 Jan. 1970, www.ncbi.nlm.nih.gov/books/NBK222318/.
Kubala, Jillian. �Vitamin A: Benefits, Deficiency, Toxicity and More.� Healthline, 4 Oct. 2018, www.healthline.com/nutrition/vitamin-a.
Martel, Julianna L. �Vitamin B1 (Thiamine).� StatPearls [Internet]., U.S. National Library of Medicine, 14 Aug. 2019, www.ncbi.nlm.nih.gov/books/NBK482360/.
Megan Ware, RDN. �Vitamin D: Health Benefits, Facts, and Research.� Medical News Today, MediLexicon International, 13 Nov. 2017, www.medicalnewstoday.com/articles/161618.php.
Meyer-Ficca, Mirella, and James B Kirkland. �Niacin.� Advances in Nutrition (Bethesda, Md.), American Society for Nutrition, 16 May 2016, www.ncbi.nlm.nih.gov/pmc/articles/PMC4863271/.
N/A, Unknown. �Office of Dietary Supplements – Vitamin E.� NIH Office of Dietary Supplements, U.S. Department of Health and Human Services, 0AD, ods.od.nih.gov/factsheets/VitaminE-HealthProfessional/.
O’Leary, Fiona, and Samir Samman. �Vitamin B12 in Health and Disease.� Nutrients, Molecular Diversity Preservation International, Mar. 2010, www.ncbi.nlm.nih.gov/pmc/articles/PMC3257642/.
Ozuguz, Pinar, et al. �Evaluation of Serum Vitamins A and E and Zinc Levels According to the Severity of Acne Vulgaris.� Cutaneous and Ocular Toxicology, U.S. National Library of Medicine, June 2014, www.ncbi.nlm.nih.gov/pubmed/23826827.
Pham-Huy, Lien Ai, et al. �Free Radicals, Antioxidants in Disease and Health.� International Journal of Biomedical Science : IJBS, Master Publishing Group, June 2008, www.ncbi.nlm.nih.gov/pubmed/23675073.
Senoo, Haruki, et al. �Hepatic Stellate Cell (Vitamin A-Storing Cell) and Its Relative–Past, Present and Future.� Cell Biology International, U.S. National Library of Medicine, Dec. 2010, www.ncbi.nlm.nih.gov/pubmed/21067523.
Wong, Cathy. �Benefits of Vitamin C You May Not Know About.� Verywell Health, Verywell Health, 17 July 2019, www.verywellhealth.com/the-benefits-of-vitamin-c-supplements-89083.
Zempleni, Janos, et al. �Biotin.� BioFactors (Oxford, England), U.S. National Library of Medicine, 2009, www.ncbi.nlm.nih.gov/pubmed/19319844.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Gut and Intestinal Health, Nutrition, Wellness
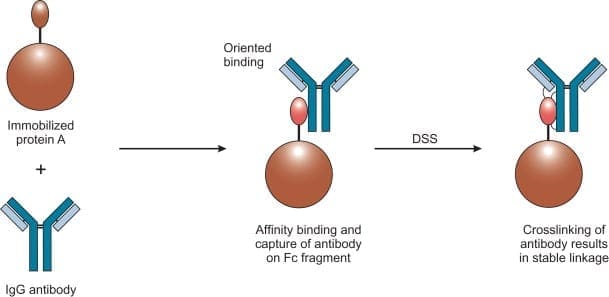
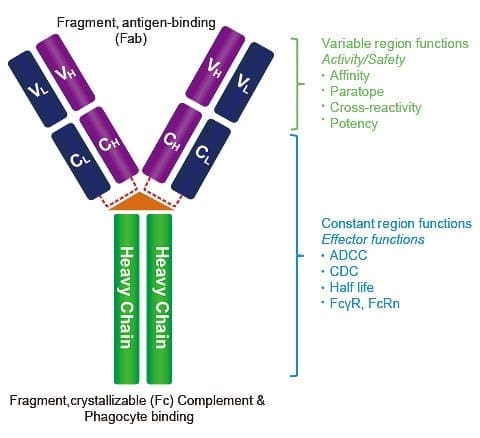
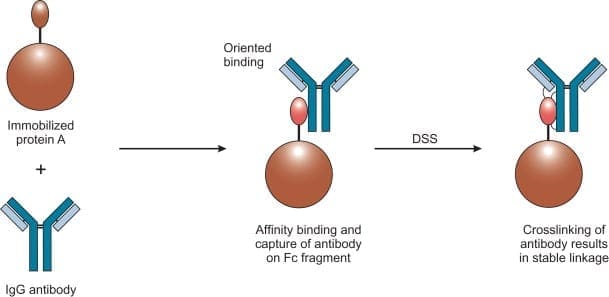
Today, we will be talking about what does the protein compounds and the peptide compounds do when a patient is being tested for food sensitivity. And we will also discuss what the Lectin and Dairy Zoomer do when a patient has a reaction to those types of food groups. In the last article, we mentioned about immunoglobulins in the intestinal barrier. And what do IgA and IgG antibodies do to the peptide and protein level?
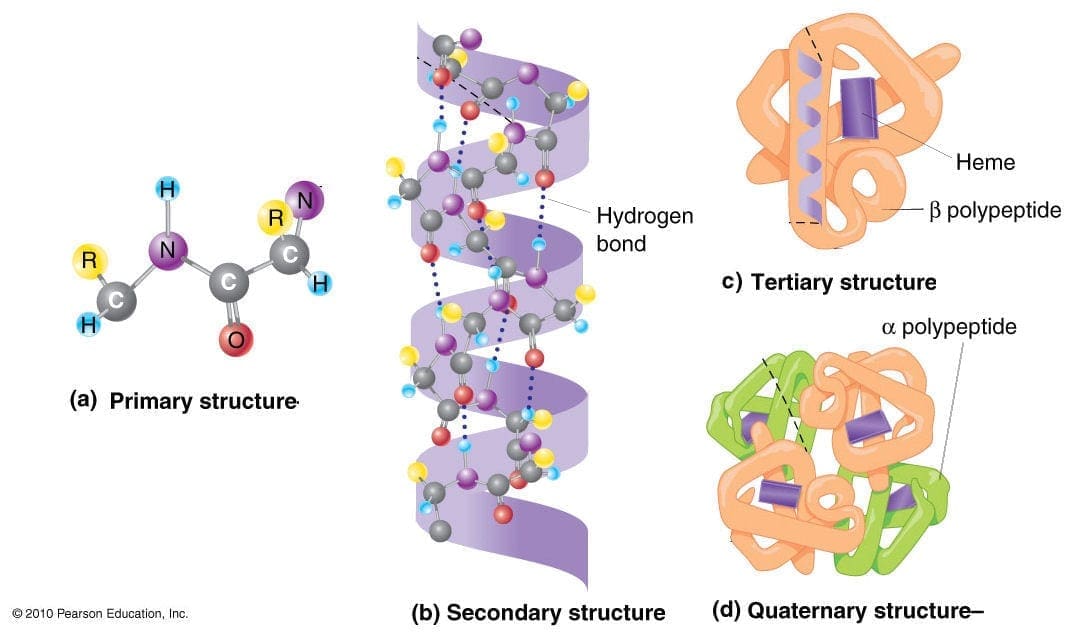
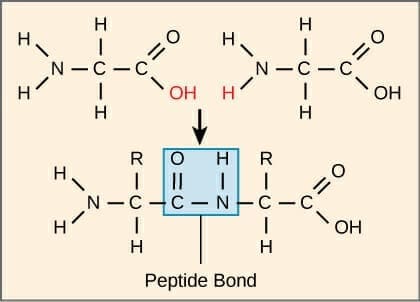
Proteins vs. Peptides
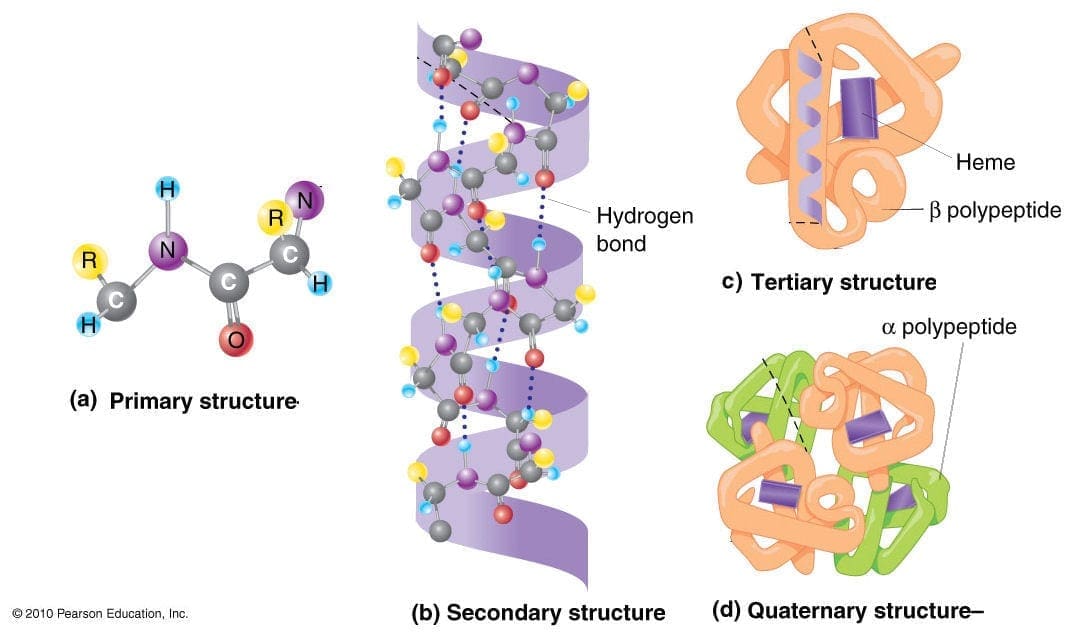
So let us take a look at proteins and peptides since this is what Vibrant Food Zoomers are actually testing on a patient. Remember that the Food Zoomers are testing the peptides in the whole protein and testing all the links to see what the patient is actually sensitive to the foods they are consuming.
