by Dr Alex Jimenez | Functional Medicine, Gastro Intestinal Health, Gut and Intestinal Health, Health, Wellness
Do you feel:
- That eating relieves fatigue?
- Hormone imbalances?
- Aches, pains, and swelling throughout the body?
- Bodily swelling for no reason?
- Inflammation on your body?
If you are experiencing any of these situations, you might be experiencing inflammation, and it might affect your endocrine system.
Inflammation and the Endocrine System
Inflammation is a defense mechanism in the body. The immune system can recognize the damaged cells, irritants, and pathogens that cause harm to the body and began the healing process. When the inflammation turns into chronic inflammation, it can cause several diseases and conditions in the body and can cause harm to an individual.
Inflammation can cause dysfunction when it is in the endocrine system. The endocrine system is a series of glands that produce and secretes hormones that the body needs and uses for a wide range of functions. When the endocrine glands produce hormones, they are sent into the bloodstream to the various tissues in the body. Once they are in the various tissues, the hormone signals the tissues to tell them what they are supposed to do. When the glands do not produce the right amount of hormones, various diseases like inflammation can affect the body.
Inflammation Symptoms and Causes
Two questions are asked concerning the interaction of the endocrine system with inflammation: How does inflammation influences the endocrine system, and does it influences disease? How do hormones influence inflammation and immune cells? A theory had integrated both questions and has recently been demonstrated in the context of chronic inflammation considering a rheumatic disease.
So how does inflammation influence the endocrine system? Inflammation symptoms can vary depending on if it is acute or chronic. The effects of acute inflammation are summed up by the acronym PRISH. They include:
- Pain: The inflamed area is most likely to be painful, especially during and after touching. The chemicals that stimulate the nerve endings are released, making the area more sensitive.
- Redness: This occurs due to the capillaries in the area that is filled with more blood than usual.
- Immobility: There may be some loss of function in the region of the inflammation where the injury has occurred.
- Swelling: A buildup of fluid causes this.
- Heat: Heat is caused by having more blood flow to the affected area and making it warm to the touch.
These acute inflammation signs only apply to an inflammation on the skin. If the inflammation occurs deep inside the body, like the endocrine system and the internal organs, some of the signs may be noticeable. Some internal organs may not have sensory nerve endings nearby; for example, they will not have pain.
With the effects of chronic inflammation, it is long term and can last for several months or even years. The results from chronic inflammation can be from:
- An autoimmune disorder that attacks normal healthy tissue and mistaking it for a pathogen that causes diseases like fibromyalgia.
- An industrial chemical that is exposed to a low level of a particular irritant over a long period.
- Failure to eliminate whatever was causing acute inflammation.
Some of the symptoms of chronic inflammation can be present in different ways. These can include:
- Fatigue
- Mouth sores
- Chest pains
- Abdominal pain
- Fever
- Rash
- Joint pain
When inflammation affects the endocrine system, it can cause the body’s system to be unbalanced, and it can lead to chronic long term illnesses.
With the second question, it is asking how do hormones influence inflammation and the immune system? When the hormone levels are either too high or too low, it can have several effects on a person’s health. The signs and symptoms can depend on hormones that are out of balance.
Inflammation and Hormones
Research has shown that some of the conditions that are affecting the endocrine system can lead to autoimmune disorders. High levels of hormones can lead to hyperthyroidism, Cushing syndrome, and Graves disease. While low levels of hormones can lead to hypothyroidism and Addison disease. When the levels of the hormones are either too high or too low, the body fluctuates from either weight gain or weight loss and disrupting the glucose levels. This can cause a person to get diabetes and obesity.
Obesity is the main risk factor for type 2 diabetes. During the development of obesity, subclinical inflammatory activity in the tissues are activated and involves the metabolism and energy homeostasis. In the body, intracellular serine/threonine kinases are activated in response to those inflammatory factors. They can catalyze the inhibitory phosphorylation of the key proteins of the insulin-signaling pathway, leading to insulin resistance in the body.
Studies have shown that inflammation is a general tissue response to a wide variety of stimuli. When inflammation is not adequately regulated, inflammatory responses may be exaggerated or ineffective, which can lead to immune dysfunction, recurring infections, and tissue damage, both locally and systemically. With various hormones, cytokines, vitamins, metabolites, and neurotransmitters being key meditators of the immune and inflammatory responses to the endocrine system.
Another study shows that aging, chronic psychological stress, and mental illnesses are also accompanied by chronic smoldering inflammation. Chronic smoldering inflammation in humans is already established with elevations of serum levels, leading to an increase in resting metabolic rate.
Conclusion
So inflammation is a double edge sword where it can heal the body but also cause the body harm if it is deep into the internal organs and body systems. With the endocrine system, the levels of the hormones can fluctuate from going too high or too low and affecting the tissues in the body, causing inflammation. �When an individual is suffering from chronic inflammation, it can change their lifestyle drastically. Some products are here to help counter the metabolic effects of temporary stress and make sure that the endocrine system is supported as well.
The scope of our information is limited to chiropractic, musculoskeletal, and nervous health issues or functional medicine articles, topics, and discussions. We use functional health protocols to treat injuries or disorders of the musculoskeletal system. Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We also make copies of supporting research studies available to the board and or the public upon request. To further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900.
References:
Coope, Andressa, et al. �MECHANISMS IN ENDOCRINOLOGY: Metabolic and Inflammatory Pathways on the Pathogenesis of Type 2 Diabetes.� European Journal of Endocrinology, U.S. National Library of Medicine, May 2016, www.ncbi.nlm.nih.gov/pubmed/26646937.
Felman, Adam. �Inflammation: Causes, Symptoms, and Treatment.� Medical News Today, MediLexicon International, 24 Nov. 2017, www.medicalnewstoday.com/articles/248423.php.
Salazar, Luis A., et al. �The Role of Endocrine System in the Inflammatory Process.� Mediators of Inflammation, Hindawi, 29 Sept. 2016, www.hindawi.com/journals/mi/2016/6081752/.
Seladi-Schulman, Jill. �Endocrine System Overview.� Healthline, 22 Apr. 2019, www.healthline.com/health/the-endocrine-system.
Straub, Rainer H. �Interaction of the Endocrine System with Inflammation: a Function of Energy and Volume Regulation.� Arthritis Research & Therapy, BioMed Central, 13 Feb. 2014, www.ncbi.nlm.nih.gov/pmc/articles/PMC3978663/.

by Dr Alex Jimenez | Chiropractic, Fibromyalgia, Functional Medicine, Wellness
Do you feel:
- Afternoon fatigue?
- Headaches with exertion or stress?
- Can you not stay asleep?
- Slow starter in the morning?
- Afternoon headaches?
If you are experiencing any of these situations, then you might be experiencing fibromyalgia.
Fibromyalgia is a common and chronic syndrome that causes pain and mental distress in the body. It causes widespread musculoskeletal pain, and it is accompanied by fatigue, sleep memory, and mood issues to the body.�The symptoms may be similar to arthritis; however, fibromyalgia is a rheumatic condition and causes soft tissue pain or myofascial pain.

The NIAMS (National Institute of Arthritis and Musculoskeletal and Skin Diseases) stated that around 5 million adults, ages 18 years and over in the United States had experienced fibromyalgia. Around 80 to 90 percent of fibromyalgia patients are mostly found in women who have this chronic disease, and men can have it as well.
Symptoms of Fibromyalgia

There are three symptoms that fibromyalgia causes a person to have discomfort in their daily lives. They are:
- Widespread pain: This pain is associated with fibromyalgia, and it is described as a constant dull ache that can last for at least three months. For it to be considered as widespread pain, it must occur both sides of the body, as well as above and below the waist.
- Fatigue: Individuals with fibromyalgia often awaken tired, even though they have been sleeping for long periods. The pain that fibromyalgia causes can disrupt the person’s sleep patterns, causing them to have sleep disorders such as restless legs syndrome and sleep apnea.
- Cognitive difficulties: This symptom is commonly known as �fibro fog.� It impairs the person�s ability to focus, pay attention, and concentrate on mental tasks.
Other symptoms can include:
- IBS (irritable bowel syndrome)
- Stiff joints and muscles in the morning
- Headaches
- Problems with vision
- Nausea
- Pelvic and urinary problems
- Depression and anxiety
In the past, studies have shown that patients diagnosed with fibromyalgia had 11 out of 18 specific trigger points all around their bodies. Healthcare providers would check their patients and document how many of these points were painful to their patients by firmly, but gently, pressing their bodies to get a diagnosis.
The typical trigger points include:
- The back of the head
- The tops of the shoulders
- The upper chest
- The hips
- The knees
- The outer elbows
Nowadays, in a 2016 revised diagnostic criteria, healthcare providers can diagnose patients with fibromyalgia if the patient has pain in 4 out of 5 areas of the body that is causing them pain. The protocol when diagnosing patients is referred to as �multisite pain.�
Fibromyalgia Affecting the Endocrine System
When it comes to fibromyalgia, the symptoms are associated with the endocrine system. Research shows that fibromyalgia-like symptoms such as muscle pain and tenderness, exhaustion, reduced exercise capacity, and cold intolerance can resemble symptoms that are associated with the endocrine dysfunction like hypothyroidism and adrenal or growth hormone insufficiency.
More research has stated that fibromyalgia causes a person to develop chronic fatigue syndrome. Chronic fatigue syndrome causes the body to have a deficiency of serotonergic activity and the hypofunction of sympathetic nervous system function that could contribute to the abnormalities of the central components of the HPA axis. It can distort the body’s hormonal pattern that is being attributed to the hyperactivity of the CRH neurons. The hyperactivity caused by the CRH neurons can be driven and sustained by stress being exerted by chronic pain that has originated in the musculoskeletal system or the alternation of the central nervous system mechanism of nociception.

Researchers believe that repeated nerve stimulation causes the brains of patients with fibromyalgia to change. The change causes an abnormal increase level of certain chemicals (neurotransmitters) in the brain that signals pain. In addition, the brain�s pain receptors will develop a sort of memory of the pain that is causing problems to the patient�s body and causing them to be more sensitive since the signals are overreacting.
Treating Fibromyalgia

Even though fibromyalgia pain can be uncomfortable and consistent enough to interfere with a person�s daily routine. There are ways to relieve the pain and inflammation that fibromyalgia causes the body. Pain medication can bring down the inflammation and help a person sleep a little better. Other safe treatments that can help manage fibromyalgia pain are:
- Acupuncture: Acupuncture is a Chinese medical system that uses needles to cause changes in the blood flow and the levels of neurotransmitters in the brain and spinal cord.
- Therapy: A variety of different therapies can help a person reduce the effects that fibromyalgia has caused.
- Yoga and tai chi: These practices combine meditation, slow movements, deep breathing, and relaxation � both help control fibromyalgia symptoms.
- Reducing stress: Developing a plan to avoid or limit overexertion and emotional stress is useful when dealing with fibromyalgia. Learning to meditate and trying stress management techniques can help a person feel calm and recharged for the rest of the day.
- Getting enough sleep: Since fatigue is one of the main characteristics of fibromyalgia, getting enough sleep is essential. Practicing good sleep habits and going to bed and getting up at the same time each day can lessen the effects of fatigue.
- Exercising regularly: At first, exercising may increase the pain, but doing it gradually and regularly over time can decrease the symptoms. This can be walking, swimming, biking, and water aerobics can be beneficial to the body.
- Pacing yourself: Keeping track of activities is beneficial for people with fibromyalgia. Moderation of daily activities on the good days can help a person overcome the symptoms when they flare-up.
- Maintaining a healthy lifestyle: Eating healthy food that has anti-inflammatory properties can be useful for the body, and finding enjoyable hobbies can be beneficial as well.
Conclusion
Fibromyalgia is a chronic illness that causes pain and inflammation that affects the soft tissue in the body. The symptoms can resemble joint inflammation and causes people to have fatigue and discomfort all over their body. When these symptoms flare up, it can cause body damage. Treatments can help a person reduce the effects of fibromyalgia and be beneficial. Some products are formulated to counter the effects of temporary stress and offer support in the gastrointestinal system and the body�s metabolism.
The scope of our information is limited to chiropractic, musculoskeletal, and nervous health issues as well as functional medicine articles, topics, and discussions. We use functional health protocols to treat injuries or chronic disorders of the musculoskeletal system. To further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at�915-850-0900�.
References:
Felman, Adam. �Fibromyalgia: Symptoms, Causes, and Treatment.� Medical News Today, MediLexicon International, 5 Jan. 2018, www.medicalnewstoday.com/articles/147083.php.
Geenen, Rinie, et al. �Evaluation and Management of Endocrine Dysfunction in Fibromyalgia.� Rheumatic Diseases Clinics of North America, U.S. National Library of Medicine, May 2002, www.ncbi.nlm.nih.gov/pubmed/12122926.
Neeck, G, and L J Crofford. �Neuroendocrine Perturbations in Fibromyalgia and Chronic Fatigue Syndrome.� Rheumatic Diseases Clinics of North America, U.S. National Library of Medicine, Nov. 2000, www.ncbi.nlm.nih.gov/pubmed/11084955.
Staff, Mayo Clinic. �Fibromyalgia.� Mayo Clinic, Mayo Foundation for Medical Education and Research, 11 Aug. 2017, www.mayoclinic.org/diseases-conditions/fibromyalgia/symptoms-causes/syc-20354780.
