Understanding the Life and Death of a Neuron
For many years, most neuroscientists believed we were born with all the neurons we were ever going to carry in our brains. As children, we may develop new neurons to help create the pathways, known as neural circuits, which function as information highways between different regions of the brain. However, scientists believed that after a neural circuit was created, developing any new neurons could interrupt the flow of information and disable the brain’s communication system. �
Introduction to Brain Basics
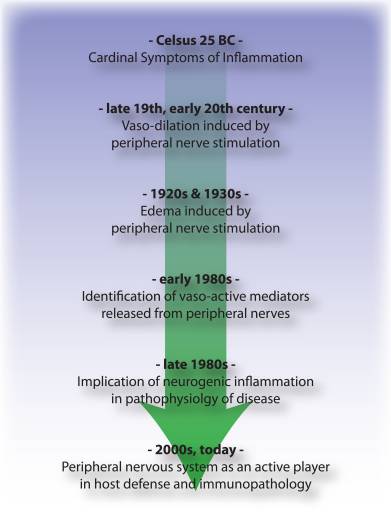
In 1962, scientist Joseph Altman questioned this belief when he saw evidence of neurogenesis, or the birth of neurons, in a region of an adult rat’s brain known as the hippocampus. He then reported that newborn neurons migrated from their birthplace in the hippocampus to other regions of the brain. In 1979, another scientist, Michael Kaplan, proved Altman’s findings in the rat brain and in 1983, Kaplan found neural precursor cells in the forebrain of an adult monkey. �
In the early 1980s, a scientist attempting to explain how birds learn how to sing suggested that neuroscientists should once again analyze neurogenesis in the adult brain and start to determine how it can make sense. In several experiments, Fernando Nottebohm and his team revealed that the numbers of neurons in the forebrains of male canaries tremendously increased during the mating season. This was the same time in which the birds had to learn new songs to attract females. �
However, why did these bird’s brains create new neurons during such a vital time in learning? Nottebohm believed it was because new neurons helped keep new song patterns inside the neural tissues of the forebrain, or the region of the brain which regulates complex behaviors. These new neurons made learning possible. If birds developed new neurons to help them remember and learn new song patterns, Nottebohm believed that the brains of mammals may also be able to do the same. �
Elizabeth Gould discovered evidence of newborn neurons in a different region of the brain in monkeys. Fred Gage and Peter Eriksson also demonstrated that the adult human brain developed new neurons in a similar region. For several neuroscientists, neurogenesis in the adult brain is still an unproven theory. However, other neuroscientists believe that the evidence provides interesting possibilities associated with the role of adult-generated neurons in memory and learning. �
Architecture of the Neuron
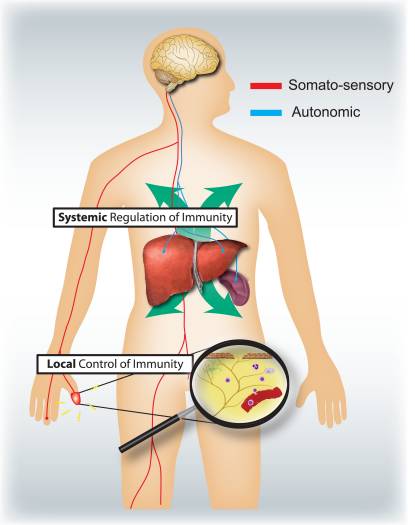
The central nervous system, which includes the brain and the spinal cord, consists of two primary types of cells: the neurons and the glia. Glia outnumber neurons in several regions of the brain, however, neurons are the key structures in the brain. Neurons are information messengers. They utilize electrical impulses and chemical signals to transfer information between different regions of the brain and between the brain and the rest of the nervous system. Everything we think, feel, and do would be impossible without the utilization of neurons and the glial cells, known as astrocytes and oligodendrocytes. �
Neurons have three primary parts including a cell body and two extensions known as an axon and a dendrite. Within the cell body is a nucleus, which regulates the cell’s activities and holds the cell’s genetic material. The axon is characterized by a very long tail and it transfers messages from the cell. Dendrites are characterized similar to that of the branches of a tree and they receive messages from the cell. Neurons communicate with one another by sending chemicals, known as neurotransmitters, across a very small region, known as a synapse, found between the axons and the dendrites of adjacent neurons. � There are three types of neurons: �
- Sensory neurons: Transfer information from the sense organs, such as the eyes and ears, to the brain.
- Motor neurons: Manage voluntary muscle activity and transfer messages from nerve cells in the brain to muscles.
