Chronic Back Pain
Back Clinic Chronic Back Pain Team. Chronic back pain has a far-reaching effect on many physiological processes. Dr. Jimenez reveals topics and issues affecting his patients. Understanding the pain is critical to its treatment. So here we begin the process for our patients in the journey of recovery.
Just about everyone feels pain from time to time. When you cut your finger or pull a muscle, pain is your body’s way of telling you something is wrong. Once the injury heals, you stop hurting.
Chronic pain is different. Your body keeps hurting weeks, months, or even years after the injury. Doctors often define chronic pain as any pain that lasts for 3 to 6 months or more.
Chronic back pain can have real effects on your day-to-day life and your mental health. But you and your doctor can work together to treat it.
Do call upon us to help you. We do understand the problem that should never be taken lightly.
by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chiropractic, Chronic Back Pain, Integrative Functional Wellness, Integrative Medicine, Wellness
If It Sounds Too Good to Be True�
When you�re in pain, you might try just about anything to feel better. Claims of miracle cures that instantly relieve back and neck pain are tempting, but they often fall short of their promises.
Save your money and steer clear of the products featured promising to eliminate your spine-related pain.
Copper Bracelets

Copper bracelets and wristbands have attracted a following of arthritis sufferers because of their perceived ability to reduce joint pain.
The key word here is perceived.
A 2013 study in the UK examining the effects of copper bracelets in patients with rheumatoid arthritis found no difference in pain outcomes between those wearing copper bracelets and those using a placebo.
While the bracelets won�t do you any harm, they�re more for looks than clinical benefit. There�s no solid medical evidence available proving they reduce pain or inflammation.
Magnets
From magnetic shoe inserts to bandages, magnets have been heavily marketed as a miracle cure to zap away a variety of back pain conditions, including fibromyalgia and arthritis. However, no proof exists to back up magnets� health claims.
While studies have examined magnets� impact on pain, the results are mixed�and the quality of some of the research is questionable. Additionally, magnets are not safe for some people, including those who use pacemakers or insulin pumps.
Colloidal Silver
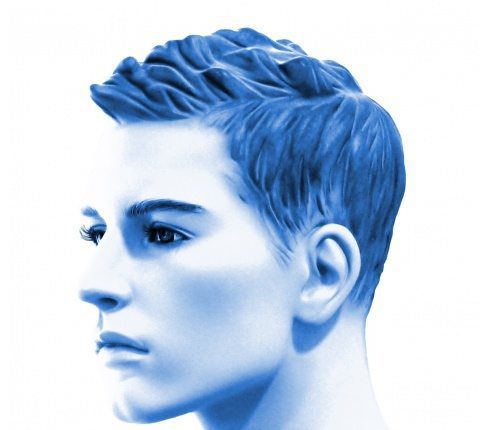
Silver jewelry? Classic. Silver home furnishings? Sure thing. Colloidal silver for your spine pain? Never a good idea.
Colloidal silver for back pain is typically found as a topical cream containing small particles of silver. In 1999, the U.S. Food and Drug Administration (FDA) recommended that people not use colloidal silver to treat any medical condition because it�s neither safe nor effective.
Even worse than the false claims of back and neck pain relief are colloidal silver�s strange and serious side effects. This product can interfere with the absorption of some prescription drugs and even permanently tint your skin a blue-gray color.
DMSO and MSM Dietary Supplements

If you have spondylosis (osteoarthritis), you may have heard of the dietary supplements dimethyl sulfoxide (DMSO) and methylsulfonylmethane (MSM). Some believe this pair of supplements can block pain and inflammation, but no real medical evidence shows these substances actually relieve painful arthritis symptoms.
Instead of eliminating your arthritis pain, MSM and DMSO might cause some unwanted side effects. Both have been linked to causing upset stomach and skin rashes, while DMSO may also leave you with garlic breath and body odor.
A Word on Drug-Supplement Interactions