Staff, Mayo Clinic. �Fibromyalgia.� Mayo Clinic, Mayo Foundation for Medical Education and Research, 11 Aug. 2017, www.mayoclinic.org/diseases-conditions/fibromyalgia/diagnosis-treatment/drc-20354785.
Unknown, Unknown. �Fibromyalgia.� National Institute of Arthritis and Musculoskeletal and Skin Diseases, U.S. Department of Health and Human Services, 30 Sept. 2019, www.niams.nih.gov/health-topics/fibromyalgia.
Wolfe, Frederick, et al. �2016 Revisions to the 2010/2011 Fibromyalgia Diagnostic Criteria.� Seminars in Arthritis and Rheumatism, W.B. Saunders, 30 Aug. 2016, www.sciencedirect.com/science/article/abs/pii/S0049017216302086?via%3Dihub.
by Dr Alex Jimenez | Functional Medicine, Gastro Intestinal Health, Gut and Intestinal Health, Health, Wellness
Do you feel:
- Edema and swelling in the ankles and the wrist?
- Muscle cramping?
- Frequent urination?
- Poor muscle endurance?
- Alternation in bowel regularity?
If you are experiencing any of these situations, then you might be experiencing chronic kidney disease.
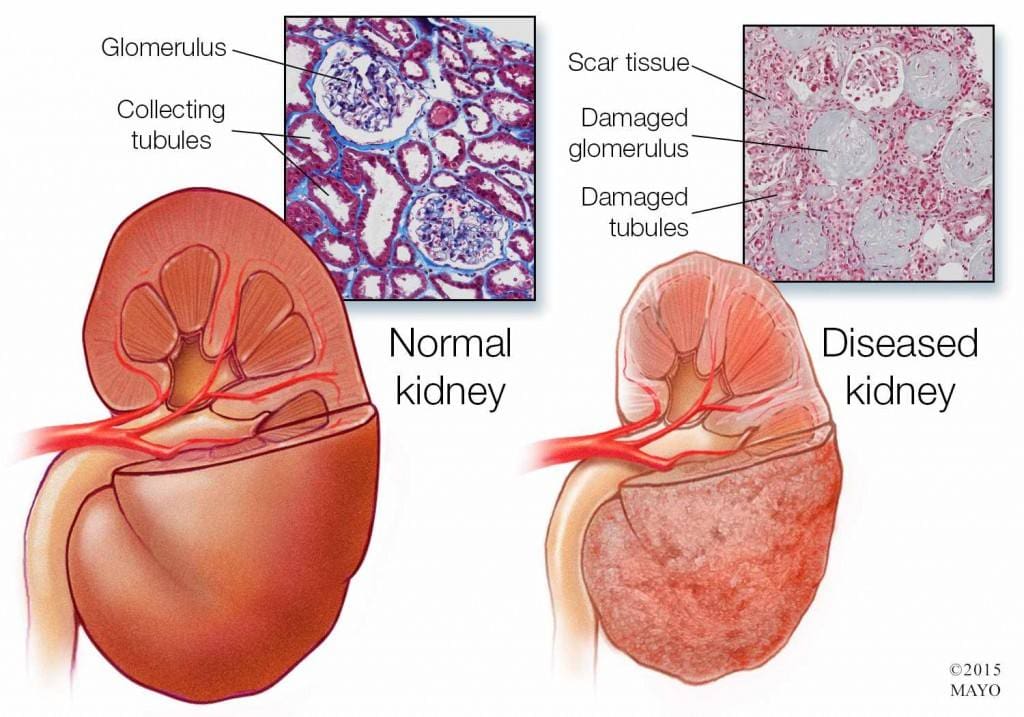
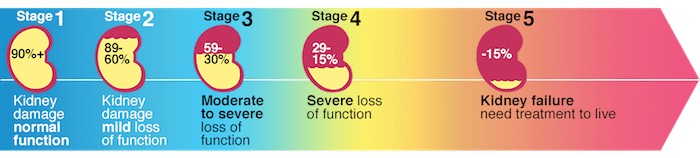
About over 10% of the adult population suffers from CKD (chronic kidney disease), and the two leading underlying causes of the end-stage of chronic kidney disease are type 2 diabetes and hypertension. Other chronic ailments like dysbiosis of the gut microbiome, inflammation, oxidative stress, as well as environmental toxins and PPI (proton pump inhibitor). All these chronic ailments have been linked to chronic kidney disease in the body.
Chronic Kidney Disease
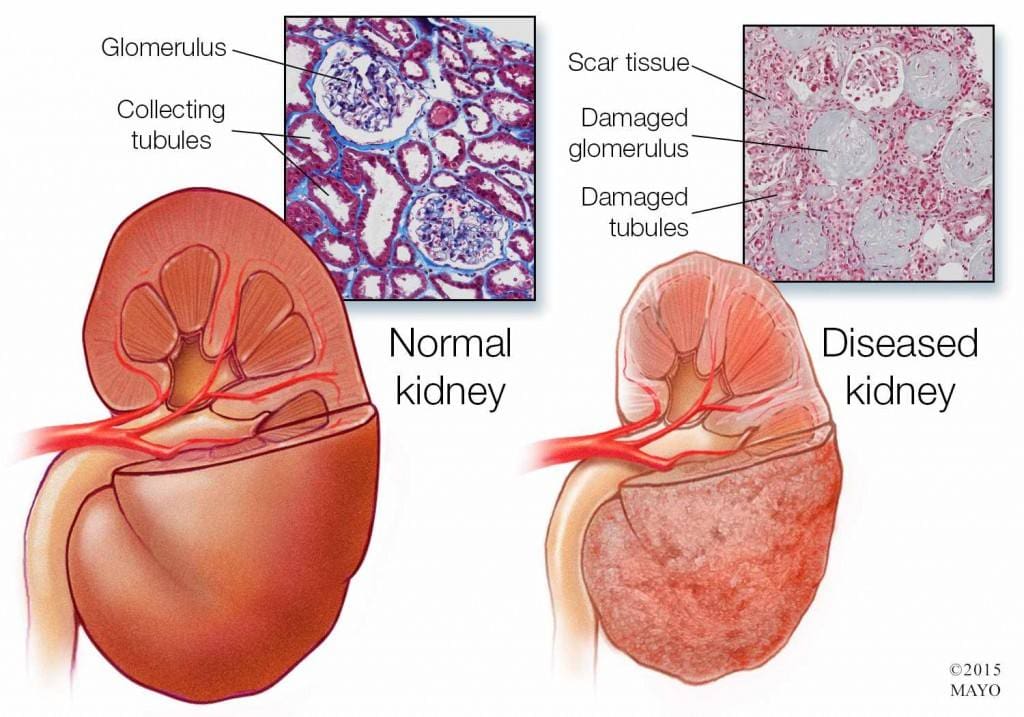
Chronic kidney disease is a slow and progressive loss of kidney function over several years. Also known as chronic renal failure, it much more widespread, and it often goes undetected and undiagnosed until the disease is well advanced. It is not unusual for anyone to realize they have chronic kidney failure when their kidneys are functioning only at 25% than average. As it advances and the kidney’s function is severely impaired, dangerous levels of waste and fluid can rapidly build up in the body.
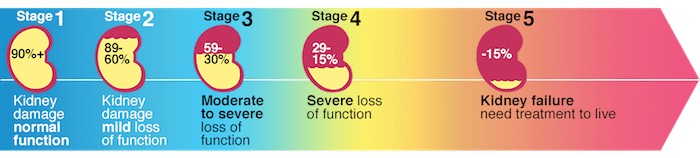
Chronic kidney failure is different from acute kidney failure due to being a slow and gradually progressive disease. When the disease is fairly well advanced, the conditions are more severe than the signs and symptoms are noticeable, making most of the damage irreversible. Here are some of the most common signs and symptoms of chronic kidney disease include:
- Anemia
- Blood in urine
- Dark urine
- Edema- swollen feet, hands, ankles, and face
- Fatigue
- Hypertension
- More frequent urination, especially at night
- Muscle cramps and twitches
- Pain on the side or mid to lower back
Dietary Fibers for CKD
Researchers have investigated that the role of dietary fibers and the gut microbiome is in renal diets. When there is a dysbiosis in the gut microbiome, it can be a risk factor for the development of chronic kidney disease, thus reducing the renal function. That function will significantly contribute to dysbiosis. The current renal dietary recommendations include a reduction of protein intake with an increase in complex carbohydrates and fiber.
A systemic review did a test that included 14 controlled trials and 143 participants that had chronic kidney disease. The test demonstrated that all 143 participants had a reduction in serum creatinine and urea that is associated with dietary fiber intake, which occurs in a dose-dependent matter. These participants had an average intake of 27 grams of fiber per day in their diet. It is also an essential note that creatinine is metabolized in the intestinal bacteria in the body.

A high fiber diet can lead to the production of SCFAs (short-chain fatty acids) in the gastrointestinal tract. They play an essential role in T regulatory cell activation, which regulates the intestinal immune system. When there is dysregulation in the immune system, it can cause an increase of inflammation that may occur in chronic kidney disease. With a high fiber diet, the intake is associated with lowering the risk of inflammation and the mortality in kidney disease.
Increasing fiber intake is relatively easy with some of these high fiber foods that are both healthy and nutritious and can help individual’s that have kidney disease. These include:
- Pears
- Strawberries
- Avocados
- Apples
- Carrots
- Beets
- Broccoli
- Lentils
Research has previously demonstrated that a high fiber diet for CDK patients is characterized by the control increase of plant-origin protein and animal-origin foods. This is useful for individuals to limit the consumption of processed food products because of modern conservation processes, which has the purpose of eliminating pathogenic bacteria. People who have chronic kidney disease that go on a high fiber diet have been linked to better kidney function and lowering the risk of inflammation and mortality.
Some individuals may experience some gastrointestinal side effects when they are trying to increase their fiber intake.�Research has been stated that patients should consider resistant starches since it has shown no side effects with the recommended doses.
Conclusion
Chronic kidney disease is a slow and progressive loss of kidney function. The signs and symptoms are noticeable as the disease progress in the later stages. With a high fiber diet, individuals can lower the risk of inflammation and mortality of CDK. When this disease causes inflammation and chronic illness in the kidneys, complications can travel through the entire body. The high fiber diet can also be beneficial for the gut microbiome to function correctly, and some products can help lower the stress hormones and make sure that the body’s hypothalamic-pituitary-adrenal axis is functioning correctly.
October is Chiropractic Health Month. To learn more about it, check out Governor Abbott�s bill on our website to get full details on this historic moment.
The scope of our information is limited to chiropractic, musculoskeletal and nervous health issues as well as functional medicine articles, topics, and discussions. We use functional health protocols to treat injuries or chronic disorders of the musculoskeletal system. To further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900 .
References:
D�Alessandro, Claudia. �Dietary Fiber and Gut Microbiota in Renal Diets.� MDPI, Multidisciplinary Digital Publishing Institute, 9 Sept. 2019, www.mdpi.com/2072-6643/11/9/2149/htm.
Gunnars, Kris. �22 High-Fiber Foods You Should Eat.� Healthline, 10 Aug. 2018, www.healthline.com/nutrition/22-high-fiber-foods.
Jurgelewicz, Michael. �New Article Investigates the Role of Dietary Fiber and the Gut Microbiome in Chronic Kidney Disease.� Designs for Health, 13 Sept. 2019, blog.designsforhealth.com/node/1105.
Khosroshahi, H T, et al. �Effects of Fermentable High Fiber Diet Supplementation on Gut Derived and Conventional Nitrogenous Product in Patients on Maintenance Hemodialysis: a Randomized Controlled Trial.� Nutrition & Metabolism., U.S. National Library of Medicine, 12 Mar. 2019, www.ncbi.nlm.nih.gov/pubmed/?term=30911321.
Krishnamurthy, Vidya M Raj, et al. �High Dietary Fiber Intake Is Associated with Decreased Inflammation and All-Cause Mortality in Patients with Chronic Kidney Disease.� Kidney International, U.S. National Library of Medicine, Feb. 2012, www.ncbi.nlm.nih.gov/pmc/articles/PMC4704855/.
Newman, Tim. �Chronic Kidney Disease: Symptoms, Causes, and Treatment.� Medical News Today, MediLexicon International, 13 Dec. 2017, www.medicalnewstoday.com/articles/172179.php.
Staff, Mayo Clinic. �Chronic Kidney Disease.� Mayo Clinic, Mayo Foundation for Medical Education and Research, 15 Aug. 2019, www.mayoclinic.org/diseases-conditions/chronic-kidney-disease/symptoms-causes/syc-20354521.
by Dr Alex Jimenez | Functional Medicine, Gut and Intestinal Health, Health, Wellness
Do you feel:
- Difficulty digesting roughage and fiber
- Indigestion and fullness the last 2-4 hours
- Pain, tenderness, soreness on the left side, under the rib cage
- Nausea or vomiting
- Stool undigested, foul-smelling, mucus-like, greasy or poorly formed
If you are experiencing any of these situations, then you might be experiencing pancreatic digestive disorders.