- All other neurons are known as interneurons.
Scientists believe that neurons are the most varied type of cell in the human body. Within these three types of neurons are hundreds of different types of neurons, each with specific message-carrying abilities. The way these neurons communicate with one another by establishing connections is ultimately what makes people unique in how we think, feel, and act. �
Birth of the Neuron
The range to which new neurons are created in the brain has been a controversial topic among neuroscientists for many years. Meanwhile, although nearly all neurons are currently present in our brains by the time we’re born, there’s recent evidence to support that neurogenesis, or the scientific word utilized to describe the birth of neurons, is a lifelong procedure. Neurons are born in regions of the brain which are full of neural precursor cells, known as neural stem cells. These cells have the potential to develop all, if not all, of the different types of neurons and glia found in the brain. Neuroscientists have discovered how neural precursor cells function in the laboratory. Although this may not be exactly how these cells behave when they are in the brain, it gives us data about how they may function when they are in the brain’s environment. �
The science of stem cells is still very recent and could ultimately change with further discoveries, however, researchers have discovered enough evidence to support as well as to be able to demonstrate how neural stem cells create the other cells of the brain. Neuroscientists refer to this as a stem cell’s lineage and it is similar in principle to the concept of a family tree. �
Neural stem cells increase by dividing into two and creating two new stem cells, two early progenitor cells, or one of each. When a stem cell divides to create another stem cell, it is believed to self-renew. This new cell has the potential to make more stem cells. When a stem cell divides to create an early progenitor cell, it is said to differentiate. Differentiation is when a new cell is more technical in structure and function. An early progenitor cell doesn’t have the potential of a stem cell to create several different types of cells. It can only make cells within their distinct lineage. Early progenitor cells may self-renew or go in either of two ways. One type will develop astrocytes. The other type will develop neurons or oligodendrocytes. �
Migration of the Neuron
Once a neuron is born, it must go to the region of the brain where it will function. But, how does a neuron understand where to go? And, what helps it get there? Neuroscientists have determined that neurons utilize two different methods to travel: �
- Several neurons migrate by following the long fibers of cells known as radial glia. These fibers extend from the inner layers to the outer layers of the brain. Neurons glide along the fibers until they reach their destination.
- Neurons also travel by using chemical signals. Scientists have found special molecules on the surface of neurons, known as adhesion molecules, which bind with similar molecules on nearby glial cells or nerve axons. These chemical signals will also ultimately help guide the neuron to its final destination in the brain.
Not all neurons are successful in their journey. Scientists believe that only one-third of these neurons will reach their destination. Some cells die during the process of neuronal growth. Some neurons may also survive, but end up where they don’t belong. Mutations in the genes which regulate migration create regions of misplaced or abnormal neurons which can cause disorders, such as epilepsy. Scientists believe that schizophrenia is partially caused by misguided neurons. �
Differentiation of the Neuron
When a neuron reaches its destination, then it must begin to perform its initial function. This final measure of differentiation is one of the most misunderstood sections of neurogenesis. Neurons are in charge of the transfer and uptake of neurotransmitters, or chemicals which deliver information between cells. Depending on its location, a neuron may perform the role of a sensory neuron, a motor neuron, or an interneuron, sending and receiving specific neurotransmitters. �
In the developing brain, a neuron depends on molecular signals from other cells, including astrocytes, to determine its form and location, the type of transmitter it creates, and to which other neurons it can connect. These newborn cells establish neural circuits, or data pathways that connect from neuron to neuron, which is determined during adulthood. However, in the mature brain, neural circuits are already developed and neurons must find a way to fit in. As a new neuron settles in, it starts to look like enclosing cells. It then develops an axon and dendrites and begins to communicate with its neighbors. �
Death of the Neuron
Although neurons are the longest living cells within the human body, large numbers of them often die during migration and differentiation. The lives of some neurons can sometimes take unexpected turns. Several health issues associated with the brain, the spinal cord, and the nerves are the consequence of the unnatural deaths of neurons and supporting cells. �
- In Parkinson’s disease, neurons which create the neurotransmitter dopamine die off at the basal ganglia, a region of the brain which controls body movements. This causes difficulty initiating movement.
- In Huntington’s disease, a genetic mutation causes the over-production of a neurotransmitter known as glutamate, which kills neurons in the basal ganglia. As a result, individuals twist and writhe uncontrollably.