Speaking of supplements, it�s important to understand that dietary supplements may not mix with over-the-counter or prescription drugs. Some interactions result in mild side effects, but others can be much more serious�even life-threatening.
If you�re using a dietary supplement�even if it�s a seemingly benign herbal or vitamin�always let your doctor and pharmacist know before taking it with an over-the-counter or prescription medication. They will share any dangerous interactions, and ensure you�re safely addressing your back and neck pain.
The Real Deals: Alternative Treatments that Work
Many who fall prey to the products listed in this slideshow have an interest in alternative or complementary therapies for back and neck pain. While some non-traditional treatments should be avoided, many have been proven to reduce spine pain.
Scientists from the National Center for Complementary and Integrative Health at the National Institutes of Health reviewed 105 U.S.-based trials from the past 50 years that included more than 16,000 participants. They found the therapies below effective at controlling pain:
� Acupuncture � Massage � Relaxation techniques � Tai chi
If you prefer alternative methods to manage for your spinal condition, explore the therapies above. They are effective, safe, and will help you live a healthier life.

Call Today!
by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chronic Back Pain, Lower Back Pain, Mobility & Flexibility
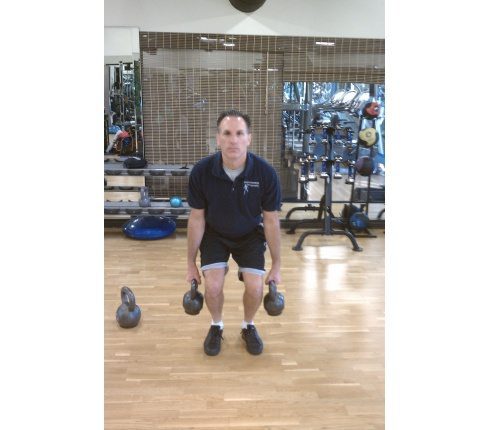
Kettlebells Strengthen the Spine
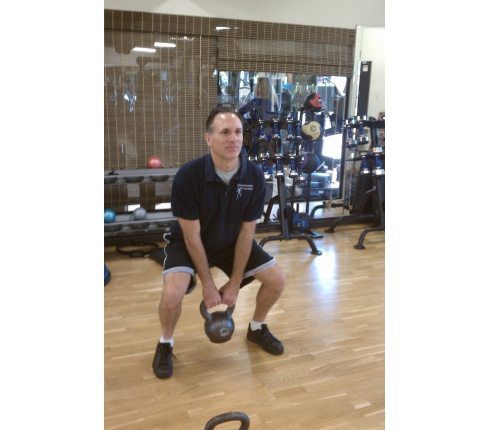
Strengthening the spinal muscles is essential for health and fitness. Functional kettlebell training is resistance training that strengthens the spine. Kettlebell training is an extremely effective type of exercise to increase functional strength, ballistic power, endurance, and flexibility in the entire body, especially the spinal and core muscles.
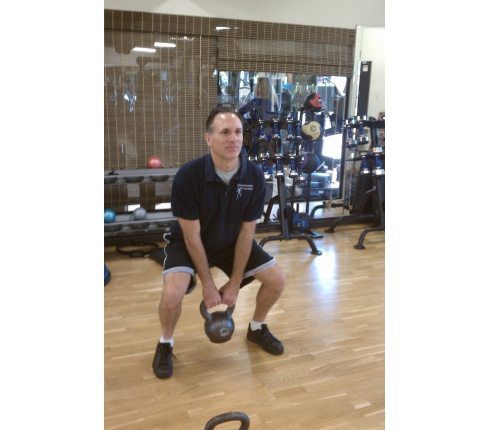
(Exercise shown is Anchor Squats.)
What Exactly Are Kettlebells?
Kettlebells are round cast iron weights with a single handle. Picture a cannonball with a u-shaped handle. Kettlebells are manufactured in a wide range of weights, for all strength levels.