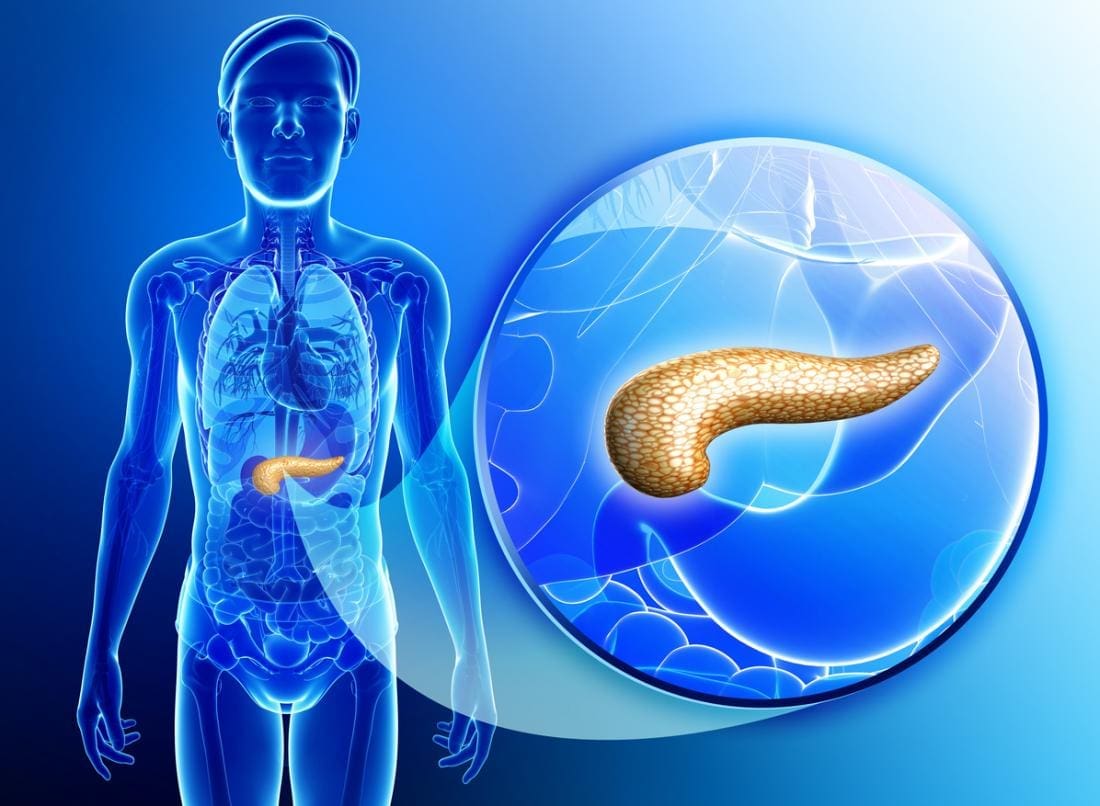
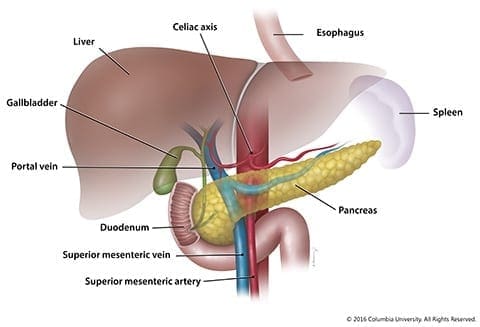
The Pancreas
The pancreas is a gland organ located in the abdomen. It is part of the digestive system, producing insulin and other vital enzymes and hormones that help break down food. It has an endocrine function, due to releasing juices directly into the bloodstream and has an exocrine function that releases juices into the ducts in the body.
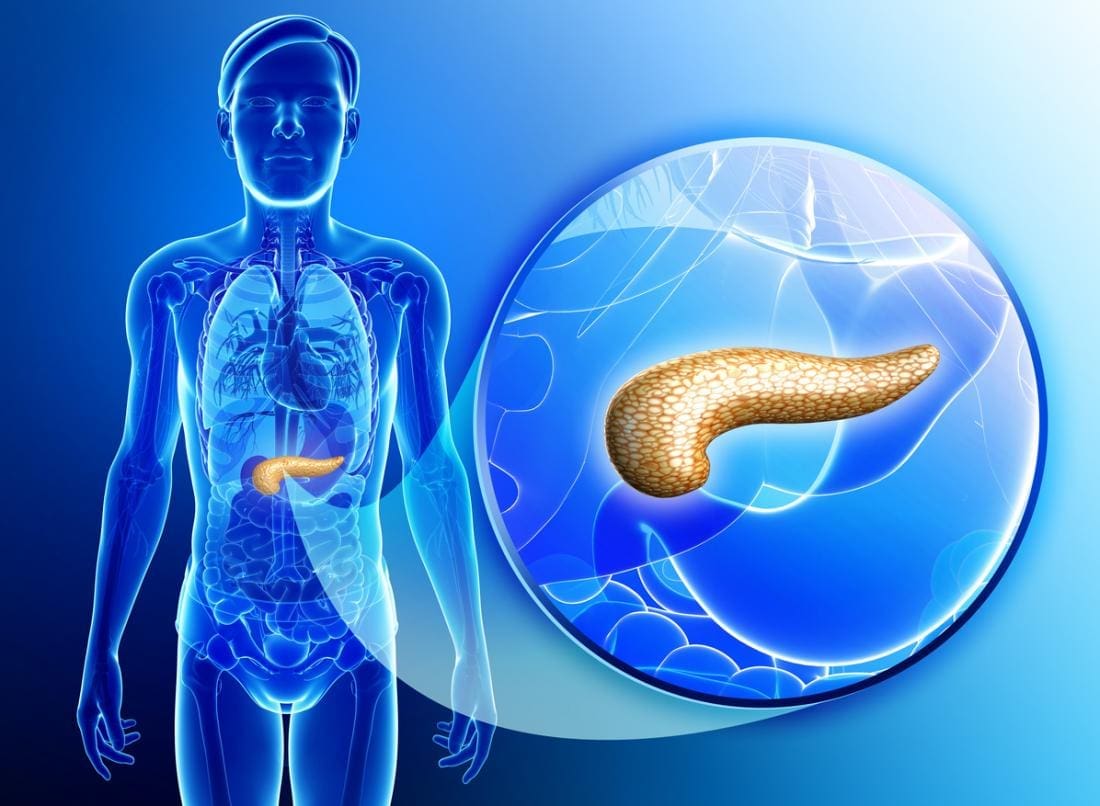
One of its many jobs the pancreas does is that it secretes out enzymes into the small intestine and continues to break down that left in the stomach. Another job is that it produces insulin and secretes it into the bloodstream, where it can regulate the body’s glucose or sugar level. When there is a problem with insulin control in the body, it can lead a person to have diabetes. Other health problems include pancreatitis and pancreatic cancer.
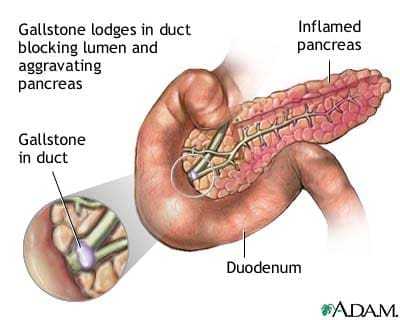
Pancreatitis

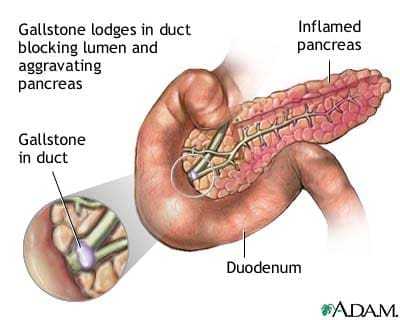
Pancreatitis is an inflammation in the pancreas. It occurs when the digestive enzymes become activated while irritating the cells in the pancreas. With repeated damages to the pancreas, it can cause either two forms of pancreatitis, which is acute pancreatitis and chronic pancreatitis. Both are very painful and can form scar tissue in the pancreas, causing it to lose its function. A poorly functioning pancreas can cause digestion problems and diabetes. Here are the conditions that can lead to pancreatitis:
- Abdominal surgery
- Alcoholism
- Certain medications
- Cystic fibrosis
- Gallstones
- Obesity
Chronic Pancreatitis
Chronic pancreatitis is a long-term progressive inflammatory disease in the pancreas that can lead to a permanent breakdown of the structure and function of the pancreas in the body. Studies stated that the most common cause of chronic pancreatitis is long term alcohol abuse, it is thought to account for between 70 to 80 percent for all cases, and significantly it affects more men than women.
Common signs and symptoms of chronic pancreatitis include:
- Severe upper abdominal pain that is more intense after a meal
- Nausea and vomiting
When the disease progresses, the episodes of pain will become more frequent and more severe to individuals. Some individuals eventually suffer from constant abdominal pain, and as chronic pancreatitis progresses, the ability of the pancreas to produce digestive juices will deteriorate, and the following symptoms appear:
- Smelly and greasy stool
- Bloating
- Abdominal cramps
- Flatulence
- Diabetes
There are numerous complications that an individual can potentially have with chronic pancreatitis. Nutrient malabsorption is one of the most complications since the pancreas is not producing enough digestive enzymes for the body to absorb the nutrients properly, leading to malnutrition. Another possible complication is the development of diabetes, where chronic pancreatitis damages the cells that produce insulin and glucagon to the body. Some individuals will also develop pseudocyst, which is fluid-filled that can form inside or outside the pancreas and can be very dangerous to the body since they can block the essential ducts and blood vessels.
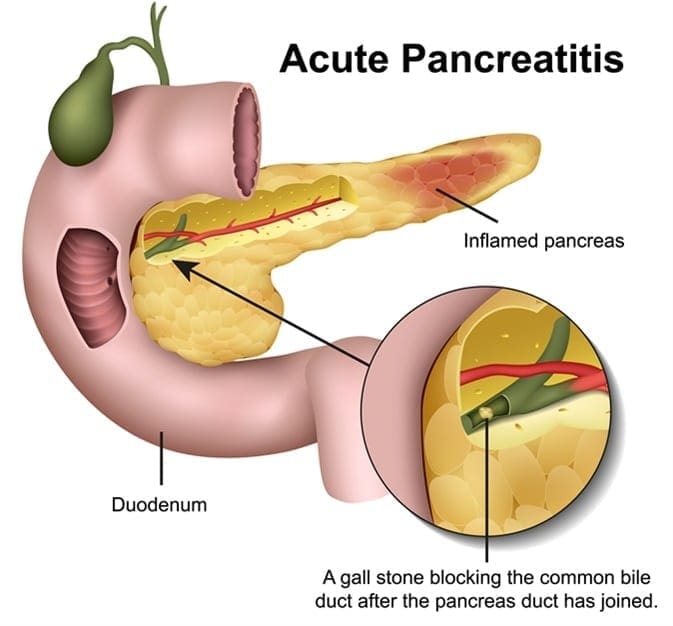
Acute Pancreatitis
Acute pancreatitis is a sudden inflammation of the pancreas. It causes the enzymes to be excessively produced, causing the pancreas gland to be swollen and inflamed. It will make digestion slow down and become painful, making the other body functions be affected as well as making the pancreas be permanently damaged and scarred.
Acute pancreatitis is painful and can develop quickly. It can trigger potentially fatal complications as the mortality rate can range from less than 5 percent to over 30 percent, depending on the severity of the condition and if it reaches to the other organs beyond the pancreas. The most common cause of acute pancreatitis is the production of gallstones in the gallbladder, alcohol misuse, and infections.
