by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chiropractic, Chronic Back Pain, Migraines, Neck Pain
About Pain Management (Medicine) Specialists
A pain medicine specialist is a medical or osteopathic doctor who treats pain due to disease, ailment, or injury. Many of these doctors are physiatrists or anesthesiologists although called interventional pain management specialists or pain medicine. Pain medicine is a mutlidisciplinary team effort generally affecting specialists in other disciplines, complimentary alternative medicine, along with radiology, psychiatry, psychology, oncology, nursing, physical therapy, and the patient’s primary care physician or other treating doctor.

Education & Training
After graduating medical school and completing a one-year internship, the physician enters a residency program normally in physical or anesthesiology medicine but sometimes from other fields like psychiatry and neurology. Upon conclusion of a residency program (typically 3 years long), the physician completes a one-year fellowship for advanced training in pain medicine.
Many pain medicine specialists are board certified. The organizations that board certify physiatrists, anesthesiologists, neurologists, and psychiatrists all collaborate to provide the board examination for the subspecialty of Pain Medicine. You can find numerous opportunities for pain management specialists to remain current with medical and technical improvements in pain medicine, such as scientific journals and society meetings.
Targets of Pain Management
The goal of pain medicine is to handle severe or long-term pain by reducing intensity and pain frequency. Besides addressing pain problems, a multidisciplinary pain management program may address your functional goals for activities of day-to-day living. Overall, a pain medicine plan aims to give you a feeling of well-being, increase your level of action (including return to work), and reduce or eliminate your reliance on drugs.
Many Kinds of Pain Treated
Pain medicine specialists treat all sorts of pain. Severe pain is described sharp or as acute and may indicate something is wrong. The pain experienced during dental work is an instance of intense pain. Pain lasting 6 months or longer is defined as chronic. This type of pain varies from mild to serious and is consistent. Spinal arthritis (spondylosis) pain is frequently chronic. A good consequence is produced by uniting different treatments regularly although chronic pain is difficult to handle.
- Degenerative disc disease
- Facet joint pain
- Sciatica
- Cervical and lumbar spinal stenosis
- Spondylolisthesis
- Whiplash
What to Anticipate During an Appointment
Your appointment with a pain or interventional pain management practitioner is much like other doctor visits. Although there are many similarities, the focus is fast managing it, and on your pain, the cause or contributing factors.
Pain medicine physicians execute a physical and neurological examination, and review your medical history paying particular focus on pain history. You may be asked many questions about your pain
- On a scale from zero to 10, with 10 being the worse pain imaginable, speed your pain.
- When did pain start? When pain started, what were you doing?
- Does pain disperse into other regions of the body?
- Is its intensity persistent, or is it worse at different times of night or the day?
- What really helps to alleviate the pain? Why is pain worse?
- What treatments have you ever attempted? What worked? What failed?
- Would you take over the counter drugs, vitamins, or herbal nutritional supplements?
- Does one take prescription medication? If so, what, how much, and how frequently?
Most pain medicine specialists utilize a standardized drawing of the front/back of the body to let you mark where pain is sensed, as well as indicate pain spread and type (eg, light, sharp). You may be asked to complete the form each time you see with the pain physician. The finished drawing helps you to evaluate your treatment progress.
Accurate Analysis Key to Treatment
Pain medicine includes diagnosing origin or the cause of pain. Making the proper identification may include getting an X ray, CT scan, or MRI study to verify the reason for your neck pr back pain. When treating spine-associated pain (which may include arm or leg symptoms), other tests, like discography, bone scans, nerve studies (electromyography, nerve conduction study), and myelography could possibly be performed. The proper analysis is crucial to some favorable treatment plan.
Some spinal ailments and pain treatment requires involvement of other specialists, such as your primary care physician, neurosurgeon, orthopaedic surgeon, and practitioners in radiology, psychiatry, psychology, oncology, nursing, physical therapy, and complimentary alternative medicine. The pain medicine specialist may consult with and/or refer you to a neurosurgeon or orthopaedic spine surgeon to determine if your pain difficulty necessitates back operation.