Proteins
Protein is basically abundant biomolecule that is consist of one or more long chains of amino acid residues. Proteins can be found in whole foods like meats and vegetables that can help the muscles in our bodies. In the last article, we talked about how IgA and IgG antibodies are used for food sensitivity testing.
However, there is a limitation of a whole protein food sensitivity testing on a patient. Practitioners do make the assumption that the patient�s gut barrier is functional and intact since there are no signs of a leaky gut syndrome presented in the results. But, if that patient has the leaky gut syndrome, then the food sensitivity test will reflect what the patient has been eating. Another assumption is that the patient�s HCI and digestive enzymes are sufficient for tolerable proteolysis. Which means that those enzymes are breaking down whole proteins into smaller peptides.
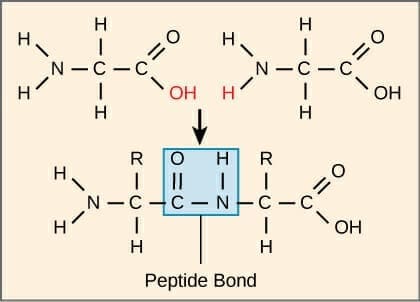
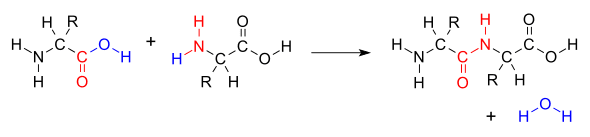
Peptides
Peptides are what in protein molecules as they are short chains of amino acids and are linked by the peptide bonds. When they are being tested by the food sensitivity tests, the reproducibility is higher. It doesn�t rely on the excess HCI (hydrochloric acid) or enzymes. What the test eliminates is the cross-reactivity because peptides in proteins are not going to have molecular mimicry to other unrelated proteins.
The antibodies are highly specific to the peptides because they are not going to be generalized or more massive antibodies of proteins since cross-reactivity is eliminated. Another thing is that the peptide test does is that it can measure thousands of peptides in one protein for a full spectrum of reactivity.
When patients are coming in with digestive problems and inflammatory condition/symptoms, practitioners take note that a lot of patients commonly have hypochlorhydria and deficiencies of enzymes and/or bile acids. Most patients sometimes have moderate to severe impairment of the intestinal barrier. When that happens, local doctors discuss with them that they may have to change their diets slowly but surely. And with integrative functional medicine that can occur.� Local practitioners look at their patient�s ailments and start detoxifying their bodies slowly. This helps their bodies heal and recommend them whole, nutritious, organic foods, and supplements to help repair the body naturally. Sometimes medicines can cause disruption to our bodies, however with whole natural foods and specific diets, it can help restore our bodies. Plus making sure that we exercise to make our bodies feel good and look good.
So now that we understand what proteins and peptides do when they are being tested. Let�s take a look at the food zoomers that can help you in case you have a sensitivity to these food groups. These are the Vibrant Lectin Zoomer and the Dairy Zoomer.
Lectin Zoomer
The Lectin Zoomer is consist of a handful of lectins and a handful of aquaporins. The most common lectins that people consume are barley, bell pepper, chickpea, corn, cucumber, potato, etc. And the most common aquaporins that people consume are spinach, soybean, tomato, tobacco, etc.
Difference between Lectins and Aquaporins
The difference between lectins and aquaporins is that lectins are sugar-binding proteins that are found in both animals and plants, which can bind to the carbohydrate structures on cells. While aquaporins are water channels that are found in cavities in both plants and humans. Some aquaporins can cross-react and can lead to primarily neurological symptoms.
How Problematic are Lectins?
Some studies show cell toxicity in humans is done by using extreme cytotoxic lectins. Ricin, for example, is a common biological warfare element that is not from the commonly consumed legumes or grains. It contains cytotoxic lectins and is being consumed by animals like mice or pigs. The assumption is being made that there are similarities with humans and animal gut glycosylation (the process of sugar-binding) in these situations.
Unfortunately, though it hasn�t been demonstrated thoroughly. But lectins have biological activity in the human body. They have been used as a cancer treatment mechanism because they can agglutinate cancer cells. Which means that they produce cytotoxicity to cancer cells and can actually carry chemotherapy across cancer cell membranes.
Even though that is a good thing, lectins can facilitate the bacterial endotoxins across the epithelial barrier and go into the peripheral tissues. And that can cause inflammation to the intestinal epithelial barrier in the small intestines. Animals studies show that raw lectin consumptions can cause hemagglutinating effects, causing inflammation.
But we as humans don�t eat raw lectins because they are cooked, not pressurized cook. Certain foods that are lectins can be eaten raw or cooked. But animal studies stated that they are using for these studies are grain and legume lectins that are raw like beans and grains. But the upside is that lectins can affect the metabolism of nutrients to increase fat loss which is a positive side effect.
Measuring the Sensitivity to Lectins
On the Food Zoomers test, lectins are really not included in each analysis, except for the Wheat Zoomer. Surprisingly, a Food Zoomer may be non-reactive, but whoever is sensitive to a lectin component in the food they eat, may be reactive. So when that happens, it is necessary to eliminate the food temporarily.
If you are sensitive to a particular food, you can have a Food Zoomer and a lectin Zoomer combine. Because if you are sensitive to the food you consume, and it doesn�t show up on the Food Zoomer, but it shows up on the Lectin Zoomer. Then you should eliminate it from your diet for a bit until you retake the test.
Conditions Associated with Lectins
If you do have a lectin sensitivity, here are some of the terms that can affect your body.
- Arthritis/rheumatoid arthritis
- Connective tissue disorder
- Gastrointestinal inflammation
- Intestinal permeability
- Possible cancer in established cancer patients
Now let�s take a look at the Dairy Zoomer and its functions if you are sensitive to whole dairy products.
Dairy Zoomer
The Dairy Zoomer is a peptide level assessment of the full spectrum of immune response possible to proteins in cow�s milk dairy. What this means that the Dairy Zoomer is only specific to cow�s milk. Since some proteins in cow�s milk are similar enough in the molecular structure to have the same homology to goat or sheep�s milk.
This means that these other kinds of milk may be potential can cause inflammatory in some individuals. The oral challenge for alternative types of fluid may be warranted, but use your best clinical judgment after the intestinal barrier is healed.
What the Dairy Zoomer does is that it takes the milk protein and breaking each individual protein down to its different peptides. If you are wondering if the Dairy Zoomer is a test for lactose intolerance, it is not. Since lactose intolerance is not an immune-based reaction to dairy and does not involve any protein constituents of the food, therefore no antibodies are being generated.
What it is going to test for is the casein and whey proteins in the milk product from all animals, and the ratio of these proteins will vary by species. But all the proteins and milk will generally fall into one of these two proteins.
What to do with the results?

Once your patient comes back after taking the Food Zoomers test, here are some of the things to look for when you are retesting them.
- If there are any IgA antibodies still in your patient, warrant an immediate elimination, regardless that it�s moderate or positive.