- In Alzheimer’s disease, unusual proteins build up in and around neurons in the neocortex and hippocampus, sections of the brain which manage memory. When these neurons die, people lose their ability to remember and perform regular tasks. Physical damage to the brain and other regions of the central nervous system can also kill nerves.
Injury to the brain, or damage caused by a stroke, can kill nerves completely or gradually starve them of the oxygen and nutrients they need to survive. Spinal cord injury may disrupt communications between the brain and nerves when these lose their link to axons located under the site of injury. These neurons survive but they may lose their ability to communicate. �
Conclusion to Brain Basics
Scientists hope that by understanding more about the life and death of neurons, they could develop treatment options and perhaps even cures for brain diseases and disorders which ultimately affect the lives of many people in the United States. �
The most current research studies suggest that neural stem cells can generate many, if not all, of the several types of neurons located in the brain and the nervous system. Determining how to control these stem cells from the laboratory into specific types of neurons can develop a new supply of brain cells to replace the ones which have been damaged or died. �
Treatment approaches may also be created to take advantage of growth factors and other signaling mechanisms within the brain which tells precursor cells to make new neurons. This will make it easy to fix, reshape, and renew the brain from within. �

A neuron is characterized as a nerve cell which is considered to be the basic building block of the central nervous system. Neurons are similar to other cells in the human body, however, neurons are responsible for transferring and transmitting information throughout the human body. As previously mentioned above, there are also several different types of neurons which are in charge of a variety of functions. Understanding the life and death of neurons is essential to help understand the mechanisms of neurological diseases and hopefully their treatment and cure.� – Dr. Alex Jimenez D.C., C.C.S.T. Insight
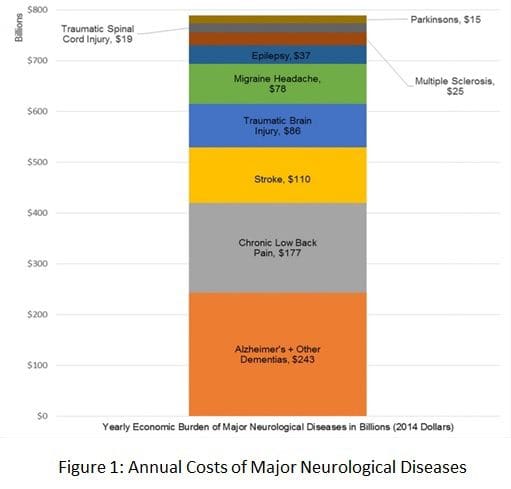
The purpose of the article is to understand the life and death of neurons and how these relate with neurological diseases. Neurological diseases are associated with the brain, the spine, and the nerves. The scope of our information is limited to chiropractic, musculoskeletal and nervous health issues as well as functional medicine articles, topics, and discussions. To further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900 . �
Curated by Dr. Alex Jimenez �
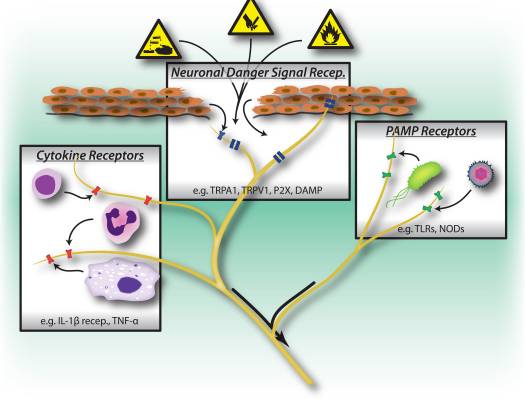
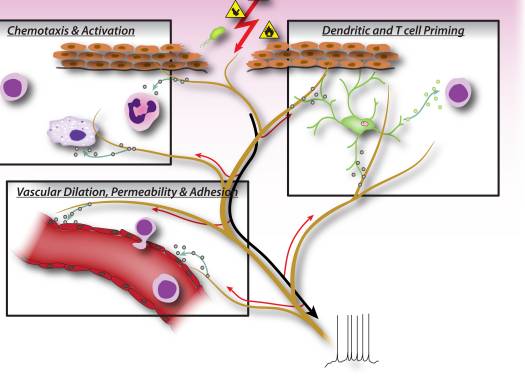
Additional Topic Discussion: Chronic Pain
Sudden pain is a natural response of the nervous system which helps to demonstrate possible injury. By way of instance, pain signals travel from an injured region through the nerves and spinal cord to the brain. Pain is generally less severe as the injury heals, however, chronic pain is different than the average type of pain. With chronic pain, the human body will continue sending pain signals to the brain, regardless if the injury has healed. Chronic pain can last for several weeks to even several years. Chronic pain can tremendously affect a patient’s mobility and it can reduce flexibility, strength, and endurance.