Call Today!
by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chiropractic, Chronic Back Pain, Integrative Functional Wellness, Integrative Medicine, Wellness
If It Sounds Too Good to Be True�
When you�re in pain, you might try just about anything to feel better. Claims of miracle cures that instantly relieve back and neck pain are tempting, but they often fall short of their promises.
Save your money and steer clear of the products featured promising to eliminate your spine-related pain.
Copper Bracelets

Copper bracelets and wristbands have attracted a following of arthritis sufferers because of their perceived ability to reduce joint pain.
The key word here is perceived.
A 2013 study in the UK examining the effects of copper bracelets in patients with rheumatoid arthritis found no difference in pain outcomes between those wearing copper bracelets and those using a placebo.
While the bracelets won�t do you any harm, they�re more for looks than clinical benefit. There�s no solid medical evidence available proving they reduce pain or inflammation.
Magnets
From magnetic shoe inserts to bandages, magnets have been heavily marketed as a miracle cure to zap away a variety of back pain conditions, including fibromyalgia and arthritis. However, no proof exists to back up magnets� health claims.
While studies have examined magnets� impact on pain, the results are mixed�and the quality of some of the research is questionable. Additionally, magnets are not safe for some people, including those who use pacemakers or insulin pumps.
Colloidal Silver
Silver jewelry? Classic. Silver home furnishings? Sure thing. Colloidal silver for your spine pain? Never a good idea.
Colloidal silver for back pain is typically found as a topical cream containing small particles of silver. In 1999, the U.S. Food and Drug Administration (FDA) recommended that people not use colloidal silver to treat any medical condition because it�s neither safe nor effective.
Even worse than the false claims of back and neck pain relief are colloidal silver�s strange and serious side effects. This product can interfere with the absorption of some prescription drugs and even permanently tint your skin a blue-gray color.
DMSO and MSM Dietary Supplements

If you have spondylosis (osteoarthritis), you may have heard of the dietary supplements dimethyl sulfoxide (DMSO) and methylsulfonylmethane (MSM). Some believe this pair of supplements can block pain and inflammation, but no real medical evidence shows these substances actually relieve painful arthritis symptoms.
Instead of eliminating your arthritis pain, MSM and DMSO might cause some unwanted side effects. Both have been linked to causing upset stomach and skin rashes, while DMSO may also leave you with garlic breath and body odor.
A Word on Drug-Supplement Interactions

Speaking of supplements, it�s important to understand that dietary supplements may not mix with over-the-counter or prescription drugs. Some interactions result in mild side effects, but others can be much more serious�even life-threatening.
If you�re using a dietary supplement�even if it�s a seemingly benign herbal or vitamin�always let your doctor and pharmacist know before taking it with an over-the-counter or prescription medication. They will share any dangerous interactions, and ensure you�re safely addressing your back and neck pain.
The Real Deals: Alternative Treatments that Work
Many who fall prey to the products listed in this slideshow have an interest in alternative or complementary therapies for back and neck pain. While some non-traditional treatments should be avoided, many have been proven to reduce spine pain.
Scientists from the National Center for Complementary and Integrative Health at the National Institutes of Health reviewed 105 U.S.-based trials from the past 50 years that included more than 16,000 participants. They found the therapies below effective at controlling pain:
� Acupuncture � Massage � Relaxation techniques � Tai chi
If you prefer alternative methods to manage for your spinal condition, explore the therapies above. They are effective, safe, and will help you live a healthier life.