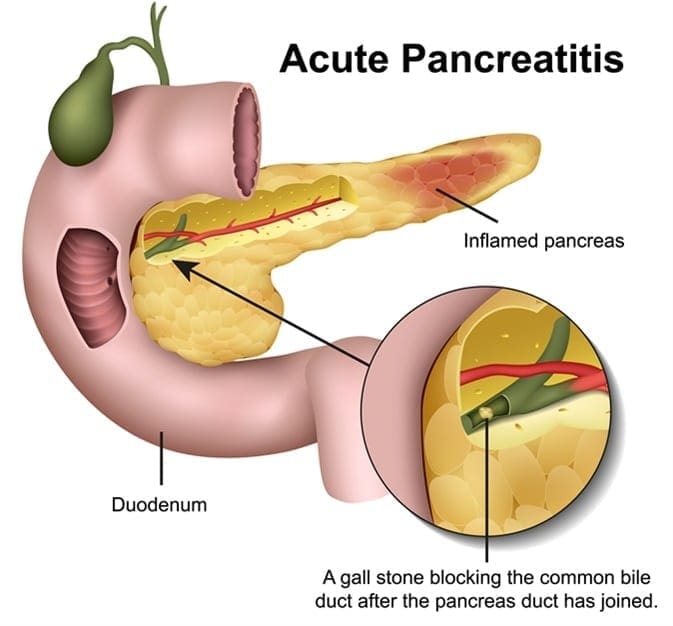
When a person has acute pancreatitis, they feel the pain in the lower abdomen and then feel it more gradually as the pain intensified until it is a constant ache. Other symptoms include:
- Vomiting and nausea
- Diarrhea
- Loss of appetite
- Pain with coughing, vigorous movements, and deep breathing
- Tenderness when the abdomen is touched
- Fever
- Jaundice, yellowish tinge on the skin and the whites of the eyes
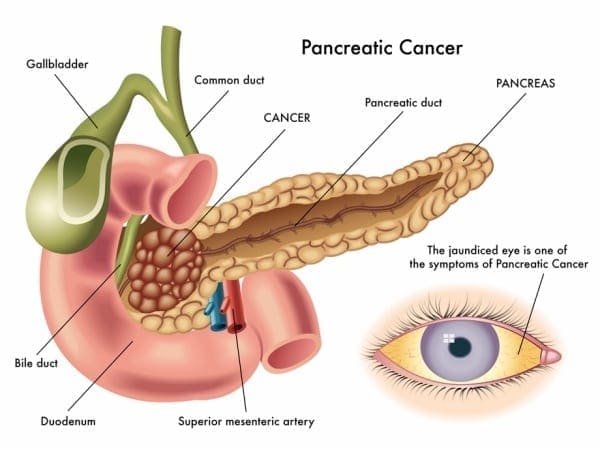
Pancreatic Cancer
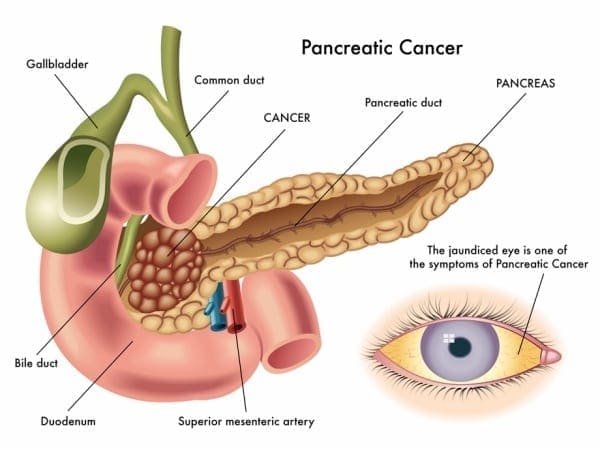
Also known as �the silent disease,” pancreatic cancer happens when uncontrolled cell growth begins to form in a part of the pancreas. Tumors develop and interfere with the way the pancreas works. Pancreatic cancer often shows any symptoms until the later stages, and it can be challenging to manage. The signs and symptoms of pancreatic cancer include:
- Pain in the upper abdomen that radiates to the back
- Unintended weight loss or loss of appetite
- Pale or grey fatty stool
- Jaundice
- New-onset diabetes
- Blood clots
- Depression
- Fatigue
Conclusion
The pancreas is located in the abdomen, and its primary function is to produce insulin and necessary enzymes and hormone to aid the digestion of food. When complications are attacking the pancreas like pancreatic cancer and pancreatitis, it can damage the pancreas to stop producing insulin and can lead to chronic illnesses to spread all over the body. Some products can help support the sugar metabolism that the pancreas creates and offer nutrients and enzymatic cofactors to the gastrointestinal system in the body.
October is Chiropractic Health Month. To learn more about it, check out Governor Abbott�s proclamation on our website to get full details on this historic moment.
The scope of our information is limited to chiropractic, musculoskeletal and nervous health issues as well as functional medicine articles, topics, and discussions. We use functional health protocols to treat injuries or chronic disorders of the musculoskeletal system. To further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900 .
Reference:
Banks, Peter A, et al. �The Management of Acute and Chronic Pancreatitis.� Gastroenterology & Hepatology, Millennium Medical Publishing, Feb. 2010, www.ncbi.nlm.nih.gov/pmc/articles/PMC2886461/.
Bartel, Michael. �Acute Pancreatitis – Gastrointestinal Disorders.� MSD Manual Professional Edition, MSD Manuals, July 2019, www.msdmanuals.com/en-gb/professional/gastrointestinal-disorders/pancreatitis/acute-pancreatitis.
Brazier, Yvette. �Acute Pancreatitis: Symptoms, Treatment, Causes, and Complications.� Medical News Today, MediLexicon International, 19 Dec. 2017, www.medicalnewstoday.com/articles/160427.php.
Brazier, Yvette. �Pancreatic Cancer: Symptoms, Causes, and Treatment.� Medical News Today, MediLexicon International, 23 Oct. 2018, www.medicalnewstoday.com/articles/323423.php.
Colledge, Helen, et al. �Chronic Pancreatitis.� Healthline, 14 Sept. 2017, www.healthline.com/health/chronic-pancreatitis.
Crosta, Peter. �Pancreas: Functions and Disorders.� Medical News Today, MediLexicon International, 26 May 2017, www.medicalnewstoday.com/articles/10011.php.
Felman, Adam. �Chronic Pancreatitis: Treatments, Symptoms, and Causes.� Medical News Today, MediLexicon International, 19 Dec. 2017, www.medicalnewstoday.com/articles/160459.php.
Health Publishing, Harvard. �Acute Pancreatitis.� Harvard Health, July 2019, www.health.harvard.edu/a_to_z/acute-pancreatitis-a-to-z.
Staff, Mayo Clinic. �Pancreatic Cancer.� Mayo Clinic, Mayo Foundation for Medical Education and Research, 9 Mar. 2018, www.mayoclinic.org/diseases-conditions/pancreatic-cancer/symptoms-causes/syc-20355421.
Staff, Mayo Clinic. �Pancreatitis.� Mayo Clinic, Mayo Foundation for Medical Education and Research, 7 Sept. 2019, www.mayoclinic.org/diseases-conditions/pancreatitis/symptoms-causes/syc-20360227.
by Dr Alex Jimenez | Functional Medicine, Gut and Intestinal Health, Health, Hormone Balance, Wellness
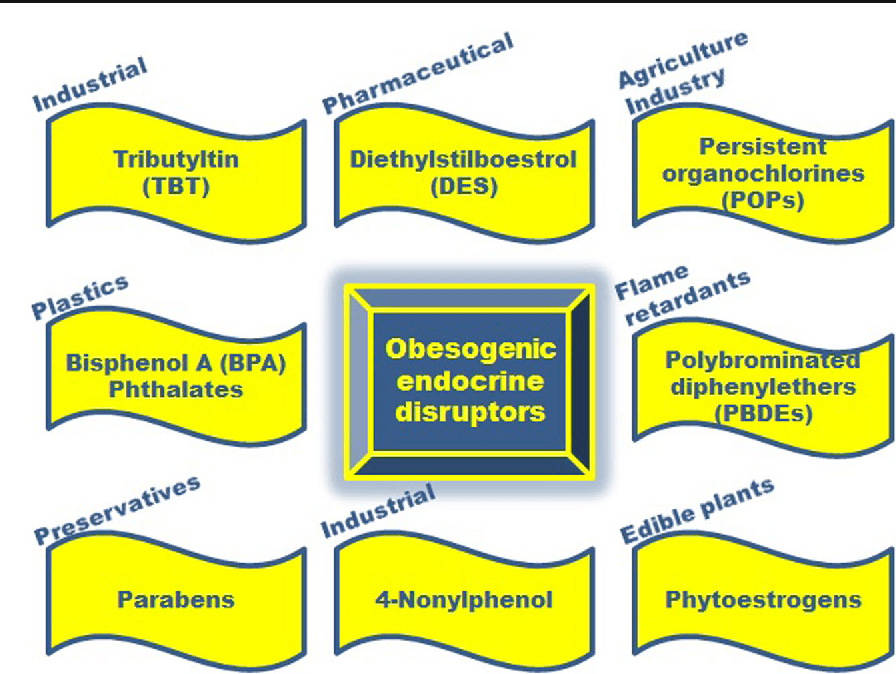
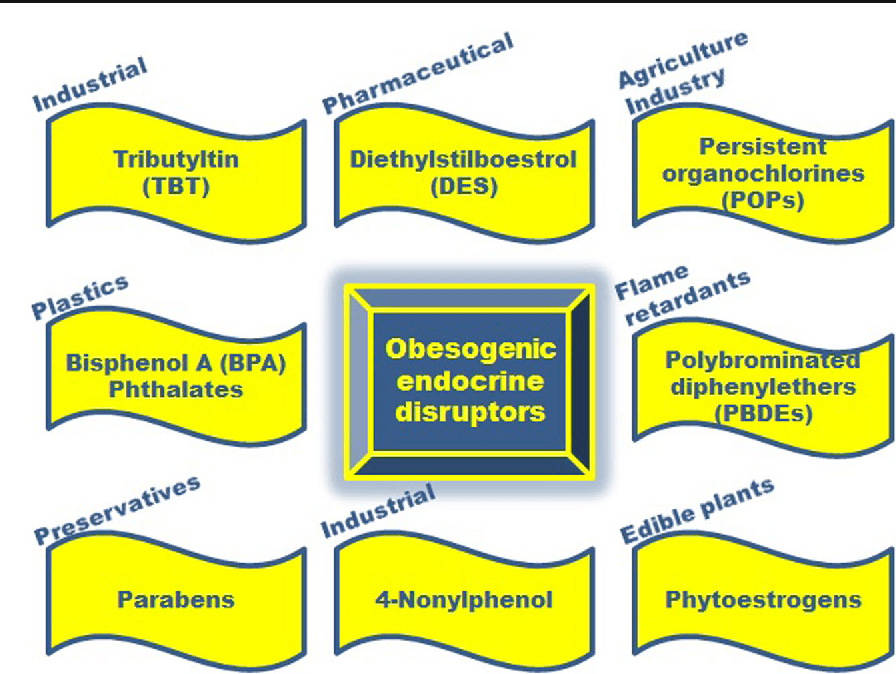
Endocrine disruptors are chemicals that may interfere with the body’s endocrine system and produce adverse developmental, reproductive, neurological, and immune effects in humans. It can be pesticides, plasticizers, antimicrobials, and flame retardants that can be EDCs. EDCs (endocrine-disrupting chemicals) can disrupt the hormonal balance and can result in developmental and reproductive abnormalities in the body.
There are four points about endocrine disruption:
- Low dose matters
- Wide range of health benefits
- Persistence of biological effects
- Ubiquitous exposure
EDC can cause significant risks to humans by targeting different organs and systems in the body. The interactions and the mechanisms of toxicity created by EDC and environmental factors can be concerning a person’s general health problems. Including endocrine disturbances in the body since many factors can cause endocrine disruptors, one of the disruptors in the food contaminated with PBDEs (polybrominated diphenyl esters) in fish meat and dairy.
Researchers also pointed out that once the contaminated foods eliminated from a person’s diet, then the endocrine disruptors decline, and the body began to heal properly. When a person eliminates the food that is causing discomfort to their bodies, they are more aware of reading the food labels to prevent discomfort anymore to the body systems.
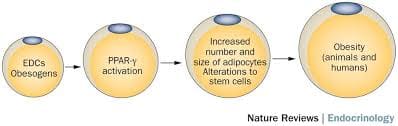
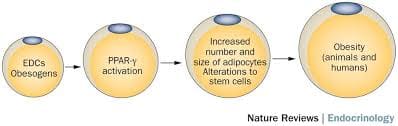
Obesogen
Obesogen is a subclass of endocrine-disrupting chemicals (EDC) that might predispose individuals to the development of obesity. Their structure is mainly lipophilic, and they can increase fat deposition. Since the fat cell’s primary role is to store and release energy, researchers have found that different obesogenic compounds may have different mechanisms of action.
Some of these actions can affect the number of fat cells that are producing, while others affect the size of the fat cells, and some obesogenic compounds can affect the hormones. These compounds will affect the appetite, satiety, food preferences, and energy metabolism when the endocrine system plays a fundamental role in the body to regulate the metabolism of fats, carbohydrates, and proteins. Any alternations in the body can result in an imbalance in the metabolism and causing endocrine disorders.
