by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Functional Medicine, Natural Health, Remedies, Skin Health, Wellness
Summer’s officially just a week away, and millions of Americans are facing high odds of suffering from sunburn in coming months.
If you catch too many rays and wind up looking like a lobster, head straight to your kitchen. No kidding. Here are some surprising home remedies to soothe the burn that are as good as — or better than — commercially available skin creams and lotions:
Cucumbers: These vegetables are rich in vitamin C and caffeic acid, both of which help to soothe irritated skin and reduce swelling. Cukes also have compounds with analgesic properties to numb pain. You can slice cold cucumbers and apply them to burned areas. Better yet, make a paste by mashing or blending a couple of cucumbers and apply it chilled.
Lettuce: The greens have painkilling compounds that can take the sting out of sunburn. Boil the leaves in water, then strain and chill the liquid. Apply the fluid with cotton balls.
Potatoes: These tubers have been used throughout history to ease burns, bites, scrapes, and other skin problems. Blend one or two until they get pasty — you may have to add a splash of water — then chill the paste and apply via cotton balls.
Honey: This remedy for burns goes back to ancient Egyptian times. Honey reduces inflammation, provides nutrients to the damaged tissue and seals in moisture. It also has antiseptic properties. Just spread some of the sweet stuff where it hurts.
Apple cider vinegar: A common home remedy for a variety of problems from poison ivy to acid reflux to allergies, the cider also works on sunburn. You may want to dilute it a little since one of the active ingredients, acetic acid, may sting when applied. Use cotton balls or soak a washcloth in the solution for more coverage.
Coconut oil: You can use this for both protection — it has a sun protection factor (SPF) somewhere between 5 and 10 — and relief if you just stay out too long without any other sunscreen. Apply it directly to sunburned areas and you can feel its soothing effects as its medium-chain fats are absorbed into your skin and work their healing magic.
Oatmeal: Regular rolled oats will do just fine as the oatmeal’s polysaccharides will help to heal your skin. Put about 2 cups into a clean tube sock and add it to a tub of tepid water. Let it soak a few minutes, then climb in. Squeeze out the sock every few minutes, which will turn the water cloudy. When you’re done, air dry or pat yourself off gently with a soft towel.
Yogurt: Yogurt contains probiotics and proteins that will help to heal your skin. Make sure the yogurt is plain with no flavoring and also that it has live, active cultures. Spread it around the burned areas, let it sit for about five minutes, then rinse it off with tepid water.
Witch hazel: The tannins from the plant’s liquid extract reduce inflammation, kill bacteria and repair damaged skin. Use cotton balls or a clean cloth to dab it on sore areas. Reapply as needed.
Aloe vera: The gel from the fleshy leaves of this plant is rich in glyconutrients that soothe and heal all kinds of skin problems, including burns. Slice open a leaf and the gel will ooze out. Apply it directly to sunburned areas.
When suffering from sunburn, also be sure to drink plenty of water, because you’re probably dehydrated too. And try to avoid harsh soaps that will wash away the natural oils of your skin and further dry it out.
Of course, the best sunburn remedy is prevention. That means staying out of the sun during peak hours, typically between 10 a.m. and 2 p.m. And dermatologists strongly recommend wearing a hat, covering exposed areas with clothing and using sunscreen with a SPF of 15 or higher.
Look for sunscreen labeled “full spectrum” to make sure it screens out both UVA and UVB rays. But beware that a lot of sunscreens have toxic chemicals. Your best bet is to check out the Environmental Working Group’s Skin Deep database online to find the safest products.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Athletes, Complex Injuries, PUSH-as-Rx
Chiropractor, Dr. Alexander Jimenez gives insight into the relevant anatomy and functional biomechanics of the piriformis muscle, highlights the role it plays in musculoskeletal dysfunction and looks at management options in cases of muscle dysfunction.
The piriformis muscle (PM) is well-known in the fraternity of sports medicine as a significant muscle in the posterior hip. It is a muscle that has a role in controlling hip joint rotation and abduction, and it is also a muscle made famous due to its �inversion of action� in rotation. Furthermore, the PM also grabs attention due to its role in the contentious �piriformis syndrome�, a condition implicated as a potential source of pain and dysfunction, not only in the general population but in athletes as well.
Relevant Anatomy
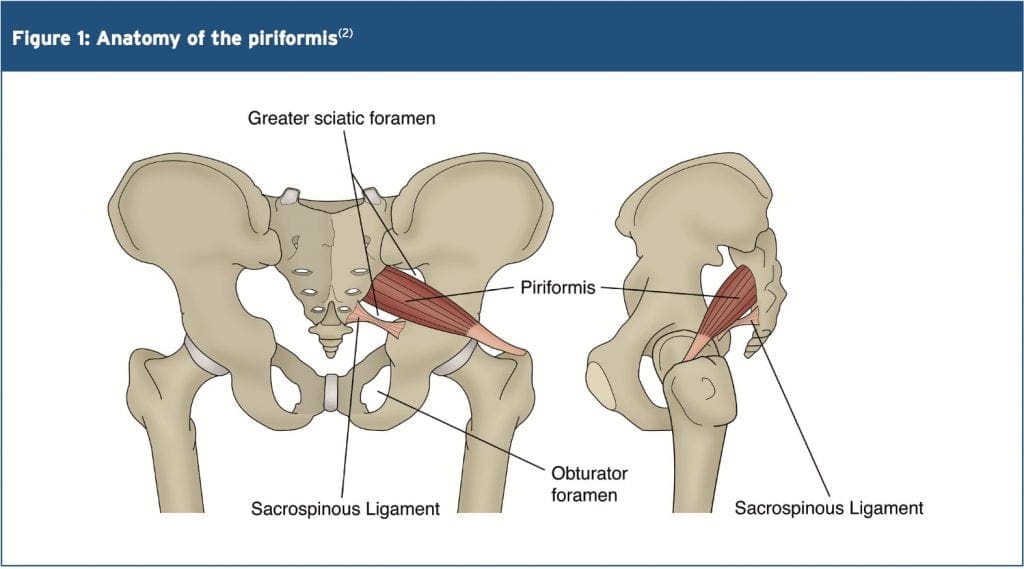
The name piriformis was first coined by Belgian Anatomist Adrian Spigelius in the early 17th century. Its name is derived from the Latin word �pirum� meaning �pear� and �forma� meaning �shape� � ie a pear shaped muscle (see Figure 1)(1).