Call Today!
by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chronic Back Pain, Lower Back Pain, Mobility & Flexibility
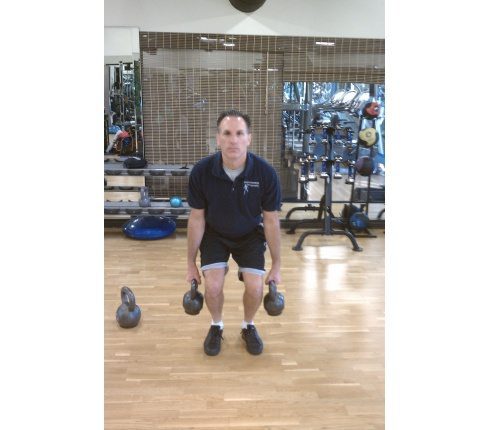
Kettlebells Strengthen the Spine
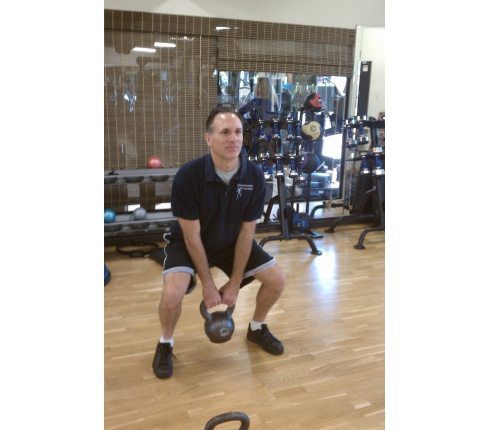
Strengthening the spinal muscles is essential for health and fitness. Functional kettlebell training is resistance training that strengthens the spine. Kettlebell training is an extremely effective type of exercise to increase functional strength, ballistic power, endurance, and flexibility in the entire body, especially the spinal and core muscles.
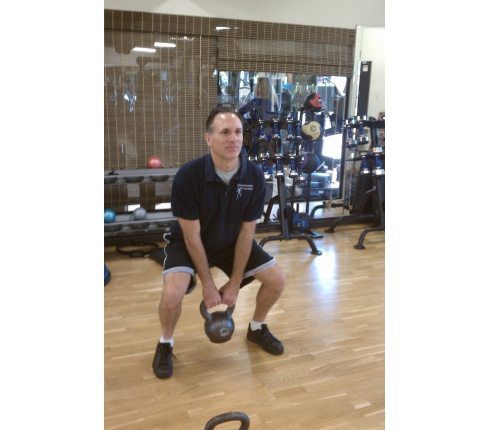
(Exercise shown is Anchor Squats.)
What Exactly Are Kettlebells?
Kettlebells are round cast iron weights with a single handle. Picture a cannonball with a u-shaped handle. Kettlebells are manufactured in a wide range of weights, for all strength levels.

Muscles Used in Kettlebell Training
Kettlebell training incorporates large functional movements. Multiple muscle groups work in synergy to complete the exercises. The spinal muscles function as either the primary mover or assist the primary mover in every kettlebell exercise. The spinal muscles also stabilize the body during functional kettlebell training, thus developing the smaller supporting structures.
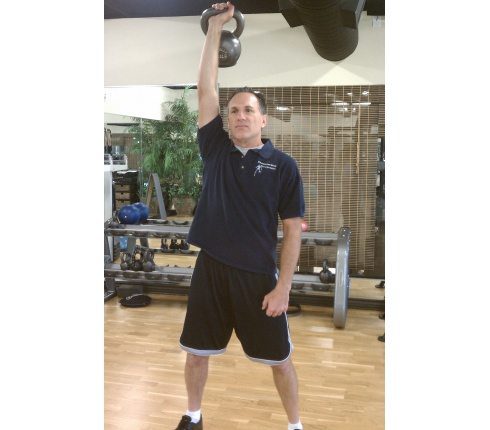
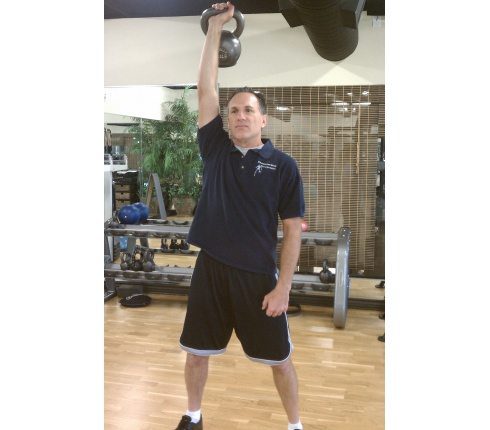
(Exercise shown is Push Press.)
High Reps Of High Importance In Kettlebell Training
Kettlebell training employs high repetitions, momentum, and centrifugal force. Momentum works the spinal muscles as the weight is raised and lowered. High repetitions combined with momentum and full body movement build strength and endurance in the entire musculoskeletal and cardio-vascular systems. Kettlebell training delivers aerobic and anaerobic benefits.