- If there are any Moderate IgG antibodies in your patient, then it should be eliminated in the short term. Then rotate after a 30-60-day elimination and assessing the status of the intestinal permeability to confirm that that gut barrier is no longer �leaky.�
- If there is a positive IgG result, then it should be eliminated long term and only reintroduced after 90+ days and confirm of an intact intestinal barrier.
Conclusion
So all in all, food sensitivity combine with the food zoomers test are an excellent way to help your body, especially the intestinal system. The Food Zoomers we used is functional for our patient�s wellness. Because we want to get rid of the excess antibodies and heal our patient�s body through the use of functional medicine.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chiropractic, Functional Medicine, Functional Medicine Series, Wellness
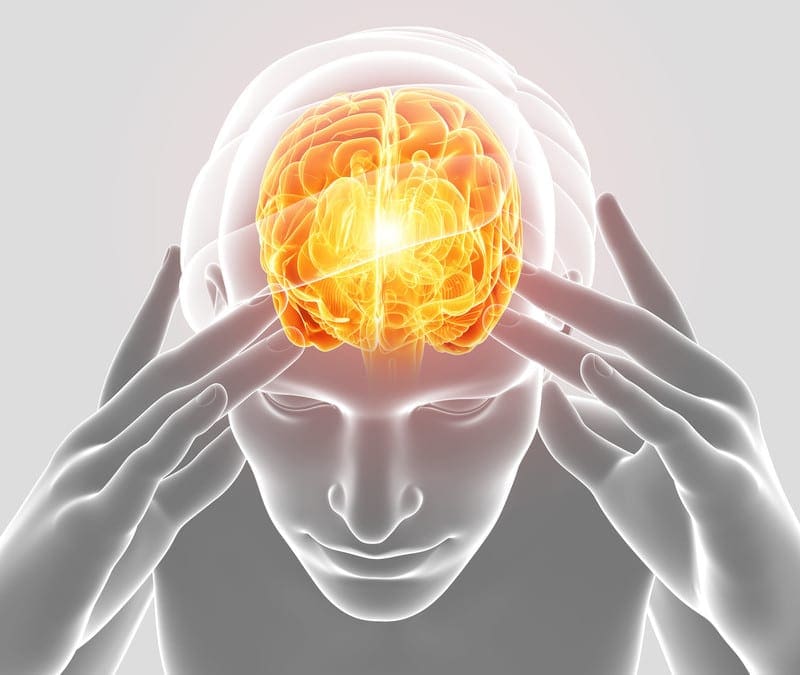
As a doctor who practices functional medicine, Dr. Jimenez utilizes the Neural Zoomer Plus. This is a blood test that analyzes neurological autoantibodies which offer very specific antibody-to-antigen recognition. The Neural Zoomer Plus tests the reactivity an individual has to 48 neurological antigens. These neurological antigens may be related to neurological disease and can help individuals assess the presence of a neurological condition.

There are 48 markers that are measured and they can be summed up and categorized into 7 larger groups. These groups include demyelination antigens, blood-brain barrier disruption, optical and autonomic nervous system disorders, peripheral neuropathy, neuromuscular disorders, brain autoimmunity, brain inflammation, and infections. (For a full list of the markers that the Neural Zoomer Plus measures, click here).�
The truth of the matter is that autoimmune disorders affect 5-10% of the general population and can target virtually and structure within the central or peripheral nervous system. Symptoms of an autoimmune disorder involving the CNS/PNS include but are not limited to:�
- Cognitive decline
- Memory loss
- Ataxia
- Balance problems
- Neuropathy
- Alzheimer’s disease
- Multiple sclerosis
- Encephalitis
- Muscle spasms
- Huntington’s disease
- Epilepsy
- Parkinson’s disease
- Dementia�
- Myasthenia gravis
- Muscle stiffness/rigidity�
- Optical decline
- Neuromyelitis Optica
- History of concussion
- Autism
- PANDAS/ANDAS/OCD
- Demyelinating diseases�
 �
�
Having the tools to prevent a disease or disorder can be life-changing. With the ability to assess these markers, the rate of cognitive decline can steadily reduce. If you suffer from any of the above symptoms, the Neural Zoomer Plus may be right for you.
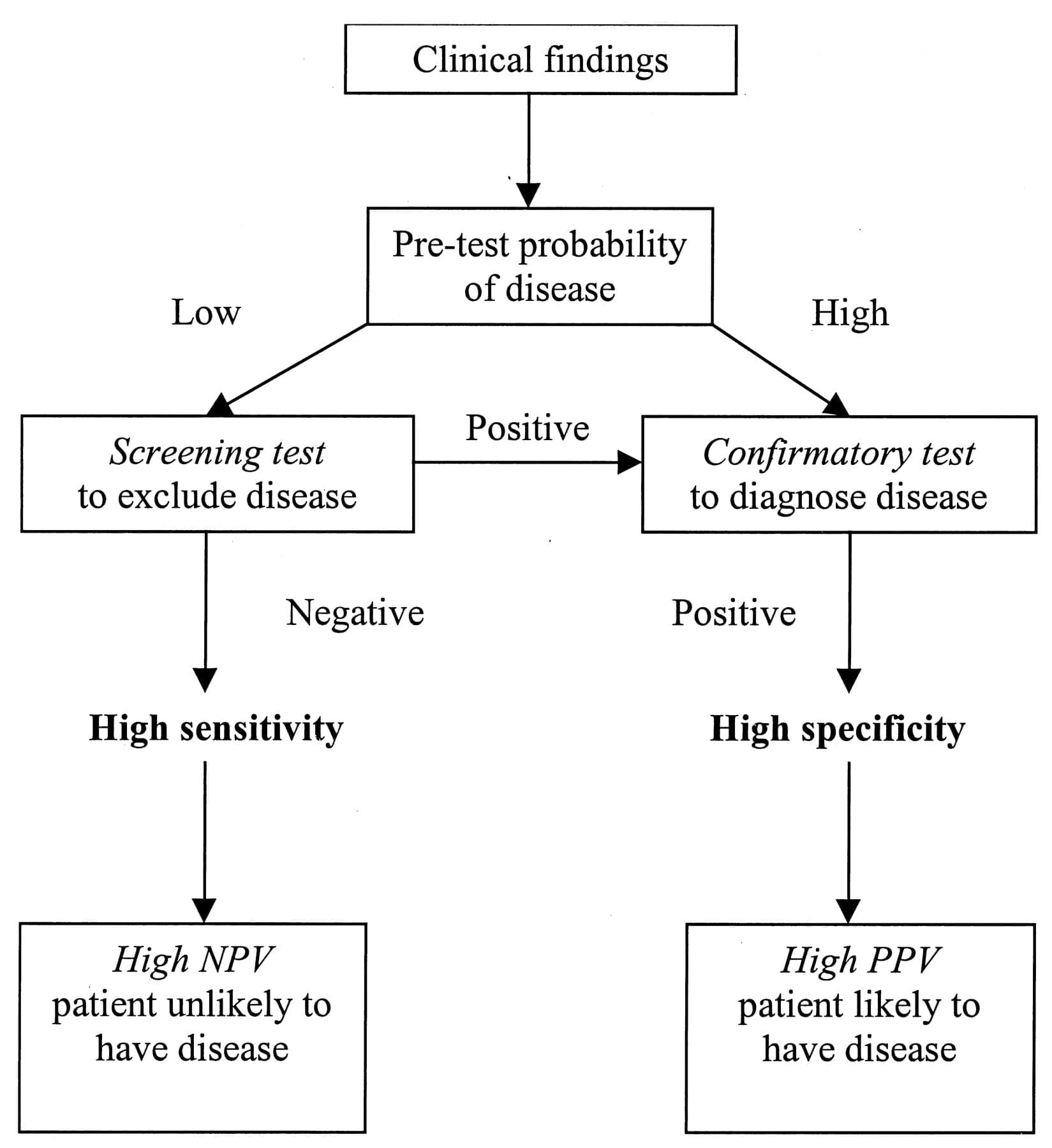
The intention of having our patients complete a Neural Zoomer Plus is to help us detect an individual’s IgA, IgG, and IgM sensitivity to antigens, down to the peptide level. Once we receive the results, not only do we have a resource that aids in the early detection of neurological diseases, but we also have a path. This path allows us to create a personalized prevention plan that will focus on the patient along with their lifestyle. – Kenna Vaughn, Senior Health Coach�

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Functional Medicine, Gastro Intestinal Health, Gut and Intestinal Health, Wellness
The usage of integrated functional medicine is essential when it comes to our bodies overall health. Local practitioners and health coaches, talk with patients on what seems to bother them. Sometimes it is a simple adjustment, but mostly it�s what�s causing them problems on the inside. Some patients have inflammation around their intestinal epithelial barriers, and it can cause a leaky gut.