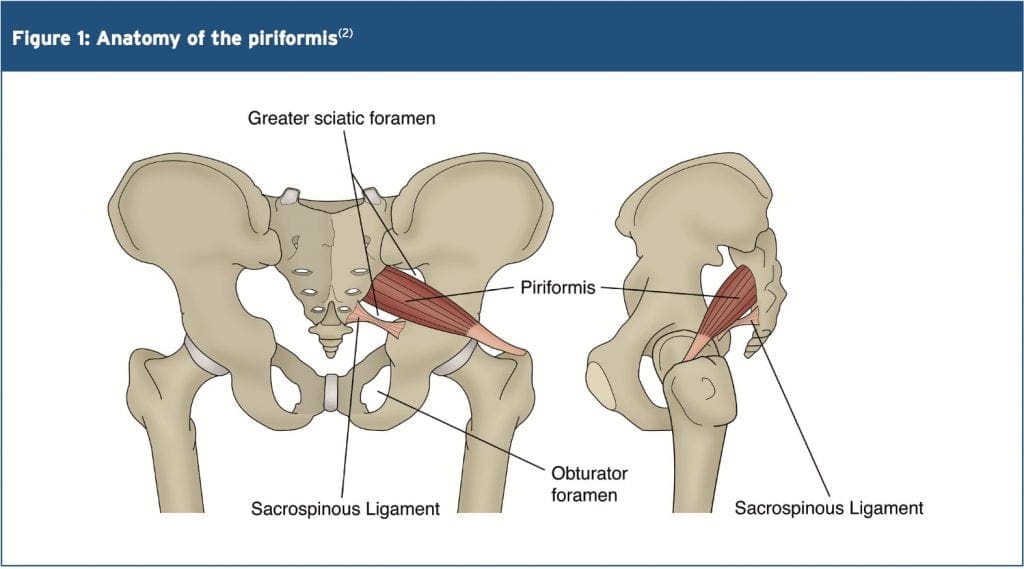
The PM originates on the anterior surface of the sacrum and is anchored to it by three fleshy attachments between the first, second, third and fourth anterior sacral foramina(2). Occasionally its origin may be so broad that it joins the capsule of the sacroiliac joint above and with the sacrotuberous and/or sacrospinous�ligament below(3,4).
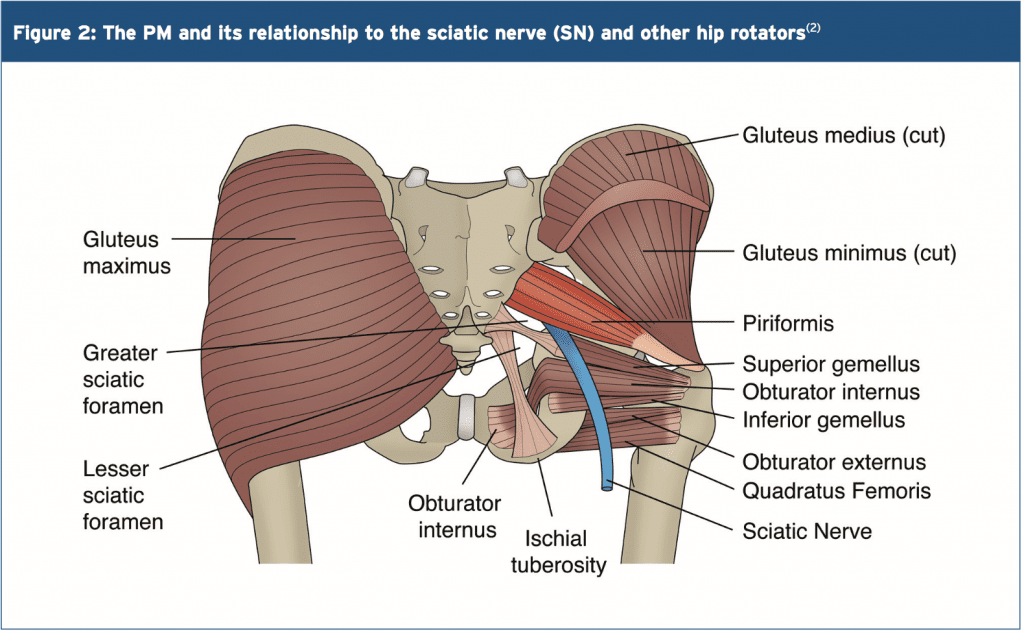
PM is a thick and bulky muscle, and as it passes out of the pelvis through the greater sciatic foramen, it divides the foramen into the suprapiriform and infra-piriform foramina(5). As it courses antero-laterally through the greater sciatic foramen, it tapers out to form a tendon that is attached to the superior-medial surface of the greater trochanter, commonly blending with the common tendon of the obturator internus and gemelli muscles(6).
The nerves and blood vessels in the suprapiriform foramen are the superior gluteal nerve and vessels, and in the infra- piriforma fossa are the inferior gluteal nerves and vessels and the sciatic nerve (SN)(5). Due to its large volume in the greater sciatic foramen, it has the potential to compress the numerous vessels and nerves that exit the pelvis.
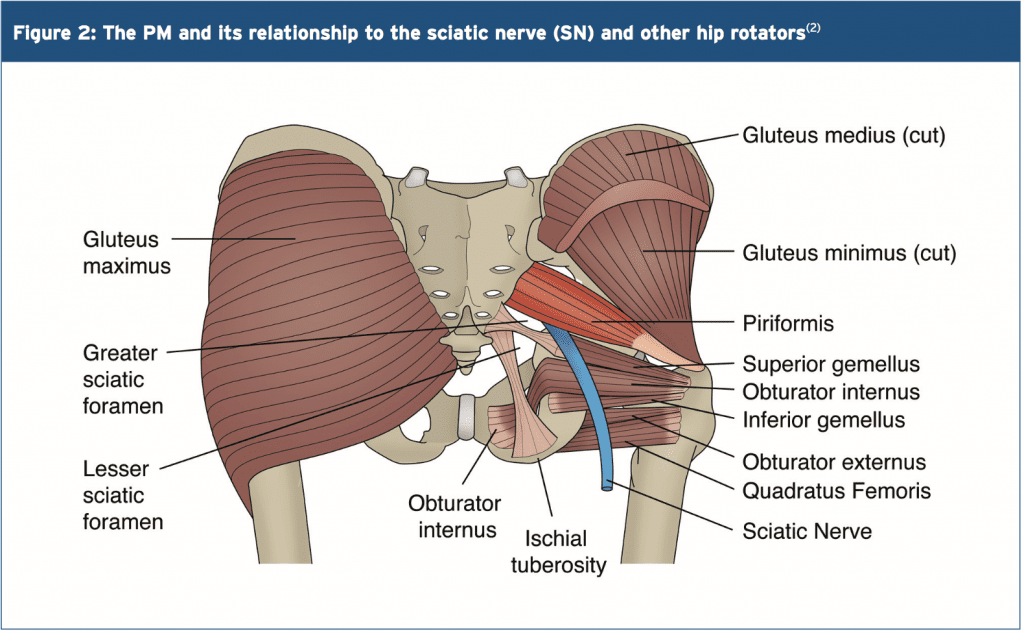
PM is closely associated with the other short hip rotators that lie inferior such as the superior gemellus, obturator internus, inferior gemellus and obturator externus(2). The primary difference between the PM and other short rotators is the relationship to the SN. The PM passes posterior to the�nerve whereas the other otators pass anterior (see figure 2).
 Variants
Variants
A few anatomical variants have been found with the PM:
1. Additional medial attachments to the first and fifth sacral vertebrae and to the coccyx(7).
2. The tendon may fuse with the gluteus medius or minimus above, or superior gemellus below(7).
3. In less than 20% of cases it is divided into two distinct portions through which part or all of the sciatic nerve may pass(7).