Muscles Used in Kettlebell Training
Kettlebell training incorporates large functional movements. Multiple muscle groups work in synergy to complete the exercises. The spinal muscles function as either the primary mover or assist the primary mover in every kettlebell exercise. The spinal muscles also stabilize the body during functional kettlebell training, thus developing the smaller supporting structures.
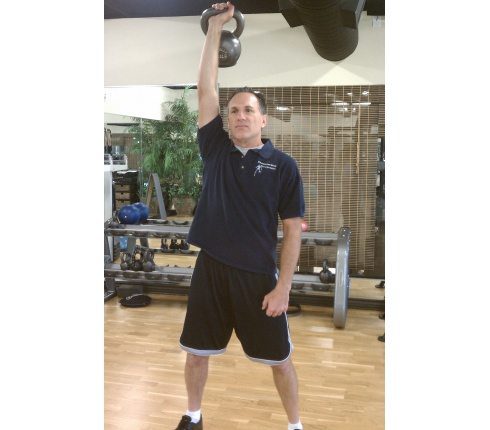
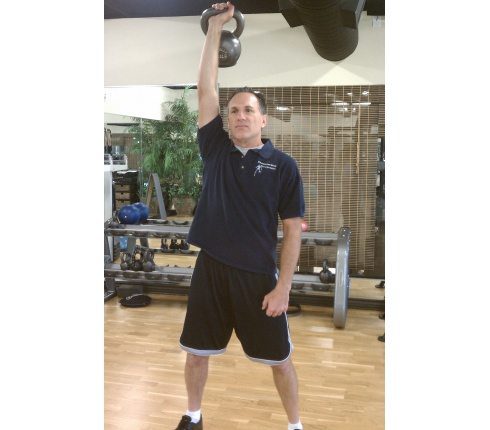
(Exercise shown is Push Press.)
High Reps Of High Importance In Kettlebell Training
Kettlebell training employs high repetitions, momentum, and centrifugal force. Momentum works the spinal muscles as the weight is raised and lowered. High repetitions combined with momentum and full body movement build strength and endurance in the entire musculoskeletal and cardio-vascular systems. Kettlebell training delivers aerobic and anaerobic benefits.

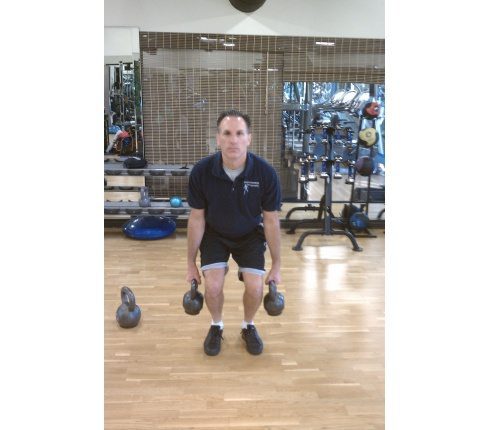
(Exercise shown is High Pulls.)
Always Learn From A Qualified Kettlebell Instructor
Perfect technique is mandatory during exercise. Correct exercise technique maximizes benefit and lowers injury risk. Poor exercise form increases the possibility of injury and diminishes results. Kettlebell exercises are learned motions, so you should learn proper training technique from a qualified kettlebell trainer. The trainer should demonstrate, instruct, and supervise your training and develop your routine.

(Exercise shown is Turkish Get-up.)
So Many Possibilities
The kettlebell�s shape allows for a wide variety of exercises. This resourceful exercise tool is used for basic exercises like squats (shown in slide 1), cleans, swings, high pulls (shown in slide 4), snatches and push presses (shown in slide 3). The versatility of the kettlebell is demonstrated with exercises such as renegade rows (a combination of push-ups and rows�shown in slide 6), suitcase swings, woodchoppers (a combination of lunges and oblique twists), windmills, and Turkish get-ups (shown in slide 5)

(Exercise shown is Renegade Rows.)
Kettlebell’s Benefits For The Spine
Functional kettlebell training is a rare type of exercises that increases aerobic and anaerobic health simultaneously. The benefits to the spine include increased strength, power, endurance, flexibility, function and mobility.
(Exercise shown is Suitcase Swings.)

Call Today!