In the previous article, we talked about what the microbiomes do in our intestines and what is their functions are in the intestinal epithelial barrier. However, today we will discuss what the immunoglobulins antibodies do with proteins and peptides in the intestinal permeability. As well as explaining what the Lectin Zoomer and the Dairy Zoomer does when a patient has a food sensitivity and needs testing in a two-part series about the intestinal permeability and food zoomers.
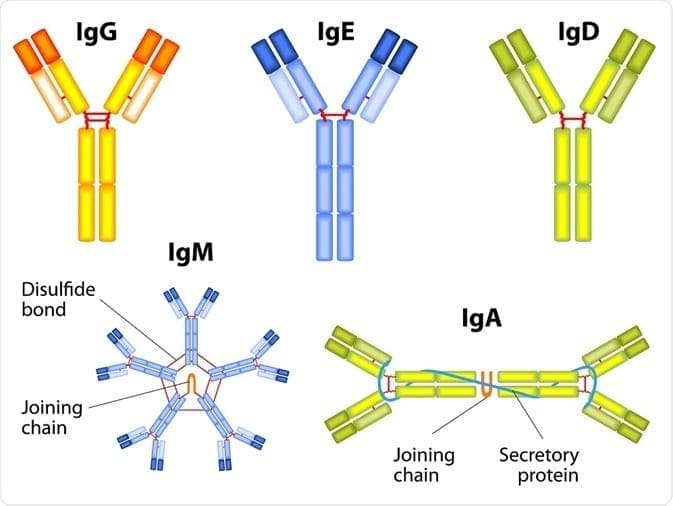
Immunoglobulins
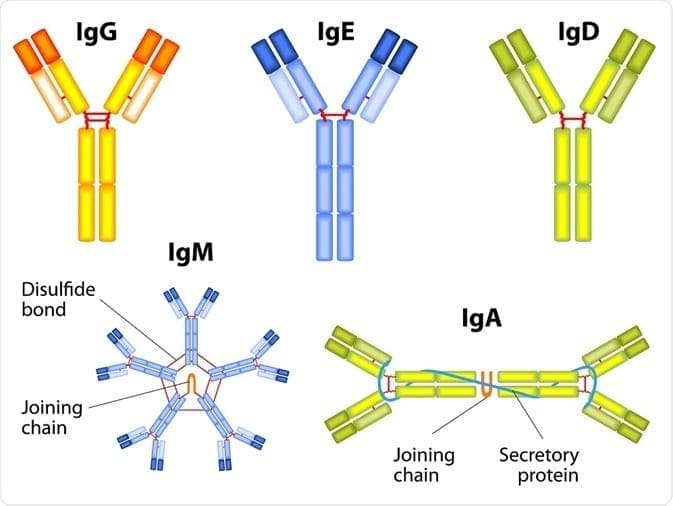
The first thing that we need to know is that immunoglobulins are immune-mediated reactions. So anything that involves the immune system will cause a hypersensitivity reaction to one or more food or foreign proteins, and their presence can be of one or more types of immunoglobulins.
There are 3 terms of hypersensitivities that can be involved with immunoglobulins:
- Allergies are the ones that are most common and are associated with anaphylaxis. Patients can have a very severe and acute immediate reaction to specific allergens like food or environmental like pollen or a bee sting.
- Non-allergies, sensitivity reactions involved either chemical mediators or antibody reactions.
- Food intolerances are non-immune-mediated reactions, and a good example is Lactose Intolerance or a bile salt deficiency. These can make somebody who has a food intolerance, can�t digest fat.
These three terms are often mistaken and used interchangeably clinically, but they are entirely different since they are not interchangeable. Especially when it comes to sensitivities and intolerances because those two commonly get used in place of each other, but they are totally different.
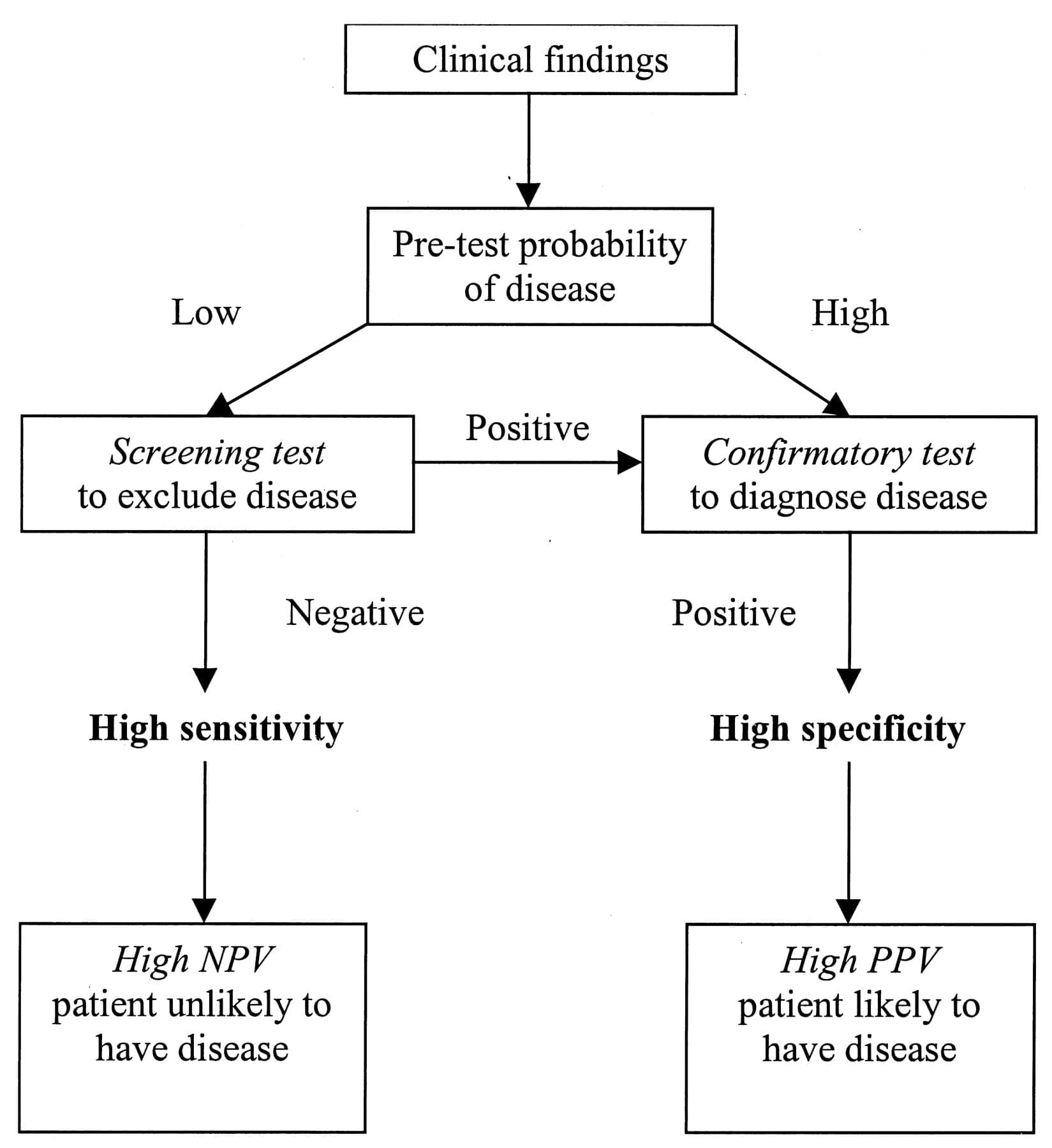
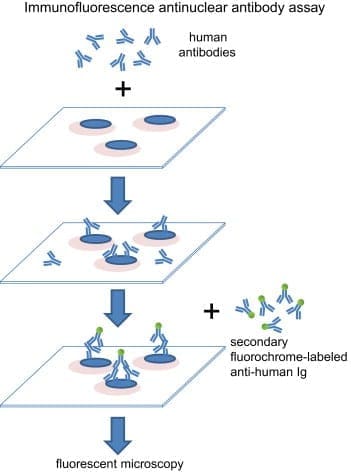
If you are testing your patient�s immunoglobulins, remember that antibodies are particular to each type of foreign substances and can be in three types of hypersensitivity. Antibodies will only bind an react to the specific proteins of the foreign material but not to the substance�s extract. The most common ones are type 3, where it involves IgG, IgA, and IgM. This type can tell us what cells and mechanisms are involved.
Type 3 Hypersensitivity Mechanisms
Here are the types of mechanisms that are involved with Type 3 immunoglobulins.
- Antigens are a foreign protein that is present and is recognized as a threat or non-self.