4. It may blend with the posterior hip joint capsule as a conjoined tendon with the obturator internus(8).
5. The distal attachment of the PM has shown to vary in dimensions and position on the supero-medial surface of the greater trochanter. It can span a distance of between 25-64% of the anterior-posterior length on the greater trochanter, with 57% attaching more anterior and 43% more posterior(9).
6. Pine et al (2011) studied the insertion point extensively and found that four types of insertion existed and these were classified based on the relationship to the obturator internus(10). The variability in position and breadth of the distal attachment of the PM muscle may influence the validity of the concept known as �inversion of action� (see below).
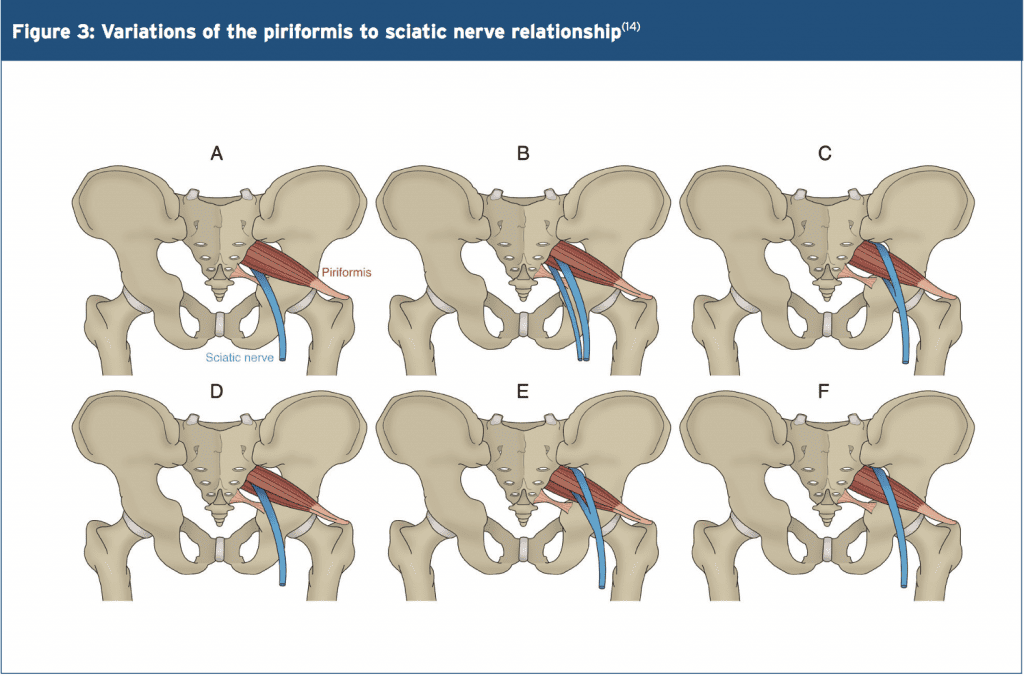
The other hotly debated issue is the relationship between the PM and the SN. The conclusion is that there are several anatomical variations of the PM and its SN relationship. The sub-types of this variation include(11-13):
- Type 1 (A below). Typical pear shape muscle with the nerve running anteriorly and inferiorly to this (in 70%-85% of cases).
- Type 2 (B below). The PM is divided into two parts with the common peroneal nerve running between the two parts and the tibial nerve running anterior and below (found in 10-20% of cases).
- Type 3 (C below). The peroneal portion loops over the top of the muscle and the tibial portion is below (found in 2-3% of cases).
- Type 4 (D below). Undivided nerve passing through the PM (occurs in about 1% of cases).
It is also believed that two other very uncommon variations occur (see E and F below).
Type A is the most common variation, showing the SN passing below the PM
Functional Considerations
The primary functional roles of the PM are;
1. Hip external rotation(15).
2. Abductor at 90 degrees of hip flexion(15).
3. In weight-bearing, the PM restrains the femoral internal rotation during stance phase of walking and running(2).
4. Assists the short hip rotators in compressing the hip joint and stabilising the joint(6).
5. As it can exert an oblique force on the sacrum, it may produce a strong rotary shearing force on the sacroiliac joint (SIJ). This would displace the ipsilateral base of the sacrum anteriorly (forward) and the apex of the sacrum posteriorly(16).
As the PM is the most posterior of the hip external rotators due to its attachment on the anterior surface of the sacrum, it has the greatest leverage to exert a rotation effect on the hip joint. It is often seen clinically that the PM appears to be tight and hypertonic, while the other short hip�rotators that are closer to the axis of rotation become inhibited and hypotonic.
Inversion Of Action
The most contentious issue related to the function of the PM is its �reversal-of- function role� or �inversion of action� role. Many authors have suggested that as the hip approaches angles of 60-90 degrees and greater, the tendon of the PM shifts superiorly on the greater trochanter. As a result, its line of pull renders it ineffective as a hip external rotator; however it does contribute to internal hip rotation. Therefore it reverses its rotation role at high hip flexion angles(15,17,18).
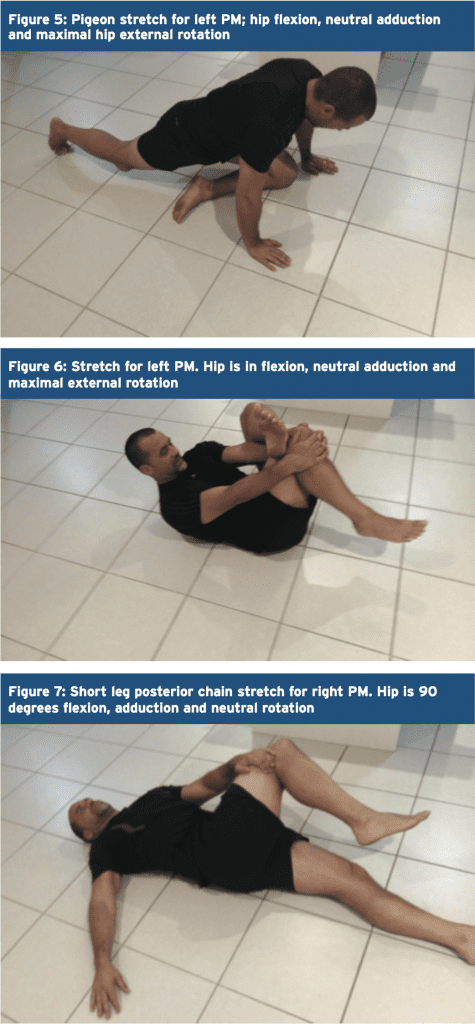
The function of the PM at varying joint angles is an important consideration for the clinician who is evaluating and treating �piriformis syndrome�. Often it has been advocated to stretch the hip into flexion, adduction and external rotation to stretch the PM over the glutes by utilising the �reversal of function� concept.
However, more recent anatomical dissection studies have shown that the attachment of the PM onto the greater trochanter can be variable and in some instances it may insert in a position whereby it is unable to reverse its function, for example in a more posteriorly placed attachment(19). Therefore, stretching the PM into external rotation when the hip is flexed beyond 90 degrees � based upon reversal of function � would be ineffective as a treatment or misleading as an examination technique(19)
MSK Dysfunction & PM Syndrome
Many decades ago, the role that the PM played in creating sciatic-like symptoms was first suggested by Yeoman (1928) when it was considered that some cases of sciatica may originate outside the spine(20). This was supported soon after when Freiberg and Vinkle (1934) successfully cured sciatica by surgically dividing the PM(21). Based on cadaver dissections Beaton and Anson (1938) gave the hypothesis that the spasm of the PM could be responsible for the irritation of the SN(12).