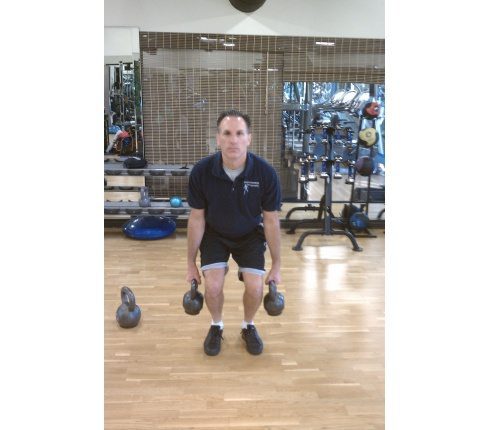
(Exercise shown is High Pulls.)
Always Learn From A Qualified Kettlebell Instructor
Perfect technique is mandatory during exercise. Correct exercise technique maximizes benefit and lowers injury risk. Poor exercise form increases the possibility of injury and diminishes results. Kettlebell exercises are learned motions, so you should learn proper training technique from a qualified kettlebell trainer. The trainer should demonstrate, instruct, and supervise your training and develop your routine.

(Exercise shown is Turkish Get-up.)
So Many Possibilities
The kettlebell�s shape allows for a wide variety of exercises. This resourceful exercise tool is used for basic exercises like squats (shown in slide 1), cleans, swings, high pulls (shown in slide 4), snatches and push presses (shown in slide 3). The versatility of the kettlebell is demonstrated with exercises such as renegade rows (a combination of push-ups and rows�shown in slide 6), suitcase swings, woodchoppers (a combination of lunges and oblique twists), windmills, and Turkish get-ups (shown in slide 5)

(Exercise shown is Renegade Rows.)
Kettlebell’s Benefits For The Spine
Functional kettlebell training is a rare type of exercises that increases aerobic and anaerobic health simultaneously. The benefits to the spine include increased strength, power, endurance, flexibility, function and mobility.
(Exercise shown is Suitcase Swings.)

Call Today!

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | UTEP (Local) RSS
Related Articles
The UTEP softball team will travel to Ruston to take on Conference USA West Division foe LA Tech April 14-15. Friday�s doubleheader will start at 2 p.m. CT/ 1 MT, while Saturday�s series finale will start at noon CT/ 11 a.m. MT.
The Miners (11-28, 5-10 C-USA) are currently tied with Southern Miss (5-10), while standing one game behind UTSA (6-9) in the West Division. The Lady Techsters (26-14, 9-3 C-USA West) are in first place and currently the no. 2 seed behind Marshall (14-1 East). FIU (8-4 East), Florida Atlantic (7-5 East), North Texas (8-7 West), Charlotte (5-7 East), WKU (6-9 East) and UTSA round out the standings. Middle Tennessee sits in last place (3-9 East).
The top eight schools, out of 12, will advance to the C-USA Tournament in Hattiesburg, Miss, May 10-13. The top three teams from each division, while the next two schools with the best records will advance to the four-day championship. Seeds three and four will receive a bye, while the top two seeds earn a double-bye to advance to the second day.
UTEP won game one against WKU, 10-2 (6), while recording 30 hits during the weekend series. The Miners and Hilltoppers game two scoring fest ranks most runs (26) between both teams in C-USA. The Miners are ranked second in C-USA in team batting average (.307), while their 329 hits rank second. Lindsey Sokoloski is ranked no. 1 in the nation in toughest to strikeout after a K-less weekend and Taylor Sargent is ranked 17th in the C-USA with a .349 batting average. Sargent was hitting .250 after March 26.
In the 2015, LA Tech took care of UTEP in three games, while the Miners returned the favor by sweeping the Lady Techsters in El Paso last season. In 2014, during Tobin Echo-Hawk�s first season, her squad swept LA Tech in Ruston as it was the first ever sweep of a conference opponent in program history.
The Miners will have their bye week following the LA Tech series and will continue play at UAB April 29-30, while the regular season will conclude in El Paso against Florida Atlantic May 6-7 (Senior Weekend).