- Antibodies will bind to the antigen to neutralize or keep it from linking to anywhere else in the body. This is where the immune complex is formed.
- Immune complexes insert themselves into the small blood vessel, joints, tissues, and glomeruli, causing symptoms to the body.
- They are far more capable of interacting with complement proteins to form medium-sized complexes; which has an excess amount of antigens that are high pathogenic.
- However, once the immune complex is in the tissue, it can induce an inflammatory response and cause damage to the body. This damage is the result of the action of cleaved complement anaphylatoxins, which can mediate a mast cell degranulation.
- With the recruitment of inflammatory cells in the tissue, it can lead to tissue damage through phagocytosis.
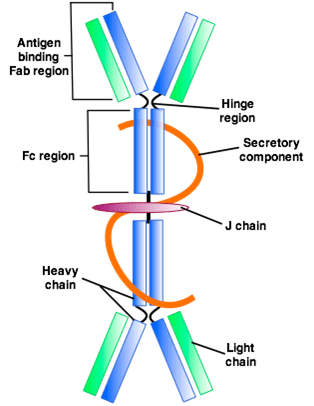
IgA and IgG
In a previous article, we mentioned the mechanics of the intestinal permeability. However, we going to discuss what IgA antibodies and IgG antibodies do to the gut and to the entire body.
IgA Antibodies
IgA antibodies are found in the body where there is a mucosal lining around the areas like the nose, breathing passages, digestive tract, ears, eyes, and vaginal region. These surfaces are exposed to the outside of the environment either by air, food, or other foreign substances regularly.
IgA antibodies actually protect the body surfaces that are exposed to outside foreign substances, and these antibodies can be found in saliva, tears, and blood.
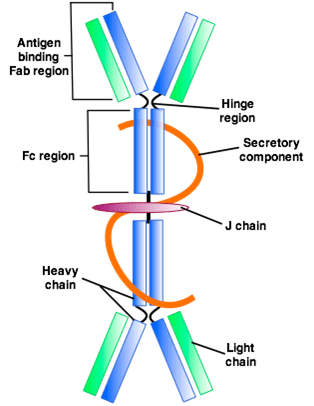
In the gut, however, it can bind to the mucosal layer on the top of the intestinal epithelial cells to form a barrier to neutralizing threats before they reach the cell. And that is very important, especially since IgA is like an insurance policy for your gut.
IgA antibodies are considered as non-inflammatory. Which means that they don�t stimulate inflammatory processes in the body like IgG does. They do, however, create a mucosal response to a foreign antigen, and it is usually microbial (ex., bacteria, yeast, viruses, parasites) or microbial toxins. They can also generate a response to pollutants, toxins, and recognized undigested food as a foreign protein.
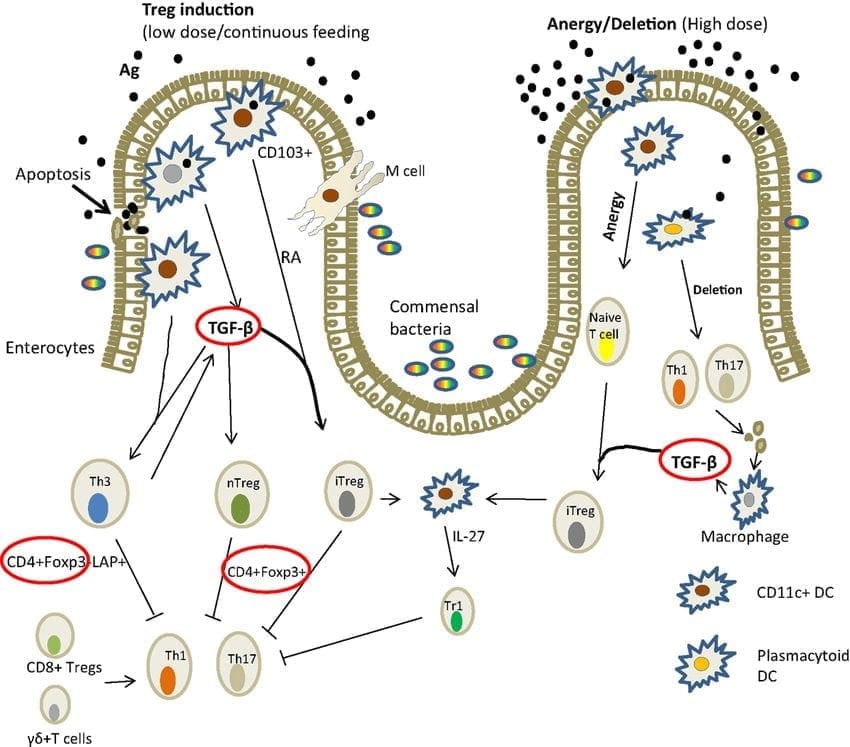
In the intestinal lumen, IgA can be indicative of an immune response stimulated by T-b cell interaction. So a healing intervention, if a patient has an abundance of IgA antibodies may need to target TH1 and TH2 balance so it can regulate T-reg production.
IgG Antibodies
IgG antibodies are found in all body fluids. They happen to be the smallest but the most common of all antibodies as they make-ups about 75% to 80% of antibodies found throughout the entire body. These antibodies are essential as they fight against bacterial and viral infections, and they are the only type that can cross the placenta.
They do indicate exposure to a specific antigen, but they don�t always necessarily indicate active inflammation; however, they can contribute to it in a dose-independent.
Why measure IgA and IgG?
So why do we measure IgA and IgG? Surprisingly some people don�t produce as much or any IgA antibodies, and therefore, local practitioners would not know if their patients have formed a reactivity to an antigen if they don�t check their IgG levels.
Surprisingly, some IgG antibodies are not an indicator of actual inflammation or disease process. Some IgG antibodies are formed in response to a protein as sort of a tracker in the body but do not elicit a reaction. However, IgA antibody is coupled with IgG to indicate a bit stronger immune response to an antigen in some cases.
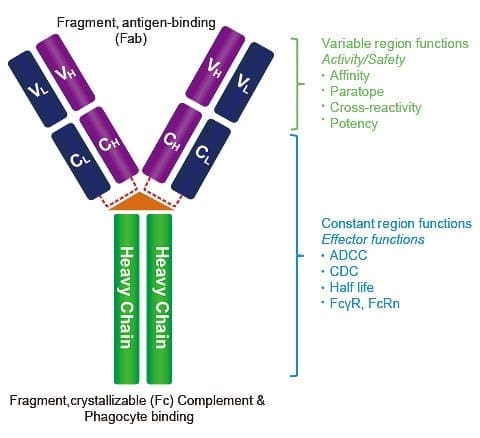
IgA and IgG in the Protein Level
IgA and IgG testing in the protein level is what the food sensitivity tests are looking at. They look for the whole protein, which is the extract level. All food sensitivity test looks for residues of carbohydrate and lipid-based particles. It�s not pure protein but that what the test does, it seems for the reactive compound. Some of the strengths are that the test gives an acute measure of IgG and IgA to a specific protein. It can also be suitable for associating Type 3 reactions involving IgG and IgA complexes, and if the IgG is pathogenic, then it will be beneficial.
Some of the weaknesses are that IgG can be a protective antibody, and it may be a good thing. It means that the immune system is handling it and there�s nothing necessarily wrong about that. IgG and IgA antibodies represent whole proteins being presented to the immune system can it also be an indicator that a patient may have a lack of sufficient digestive capacity when many food sensitivities are being detected.
IgG and IgA in the Peptide Level
When IgG and IgA are being tested at the peptide level, this is where the food zoomer test focuses on. This is because there is a high level of antibodies specificity, cross-reactivity is minimized if not completely eliminated. The concept of foods that are cross-react, for example, gluten, might cross-react to other foods that are similarly shaped in their molecular structure, then you should eliminate the gluten out of your diet as well as the foods that are in contact with them.
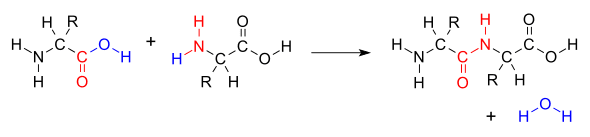
However, if the antibodies to gluten are being picked up at the peptide level, then it won�t look at those foods that are being cross-reactive to gluten. The antibodies will only bind to the individual peptides than the whole protein. This will be a more accurate assessment of whether or not that the patient is sensitive to the foods their body is reacting to.
What is Loss of Oral Tolerance?
Loss of oral tolerance is a term used to describe the phenomenon of someone developing a sensitivity, whether it is accompanied by symptoms or not, and it�s usually a commonly consumed or semi-regularly consumed food. When that happens, there is a production of inflammatory cytokines and antibodies that will respond to the continued exposure to the food.