The term �piriformis syndrome� was first coined by Robinson in 1947(22) and was applied to sciatica thought to be caused by an abnormality in the PM (usually traumatic in origin) with emphasis on ruling out more common causes of sciatica such as nerve root impingement from a disc protrusion. It soon became an accepted clinical entity � but with no consensus about the exact clinical signs and diagnostic tests to differentiate it from other sources of sciatica(23,24).
Piriformis syndrome can be defined as a clinical entity whereby the interaction�between the PM and SN may irritate the SN and produce posterior hip pain with distal referral down the posterior thigh, imitating �true sciatica�. Isolating the dysfunction to this region usually follows exclusion of the more common causes of buttock pain and sciatica.
More specifically, complaints of buttock pain with distal referral of symptoms are not unique to the PM. Similar symptoms are prevalent with the more clinically evident lower back pain syndromes and pelvic dysfunctions. Thus, a thorough evaluation of these regions must be performed to exclude underlying pathology(4). It has been suggested that piriformis syndrome� is responsible for 5-6% of cases of sciatica(25,26). In the majority of cases, it occurs in middle-aged patients (mean age 38 yr)(27) and is more prevalent in women(28).
Pathogenesis Of Piriformis Syndrome (PS)
PS may be caused by or relate to three primary causative factors;
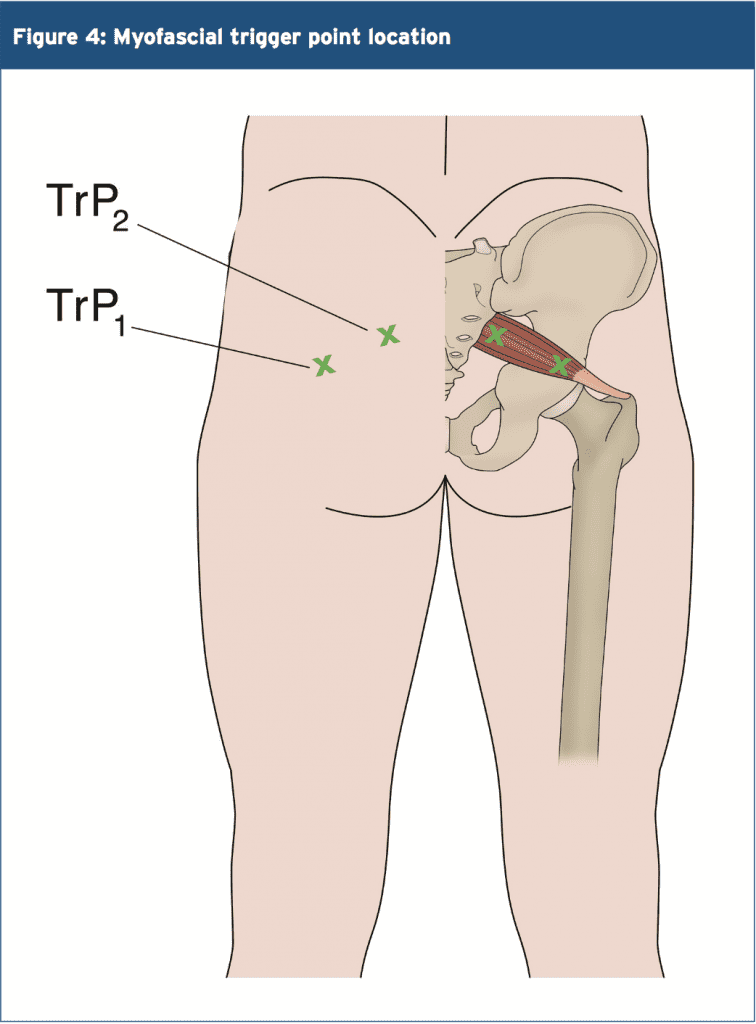
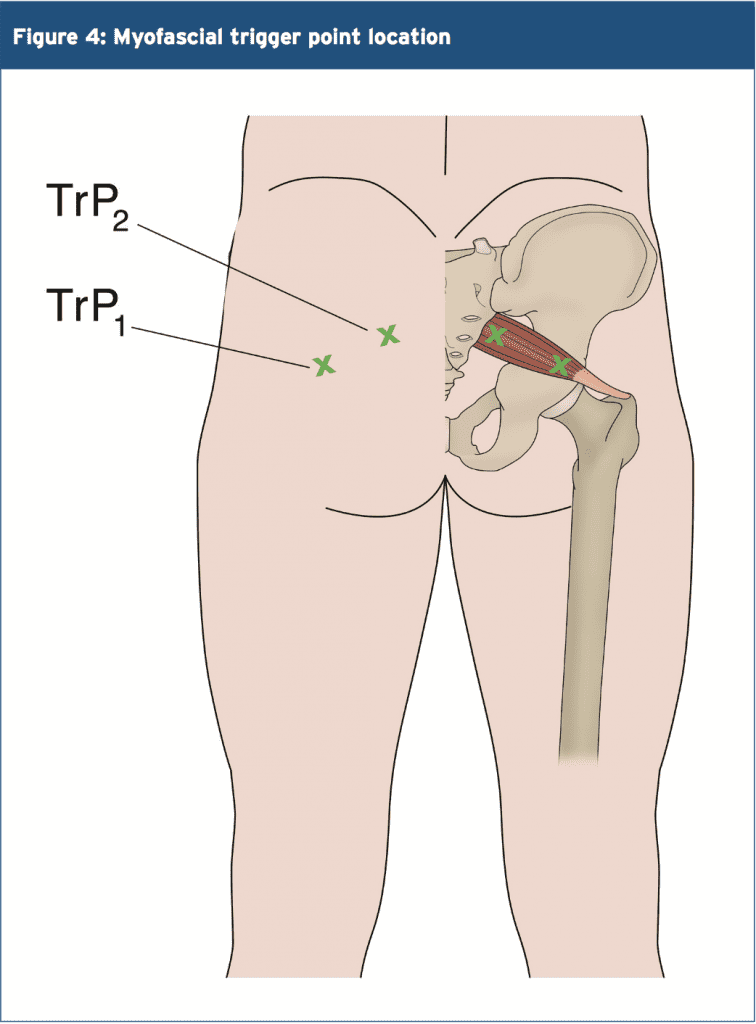
1. Referred pain due to myofascial trigger points (see Figure 4)(2,28-30). Examples include tight and shortened muscle fibres precipitated by muscle overuse such as squat and lunge movements in external rotation, or�direct trauma(16). This increases the girth of the PM during contraction, and this may the source of the compression/entrapment.
2. Entrapment of the nerve against the greater sciatic foramen as it passes through the infrapiriform fossa, or within a variant PM(29,31).