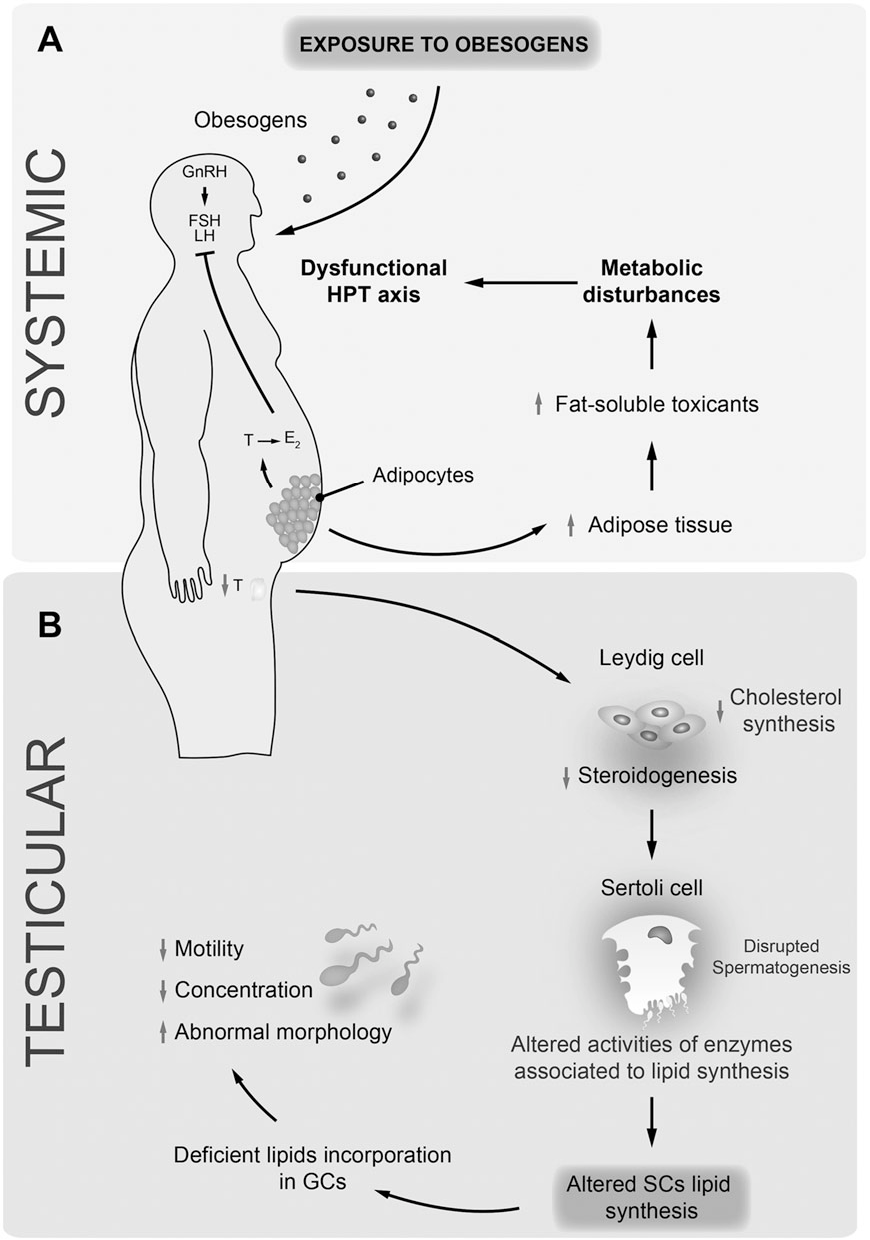
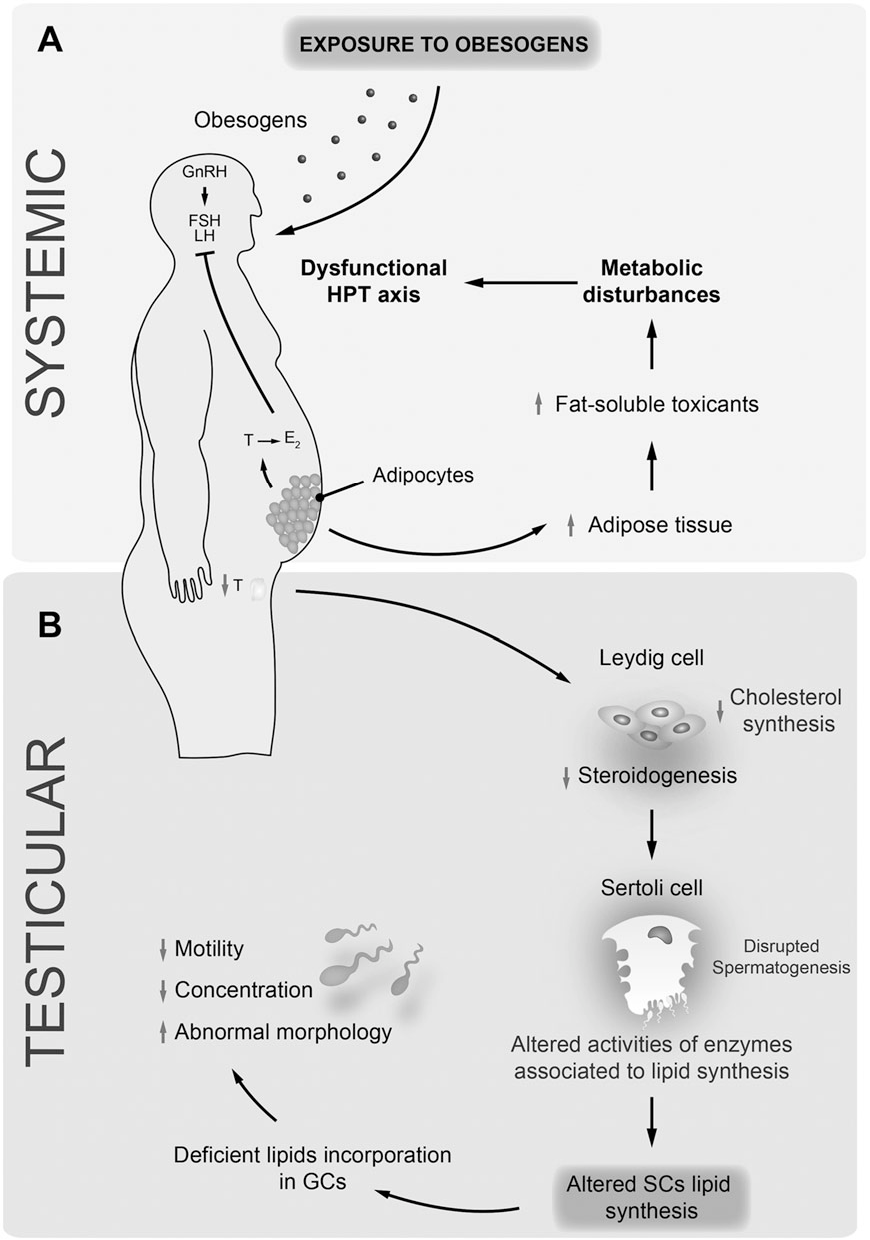
Studies even stated that exposure to obesogens could be found either before birth on utero or in the neonatal period. Obesogens can even cause a decrease in male fertility. When this disruption happens to the male body, environmental compounds can cause a predispose to weight gain, and obesogens can appoint as one of the contributors because of their actions as endocrine disruptors. Obesogens can even change the functioning of the male reproductive axis and testicular physiology. The metabolism in the male human body can be pivotal for spermatogenesis due to these changes.
Endocrine Disruptors and Obesity
Some endocrine disruptors that can affect the body can be through pharmaceutical drugs that can cause weight gain. A variety of prescription drugs can have an adverse effect that can result in weight gain since the chemicals found in prescription drugs have similar structures, and modes of action might have a role in obesity. Prescription medicine can stimulate the gut to consume more food, thus involving the body to gain weight.
Another endocrine disruptor is PAHs (polycyclic aromatic hydrocarbons). These are a family of environmental chemicals that occur in oil, coal, and tar deposits. They produce as by-products of fuel-burning like fossil fuel, biomass, cigarette smoke, and diesel exhaust. PAHs can either be manufactured to be used as medicines and pesticides or be released naturally from forest fires and volcanoes.
There are standard ways a person can be exposed to PAHs. One is through eating grilled, charred, or charcoal-broiled meats that a person eats. The other is through inhalation of smoke from cigarettes, vehicle exhaust, or emissions from fossil fuels that can irritate the eyes and breathing passageways in the body.
Coping with EDC Exposure
Even though obesity can adversely affect the body in a variety of health outcomes, there are ways to cope and minimize the exposure of EDC. Research shows that a person can minimize EDC exposure by consuming organic fruits, vegetables, and grain products insofar as possible. This includes an increasing number of fungicides routinely applied to fruits and vegetables that are being identified as obesogens and metabolic disruptors in the body.
Xenoestrogen vs. Phytoestrogen
When a person has an endocrine disorder, it might be due to the food they are consuming. Phytoestrogens are plant-derived compounds that are in a wide variety of food, mostly in soy. They are presented in numerous dietary supplements and widely marketed as a natural alternative to estrogen replacement therapy.
There is a health impact on phytoestrogen, and the plant-derived compound can either mimic, modulate, or disrupt the actions of endogenous estrogen. Xenoestrogen�are synthetically derived chemical agents from certain drugs, pesticides, and industrial by-products that mimic endogenous hormones or can interfere with endocrine disruptors. These chemical compounds can cause an effect on several developmental anomalies to humans. It can also interfere with the production and metabolism of ovarian estrogen in females.
Conclusion
Endocrine disruptors can interfere with the body’s endocrine system causing a health risk to an individual. EDC (endocrine-disrupting chemicals) can target many different organs and systems of the body by various factors that the human body is being exposed to. One of the EDC factors is obesogen, and it can cause a person to gain weight and be obese. Another factor is the exposure of PAHs (polycyclic aromatic hydrocarbons) through environmental factors like smoke inhalation or consuming charcoal-broiled meats. There are ways to cope with EDC exposure, and one is eating organic foods, especially fresh fruits and vegetables. Another is products that target the endocrine system and helps support the liver, intestines, body metabolism, and estrogen metabolism to ensure not only a healthy endocrine system but also a healthy body to function correctly.
October is Chiropractic Health Month. To learn more about it, check out Governor Abbott’s proclamation on our website to get full details on this historic event.
The scope of our information is limited to chiropractic, musculoskeletal and nervous health issues as well as functional medicine articles, topics, and discussions. We use functional health protocols to treat injuries or chronic disorders of the musculoskeletal system. To further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900 .
References:
Cardoso, A M, et al. �Obesogens and Male Fertility.� Obesity Reviews : an Official Journal of the International Association for the Study of Obesity, U.S. National Library of Medicine, Jan. 2017, www.ncbi.nlm.nih.gov/pubmed/27776203.
Darbre, Philippa D. �Endocrine Disruptors and Obesity.� Current Obesity Reports, Springer US, Mar. 2017, www.ncbi.nlm.nih.gov/pmc/articles/PMC5359373/.
Holtcamp, Wendee. �Obesogens: an Environmental Link to Obesity.� Environmental Health Perspectives, National Institute of Environmental Health Sciences, Feb. 2012, www.ncbi.nlm.nih.gov/pmc/articles/PMC3279464/.
Janesick, Amanda S, and Bruce Blumberg. �Obesogens: an Emerging Threat to Public Health.� American Journal of Obstetrics and Gynecology, U.S. National Library of Medicine, May 2016, www.ncbi.nlm.nih.gov/pmc/articles/PMC4851574/.
Janesick, Amanda S, and Bruce Blumberg. �Obesogens: an Emerging Threat to Public Health.� American Journal of Obstetrics and Gynecology, U.S. National Library of Medicine, May 2016, www.ncbi.nlm.nih.gov/pubmed/26829510.
Kyle, Ted, and Bonnie Kuehl. �Prescription Medications & Weight Gain.� Obesity Action Coalition, 2013, www.obesityaction.org/community/article-library/prescription-medications-weight-gain/.
L�r�nd, T, et al. �Hormonal Action of Plant Derived and Anthropogenic Non-Steroidal Estrogenic Compounds: Phytoestrogens and Xenoestrogens.� Current Medicinal Chemistry, U.S. National Library of Medicine, 2010, www.ncbi.nlm.nih.gov/pubmed/20738246.
Patisaul, Heather B, and Wendy Jefferson. �The Pros and Cons of Phytoestrogens.� Frontiers in Neuroendocrinology, U.S. National Library of Medicine, Oct. 2010, www.ncbi.nlm.nih.gov/pmc/articles/PMC3074428/.
Singleton, David W, and Sohaib A Khan. �Xenoestrogen Exposure and Mechanisms of Endocrine Disruption.� Frontiers in Bioscience : a Journal and Virtual Library, U.S. National Library of Medicine, 1 Jan. 2003, www.ncbi.nlm.nih.gov/pubmed/12456297.
Unknown, Unknown. �Endocrine Disruptors.� National Institute of Environmental Health Sciences, U.S. Department of Health and Human Services, 2015, www.niehs.nih.gov/health/topics/agents/endocrine/index.cfm.
Unknown, Unknown. �Polycyclic Aromatic Hydrocarbons (PAHs): Your Environment, Your Health | National Library of Medicine.� U.S. National Library of Medicine, National Institutes of Health, 31 Apr. 2017, toxtown.nlm.nih.gov/chemicals-and-contaminants/polycyclic-aromatic-hydrocarbons-pahs.
Yang, Oneyeol, et al. �Endocrine-Disrupting Chemicals: Review of Toxicological Mechanisms Using Molecular Pathway Analysis.� Journal of Cancer Prevention, Korean Society of Cancer Prevention, 30 Mar. 2015, www.jcpjournal.org/journal/view.html?doi=10.15430%2FJCP.2015.20.1.12.

by Dr Alex Jimenez | Functional Medicine, Health, Hormone Balance, Wellness
The body secretes and circulates 50 different hormones to different organs in the body. Hormones are the chemical substances that coordinate the activities of living organism growth. They are secreted through the endocrine glands and travel through the bloodstream to different organs in the body to function properly. When there is an excessive quantity or an reduced quantity of hormones being produced, it can cause the body to malfunction and develop chronic illnesses.