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chiropractic, Chronic Back Pain, Migraines, Neck Pain
You get up with it. You go to sleep with it. An incredible number of men and women live with chronic back or neck pain every day. What’s chronic pain? It is technically defined as pain that lasts for 12 weeks or more�even after pain isn’t any longer acute (short-term, serious pain) or the injury has healed.
Accurate Analysis
Getting an exact identification of the reason for neck pain or your back is vital to the outcome of your treatment plan. Depending on the severity and cause of your pain that is chronic, you might need to find out different specialists in addition to your own primary care physician�pain medicine specialist, orthopaedic spine surgeon, neurosurgeon, physiatrist, rheumatologist, physical therapist among others. Over time your chronic pain need to be reevaluated, and may transform, which might affect the way it is handled.
Your chronic back or neck pain treatment generally features a variety of treatments to maximize results that are great. A number of the treatments your doctor prescribes and recommends may include:
Physical Therapy:
Extending and strengthening muscles is vital in the treatment of neck pain or chronic back.
Chiropractic Care:
Depending on your own diagnosis, chiropractic care may be recommended by your doctor. Studies have demonstrated that two weeks of day-to-day exploitation by a chiropractor can result in considerable progress in a few patients with persistent low back pain and referred leg pain.

Medicines:
There are lots of different prescription medications to take care of neuropathic pain, inflammation, muscle spasms, and pain. Additionally, you will find drugs to treat conditions that often accompany chronic pain, including drugs that will help you sleep, alleviate depression, and reduce nervousness.
Processes:
Your doctor may recommend a spinal cord stimulator, spinal injections, drug heart, or spine surgery. You can get a second opinion, in the event you might be uncertain about the treatment plan recommended.
Coping skills:
Never underestimate the power of your head. Your mood and mental perspective can greatly make an impact on your level of pain. Talk with a trained specialist to understand relaxation and coping skills.
Complementary Treatments:
Many physicians recommend acupuncture and other types of traditional Chinese medicine. Speak to your doctor about these choices.
A couple of words about …. age, fitness, body weight
You probably involve some control over body weight and your level of fitness, although you can�t stop aging or its effects. While you can�t stop the clock on the cellular changes that are recognized to accompany aging�such as loss of muscle mass and bone density �you can take little steps today to build a more stronger�you tomorrow.
It�s understood that patients with chronic back or neck pain may not feel like being active, going to the gym and even adhering to a home exercise program. Yet, being active can help chronic pain because during exercise your body releases endorphins�your body�s natural painkiller.
Moreover, by teaming up together with and/or your physician physical therapist you can start to build abdominal muscles that are strong �essential to your own body�s center strength which helps support your back.
Did you know that by simply losing even 5 to 10 pounds you can reduce back pain? It�s true. Carrying around extra weight translates to added stress to the low back that may exacerbate pain.
Conclusion
In many instances, aggressive and early treatment of chronic back or neck pain can make a life-changing difference. But remember that knowledge is power: Be certain you comprehend your alternatives before deciding which route to take.

Call Today!
by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chiropractic, Chronic Back Pain, Lower Back Pain
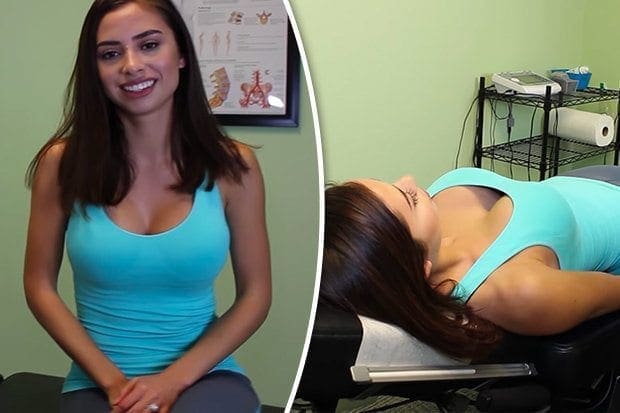
Viewers can�t get enough of the informative clip that sees a chiropractor helping a patient suffering from lower back pain.�Dr Jeffrey Gerdes of the ChiroCare and Rehab centre based in North Carolina, US, talks his way through the demonstrationHis patent tells him: �I�m getting excruciating pains in my back and they�re very instant and they�re immobilising.�It�s so excruciating that I have to stop for a second and re-coup so I�m not sure what�s happening.� The doctor asks her to lie on her side and gently cracks her back.
CRACKING:
But the sound that emerges leaves him stunned. �Wow, gosh that was loud,� Dr Jeffrey says.Viewers can�t get enough of the footage, with more than 876,000 people watching the clip on the chiropractor�s YouTube channel.But many seem to have been distracted more by the stunner getting treatment than the actual techniques involved.�Well, did anyone else manage to take any of that in?� one viewer said.