3. SIJ dysfunction causing PM spasm(29,32).
Janvokic (2013) has presented a number of causative factors in PS(29);
1. Gluteal trauma in the sacroiliac or gluteal areas.
2. Anatomical variations.
3. Myofascial trigger points.
4. Hypertrophy of the PM or spasm of the PM.
5. Secondary to spinal surgery such as laminectomy.
6. Space occupying lesions such as neoplasm, bursitis, abscess, myositis. 7. Intragluteal injections.
8. Femoral nailing.
Symptoms
Typical symptoms reported in piriformis syndrome include:
- A tight or cramping sensation in the buttock and/or hamstring(33).
- Gluteal pain (in 98% of cases)(34).
- Calf pain (in 59% of cases)(34).
- Aggravation through sitting and squatting(35), especially if the trunk is inclined forward or the leg is crossed over the unaffected leg(36).
- Possible peripheral nerve signs such as pain and paraesthesia in the back, groin, buttocks, perineum, back of the thigh (in 82% of cases)(34).
Physical Findings & Examinations
- Palpable spasm in and around the PM and obturator internus and external tenderness over the greater sciatic notch (in 59-92% of cases)(34,35). The patient is placed in the Sims position. The piriformis line overlies the superior border of the PM and extends from immediately above the greater trochanter to the cephalic border of the greater sciatic foramen at the sacrum. The line is divided into equal thirds. The fully rendered thumb presses on the point of maximum trigger-point tenderness, which is usually found just lateral to the junction of the middle and last thirds of the line.
- Hip flexion with active external rotation or passive internal rotation may exacerbate the symptoms(36).
- Positive SLR that is less than 15 degrees the normal side(37).
- Positive Freiberg�s sign (in 32-63% of cases)(34,35). This test involves reproducing pain on passive forced internal rotation of the hip in the supine position � thought to result from passive stretching of the PM and pressure on the sciatic nerve at the sacrospinous ligament.
- Pacers sign (in 30-74% of cases)(34,35). This test involves reproducing pain and weakness on resisted abduction and external rotation of the thigh in a sitting position.
- Pain in a FAIR position(34). This involves the reproduction of pain when the leg is held in flexion, adduction and internal rotation.
- An accentuated lumbar lordosis and hip flexor tightness predisposes one to increased compression of the sciatic nerve against the sciatic notch by a shortened piriformis(38).
- Electro-diagnostic tests may prove useful (see below).
Investigations
Conventional imaging such as X-ray, CT scan and MRI tend to be ineffective in diagnosing piriformis syndrome.
However, some value may exist in electro- diagnostic testing.
It is beyond the scope of this paper to discuss in detail the process of electro- diagnostic testing; the reader is directed to references for more a more detailed description of how these tests are administered(35,36,39). However the purpose of these tests is to find conduction faults in the SN. Findings such as long-latency potentials (for example the H reflex of the tibial nerve and/or peroneal nerve) may be normal at rest but become delayed in positions where the hip external rotators are tightened(27,36,39).
It is accepted that the tibial division of the SN is usually spared, the inferior gluteal nerve that supplies the gluteus maximus may be affected and the muscle becomes atrophied(40). However testing of the peroneal nerve may provide more conclusive results as is more likely to be the�impinged portion of the SN. The H-wave may become extinct during the painful position of forced adduction-internal rotation of the affected leg(36).
The �Myth� Of Piriformis Syndrome
Stewart 2003 argues that piriformis syndrome is an often over-used term to describe any non-specific gluteal tenderness with radiating leg pain(41). He argues that only in rare cases is the PM implicated in nerve compression of the SN to truly qualify as a piriformis syndrome. He cites only limited evidence and cases where the diagnosis of piriformis syndrome can be made.
1. Compressive damage to the SN by the PM. Stewart cites studies whereby in few isolated studies, the SN was seen to be compressed by the PM in instances such as hypertrophy of the muscle,�usual anatomical anomalies such as a bifid PM, and due to compression by fibrous bands.
2. Trauma and scarring to the PM leading to SN involvement; it is possible that rare cases of true Piriformis Syndrome have been caused by direct heavy trauma to the PM due to a blunt trauma to the muscle. This is termed �post- traumatic PS�.
McCory (2001) supports this argument by stating that it is more likely that (given the anatomical relationship of the PM to the various nerves in the deep gluteal region) the buttock pain represents entrapment of the gluteal nerves, and the hamstring pain entrapment of the posterior cutaneous nerve of the thigh, rather than the SN alone(33). This would explain the clinically observed phenomenon in the absence of distal sciatic neurological signs. Whether the PM is the cause of the compression has not been clearly established. It is possible that the obturator internus/gemelli complex is an alternative cause of neural compression. He suggests using the term �deep gluteal syndrome� rather than piriformis syndrome.
Treatment
When it is believed that a piriformis syndrome exists and the clinician feels that a diagnosis has been made, the treatment will usually depend on the suspected cause. If the PM is tight and in spasm then initially conservative treatment will focus on stretching and massaging the tight muscle to remove the PM as being the source of the pain. If this fails, then the following have been suggested and may be attempted(23,36):
- Local anaesthetic block � usually performed by anaesthesiologists who have expertise in pain management and in performing nerve blocks.
- Steroid injections into the PM.
- Botulinum toxin injections into the PM.
- Surgical Neurolysis.
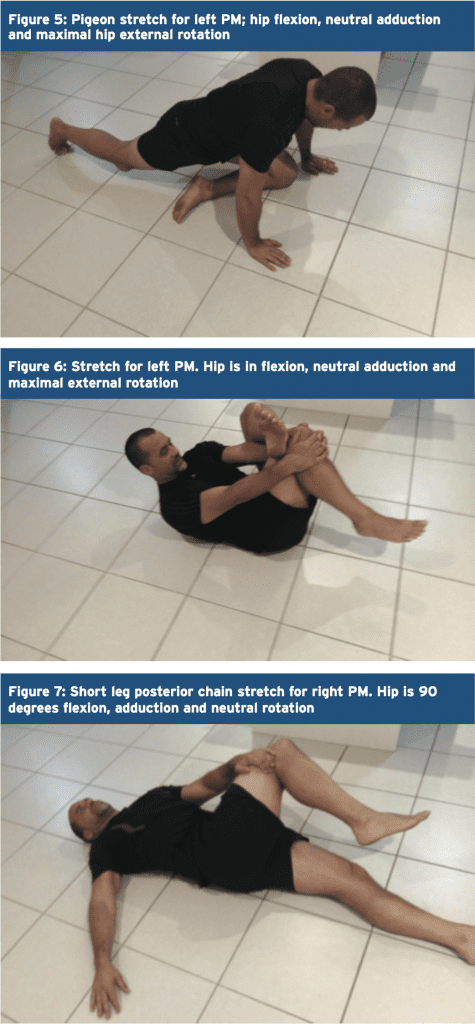
Here, we will focus on therapist-directed interventions such as stretching of the PM and direct trigger point massage. It has always been advocated that PM stretches are done in positions of hip flexion greater than 90 degrees, adduction and external rotation to utilize the �inversion of action� effect of the PM to isolate the stretch to this muscle independent of the other hip external rotators.