The Pituitary Gland Functions
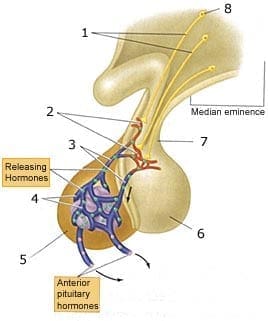
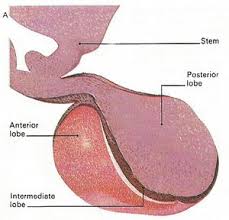
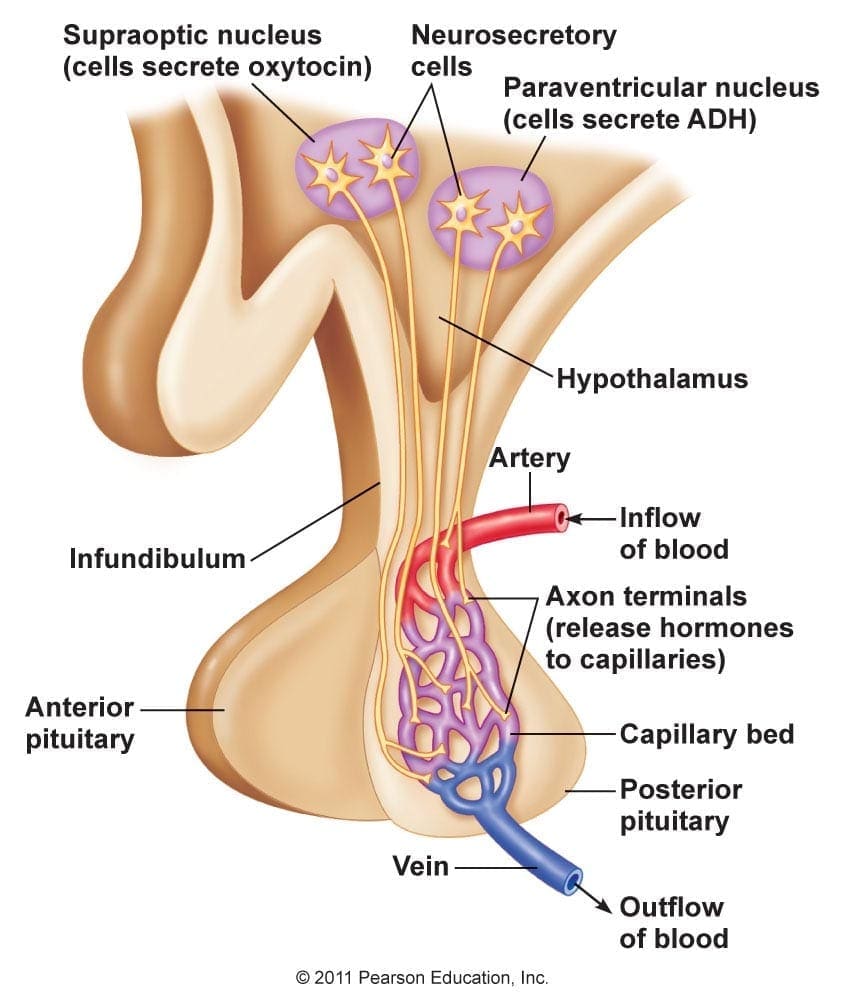
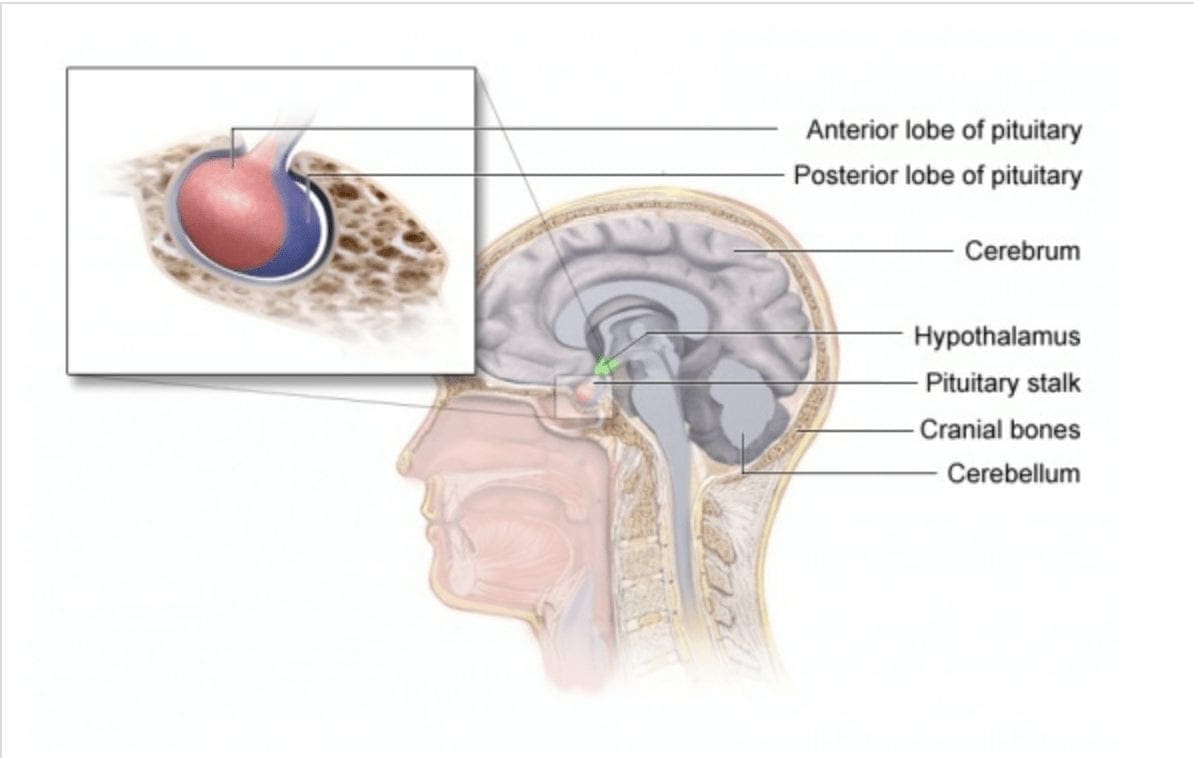
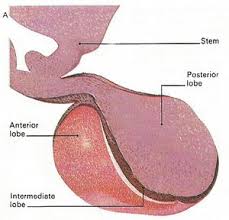
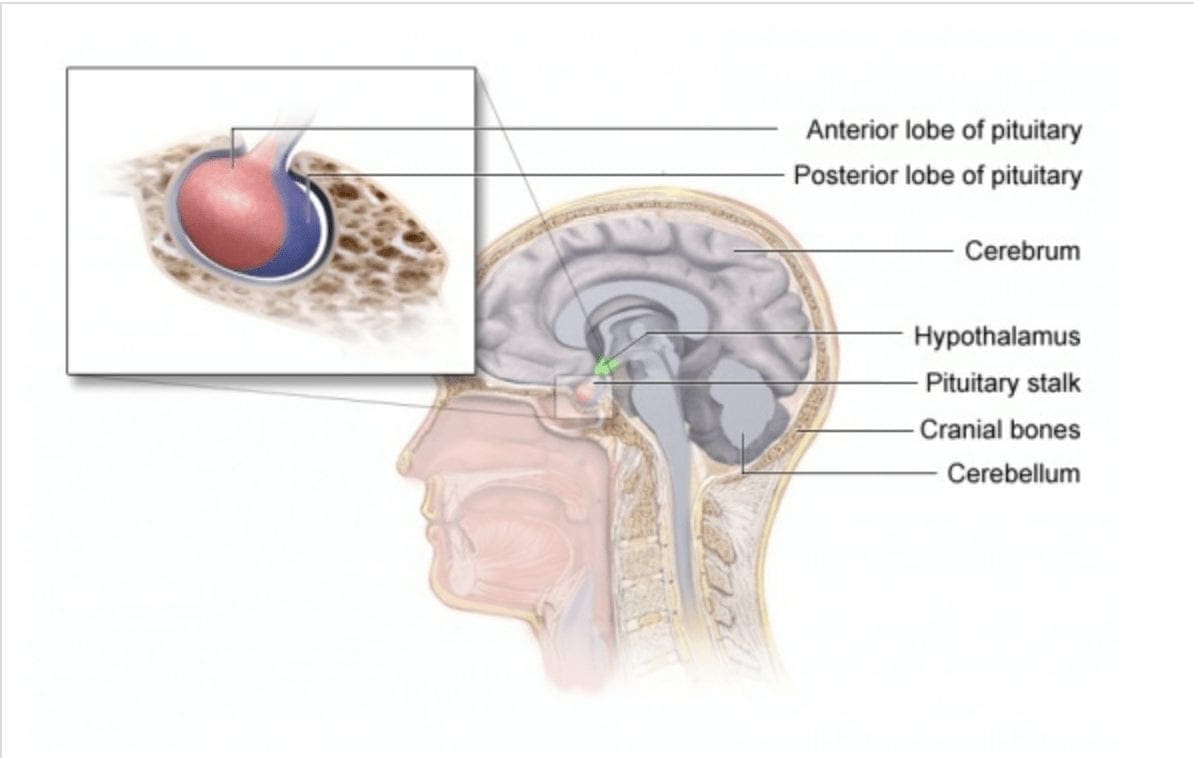
In neuroendocrinology, an endocrine gland can�t make a hormone without activation from a pituitary-stimulating hormone. The pituitary-stimulating hormone helps regulate hormones by secreting them to the endocrine glands. The pituitary gland is known as the �master gland� since it controls the activity of the other endocrine glands and it consists of 3 parts known as the anterior, intermediate and posterior lobes.
Anterior Lobe
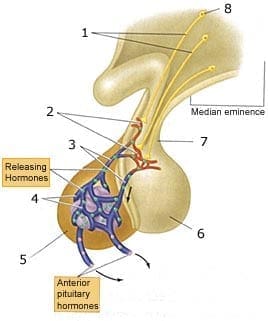
The anterior pituitary gland is located in the sella turcica and is controlled by the hypothalamus in the brain. It secretes a quantity of peptides and glycoprotein hormones that help regulate the growth, metabolism, reproduction and stress response. The anterior pituitary gland produces 6 hormones that circulate to their respective targets in the body.
- ACTH (Adrenocorticotropic hormone): This hormone is a tropic hormone as it regulates cortisol and androgen production to the adrenal cortex. Cortisol or stress hormones stimulates the release of ACTH, while the adrenal cortex secretes glucocorticoids to the body�s metabolism.
- GH (Growth hormone): This hormone helps regulate the body�s growth, metabolism, and composition. GH is secreted by the somatotroph cells located primarily in the lateral wings of the anterior lobe. GH can also secrete in al pulsatile fashion and can have a maximal release during a circadian rhythm at night.
- TSH (Thyroid stimulating hormone): This hormone is involved by coordinating the signal regulation of the hypothalamus, the pituitary, and the thyroid. It requires the oxidation of dietary iodine, since iodine is absorbed through the small intestine and transported to the thyroid. After the iodine is transported it can be concentrated, oxidized and then incorporated into thyroglobulin to be formed to T4 and T3 later on.
- LH (Luteinizing hormone): This hormone is highly important to both men and women, since it affects the sex organs and plays a role in puberty, menstruation and fertility. For women, it creates progesterone, which help regulate menstruation and supports pregnancy in the female body. For men, it creates testosterone, which helps regulates fertility, muscle mass, fat distribution, and red blood production in the male body.
- FSH (Follicle stimulating hormone): This hormone plays an important part in the reproductive system and is responsible for ovarian follicles. For females, FSH helps produce estrogen, which is a group of sex hormones that help promote the development and maintenance of female characteristics in the human body, For males, FSH helps produce spermatogenesis and regulates sperm function in the male body.
- Prolactin: This is a protein hormone in the anterior lobe. It has the ability to promote lactation to nursing mothers. It synthesizes within the pituitary gland, the central nervous system, the immune system, and the uterus.
Intermediate lobe
The intermediate lobe is composed of a homogeneous population of the endocrine cells, the melanotrophs and secretes several bioactive peptides. It contains very few blood vessels and can be virtually avascular. The melanotrophs are richly supplied by nerve fibers that originate from the hypothalamus.
- Melanocyte-stimulating hormone: This hormone has many functions in a diverse physiological role. It affects skin pigmentation and studies have shown that it has antiapoptotic and anti-inflammatory effects that help decrease in nephrotoxin exposure to the body.