Call Today!

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chronic Back Pain, Injury Care, Posture, Wellness
Ergonomics is a scientific discipline that’s been in existence for many years. Keeping their work environments safe and efficient and traditionally concerned with factory workers, ergonomic professionals have expanded their work to include all types of workers from laborers to seniors to office workers & students.
In addition, it looks for means to adjust our environment to lower the risks of illness and harm, enhance productivity, and improve the caliber of our work life.
The Goals of Ergonomics
The profession of ergonomics has two main concentrations (which frequently overlap):
1. Industrial ergonomics – occasionally called work-related biomechanics – is concerned with the physical aspects of work including force, position, and repetitive movements.
2. Human factors ergonomics looks as the psychological features of work like mental anxiety and decision-making.
The aims of ergonomics contain the following:
- Reduce work-related injury and illness
- Help include workers’ compensation costs for companies
- Enhance the standard of work
- Reduce absenteeism
- Help companies comply with government regulations regarding work surroundings
Ergonomics professionals include:
- Engineers
- Security professionals
- Industrial hygienists
- Physical therapists
- Occupational therapists
- Nurse practitioners
- Chiropractors
- Occupational doctors
How Ergonomics Enhances Work & Safety
The association between work injury and illness is old. It is even believed that Ancient Man concerned himself with developing the right tools that allowed for the efficiency and least amount�of distress.
Now, we continue to look for ways to boost the relationship between our “tools” and�our jobs. One means to do that is to look at the risk factors in the workplace. These are able to be divided into 3 areas: physical characteristics, environmental features, and workplace hazards.
1. Physical Characteristics Of Work:
- Bearing
- Drive
- Repetition
- Duration
- Recovery time
- Velocity/acceleration
- Heavy exertion that is dynamic
2. Segmental Vibration Environmental Characteristics Of Work:
- Heat
- Cold
- Lighting
- Sound
- Entire body vibration
3. Workplace Dangers:
- Physical pressure
- Mental pressure
- Workload
- Hours (shifts, overtime)
- Slips and falls
- Fire
- Exposure hazards (electrical, chemical, biological, radiation)

Call Today!

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chiropractic, Chronic Back Pain, Spine Care
Living with chronic back or neck pain can lead to depression, feelings of worry, nervousness, hopelessness, as well as other mental health-associated symptoms. Your pain medicine physician or your back specialist may refer you to a psychologist or psychiatrist. Referring you doesn�t mean your physician believes your pain is all in your mind! Rather, he/she is taking an optimistic step in treating you as a whole individual � by treating both the physical and psychological pain.
Chronic Neck &�Back�Pain Is Complicated
As someone living with chronic pain caused spondylosis, degenerative disc disease, spinal cord injury or some other back problem, you understand pain is a complicated issue, and treatment requires the expertise of a spine�specialist. Perhaps your pain management plan features a blend of treatments � medication for neuropathic pain, a periodic epidural spinal shot, a muscle relaxant, or physical therapy. Treatment of stress, nervousness, and depression (there are various types) needs the same level of expertise but from somebody who focuses on managing mental health problems.
Depression & Chronic Pain
Are you aware that depression and chronic pain often go together? Depression is a critical condition, and nothing to be embarrassed of. It has been reported that as many as 50% of individuals with chronic pain are depressed.1 So, if you are depressed, you’re far from being alone.
The signs and symptoms of depression can manifest themselves differently in each individual, but tiredness, sleep disruption, changes in eating habits, listlessness, and feelings of hopelessness are all quite common. Aches and pains are a very common symptom of depression notably, depression can lead directly to neck and long-term back pain.
Treating Depression & Pain
Two classes of antidepressants often used to treat depression in those that experience chronic pain are selective serotonin reuptake inhibitors (SSRIs) and serotonin and norepinephrine reuptake inhibitors (SNRIs). Generally prescribed SSRIs include and fluoxetine (Prozac) and sertraline (Zoloft), whereas usually prescribed SNRIs include duloxetine (Cymbalta) and venlafaxine (Effexor). These drugs have now been demonstrated to be effective and safe for handling depression in the context of continual pain, but like all medicines, they come with some risk of unwanted effects. As always, be sure to go over these drugs in detail together with your physician before beginning any treatment regimen that includes them, and inform your physician of all of the medicines (including over the counter medicines), herbal remedies, and nutritional supplements you’re currently taking so as to avoid any negative drug interactions.
Moreover, or in addition to medications, other types of treatment may include:
- Talk therapy, more officially called cognitive behavioral therapy (CBT). The focus of CBT is to help the individual manage their situation and may include learning how to problem solve, thus engaging the individual to alter specific thought patterns to your more positive outlook, and conquering�fears.
- Practice relaxation techniques such as meditation or breathing exercises.
- Routine exercise might help curb feelings of worry, stress as well as depression. Exercise causes the entire body to release endorphins, which can cause you to feel much better and may reduce pain perception too.