However, recent evidence from Waldner (2015) using ultrasound investigation discovered that there was no interaction between hip flexion angle and the thickness of the PM tendon in both internal and lateral hip rotation stretching � suggesting that the PM does not invert its action(19). Furthermore, Pine et al (2011)(9) and Fabrizio et al (2011)(10) in their cadaveric studies found that the PM insertion is a lot more complex and varied than first thought. It is possible that the PM may invert its action only in some subjects but not others.
Therefore, due to the disagreements and confusions over the �inversion of action� concept, it is recommended that the clinician �covers all bases� and performs two variations of a PM stretch � stretches in flexion, adduction and external rotation and stretches in flexion, adduction and internal rotation. Examples of these stretches are given in figures 5-7 below.
 Trigger Points & Massage
Trigger Points & Massage
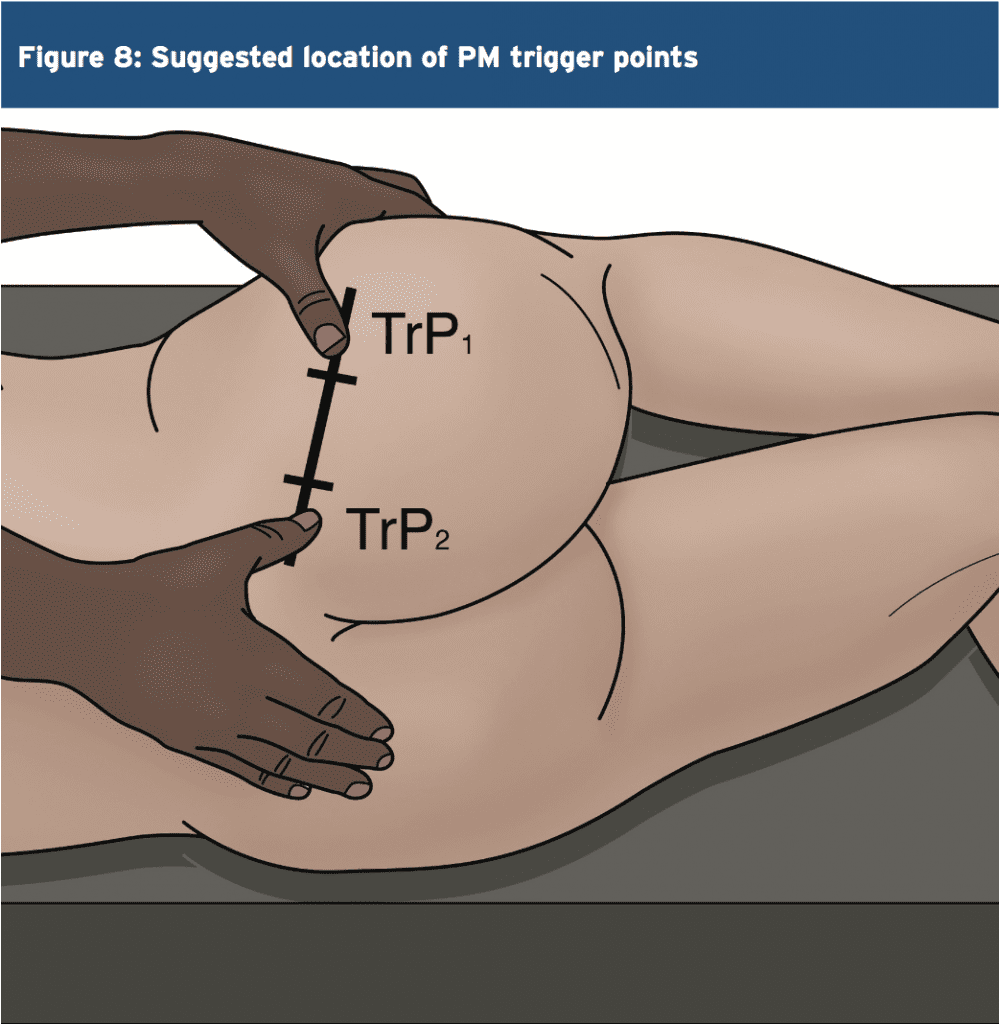
(see Figure 8)
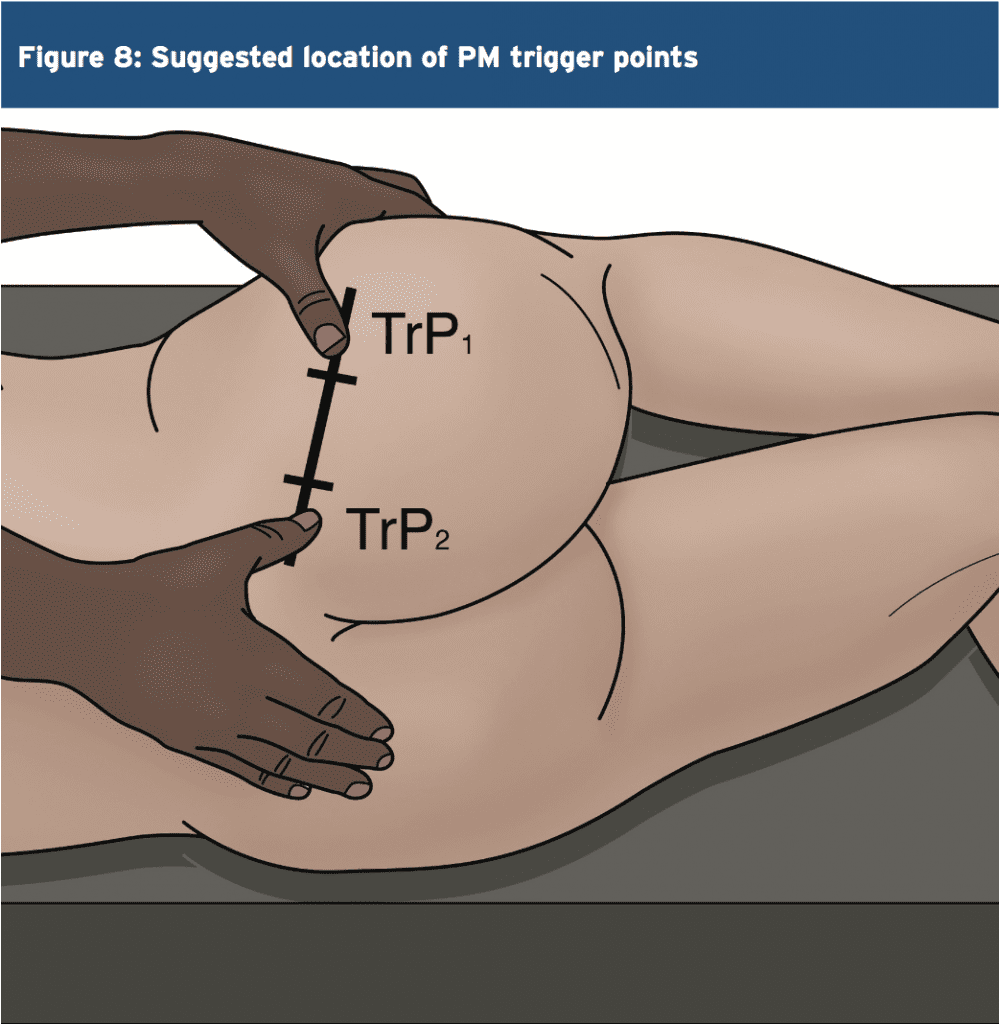
The best approach to palpate the PM trigger points is in the position suggested by Travel and Simons(2) and this is shown below. In this position, the clinician can feel for the deep PM trigger points and apply a sustained pressure to alleviate the trigger�points � and also apply a flush massage to the muscle in this position.�In this position the large gluteus maximus is relaxed and it is easier to feel the deeper PM.
