Your Pelvic Health: A Guide To Pelvic Floor Physical Therapy
For individuals experiencing pelvis pain symptoms and associated problems, can integrating pelvic floor physical therapy exercises help with treatment and prevention?
Pelvic Floor Physical Therapy
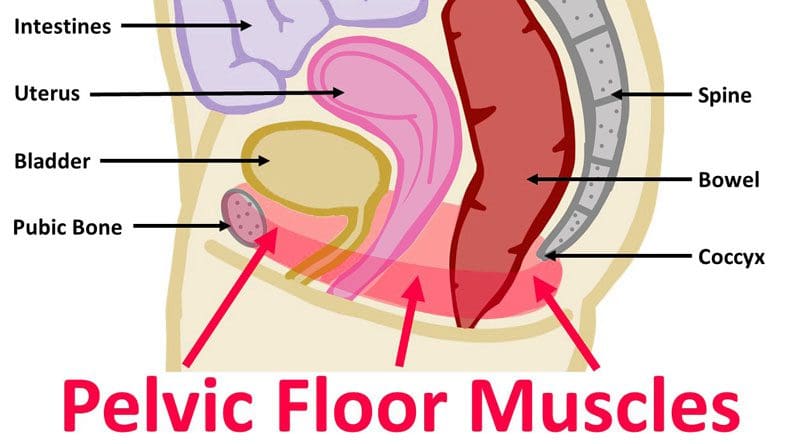
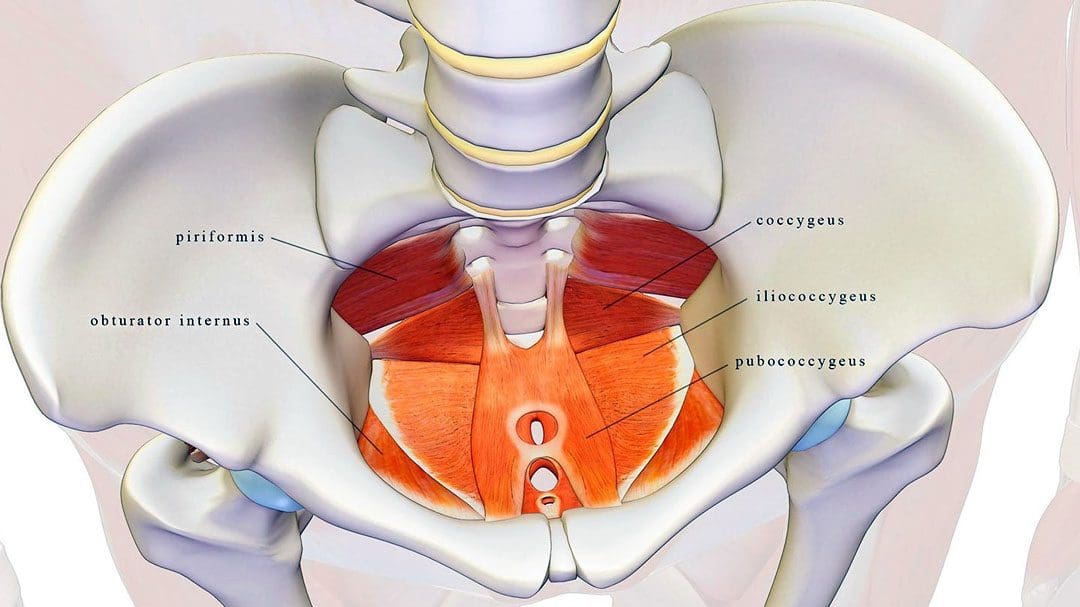
- The pelvic floor muscles are located at the base of the pelvis and protect the pelvic organs like the vagina, cervix, uterus, bladder, urethra, and rectum. (U.S. Food and Drug Administration. 2019)
- They provide posture support, aid in orgasm function, facilitate sphincter function, and help pump lymphatic blood. (Dulcegleika Vilas Boas Sartori, et al., 2021) (Varuna Raizada, Ravinder K. Mittal. 2008)
When the muscles fail to function correctly, individuals can experience symptoms like:
- Painful intercourse
- Prolapse – when an organ or tissue drops or shifts out of place.
- Urinary incontinence
- Constipation problems
- These conditions are common in pregnant individuals or older women.
These symptoms can be treated with pelvic floor physical therapy to alleviate discomfort. Pelvic floor physical therapy can help women and individuals with vaginas:
- Alleviate issues like painful sex, urinary leakage, and prolapse.
- In physical therapy, individuals work on breathing, relaxation, and lengthening and strengthening techniques to train their muscles to function optimally.
Causes of Pelvic Floor Issues
Pelvic floor dysfunction tends to happen with age, during pregnancy, or in combination with events like the postpartum period and menopause, which can lower hormone levels.
- Individuals who are pregnant are especially prone to pelvic floor issues but might not know they have a problem.
- The pregnancy weight of a uterus can pressure and strain the muscles.
- Vaginal childbirth can also stretch or weaken the muscles. (Ilaria Soave, et al., 2019)
Symptoms
Symptoms can include: (Columbia Surgery. 2022)
- Pain in the pelvis region
- Back pain
- Painful urination
- Constipation
- Urinary leakage or incontinence
- Stool leakage or incontinence
- Painful intercourse
- If left untreated, these symptoms can worsen over time.
Pelvic Floor Physical Therapy
An individual will meet with a specialist to discuss symptoms and undergo a physical examination that includes:
- Pelvic floor exam.
- Evaluation of posture, mobility, and core strength.
- Once the initial exams and evaluation are complete, the practitioner will go over pelvic floor exercises and provide a treatment plan.
- Recommended exercises vary based on symptoms but focus on relaxing, stretching, and/or strengthening muscles.
Muscle Relaxation
- To relax the muscles, a therapist may recommend breathing exercises.
- For pregnant individuals, this means timing breaths with contractions.
- For individuals experiencing constipation, breathing exercises can help the body relax and reduce strain.
Stretching Muscles
- Stretching can help relieve muscle tightness and stiffness.
- A therapist may help stretch the pelvic floor through various therapy modalities.
- This type of physical therapy can help loosen tight muscles or help gently reset dislocated organs back into place.
Strengthening Muscles
- After the pelvic floor is loose and relaxed, the focus typically switches to strengthening the muscles.
- Strength work may target abdominal muscles or the pelvic floor muscles themselves.
With time, commitment, and targeted treatment, individuals can use pelvic floor physical therapy to loosen tissues, strengthen muscles, and restore function.
Spinal Decompression In Depth
References
U.S. Food and Drug Administration. (2019). Pelvic organ prolapse (pop).
Sartori, D. V. B., Kawano, P. R., Yamamoto, H. A., Guerra, R., Pajolli, P. R., & Amaro, J. L. (2021). Pelvic floor muscle strength is correlated with sexual function. Investigative and clinical urology, 62(1), 79–84. doi.org/10.4111/icu.20190248
Raizada, V., & Mittal, R. K. (2008). Pelvic floor anatomy and applied physiology. Gastroenterology clinics of North America, 37(3), 493–vii. doi.org/10.1016/j.gtc.2008.06.003
Soave, I., Scarani, S., Mallozzi, M., Nobili, F., Marci, R., & Caserta, D. (2019). Pelvic floor muscle training for prevention and treatment of urinary incontinence during pregnancy and after childbirth and its effect on urinary system and supportive structures assessed by objective measurement techniques. Archives of gynecology and obstetrics, 299(3), 609–623. doi.org/10.1007/s00404-018-5036-6
Columbia Surgery. (2022). Pelvic floor disorders: frequently asked questions.