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | UTEP (Local) RSS
Related Articles
IRVING, Texas- For his efforts toward a share of eighth place at the prestigious 71st Annual Western Intercollegiate, UTEP men�s golfer Charles Corner was named the Conference USA Golfer of the Week for the first time on Wednesday.
�He�s [Corner] been playing great all spring, I�m very happy for him,� head coach Scott Lieberwirth said. �To get a top-10 [finish] in an event that strong, that�s a huge confidence boost to continue on through the rest of the season. His game is right there and I�m convinced he�s got all the capability to breakthrough and even win the conference individually. The state of his game is in a great spot, as good as it�s been in the three years he�s been here.�
Climbing three spots after the final round, Corner spearheaded the Miners� charge at the Intercollegiate, firing a two-over-par 212 (72-69-71) to top his team�s scorecard and help the Miners to a seventh-place finish. The team bested No. 17 Texas, No. 25 Arizona State and No. 32 San Diego State after shooting 1,084 (361-356-367) in the 15-team field, which included eight nationally-ranked teams.
�A third of the way through the final round I heard I was in fourth place at one point and I just stuck to my game plan and kept doing my thing,� Corner said. �It came down to a pretty good score on the final day. It�s good to get those results, especially this time of the year when we need to finish off strong before conference, so its defiantly really positive and good for the team.�
Of the 96 players in the tournament, only three shot under par. Corner�s score was better than 19 players ranked in the Golfstat Top 100, including six of the top-10 players.
A junior from Cayuga, Ontario, Canada has recorded a 72.5 scoring average, third-best on the UTEP squad. He has tallied three top-10 finishes this year in 10 tournaments, with his work at the Western Intercollegiate marking the first time he was the top finisher for UTEP this year.
Corner is the third Miner to earn the C-USA Golfer of the Week honor this season. Andreas Sorensen earned his first recognition the week of September 14 and Frederik Dreier got the nod on October 19.
�It gives me and the team a lot of momentum,� Corner said. �We finished pretty well [at the Western Intercollegiate], we beat a lot of good schools that are ranked better than us so that�s always nice.�
Corner and the rest of the UTEP squad will head to the Conference USA Championships April 23-26 in Texarkana, Ark.
�I think everyone is pretty pumped up that we beat Texas and some high ranked teams, that�s only going to carry over and do good things for us. Those are some big wins, so its good for us to know we can compete against those [ranked] schools going into conference play.�

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chiropractic, Sciatica
Several lumbar spine (lower back) disorders may cause sciatica. Sciatica is usually referred to as light to severe pain in the left or right leg. Occasionally doctors call a radiculopathy that is sciatica. Radiculopathy is a medical term used to spell out pain, numbness, tingling, and weakness in legs or the arms caused by a nerve root issue. It’s known as a cervical radiculopathy, in the event the nerve difficulty is in the neck. But since sciatica influences the low back, it is called a lumbar.
Pathways To Sciatic Nerve Pain
Five sets of matched nerve roots in the lumbar spine combine to generate the sciatic nerve. Beginning at the rear of the pelvis (sacrum), the sciatic nerve runs in the trunk, under the buttock, and down through the hip region into each leg. Nerve roots aren’t “solitary” structures but are part of the entire body’s entire nervous system capable of transmitting pain and sensation to different parts of the body. Radiculopathy happens when compression of a nerve root from a disc rupture (herniated disc) or bone spur (osteophyte) happens in the lumbar spine prior to it joining the sciatic nerve.
What Causes Sciatic Nerve Compression?
Several spinal ailments can cause spinal nerve compression and sciatica or lumbar radiculopathy.
- spondylolisthesis
- Injury
- piriformis syndrome
- spinal tumors
Common Sciatica Cause #1: Lumbar Bulging Disc or Herniated Disc
A bulging disk is also called a contained disc illness. What this means is the gel-like center (nucleus pulposus) remains “included” within the tire-like outer wall (annulus fibrosus) of the disk.
A herniated disc happens when the nucleus breaks through the annulus fibrosus. It is called a “non-controlled” disk disorder. Whether a disc bulges or herniates, disk stuff compress delicate nerve tissue and cause sciatica and can press against an adjacent nerve root.
The effects of a herniated disc are worse. In both instances, nerve compression and irritation cause inflammation and pain, muscle weakness, tingling, and often ultimately causing extremity numbness.
Common Sciatica Cause #2: Lumbar Spinal Stenosis
Spinal stenosis is a nerve compression illness most frequently affecting older adults. Leg pain similar to sciatica may happen as an effect of lumbar spinal stenosis. The pain is generally positional, frequently brought on by actions like standing or walking and relieved by sitting down.
Spinal nerve roots branch outward through passageways in the spinal cord called neural foramina comprised of bone and ligaments. Between each group of vertebral bodies, located on the left and right sides, is a foramen. Nerve roots pass through these openings and extend outward to innervate other portions of the body. The term foraminal stenosis can be used when these passageways become clogged causing nerve compression or narrow.
Common Sciatica Cause #3: Spondylolisthesis
Spondylolisthesis is a disorder that almost all commonly influences the lumbar spine. It’s distinguished by one vertebra slipping forwards over an adjacent vertebra. When a vertebra slips and is displaced, spinal nerve root compression happens and frequently causes sciatic leg pain. Spondylolisthesis is categorized as developmental (located at birth, grows during childhood) or got from spinal degeneration, trauma or physical stress (eg, lifting weights).
Common Sciatica Cause #4: Trauma
Examples include motor vehicle accidents, falling down, football and other sports. The impact may injure the nerves or, sometimes, the nerves may compress.
Piriformis syndrome is named after the piriformis muscle and the pain caused when the sciatic nerve is irritated by the muscle. The piriformis muscle and the thighbone is found in the lower part of the spine, connect, and aids in hip rotation. The sciatic nerve runs beneath the piriformis muscle. Piriformis syndrome grows when muscle spasms develop in the piriformis muscle thereby compressing the sciatic nerve. It may be challenging to diagnose and treat because of the shortage of x ray or magnetic resonance imaging (MRI) findings.
Common Sciatica Cause #5: Piriformis Syndrome
Piriformis syndrome is named after the piriformis muscle when the muscle irritates the sciatic nerve and the pain caused. The piriformis muscle and the thighbone is located in the low part of the backbone, connect, and aids in hip rotation. When muscle spasms develop in the piriformis muscle thus compressing the sciatic nerve, piriformis syndrome develops. It can be hard to diagnose and treat due to the lack of x-ray or magnetic resonance imaging (MRI) findings.
Common Sciatica Cause #6: Spinal Tumours
Spinal tumors are abnormal growths which are either benign or cancerous (malignant). Fortunately, spinal tumors are uncommon. But when a spinal tumor develops in the lumbar region, there’s a risk for sciatica to grow as a result of nerve compression.
Call your doctor should you imagine you have sciatica. The very first step toward relieving pain is a proper diagnosis.