For the inflammatory responses to be eliminated, patients have to remove the offending food for about 3 to 4 weeks if IgA antibodies are present or 3 to 6 months if the IgG antibodies are present as well. This is the only way for the antibodies to disappear, and the intestinal permeability can heal. But the disappearance of antibodies does not guarantee that oral tolerance has been established. If you are retesting a patient and if the antibodies are gone, that indicates that the patient has done an excellent job in eliminating that food from their diet. However, the only way to know is to reintroduce the food and retest after a few months, just to make sure that no antibodies are being produced after the intestinal barrier has been fully healed.
Conclusion
All in all, that is what the intestinal permeability does when we have IgA and IgG antibodies and what do they do when there is food sensitivity in the body.� However, it is crucial that our patients understand that we here at Injury Medical Clinic, take the time to study what causes inflammation in our patients and using integrated functional medicine to make sure that their intestines are being healed naturally. In the next article, we will discuss the difference between peptides and proteins, and about the Lectin and Dairy Zoomer.
by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chiropractic, Functional Medicine, Health
The Neural Zoomer Plus is a blood test that is designed to test 48 neurological antigens. When testing for these antigens, the results these markers find can help physicians determine if a patient is at risk for neurological conditions later on. To view last week’s article containing a full list of the signs and 48 markers, click here.�
When a patient comes to us with concerns, we listen very intently and make sure our patient’s concerns are addressed. More often than not, patients reveal they are having issues that relate to neurological declines, such as, muscle spasms or memory loss. With symptoms like these, the patient is referred to get a Neural Zoomer Plus.�
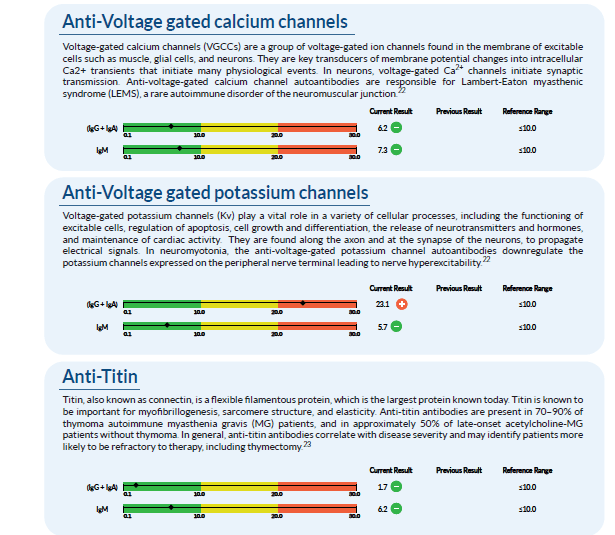
Once we receive the results back, it is compiled into a large report. From here, we assess it and go through all of the markers with an additional team of clinicians. An example of a few of the markers tested in a Neural Zoomer Plus is below. One can see that this patient has an elevated �Anti-Voltage gated potassium channel�. Anti- Voltage-gated potassium channels are responsible for multiple cellular processes such as cell growth and differentiation.�
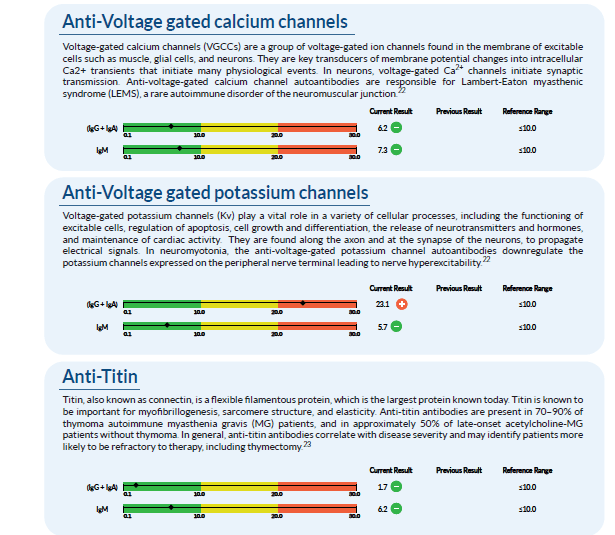
After analyzing the data, we take these findings and create a treatment protocol that is specific to each patient and their lifestyle. Due to the fact that this patient shows an elevation in specific markers, there are certain adjustments we make in order to help prevent or reverse the cognitive and physical effects of neurological disorders.�
The first step we take is to change the diet of the patient. Many foods are not properly digested, leading to gut inflammation, which further leads to �leaky gut� which then enters the bloodstream and into the blood-brain barrier, causing neurological decline. In order to reverse these effects, we want to make sure the gut is getting the proper nutrients from foods that will not cause inflammation. For this patient, we recommend the Wahls Protocol.�
The second step we take is to usually get the patient involved in a more active lifestyle. By having this patient start to exercise with activities like yoga, it can improve the state of mind and their mind-body connection.�
The third step is usually nutraceuticals. These are supplements that will naturally help the body and brain with no addictive or harsh chemicals. With every patient, the nutraceuticals and amount needed vary depending on their specific body. For this case, we recommend:��
N-acetyl-L-cysteine:� (NAC) is a precursor to glutathione, the body�s most important cellular�antioxidant. NAC supplements have been shown to increase cellular glutathione levels.
Vitamins B12, B6, and folate: These are metabolic cofactors important for cellular metabolism and maintenance of all tissue cell types, but particularly important to nerve cells. Deficiencies in�B12 or folate can raise homocysteine levels, which have been associated with a higher risk for�vascular disease and dementia.
Alpha Lipoic Acid:� (ALA) is an essential cofactor in normal cellular metabolism and cellular�energy production.
Vitamin C and vitamin E: Can reverse symptoms caused by vitamin C and E�deficiencies.
As mentioned before, each patient is different and their lab work shows varying needs. However, with the Neural Zoomer Plus, we are able to get ahold of these symptoms, create a personalized treatment plan, and get them under control.�
As one can see, the data and knowledge we gain from these tests are truly eye-opening and give us an early advantage to help reverse or aid in prevention methods. We take the needs and concerns of every patient very seriously and work extremely hard to figure out the right method of treatment for them. Our goal is to help ensure that this lifestyle change is as smooth and easy on the patient as possible so they can get back to enjoying the activities they love and spending time with loved ones. The transition into a new lifestyle can be stressful, but with the information we gain from the tests, the knowledge we use from the doctor, and the willingness to change from the patient, we are set up to be the best team you can have to get your life back! – Kenna Vaughn, Senior Health Coach�

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chiropractic, Functional Medicine, Nerve Injury, Wellness
When we look at our patients, we try to figure out what is causing their ailments from living their best lives. Some practitioners would prescribe medications to alleviate pain. While other practitioners will start trying to figure out what is causing the patient to have these ailments. Here at Injury Medical Clinic, we talk to our patients about the importance of functional medicine and how it can benefit them. In this article, we will be discussing Connective Tissue Disorder and how it is linked to wheat-related disorders.
What is Connective Tissue Disorder?
CTD (Connective Tissue Disorder) is an autoimmune disorder that can affect the connective tissues such as the collagen and elastin in our skins. This disease is highly inflammatory and can occur alongside with other autoimmune diseases, and it is common if families have a history of Connective Tissue Disorder.

About 3% of the population has a connective tissue disorder, and it is most likely to occur in women than men. In fact, women who are diagnosed with connective tissue disorder have a ration of 10:1, compared to men.
CTD includes (but is not limited to) the following conditions:
- Systemic Lupus Erythematosus (SLE): SLE is a widespread and chronic autoimmune condition, for unknown reasons, can cause the immune system to attack the body�s own tissue and organs, including joints, kidneys, heart, lungs, brain, blood, and skin.
- Sjogren�s Syndrome: This autoimmune disease causes white blood cells to attack moisture-producing glands, such as the tear ducts and salivary glands. This can make it very difficult for the body to produce tears and saliva.
- Systemic sclerosis (scleroderma): This condition causes the skin and connective tissue to harden and tighten.
- Rheumatoid arthritis (RA): RA is a chronic inflammatory condition and an autoimmune disorder that can generally affect the lining of the joints, but mostly in the hands and feet. Rheumatoid arthritis causes painful swelling that can eventually lead to deformity and erosion in the joints and bones.
- Polymyositis: This is a persistent inflammatory muscle disease that causes weakness in the skeletal muscles, which can affect your body movement.
- Dermatomyositis: This is an uncommon inflammatory disease that is marked by muscle weakness and can cause a distinctive skin rash.
