Individuals who have experienced spinal or back trauma, suffered fractures, are going through spinal degeneration, or are dealing with a spinal condition have an increased risk of anterolisthesis, where a vertebra slips forward relative to the vertebra below it. Can healthcare providers help prevent and treat the condition?
Contents
Anterolisthesis
The spine consists of 33 individual bones or vertebrae stacked on one another. Anterolisthesis occurs when one vertebral segment slips forward over another. The condition can be mild, asymptomatic, or cause significant pain and neurological symptoms. Many different things, including osteoarthritis, osteoporosis, trauma, or a fracture, can cause this vertebral shifting. (Cedars Sinai, 2022) Spondylolisthesis is a general term for shifting a spinal vertebra over the one below it. It includes anterolisthesis, forward moving, and the less common retrolisthesis, or backward shifting.
Grades
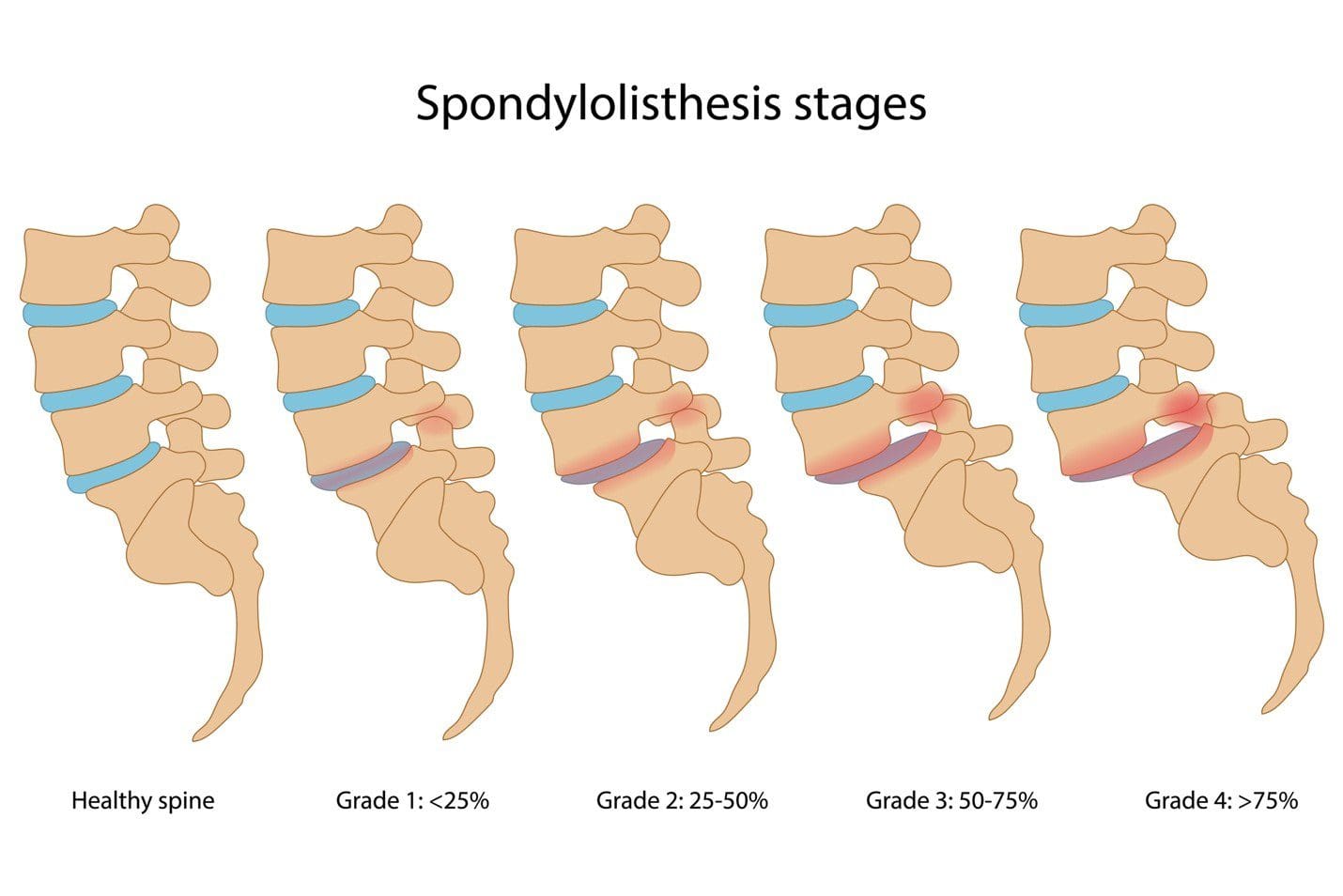
Anterolisthesis is typically graded using the Meyerding scale, which assigns one of five grades according to how much slippage has occurred. These grades include:
Grade 1
- 0 to 25% slippage
Grade 2
- 25 to 50% slippage
Grade 3
- 50 to 75% slippage
Grade 4
- 75 to 100% slippage
Grade 5
- More than 100% slippage or spondyloptosis
Grade 1 and 2 cases are generally mild, while grades 3, 4, and 5 are more severe. (Koslosky E., and Gendelberg D. 2020)
Symptoms
Anterolisthesis can lead to various symptoms, depending on the severity and if the surrounding spinal nerves have been affected. The most common complaints include:
- Lower back stiffness
- Lower back pain
- Shooting pain into the leg
- Weakness when standing or walking for a long time
- Cramping in the leg muscles
- Numbness or tingling in the leg that improves when sitting or bending forward (American Academy of Orthopaedic Surgeons, 2021)
Causes
Cases of anterolisthesis are also typically categorized based on what led to the condition. The most common causes include:
Degenerative anterolisthesis
- Shifting occurs when arthritis (spondylosis) causes the spine’s joints and discs to deteriorate.