Summary
The PM is a deep posterior hip muscle that is closely related anatomically to both the sacroiliac joint and the sciatic nerve. It is a hip external rotator at hip flexion angles of neutral to 60 degrees of hip flexion, an abductor when in flexion and also contributes to hip extension.
It has been previously accepted that the PM will �invert its action� or �reverse its function� after 60 degrees of flexion to become a hip internal rotator. However, recent ultrasound and cadaveric studies has found conflicting evidence that this �inversion of action� may in fact not exist.
PM is a muscle that is a dominant hip rotator and stabiliser, and thus has a tendency to shorten and become hypertonic. Therefore, stretching and massage techniques are best utilised to reduce the tone through the muscle. Furthermore, it has also been implicated in compression and irritation of the sciatic nerve � often referred to as piriformis syndrome�.
References
1. Contemp Orthop 6:92-96, 1983.
2. Simons et al (1999) Travell and Simons� Myofascial Pain and Dysfunction. Volume 1 Upper Half of the Body (2nd edition). Williams and Wilkins. Baltimore.
3. Anesthesiology; 98: 1442-8, 2003.
4. Joumal of Athletic Training 27(2); 102-110, 1996.
5. Journal of Clinical and Diagnostic Research. Mar, Vol-8(3): 96-97, 2014.
6. Clemente CD: Gray�s Anatomy of the Human Body, American Ed. 30. Lea & Febiger, Philadelphia, 1985 (pp. 568-571).
7. Med J Malaysia 36:227-229, 1981.
8. J Bone Joint Surg;92-B(9):1317-1324, 2010.
9. J Ortho Sports Phys Ther. 2011;41(1):A84, 2011.
10. Clin Anat;24:70-76, 2011.
11. Med Sci Monit, 2015; 21: 3760-3768, 2015.
12. J Bone Joint Surg Am 1938, 20:686-688,1938.
13. Journal of Clinical and Diagnostic Research. 2014 Aug, Vol-8(8): 7-9, 2014.
14. Peng PH. Piriformis syndrome. In: Peng PH, editor. Ultrasound for Pain Medicine Intervention: A Practical Guide. Volume 2. Pelvic Pain. Philip Peng Educational Series. 1st ed. iBook, CA: Apple Inc.; 2013 .
15. Kapandji IA. The Physiology of Joints. 2nd ed. London: Churchill Livingstone; 1970: 68.
16. J Am Osteopath Assoc 73:799-80 7,1974.
17. J Biomechanics. 1999;32:493-50, 1999.
18. Phys Therap. 66(3):351-361, 1986.
19. Journal of Student Physical Therapy Research. 8(4), Article 2 110-122, 2015.
20. Lancet. 212: 1119-23, 1928.
21. J Bone Joint Surg Am 16:126�136, 1934.
22. Am J Surg 1947, 73:356-358, 1947.
23. J Neurol Sci; 39: 577�83, 2012.
24. Orthop Clin North Am; 35: 65-71, 2004
25. Arch Phys Med Rehabil; 83: 295-301,2002.
26. Arch Neurol. 63: 1469�72, 2006.
27. J Bone Joint Surg Am; 81: 941-9,1999.
28. Postgrad Med 58:107-113, 1975.
29. Can J Anesth/J Can Anesth;60:1003�1012, 2013.
30. Arch Phys Med Rehabil 69:784, 1988.
31. Muscle Nerve; 40: 10-8, 2009.
32. J Orthop Sports Phys Ther;40(2):103-111, 2010.
33. Br J Sports Med;35:209�211, 2001.
34. Man Ther 2006; 10: 159-69, 2006.
35. Eur Spine J. 19:2095�2109, 2010.
36. Journal of Orthopaedic Surgery and Research, 5:3, 2010.
37. Muscle & Nerve. November. 646-649, 2003.
38. Kopell H, Thomnpson W. Peripheral Entrapment Neuropathies. Huntington, NY: Krieger, 1975:66.
39. Arch Phys Med Rehabil;73:359�64, 1992.
40. J Bone and Joint Surg, 74-A:1553-1559, 1992.
41. Muscle & Nerve. November. 644-646, 2003
by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | UTEP (Local) RSS
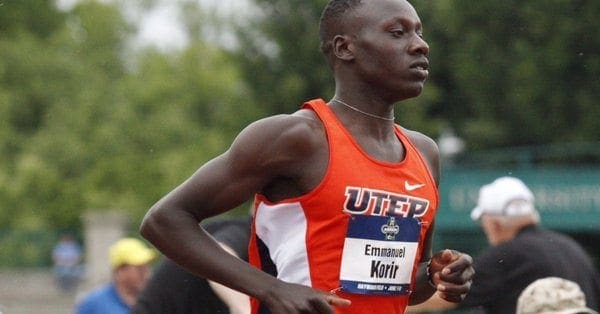
Eugene, Or. – UTEP’s Emmanuel Korir and Michael Saruni make history by being the first freshman duo from the same school to make the 800m final in meet history at the NCAA Championships on Wednesday night.
Running at their first ever NCAA Championships, All-American duo Korir and Saruni did not disappoint. Korir won the first of three heats in the men’s 800m semifinal with the fastest qualifying time of 1:46.38. Saruni’s time of 1:46.63 was enough to win the final heat of the 800m and the third-fastest qualifying time.
Korir and Saruni will run on Friday’s 800m final set to start at 7:45 p.m. MT.
In a valiant effort running the 4x400m relay, Saruni, Korir, Asa Guevara and James Bias clocked 3:18.65. Saruni and Korir had just 90 minutes to recuperate and compete in the mile relay.
Day two of the NCAA Championship will see Tobi Amusan in the 100m hurdles set to start at 6:25 p.m., Lilian Koech in the 800m set for a 7:10 p.m. start and Winny Koech to close out the night in the 10,000m final running at 8:05 p.m.
You can watch the 2017 NCAA Division I Outdoor Track and Field Championships live on the ESPN family of networks. Both the final day of the men’s championship and women’s championship will be aired in prime time on ESPN.
For live results and breaking news be sure to follow @UTEPTrack on Twitter and uteptrack on Instagram.
by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | UTEP (Local) RSS
The 2017 edition of the UTEP Men’s Basketball Camps is almost here. The Miner coaching staff and players will conduct two camps for boys and girls of all skill levels, ages 7-17. The first is June 19-21, and the second is June 26-29.
The camp will be held at the Don Haskins Center from 9 a.m. – 4 p.m. each day and will teach the fundamentals of basketball through a variety of skill work, games and contests.
Each camper will receive a t-shirt on the first day of camp, and certificate at the end of the camp. Various trophies and prizes will be awarded to campers who stand out in talent, skill level, hustle and sportsmanship.