Formulas for Methylation Support
XYMOGEN�s Exclusive Professional Formulas are available through select licensed health care professionals. The internet sale and discounting of XYMOGEN formulas are strictly prohibited.
Proudly,�Dr. Alexander Jimenez makes XYMOGEN formulas available only to patients under our care.
Please call our office in order for us to assign a doctor consultation for immediate access.
If you are a patient of Injury Medical & Chiropractic�Clinic, you may inquire about XYMOGEN by calling 915-850-0900.
For your convenience and review of the XYMOGEN products please review the following link.*XYMOGEN-Catalog-Download �
* All of the above XYMOGEN policies remain strictly in force. �
�







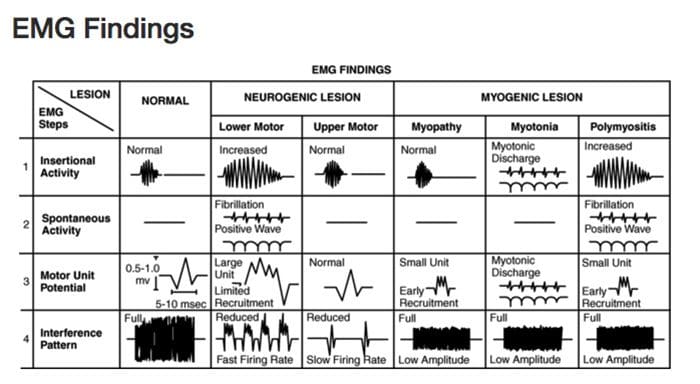 Diagnostic Needle EMG
Diagnostic Needle EMG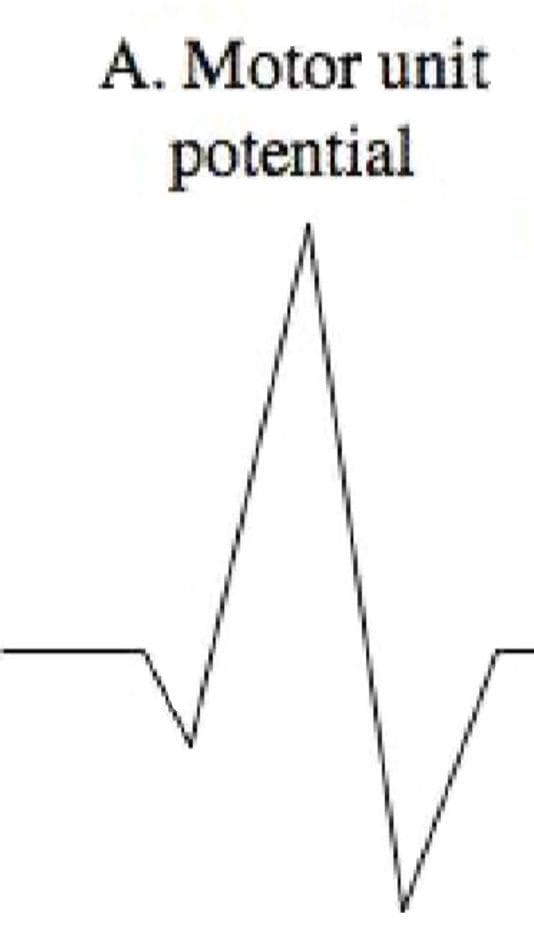 Polyphasic MUPS
Polyphasic MUPS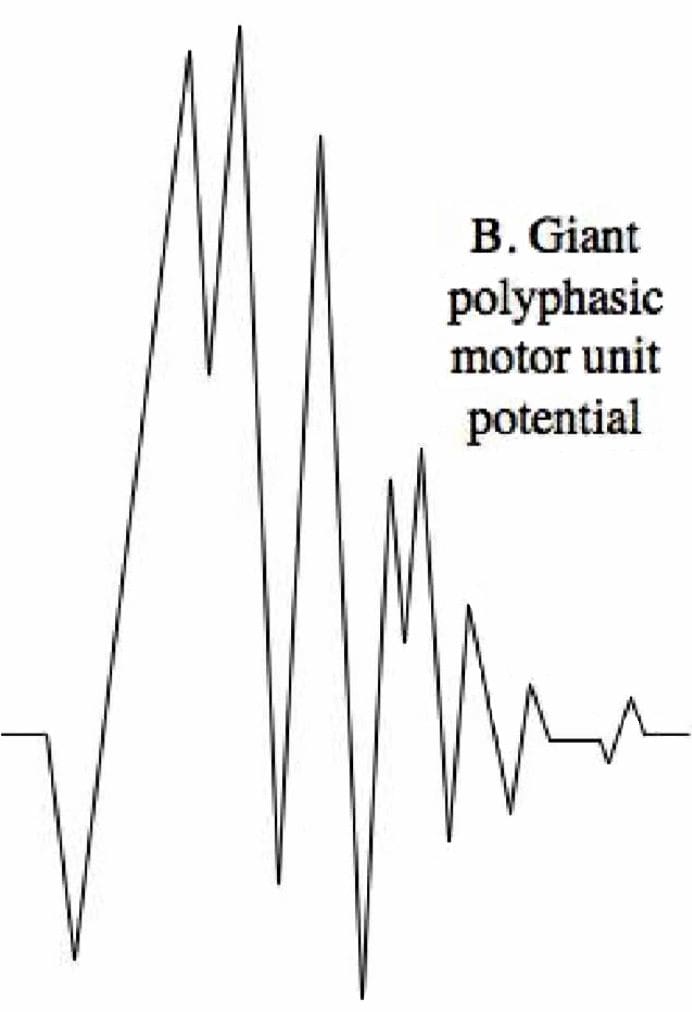 Complete Potential Blocks
Complete Potential Blocks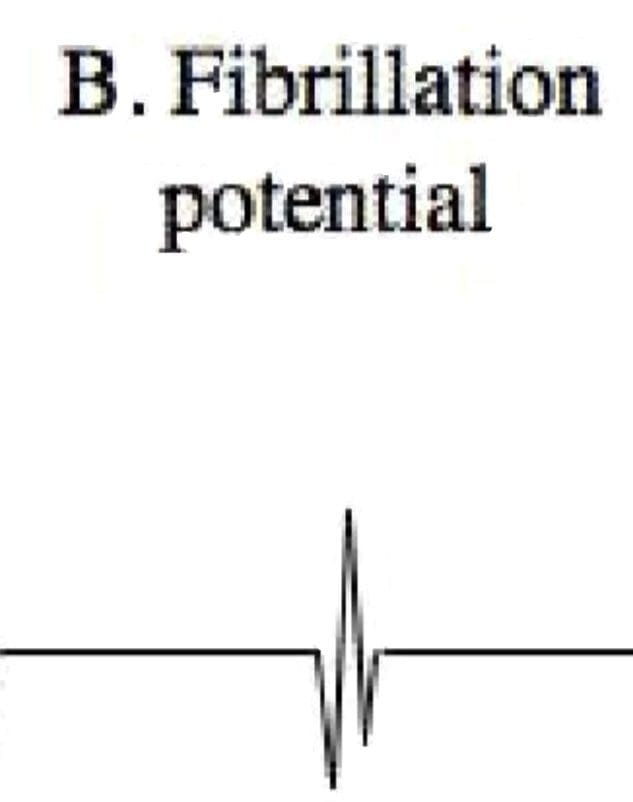 Positive Sharp Waves
Positive Sharp Waves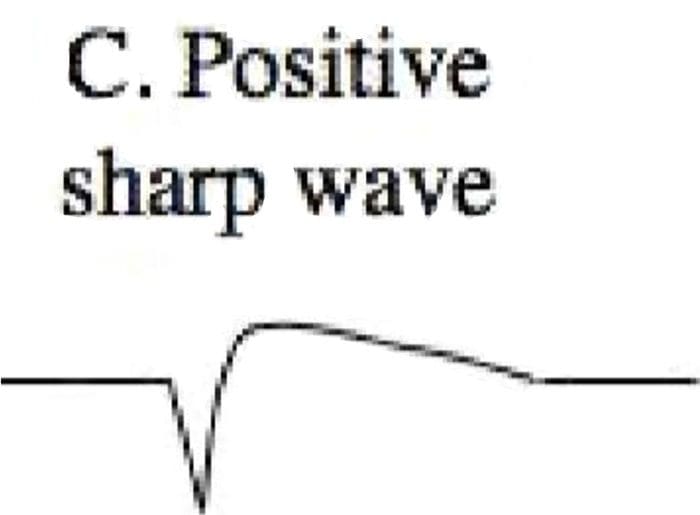 Abnormal Findings
Abnormal Findings