- The degenerative version of the anterolisthesis is the most common, particularly in women and adults over 50.
- African Americans tend to experience this condition at a higher rate than the general population. (American Academy of Orthopaedic Surgeons, 2021)
Isthmic anterolisthesis
- Slippage is caused by a fracture in a portion of the spine called the pars, also known as a pars defect.
Congenital or Dysplastic anterolisthesis
- Slippage is caused by a condition present at birth or spinal abnormality.
Traumatic anterolisthesis
- Acute shifting of the vertebrae caused by a traumatic injury.
Pathologic anterolisthesis
- Anterolisthesis occurs because of a bone disease like osteoporosis.
Iatrogenic – Postsurgical anterolisthesis
- Slippage that occurs as a result of a prior spinal decompression surgical procedure. (Hospital for Special Surgery, 2023)
Diagnosis
Diagnosis begins with a subjective evaluation and a physical examination. During these, the healthcare provider will assess sensation, strength, and reflexes and will order one of several diagnostic tests, including:
X-rays
- Visualizes the vertebrae in the spine and their position relative to those above and below.
- Also provides a clear picture of spinal arthritis or disc degeneration.
Magnetic Resonance Imaging – MRI
- Allows the spinal cord, nerves, muscles, and discs to be assessed for compression or damage.
Computed Tomography – CT scan
- Provides a cross-sectional image of the spine in very clear detail. (American Academy of Orthopaedic Surgeons, 2021)
Treatment
Several factors determine how the condition is treated, including:
- The grade of the slippage.
- The cause.
- The symptoms.
- The presence of instability on a diagnostic test such as an X-ray.
Stable and mildly symptomatic cases are usually treated with a combination that can involve:
- Physical therapy
- Activity modification
- Bracing
- Nonsteroidal anti-inflammatory medications/NSAIDs like ibuprofen.
- Spinal injections
In more severe cases in which spinal instability or significant neurological symptoms are present, surgery may be recommended. This commonly involves a spinal decompression or fusion procedure. The technique varies based on the surgeon’s preferences and anatomy. (Koslosky E., and Gendelberg D. 2020)
Prognosis
Most individuals with this condition don’t know they have it until it is found accidentally on an X-ray or an MRI for something else. Mild cases can cause minimal symptoms and can be well-managed with conservative treatments. Cases of unstable anterolisthesis or those with neurological compression often require surgical intervention. These surgeries restore stability to the spine and alleviate any pressure on the nerves. More than 85% of individuals who need surgery have a successful outcome. (American Academy of Orthopaedic Surgeons, 2021)
Self-Care and Management
For individuals experiencing pain, numbness, or tingling from anterolisthesis, getting symptoms evaluated by a healthcare provider is an important first step. The healthcare provider may suggest one of several management strategies, which include:
Core Strengthening
- To alleviate symptoms, exercises targeting the core muscles in the hips, pelvis, abdomen, and lower back are recommended.
- Formal physical therapy may also be recommended.
Over-the-counter Meds
- A healthcare provider may suggest pain-relieving medications like ibuprofen or naproxen to reduce soreness.
Activity Modification
- Sticking to gentle, pain-free activities and avoiding excessive or repetitive extension of the spine can help prevent symptom aggravation. (American Academy of Orthopaedic Surgeons, 2021)
Injury Medical Chiropractic and Functional Medicine Clinic
At Injury Medical Chiropractic and Functional Medicine Clinic, our areas of practice include Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Wellness & Nutrition, Functional Medicine Treatments, and in-scope care protocols. We focus on what works for you to relieve pain and restore function. If other treatment is needed, individuals will be referred to a clinic or physician best suited to their injury, condition, and/or ailment.
Degenerative Disc Disease Treatment
References
Cedars Sinai. (2022). Anterolisthesis. https://www.cedars-sinai.org/health-library/diseases-and-conditions/a/anterolisthesis.html
Koslosky, E., & Gendelberg, D. (2020). Classification in Brief: The Meyerding Classification System of Spondylolisthesis. Clinical orthopaedics and related research, 478(5), 1125–1130. https://doi.org/10.1097/CORR.0000000000001153
American Academy of Orthopaedic Surgeons. (2021). Adult spondylolisthesis in the low back. https://orthoinfo.aaos.org/en/diseases–conditions/adult-spondylolisthesis-in-the-low-back
Hospital for Special Surgery. (2023). Spondylolisthesis. https://www.hss.edu/condition-list_spondylolisthesis.asp
General Disclaimer, Licenses and Board Certifications *
Professional Scope of Practice *
The information herein on "The Impact of Anterolisthesis on Spinal Health" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and on our family practice-based chiromed.com site, focusing on naturally restoring health for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez, DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card