Call Today!
by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Fitness
(HealthDay News) — Healthy aging of the brain relies on the health of your heart and blood vessels when you’re younger, a new study reports.
People with risk factors for heart disease and stroke in middle age are more likely to have elevated levels of amyloid, a sticky protein known to clump together and form plaques in the brains of people with Alzheimer’s disease, the researchers said.
Amyloid In The Brain
MRI scans revealed larger deposits of amyloid in the brains of seniors who smoked, had high blood pressure, were obese, diabetic or had elevated cholesterol levels when they were middle-aged, said lead researcher Dr. Rebecca Gottesman. She’s an assistant professor of neurology at the Johns Hopkins University School of Medicine in Baltimore.
All of these risk factors can affect the health of a person’s blood vessels, otherwise known as vascular health, leading to hardening of the arteries and other disorders.
“Amyloid is what we think, by leading hypotheses, accumulates to cause Alzheimer’s disease. So this suggests that vascular risk in middle age may play a direct role in the development of Alzheimer’s disease,” Gottesman said.
Two or more risk factors nearly tripled a person’s risk of large amyloid deposits. One risk factor alone increased the likelihood of amyloid deposits by 88 percent, the study found.
Obesity
Obesity in particular stood out as a strong risk factor, on its own doubling a person’s risk of elevated amyloid later in life, said Steven Austad, chair of biology of aging and the evolution of life histories at the University of Alabama, Birmingham.
“In terms of one risk factor by itself, that turned out to be the most important one, which is interesting,” Austad said. “Twenty years ago obesity was not the problem that it is now, suggesting that 20 years from now things might be considerably worse.”
Gottesman and her colleagues examined data from nearly 350 people whose heart health has been tracked since 1987 as part of an ongoing study. The average age of the study participants was 52 at the start of the study. Sixty percent were women, and 43 percent were black. The average follow-up time was almost 24 years.
When the participants entered the study, none of them had dementia. About two decades later, they were asked to come back and undergo brain scans to check for signs of amyloid.
The researchers discovered a link between heart risk factors and brain amyloid. The relationship did not vary based either on race or known genetic risk factors for Alzheimer’s.
Poor Blood Vessel Upkeep
Heart risk factors that cropped up late in life were not associated with brain amyloid deposits. What a person does in their middle age is what apparently contributes to their later risk of elevated amyloid, not what happens later, Gottesman said.
The study did not prove a cause-and-effect relationship, but there are several theories why the health of a person’s blood vessels might be linked to Alzheimer’s.
Blood and spinal fluid contain amyloid, and some think that unhealthy blood vessels might allow amyloid to leak out of the bloodstream and into brain tissue, said Austad, a spokesman for the American Federation for Aging Research.
“The idea that the first injury to the brain is really an injury to the blood vessels of the brain has been around for a while, and this would support that, generally,” Austad said. “The amyloid plaques, you’re not seeing them inside the vessels. You’re seeing them outside the vessels, in the brain.”
Blood vessels also play a role in flushing out broken-down amyloid particles that naturally occur in a person’s brain, said Keith Fargo, director of scientific programs and outreach for the Alzheimer’s Association.
“You can imagine if there’s something wrong with your brain’s circulation, it could affect the clearance of this amyloid in some way,” Fargo said.
Hardened arteries also can lead to strokes or mini-strokes that affect the ability to think and remember in some people as they age, which contributes to dementia and Alzheimer’s, Gottesman said.
Based on these findings, people who want to protect their brain health should protect their heart health, and the sooner the better, Fargo said.
“You don’t want to wait until your 60s to start taking care of yourself. It has to be a lifetime commitment,” Fargo said.
The findings were published April 11 in the Journal of the American Medical Association.
SOURCES: Rebecca Gottesman, M.D., Ph.D., assistant professor of neurology, Johns Hopkins University School of Medicine, Baltimore; Steven Austad, Ph.D., chair of biology of aging and the evolution of life histories, University of Alabama, Birmingham, and scientific director, American Federation for Aging Research; Keith Fargo, Ph.D., director of scientific programs and outreach, Alzheimer’s Association; April 11, 2017, Journal of the American Medical Association
News stories are written and provided by HealthDay and do not reflect federal policy, the views of MedlinePlus, the National Library of Medicine, the National Institutes of Health, or the U.S. Department of Health and Human Services.