Posterior lobe
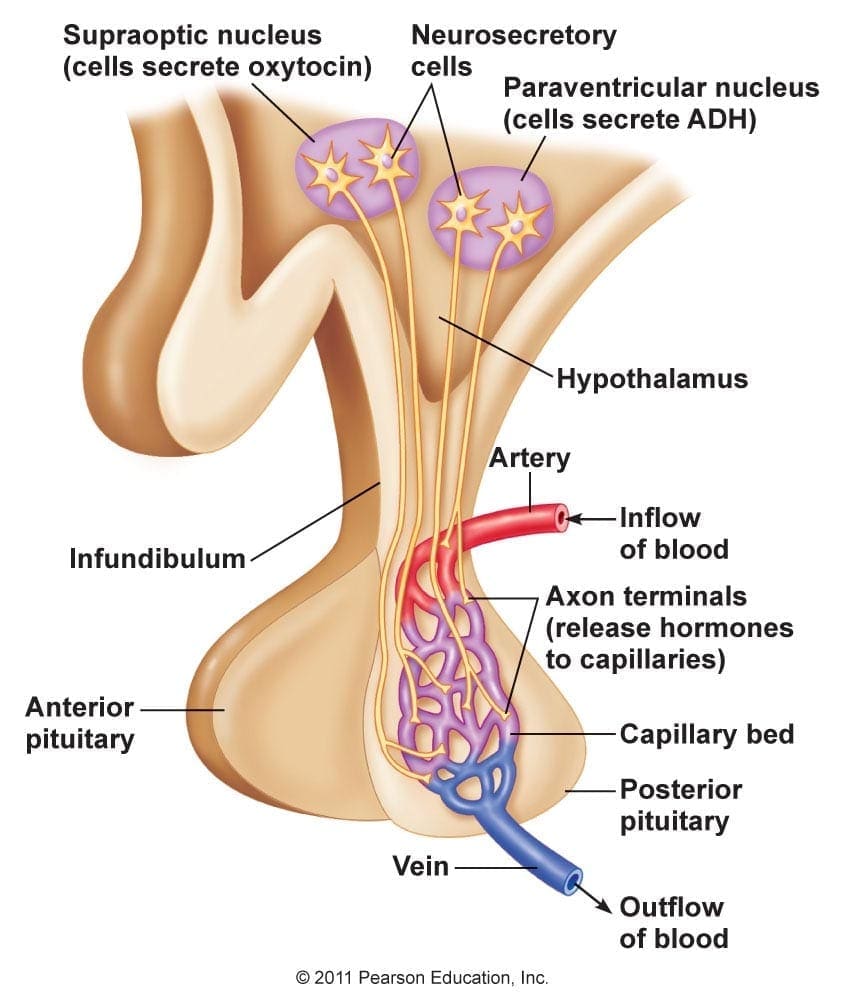
The posterior lobe is similar to the anterior lobe since they both control endocrine function and the body�s hormonal response to the environment. The hypothalamus receives neural signals from the brain and secretes polypeptide and neuropeptide hormones for storage in the posterior lobe until they are ready to be released. The hormones in the posterior lobe are in charge of regulating water retention and inducing uterine contractions.
- ADH (Antidiuretic hormone): Also known as vasopressin, this hormone is a nonapeptide that is synthesized in the hypothalamus. It plays a bunch of important roles in controlling the body�s osmotic balance, regulates blood pressure, and makes sure that the kidneys are working. ADH is mainly responsible for tonicity homeostasis as they act primarily in kidneys to increase water reabsorption.
- Oxytocin: Also known as the �love hormone�, oxytocin is also a neurotransmitter that is involved in childbirth and breast-feeding. It has benefits as a treatment for a number of conditions like depression, anxiety and intestinal problems and is produced in the hypothalamus. Studies show that females have a higher level of oxytocin than males, especially to nursing mothers with their babies.
Free-fraction Hormones
When an endocrine gland synthesizes a hormone, it is released into circulation and bound to as a protein. Hormones attach themselves to proteins but they can�t bind to hormone receptors. So what a hormone needs to do is to lose its binding protein to become a �free-fraction� hormone. Studies have stated that a fraction of a hormone that is free is called in vitro and it is equivalent to the fraction of a hormone that is free and available to be transported into tissues are called in vivo. Free-fraction hormones make up less than 1% of all circulating hormones since they don�t impact the hypothalamus-pituitary feedback loop.
Hormone Metabolites
Hormones are metabolized by hepatic and microbiome biotransformation pathways into various hormone metabolites. Hormone metabolites have their own impact on cell receptors, studies have shown that this impact is not fully understood yet but hormone metabolites are not a reflection of direct endocrine gland production but it can be metabolized in the liver as well. Hormone metabolites can bind to hormone receptors or can be eliminated by renal or fecal clearance pathways.
Conclusion
All in all, the body secretes and circulates 50 different hormones to different organs in the body. These hormones are chemically produced in the body and keep an eye on what each of the different organs is doing. It is important that the hormone receptors are functioning properly so that an individual is feeling good both inside and out. If there is a hormonal imbalance in the body, it can cause dysfunction and chronic illnesses to a person.
October is Chiropractic Health Month. To learn more about it, check out Governor Abbott�s proclamation on our website to get full details on this declaration.
The scope of our information is limited to chiropractic, musculoskeletal and nervous health issues as well as functional medicine articles, topics, and discussions. We use functional health protocols to treat injuries or chronic disorders of the musculoskeletal system. To further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900 .
References:
Allen, Mary J. �Physiology, Adrenocorticotropic Hormone (ACTH).� StatPearls [Internet]., U.S. National Library of Medicine, 3 Mar. 2019, www.ncbi.nlm.nih.gov/books/NBK500031/.
Clinic, Cleveland. �Overactive Pituitary Gland & Hyperpituitarism.� Cleveland Clinic, 22 Mar. 2017, my.clevelandclinic.org/health/diseases/15173-pituitary-gland–hyperpituitarism-overactive-pituitary-gland.
Cuzzo, Brian. �Vasopressin (Antidiuretic Hormone, ADH).� StatPearls [Internet]., U.S. National Library of Medicine, 2 Feb. 2019, www.ncbi.nlm.nih.gov/books/NBK526069/.
Ellis, Mary Ellen, and Rachel Nall. �Luteinizing Hormone (LH) Test: What It Is and Why It’s Important.� Healthline, 29 Aug. 2017, www.healthline.com/health/lh-blood-test.
Ellis, Ronald E, and Gillian M Stanfield. �The Regulation of Spermatogenesis and Sperm Function in Nematodes.� Seminars in Cell & Developmental Biology, U.S. National Library of Medicine, May 2014, www.ncbi.nlm.nih.gov/pmc/articles/PMC4082717/.
Freeman, M E, et al. �Prolactin: Structure, Function, and Regulation of Secretion.� Physiological Reviews, U.S. National Library of Medicine, Oct. 2000, www.ncbi.nlm.nih.gov/pubmed/11015620.
Genes, S G. �Role of the Liver in Hormone Metabolism and in the Regulation of Their Content in the Blood.� Arkhiv Patologii, U.S. National Library of Medicine, 1977, www.ncbi.nlm.nih.gov/pubmed/334126.
Goyal, Shikha. �List of Important Hormones and Their Functions.� Jagranjosh.com, 12 Mar. 2019, www.jagranjosh.com/general-knowledge/list-of-important-hormones-and-their-functions-1516176713-1.
Gunawardane, Kavinga. �Normal Physiology of Growth Hormone in Adults.� Endotext [Internet]., U.S. National Library of Medicine, 12 Nov. 2015, www.ncbi.nlm.nih.gov/books/NBK279056/.
Hadley, M E, et al. �Biological Actions of Melanocyte-Stimulating Hormone.� Ciba Foundation Symposium, U.S. National Library of Medicine, 1981, www.ncbi.nlm.nih.gov/pubmed/6268380.
Lamacz, M, et al. �The Intermediate Lobe of the Pituitary, Model of Neuroendocrine Communication.� Archives Internationales De Physiologie, De Biochimie Et De Biophysique, U.S. National Library of Medicine, June 1991, www.ncbi.nlm.nih.gov/pubmed/1717055.
Lee, Heon-Jin, et al. �Oxytocin: the Great Facilitator of Life.� Progress in Neurobiology, U.S. National Library of Medicine, June 2009, www.ncbi.nlm.nih.gov/pmc/articles/PMC2689929/.
M., William. �Transport of Protein-Bound Hormones into Tissues in Vivo *.� OUP Academic, Oxford University Press, 1 Jan. 1981, academic.oup.com/edrv/article-abstract/2/1/103/2548700?redirectedFrom=fulltext.
MacGill, Markus. �Oxytocin: The Love Hormone?� Medical News Today, MediLexicon International, 4 Sept. 2017, www.medicalnewstoday.com/articles/275795.php.
MacGill, Markus. �Testosterone: Functions, Deficiencies, and Supplements.� Medical News Today, MediLexicon International, 6 Feb. 2019, www.medicalnewstoday.com/articles/276013.php.
Nichols, Hannah. �Estrogen: Functions, Uses, and Imbalances.� Medical News Today, MediLexicon International, 2 Jan. 2018, www.medicalnewstoday.com/articles/277177.php.
Patel, Hiran. �Physiology, Posterior Pituitary.� StatPearls [Internet]., U.S. National Library of Medicine, 27 Oct. 2018, www.ncbi.nlm.nih.gov/books/NBK526130/.
Rawindraraj, Antony D. �Physiology, Anterior Pituitary.� StatPearls [Internet]., U.S. National Library of Medicine, 25 Apr. 2019, www.ncbi.nlm.nih.gov/books/NBK499898/.
Researchers, Various. �Thyroid Hormone Synthesis.� Thyroid Hormone Synthesis – an Overview | ScienceDirect Topics, 2019, www.sciencedirect.com/topics/medicine-and-dentistry/thyroid-hormone-synthesis.
Rousset, Bernard. �Chapter 2 Thyroid Hormone Synthesis And Secretion.� Endotext [Internet]., U.S. National Library of Medicine, 2 Sept. 2015, www.ncbi.nlm.nih.gov/books/NBK285550/.
Seladi-Schulman, Jill. �Everything You Need to Know About Progesterone.� Healthline, 29 Apr. 2019, www.healthline.com/health/progesterone-function.

by Dr Alex Jimenez | Functional Medicine, Health, Wellness
The endocrine system is a network of glands and organs surrounding the body. While it is similar to the nervous system, it plays a vital role in controlling and regulating many body functions, as well as using chemical messengers called hormones. Since hormones circulate throughout the entire body, each type of hormone targets specific organs and tissues. The whole system is made up of glands and organs that release hormones into the body. Each has a different function to make sure that the human body is working correctly. If there is a disruption in one of the organs, it can cause problems and possibly lead to chronic illnesses later on.
Functioning The Endocrine System
In the endocrine system, it is responsible for regulating the body through the release of hormones. These hormones are secreted by the glands that travel through the bloodstream to various organs and tissues, telling them what to do or how to function in the body properly. Some of the bodily functions are controlled by the endocrine system. This includes the body�s metabolism, growth and development, heart rate, blood pressure, body temperature, appetite, and sleeping and waking cycles.

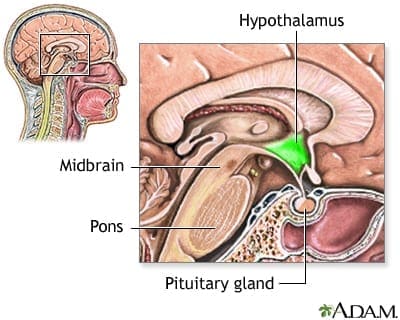
Studies have shown that the endocrine and the nervous system work closely together since the brain continuously sends instructions to the endocrine system while returning the favor, the endocrine glands receive feedback to the brain. With an intimate relationship, both methods are referred to as the neuroendocrine system. The neuroendocrine system is a mechanism where the hypothalamus maintains homeostasis, regulates reproduction, metabolism, and blood pressure. The neuroendocrine system works together with the immune system as they play an essential role in maintaining and restoring homeostasis in the body to function correctly.
The Organs of the Endocrine System
The endocrine system has a complex network of glands that secrete substances. The glands produce, store, and release throughout the body, targeting specific organs and tissues. Here are what each gland does in the endocrine system and what their functions are in the body.
Hypothalamus
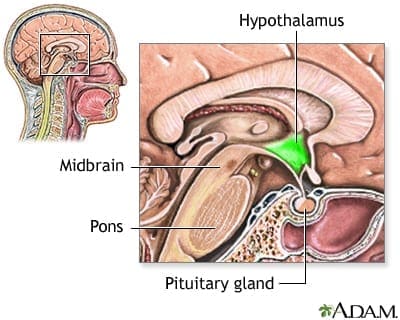
The hypothalamus gland is known as the master switchboard located in the center of the brain. Its role is significant because it controls and creates many hormones in the body. It also makes sure that it has to keep the body in a homeostasis state as much as possible. If the hypothalamus is not working correctly, it can cause problems for the body, and it can lead to a wide range of rare disorders.
Pituitary
The pituitary gland is known as the master gland due to regulating the other endocrine glands activities. It plays an essential role by balancing hormone levels in the body, and together with the hypothalamus gland, they control the involuntary nervous system. This system helps manage the balance of the energy, heat, and water in the body. The pituitary gland also produces several hormones that can either regulate most of the other hormone glands or a direct effect on specific organs. When the endocrine glands produce too little or an excessive quantity of hormones, it can cause the body to be imbalanced.
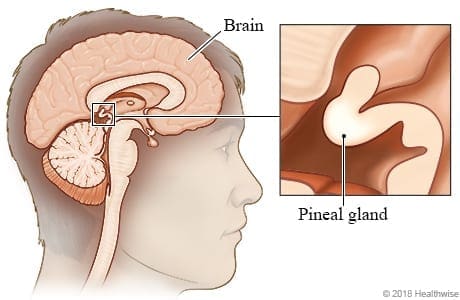
Pineal
The pineal gland is a small, pea-shaped gland that is in the brain and is sometimes called �the third eye.� It plays a role in producing and regulates hormones in females that may affect fertility and the menstrual cycle, including producing and excreting melatonin in the body. A 2016 study suggests that melatonin can help protect against cardiovascular diseases; however, there is still more research being done about the potential function of melatonin in the body.