These conditions can group together and can be very hard to diagnose because of the research and many tests that the patient is taking. Surprisingly, the average patient suffers from symptoms for 3.6 years before meeting diagnostic criteria. And the systems alone are difficult to classify, and often mimic or overlap other conditions. Some of the symptoms include hair loss, muscle pain, numbness or tingling, inflammation, low-grade fever, weakness and fatigue, joint pain, sensitive skin, and rashes.
Increased Need For Advanced Testing and Early Diagnosis

Sadly though, patients wait longer when they have these conditions, and it can worsen in the process as it takes years to get diagnosed for CDT. Practitioners can use treatments on their patients, but the medications act as a band-aid to mask the symptoms, but it does not adequately address the root causes of the disease. Sometimes the symptoms can progress faster than the current diagnostic test. So if you want to make sure your patients have any autoimmune diseases, run a diagnostic test on them, so you can detect early stages of the disease and start treating them so it can go away.
ENA and ANA
Extractable nuclear antigen (ENA) is a blood test that looks for antibodies to about 6 or 7 different proteins in the body.
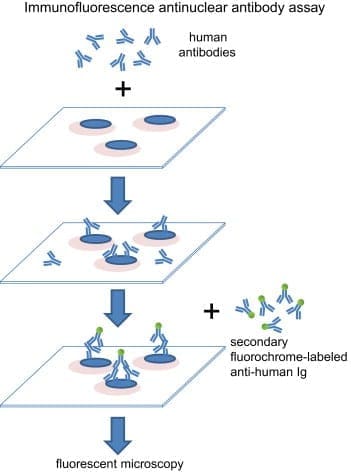
Antinuclear antibody (ANA) is used as an initial test that can help evaluate a person for an autoimmune disorder that can affect many tissues and organs throughout the body. It is most often used when practitioners are diagnosing patients for systemic lupus erythematosus.
Surprisingly ENA can be more predictive than ANA. However, patients were followed for 2 years, and about 20% of those patients developed positive ENA.
Vibrant Wellness Wheat Zoomer
In�a�previous article, we talked about gluten sensitivity and introduced the wheat zoomer. What the Vibrant Wheat Zoomer does is that it actually runs a test on your microbiomes to determine if you have a wheat sensitivity or a gluten sensitivity. It can actually detect IgG and IgA antibodies as well as detecting if your body has the celiac disease and intestinal permeability.� It pairs well with the Vibrant Gut Zoomer, and here at Injury Medical, we use the Wheat Zoomer on our patients to inform them about what is causing them to have gut inflammation or even leaky gut.
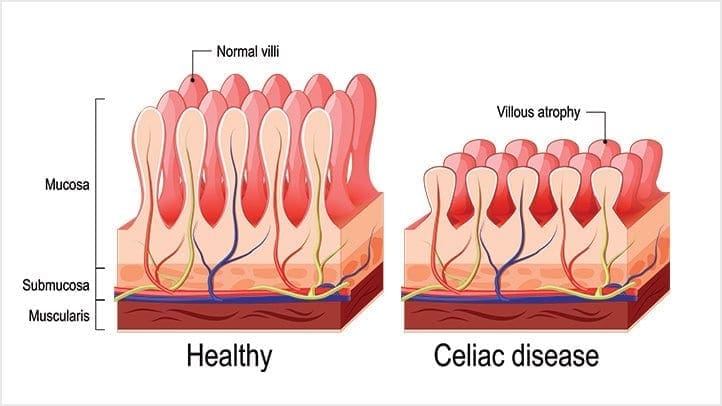
Celiac Disease and Wheat Allergens
Celiac Disease and Wheat Allergens is an autoimmune disorder in genetically susceptible individuals, and it affects about 1% of the population. In a previous article, we mentioned the hidden problems that gluten does to the body. And surprisingly, any wheat-related disorders can exist on a spectrum, this includes wheat allergy, gluten sensitivity, and wheat sensitivity.
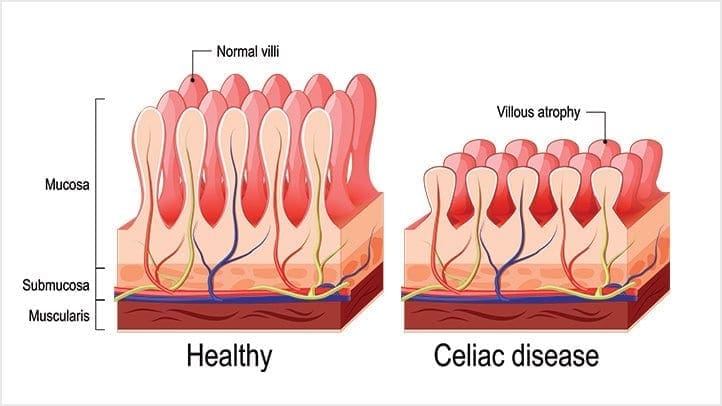
When a person, has the celiac disease, having any traces of wheat can actually upset their intestinal permeability and causing them to have a leaky gut.
The Connection to CTD and Celiac Disease
But how do connective tissue disorder and celiac disease are connected? Well, surprisingly, Rheumatoid arthritis (RA) and celiac disease (CD) share multiple aspects in epidemiology and clinical manifestations. Both disorders have been proven to be influenced by comparable environmental factors and a recent incidental surge of associated antibodies. Even though they have different depositions, both of them are mediated by endogenous enzymes that target different tissues and organs.
Conclusion
However through functional medicine; local chiropractors and health coaches here at Injury Medical Clinic, strive to understand what do our patients need to make their bodies feel better. If we can use functional medicine to prevent leaky gut at the early stages and help our patients with any ailments that they may have, then we can gently push them into the right direction of exercising throughout the week (even if it is about thirty minutes) and eating nutritious, whole, organic foods; as well as, preventing their ailments coming back then their bodies can finally heal.
by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Functional Medicine, Gut and Intestinal Health, Health, Wellness
In the last article, we talked about what the polyphenols do in the microbiome and in the previous section, we discussed about the microbiome functions in our bodies. However, today we will be concluding the three-part series of the microbiome functions in our bodies as well as presenting on the top 5 environmental toxins that can disrupt the gut microbiome, finding ways to de-stress ourselves, and learning about the different foods that can help detoxify our bodies so we can live a healthier life.
Top 5 Environmental Toxins Disrupting the Gut Microbiome
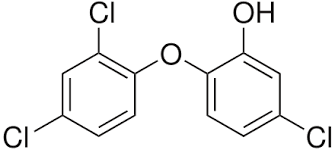
Triclosan
This is a synthetic antibacterial chemical found in personal care products such as soap, mouthwash, toothpaste, hand sanitizer, and deodorant. It is easily absorbed through the skin and gastrointestinal tract and rapidly alters the microbial composition of the digestive tract if it is ingested. However, this rapid restructuring of the gut microbiome impairs the immune system-regulating activities of gut microbes.
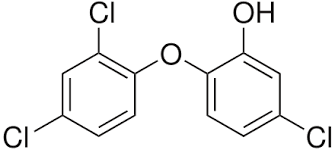
We use this chemical mostly in our daily skincare and hygiene routine so that way we won�t be sick. We tend to use this chemical compound to make us smell, look, and feel good frequently, especially in the cold and flu seasons where we use them the most so we won�t get sick. In fact, the frequent use of antibacterial products has been associated with an increased risk of food sensitivities, seasonal allergies, and asthma.
Pesticides

Surprisingly there are a staggering 1 billion pounds of pesticides used per year in the United States, and 5.6 billion pounds are used worldwide. Most farmers used it to spray down the insects so that way their crops won�t be destroyed. And we used pesticides on our lawns to get rid of weeds and keep the bugs off our gardens.
However, did you know that pesticides can kill beneficial bacteria in our gut? Studies, especially animal studies, indicate that pesticides can destroy the beneficial gut bacteria and can increase the risk of intestinal dysbiosis and cause immune system disorders, among with many other chronic health issues.
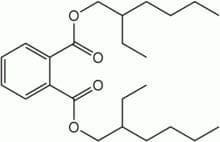
Plasticizers
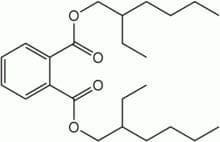
These are chemicals that provide flexibility or rigidity to plastic products. These chemicals are highly prevalent in our environment and have a significant impact on gut bacteria. �Surprisingly the most common plastics are mostly BPA (Bisphenol-A).

Bisphenol-A (BPA) can be found in plastic water bottles, receipts, and the lining of canned foods. They can alter the healthy gut flora and disrupts the body�s hormonal system by mimicking the hormone estrogen. We do use these to put our leftovers in after we consume food. But now and days when we meal prep our food, we do look for containers that are BPA- free. However, while often being marketed as �BPA-free,� the plastic alternatives may be equally, if not more, harmful to our gut microbes.