Call Today!
Reference
1. Tartakovsky M. Living with chronic pain and melancholy. PsychCentral.com. http://psychcentral.com/lib/living-with-chronic-pain-and-depression/. Got July 30, 2015.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chiropractic, Chronic Back Pain, Spine Care
Pain in the upper and/or mid back is not as common than lower back or neck pain. The upper back is called the thoracic spinal column, and it is the most secure part of the spine. The reach of movement in the upper back is limited because of the backbone�s attachments to the ribs (rib cage).
Upper back pain is generally caused by soft tissue injuries, like sprains or strains, muscle tension caused by bad posture, or looking downward for long time spans (eg, texting, mobile phone use).
- Pain
- Tightness
- Stiffness
- Muscle spasm
- Tenderness to touch
- Headache
What causes or leads to upper back pain?
An episode of upper back pain can be actuated by distinct moves and actions, including:
- Twisting
- Excessive bending
- Whiplash or alternative neck injury
- Lifting improperly
- Poor muscle tone
- Persistent movements, overuse
- Contact sports
- Carrying a load that is heavy
- Smoking
- Being overweight
Poor posture�working at the computer for�a long time without taking a break to walk around and extend, or in general can promote upper back pain. Both muscle fatigue and muscle pull, which often result from poor posture, can trigger the pain.
So what can I do about it?
Usually, upper back pain is not a cause for worry; however, it can be uncomfortable, painful, and inconvenient. Also, if pain develops suddenly and is serious�such as from an injury (eg, fall)�and, certainly if pain and symptoms (eg, weakness) progressively worsen you should seek medical attention.
Generally, the next home treatments can help relieve back pain that is upper.
- Short term rest
- Mild�Stretches
- Over the counter medicine, for example ibuprofen, (Motrin�), naproxen sodium (Aleve�), or acetaminophen (Tylenol�). Take with food, and don’t take more than the recommended dose.
- Use a cold pack that is commercially available or fill a plastic bag with ice and seal it wrap it. Apply to the painful area for 20 minutes every 2-3 hours for the first 2 to 3 days.
- Heat (after the very first 72 hours). After using moist heat, gently stretch the muscles to enhance mobility and alleviate stiffness.
Your physician may prescribe drugs, like a muscle relaxant or perform trigger point injections to greatly help break up muscle spasms. He or she may also recommend physical therapy to increase flexibility, mobility and alleviate pain. Other treatments your doctor may suggest include acupuncture and chiropractic care.
Most cases of upper back pain resolve in 1 to 2 weeks without additional treatment. When you’re able to perform them without pain restart your regular activities slowly. Don�t rush matters, however: you could interfere with your healing and risk reinjury.
As always, abrupt or severe pain ought to be dealt with promptly.

Call Today!
Composed by Stewart G. Eidelson, MD