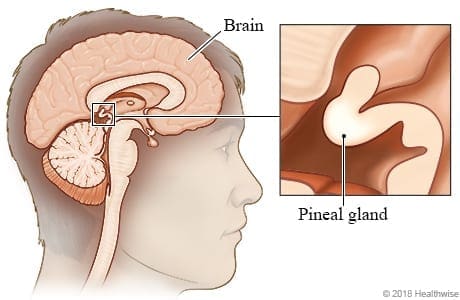
When the pineal gland is not producing the correct amount of melatonin, it can cause an individual to have sleep disorders and accumulate an excessive quantity of calcium in the body. One of the most prominent symptoms that can cause pineal gland dysfunction is a change in circadian rhythms. A person can disrupt their circadian rhythm either sleeping too much or too little, having restless nights, and feeling sleepy at unusual times.
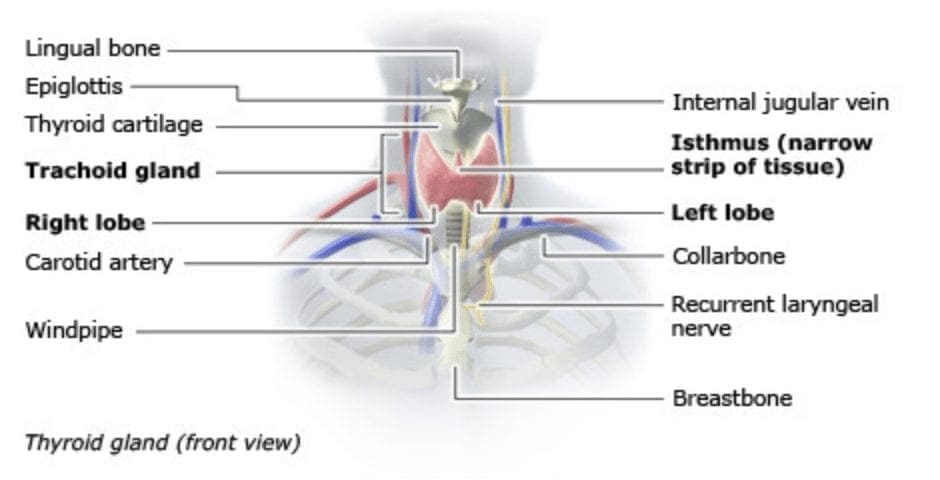
Thyroid
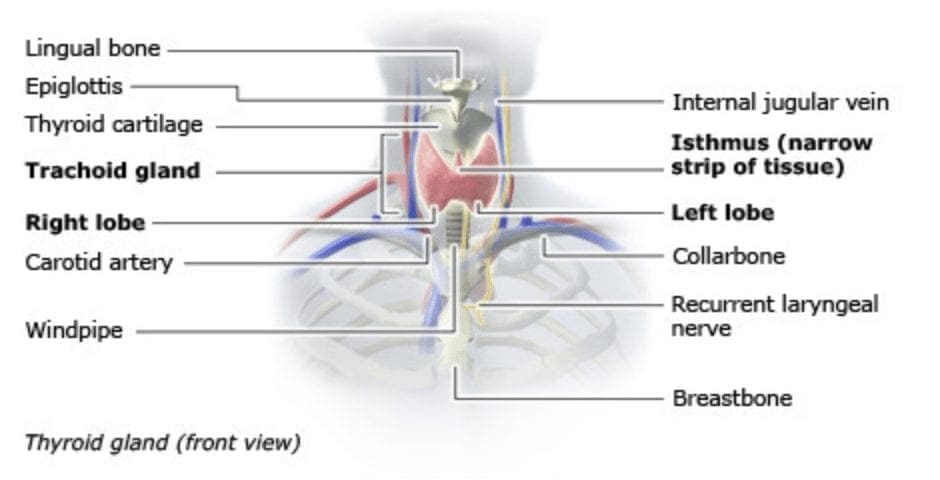
The thyroid gland a butterfly wing-shaped gland that is located in the anterior neck. It plays a huge vital role in the metabolism, growth, and development of the human body. It regulates many body functions by constantly releasing a steady amount of hormones in the bloodstream. When the thyroid produces too much or too little hormones, it can cause hyperthyroidism and hypothyroidism in the body, causing many chronic illnesses in the body.
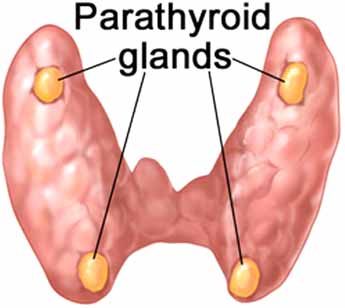
Parathyroid
The parathyroid gland is located behind the thyroid and plays a vital role in maintaining bone health, making sure the nervous system is running smoothly, and that muscles are pumping regularly. Parathyroid glands release PTH (parathyroid hormone), which regulates calcium in the bloodstream. Research shows that calcium is the only mineral in the body that has its very own dedicated regulatory gland. Calcium not only helps with bone strength, but it conducts electrical impulses in the nervous system and its energy in muscle cells. The PTH can also signal the kidneys and small intestines to save calcium from being digested.
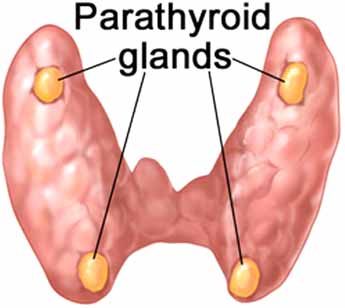
When the parathyroid gland produces an excessive amount or a decreased amount of PTH, it can cause hyperparathyroidism and hypoparathyroidism leading the body to have many malfunctions, including weak bones in the body.
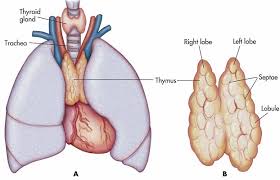
Thymus
The thymus gland is known as �the forgotten, but very important organ.� �It produces progenitor cells, which matures into T-cells and helps the organs in the immune system to grow properly. According to an article published by the NLM (U.S. National Library of Medicine), it stated that the thymus is the primary cell donor for the lymphatic system.
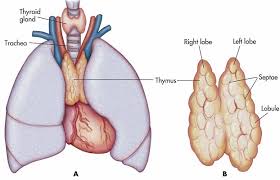
One of the most common diseases that can cause thymus dysfunction is MG (myasthenia gravis), PRCA (pure red cell aplasia), and hypogammaglobulinemia. These diseases can attack the body and cause chronic illnesses in the immune system.
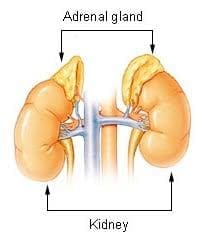
Adrenal
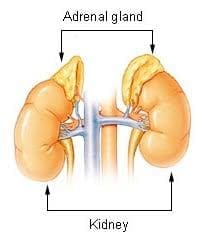
The adrenal glands are located on the top of the kidneys and help produce sex hormones and cortisol, they even work together with the pituitary glands. When cortisol is released from the adrenal glands, it can help with the response to stress and many essential functions in the body. When abnormal signals are disrupting the number of hormones that the pituitary glands telling the adrenal glands to produce. It can cause vitamin D to unbalance and many chronic illnesses.
Pancreas
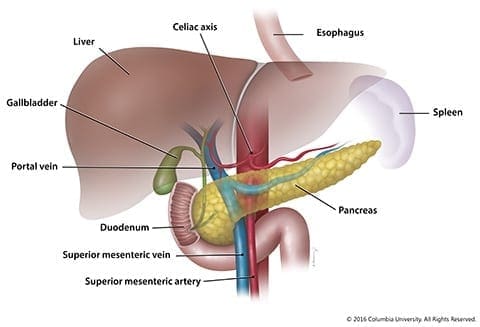
The pancreas is located in the abdomen and is part of the digestive system. It produces insulin, essential enzymes, and hormones that help break down food and sends it to the small intestine. When the pancreas produces the insulin hormone, it secretes it into the bloodstream, regulating the body�s glucose levels. There are many problems if the pancreas is not functioning correctly, causing the entire body to malfunction. If the pancreas is not producing enough insulin in the body, an individual is at risk for diabetes. Another factor is the development of pancreatic cancer caused by smoking or heavy drinking. The best way to keep a healthy pancreas is to maintain a healthy balanced diet.
Conclusion
The endocrine system is a network of glands and organs that surrounds the body. Each gland sends out hormones throughout the body and transfers to the specific organs that need these hormones to function correctly. If there is a disruption in the endocrine system, it can cause the body to malfunction and develop chronic illnesses.
October is Chiropractic Health Month. To learn more about it, check out Governor Abbott�s declaration on our website to get full details on this proclamation.
So the mechanisms of an autoimmune disease can be either by genetics or by environmental factors that can cause an individual to have problems in their body. There are many autoimmune diseases, both common and rare, that can affect the body. The scope of our information is limited to chiropractic, musculoskeletal and nervous health issues as well as functional medicine articles, topics, and discussions. We use functional health protocols to treat injuries or chronic disorders of the musculoskeletal system. To further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900 .
References:
Bradford, Alina. �Parathyroid Glands: Facts, Function & Disease.� LiveScience, Purch, 5 May 2017, www.livescience.com/58980-parathyroid-glands.html.
Cherney, Kristeen. �Adrenal Glands.� Healthline, 26 July 2016, www.healthline.com/health/adrenal-glands.
Chu, Linda C, et al. �Diagnosis and Detection of Pancreatic Cancer.� Cancer Journal (Sudbury, Mass.), U.S. National Library of Medicine, 2017, www.ncbi.nlm.nih.gov/pubmed/29189329.
Crosta, Peter. �Pancreas: Functions and Disorders.� Medical News Today, MediLexicon International, 26 May 2017, www.medicalnewstoday.com/articles/10011.php.
Duggal, Neel. �5 Functions of the Pineal Gland.� Healthline, 7 Apr. 2017, www.healthline.com/health/pineal-gland-function.
Imrich, Richard. �The Role of Neuroendocrine System in the Pathogenesis of Rheumatic Diseases (Minireview).� Endocrine Regulations, U.S. National Library of Medicine, June 2002, www.ncbi.nlm.nih.gov/pubmed/12207559.
Johnson, Jon. �Hypothalamus: Function, Hormones, and Disorders.� Medical News Today, MediLexicon International, 22 Aug. 2018, www.medicalnewstoday.com/articles/312628.php.
Mannstadt, Michael, et al. �Hypoparathyroidism.� Nature Reviews. Disease Primers, U.S. National Library of Medicine, 31 Aug. 2017, www.ncbi.nlm.nih.gov/pubmed/28857066.
N/A, Uknown. �Circadian Rhythms.� National Institute of General Medical Sciences, U.S. Department of Health and Human Services, Aug. 2017, www.nigms.nih.gov/education/pages/factsheet_circadianrhythms.aspx.
Rosenow, E C, and B T Hurley. �Disorders of the Thymus. A Review.� Archives of Internal Medicine, U.S. National Library of Medicine, Apr. 1984, www.ncbi.nlm.nih.gov/pubmed/6608930.
Seladi-Schulman, Jill. �Endocrine System Overview.� Healthline, 22 Apr. 2019, www.healthline.com/health/the-endocrine-system.
Sun, Hang, et al. �Effects of Melatonin on Cardiovascular Diseases: Progress in the Past Year.� Current Opinion in Lipidology, Lippincott Williams & Wilkins, Aug. 2016, www.ncbi.nlm.nih.gov/pmc/articles/PMC4947538/.
Tirabassi, Giacomo, et al. �Adrenal Disorders: Is There Any Role for Vitamin D?� Reviews in Endocrine & Metabolic Disorders, U.S. National Library of Medicine, Sept. 2017, www.ncbi.nlm.nih.gov/pubmed/27761790.
Unknown, Unknown. �How Does the Pituitary Gland Work?� InformedHealth.org [Internet]., U.S. National Library of Medicine, 19 Apr. 2018, www.ncbi.nlm.nih.gov/books/NBK279389/.
Unknown, Unknown. �How Does the Thyroid Gland Work?� InformedHealth.org [Internet]., U.S. National Library of Medicine, 19 Apr. 2018, www.ncbi.nlm.nih.gov/books/NBK279388/.
Villines, Zawn. �Pineal Gland Function: Definition and Circadian Rhythm.� Medical News Today, MediLexicon International, 1 Nov. 2017, www.medicalnewstoday.com/articles/319882.php.
Vorvick, Linda J., et al. �Endocrine Glands – Health Video: MedlinePlus Medical Encyclopedia.� MedlinePlus, U.S. National Library of Medicine, 10 May 2019, medlineplus.gov/ency/anatomyvideos/000048.htm.
Yuen, Noah K, et al. �Hyperparathyroidism of Renal Disease.� The Permanente Journal, The Permanente Journal, 2016, www.ncbi.nlm.nih.gov/pubmed/27479950.
Zdrojewicz, Zygmunt, et al. �The Thymus: A Forgotten, But Very Important Organ.� Advances in Clinical and Experimental Medicine : Official Organ Wroclaw Medical University, U.S. National Library of Medicine, 2016, www.ncbi.nlm.nih.gov/pubmed/27627572.