Bisphenol-S and bisphenol-F demonstrate endocrine-disrupting effects that are comparable to BPA. These adverse effects may extend to the gut microbiome, causing disruption. Phthalates are another class of endocrine-disrupting plasticizers that are used as solvents in personal care products and vinyl plastic, and they also reduce the levels of beneficial gut bacteria.
Heavy Metals
Heavy metals, such as cadmium, lead, and arsenic, can reduce the levels of beneficial bacteria in the gut that protect against intestinal inflammation and may promote inflammatory gastrointestinal disorders. All microbes are responsible for methylating or demethylating metals, and the exposure may exceed the capacity to perform this. Due to industrial pollution, heavy metals are the most common contaminants that are in the soil and drinking water when we grow food and drink from the tap.
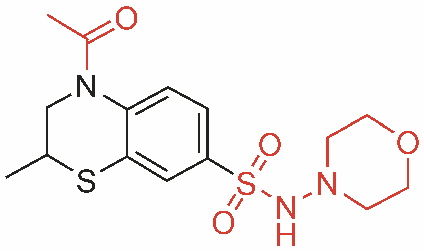
Pharmaceutical Drugs

Surprisingly most pharmaceutical drugs can help our bodies fight off infections or alleviate some pains we may be inflicted. But those antibiotics can disrupt the gut microbiome and cause an imbalance to our gut bacteria. We here at Injury Medical clinic, actually recommend our patients to alternatives to these drugs if you don�t want to disrupt your gut microbiome.
Functional medicines like whole foods and supplements can actually alleviate the pains that may cause disruption in your body.
Protecting the Microbiome From Environmental Toxins
When you want to live a healthier life and want to protect your body�s microbiome try these alternatives to get rid of these environmental toxins.
- Instead of using conventional cleaning products, which often contain triclosan, try switching to a plant-based brand. Also, try making your own cleaning products at home with natural ingredients.
- Avoid commercial body care products, as these are a significant source of triclosan, phthalates, and parabens. If you have any absorption of these chemicals, try checking out the Environmental Working Group�s Skin Deep Cosmetics Database. This database can help you find natural, healthy body care products that don�t contain microbiome-disrupting chemicals.
- Eat organic produce. Conventionally-grown fruits and vegetables are a significant source of microbiome-disrupting pesticide exposure. Research indicates that consuming organic food can significantly lower your body burden of pesticides, thus protecting your gut microbes. But y9ou are going to eat organic produce, remember to wash it first to get rid of excess pesticides.
- Try reducing your plastic intakes and limit your consumption of canned foods to reduce your exposure to BPA and BPA alternatives. When you are meal prepping, try using glass or stainless-steel water bottles and storage dishes instead of plastic, and opt for fresh food instead of canned.
- Try filtering your drinking and bathing water. Unfortunately, tap water is rife with pesticide residues, heavy metals, plasticizers, and pharmaceutical drug residues and can come off as a milky white if it�s not treated. So try to consider investing in a high-quality water filter that can remove these substances from your drinking water.
- Support your gut microbiome by consuming prebiotics and probiotics. In a previous article, we talked about probiotics in our gut. Probiotics can add beneficial bacteria to your stomach and may even help in the metabolism of toxins that are in your body�s microbiome. Prebiotics, a form of indigestible dietary fiber, that feeds probiotics and helps to support their growth and proliferation in the gastrointestinal tract.
Other Forms of Whole Body Detoxification

There are many ways to try and detoxify our bodies, so here are some examples:
- Sauna therapy
- Yoga, trampoline
- Meditation
- Energy healing/shamanism
- Taking a much-needed vacation
- Learn communication methods to accommodate multiple needs and to deal with stressful situations
Rebuilding the Gut Microbiome
When local health coaches, practitioners, and chiropractors are helping patients, they can provide a comprehensive strategy to help them gain a healthier life. When you want to rebuild your gut microbiome, try to reconstruct the natural digestive function with food/herbals. This will help support the immune system and nutritional status by creating the good bacteria in your liver and flushing out the toxins out of your system. However, try to avoid any foods that can trigger inflammation and can cause leaky gut.
Rebuild Natural Digestive Function
When you are rebuilding your natural digestive function, try finding food and supplements that contain zinc, Vitamin C, and bitter greens that can aid in the production of hydrochloric acid (HCL). However, avoid excessive amounts of fat in your diet so you won�t cause a leaky gut Also take some enzymes if you need them until your digestive is balanced and fully restored.
Support the Immune System and Nutritional Status
When your immune system is being overworked, try using micronutrient testing to identify deficiencies. Most SIBO patients are typically low in B12/iron, zinc, magnesium, and vitamin D.� But all these vitamins and supplements can support the immune system. With SIBO patients, they try to work on cleaning out their liver since it�s one of the major organs that flushes out the toxins in our bodies. If you do have SIBO, try adding more fruits and plant foods that can help �clean out the liver.� Certain fruits can be tolerated and titrated up after treatment over time, but try to reduce meat/animal fats and fats in general; since they are harder to digest and can contribute to imbalanced bile acid secretion. Also, use liver support herbs and supplements such as glutathione and silymarin.
Avoid Foods that Can Provoke Inflammation

In a previous article, we talked about food sensitivity and what to do if you have it. Some testing can be helpful to determine if other foods may need to be eliminated. Here are the most common foods that provoke inflammation in dysbiosis are:
- Gluten
- Dairy
- Eggs
- Soy
- Corn
So if you have a food sensitivity, start by slowly build the natural SCFA�s with small amounts of natural resistant starch (e.g., cooked/cooled potatoes). However, if the patient is being treated with SIBO, introduce it after. Also considering adding other sources of food so it can help grow the good bacteria in your gut. But also keep HCL production active to clean out the stomach and upper part of the small intestine.
This will ensure that the good bacteria will grow over time with your diet and the help of probiotics and fermented food. But if a patient has SIBO take caution so the patient won�t disrupt the treatments they are in and are completed.
If you are taking care of a patient, carefully choose probiotic based on symptoms they have. Some will need a d-lactate free formula, and you can bring up the dosage over time until their treatment is complete. Some CFUs (colony forming units) will vary by product and viability through the GI tract (enteric-coated vs. not), and some probiotics may need to be used long term in some individuals.
Fermentation

Fermented foods are very beneficial to our gut flora as they actually help in the production of good bacteria in our intestinal barriers. Fermented foods and beverages are literally alive with strong pronounced flavor and nutrition. However, not all preserved foods are fermented with live cultures; some may be brined through the use of vinegar and/or salt, and do not impart probiotic benefit.
 �Fermentation is the transformation of food by various bacteria, fungi, and the enzymes they produce. It is important to recognize that fermentation is a natural phenomenon much broader than social, culinary practices; cells in our bodies are capable of fermentation. In other words, humans did not invent fermentation; it would be more accurate to state that fermentation created us.� � Dr. Alex Jimenez�D.C., C.C.S.T.
�Fermentation is the transformation of food by various bacteria, fungi, and the enzymes they produce. It is important to recognize that fermentation is a natural phenomenon much broader than social, culinary practices; cells in our bodies are capable of fermentation. In other words, humans did not invent fermentation; it would be more accurate to state that fermentation created us.� � Dr. Alex Jimenez�D.C., C.C.S.T.
Conclusion
So all in all, those are some of the many ways to actually help our bodies microbiome when we want to live a healthier life. Here at Injury Medical Clinic, local chiropractors and health coaches, actually use functional medicine to patients so that way, they can fix their ailments naturally, without the use of drugs and non-conventional methods. If we can change a person�s lifestyle with functional medicine, we can repair the microbes in our bodies, one at a time naturally, of course.











 �
�








 �Fermentation is the transformation of food by various bacteria, fungi, and the enzymes they produce. It is important to recognize that fermentation is a natural phenomenon much broader than social, culinary practices; cells in our bodies are capable of fermentation. In other words, humans did not invent fermentation; it would be more accurate to state that fermentation created us.� � Dr. Alex Jimenez�D.C., C.C.S.T.
�Fermentation is the transformation of food by various bacteria, fungi, and the enzymes they produce. It is important to recognize that fermentation is a natural phenomenon much broader than social, culinary practices; cells in our bodies are capable of fermentation. In other words, humans did not invent fermentation; it would be more accurate to state that fermentation created us.� � Dr. Alex Jimenez�D.C., C.C.S.T.