Campers can bring their own lunch, or purchase lunch and/or snacks on site. The cost is $200 for the June 19-21 camp, and $250 for the June 26-29 camp.
Campers receive $50 off by signing up for both camps. UTEP staff and military members receive a $50 discount for each camp. Walk-ups will be accepted.
Registration will take place in the East concourse of the Don Haskins Center. With Glory Road closed for both camps, parking will be available by the UTEP Ticket Center off of Mesa Street.
To register or for more information, call UTEP Director of Basketball Operations Evan Eustachy at (915) 747-6235 or visit the camp’s website.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | UTEP (Local) RSS
Eugene, Or. – Tobi Amusan’s dazzling sophomore season continues as she earned an automatic qualifying spot in the 100m Hurdles on day two of the NCAA Championships on Thursday evening.
Amusan was tasked with running in the second and most competitive heat of three in the 100m hurdle semifinals. The sophomore clocked the fastest qualifying time of 12.79, beating the likes of Drior Hall (USC) and the 2017 (60m hurdle) NCAA Indoor Champion Sasha Wallace (Oregon).
Last year the Nigerian native finished runner up to Kentucky’s Jasmine Camacho-Quinn (12.84), who also qualified to the final. Amusan will take the track again on Saturday at 5:10 p.m. MT live on ESPN.
Sophomore 800m runner Lilian Koech’s season came to a halt on Thursday evening. The Kenya native clocked a time of 2:09.30 to finish 23rd overall.
Winny Koech’s season also came to an end as she ran a time of 34:51.32 in the 10,000m final on Thursday evening.
Friday’s action will see three Miners compete. Emmanuel Korir and Michael Saruni will run in the men’s 800m final set to start at 7:45 p.m. live on ESPN. Saruni (1:46.38) and Korir (1:46.63) qualified to the No. 1 and No. 3 spots in tomorrow’s final.
Lucia Mokrasova will also be in action as she will complete the first of four events (100m hurdles, high jump, shot put and 200m dash) of the heptathlon. The heptathlon competition can be viewed on espn3.com and begins at 1:30 pm.
For live results and breaking news be sure to follow @UTEPTrack on Twitter and uteptrack on Instagram.
by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | UTEP (Local) RSS
Eugene, Or. – It was a bittersweet victory for the Miners as UTEP’s freshman Emmanuel Korir captured his second NCAA title in the 800m at the historic Hayward Stadium on Friday evening.
Running in the 800m final were both freshman Michael Saruni and Korir, who were favored to finish the event No. 1 and No. 2. Korir, a bit shaken up, narrowly held onto his lead and finished the race in a time of 1:45.03. It marks his second NCAA track and field title (800m indoor and outdoor).
“It was very unfortunate that Michael went down in the 800m, it would’ve been a very exciting finish to see who would be the national champion had he not fallen,” head coach Mika Laaksonen stated. “Emmanuel should feel very fortunate, Michael would have really challenged him at the end. He [Korir] is such a talented runner this may have been his last race for us.”
Saruni, having taken a hard fall, showed great determination and strength to finish the race with a time of 2:15.56. The Kenya native still earned All-American honors for his performance.
The only female competing for the Miners on Friday was junior Lucia Mokrasova. Under difficult weather conditions, she tallied a total of 3,178 points through the first four events of the women’s heptathlon.
She started the day off with a time of 14.49 in the 100m hurdles for 910 points. She followed that up by clearing 1.54m in the high jump accumulating 666 points. Her best event was undoubtedly the shot put. The Slovakia native heaved the ball out to 13.36m (43-10) garnering 751 points; the throw was the enough to place her first in the 24-athlete field.
She closed out the night with a time of 25.93 for 851 points in the 200m.
Mokrasova will conclude the heptathlon Saturday with the long jump (12:30 p.m. MT/espn3.com), javelin throw (1:45 p.m./espn3.com) and the 800m run (6:30 p.m./ESPN).
Saturday will feature the women’s final day of competition with sophomore sensation Tobi Amusan running in the 100m hurdle final for the second time in her career. Amusan qualified with the fastest time of 12.79. The Nigerian native will take the track at 5:10 p.m. live on ESPN.
Senior Samantha Hall will make her final appearance in the Orange and Blue as she competes in the women’s discus throw. Hall comes into the competition ranked 7th among the 24-athlete field. The discus throw starts at 4:00 p.m. on ESPN3.com.
For live results be sure to follow @UTEPTrack on Twitter and uteptrack on Instagram.
by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | UTEP (Local) RSS
Eugene, Or. – Tobi Amusan finds redemption as she won her first NCAA title in the 100m hurdles at historic Hayward Stadium on the final day of the NCAA Championships, Saturday evening.
“Amusan is another special talent. She executed her race very well and all the hard work she put in this season paid off,” head coach Mika Laaksonen said. “This was her closest race yet and she stepped up to the challenge.”
The freshman exploded out of the blocks and held onto a narrow lead over the defending champion Jasmine Camacho-Quinn (Kentucky). In the closing moment of the race Amusan leaned over the finish line to clock a time of 12.57, while Camacho-Quinn was close behind at 12.58.
The Nigerian native broke the UTEP school record in this event earlier this year at the UTEP Springtime stopping the clock at 12.63. Her time of 12.57 demolished that record and sets a personal best.
The last time UTEP track and field had multiple individual NCAA Champions was back in 1978 (Peter Lemashon, 800m, Michael Musyoki, 10,000m, Jennifer Smit, Shot Put and Ria Stahlman, Discus).
Korir and Amusan add to UTEP’s total of NCAA Champions to 107. Korir becomes just the second Miner to ever win the 800m NCAA title, while Amusan is the first to ever achieve the NCAA crown in the 100m hurdles.
Two other Miners competed on Saturday evening. Samantha Hall in the women’s discus throw and Lucia Mokrasova completing the final three events in the women’s hepthathon.
Hall showed poise in the first flight of two in the discus event. The senior launched the discus out to 54.66m (179-4), placing 10th overall and just narrowly missing out of the top nine who advance to the event’s final. The Jamaican native finishes her career at UTEP ranking fifth on the all-time list for the indoor shot put (14.90m), fifth in the outdoor shot put list (14.77m) and holds the school record in the discus throw (58.50m). Hall is a two-time Conference USA Champion in the discus throw. Hall garnered All-American second team honors.
In just her second appearance at the NCAA Championships, Mokrasova finished in 17th place with a total of 5,172 points. The junior started the day off by leaping 5.34m (17-16.25) in the long jump for 654 points. She followed that up with a javelin heave of 37.10m (121-9) and closed out the event with an 800m time of 2:13.46 (915 points). The Slovakia native finished the season with a new school record in the event, when she scored 5,671 points earlier this year at the Texas Relays.
The UTEP track and field team close out the 2017 campaign with two women conference titles both indoor and outdoor. The 2017 C-USA Outdoor Championship title was the first outdoor conference title in women’s program history. The Miners finish with three outdoor All-Americans, Michael Saruni, Korir and Amsuan and a second team All-American (Hall).
For live results and breaking news be sure to follow @UTEPTrack on Twitter and uteptrack on Instagram.


 Variants
Variants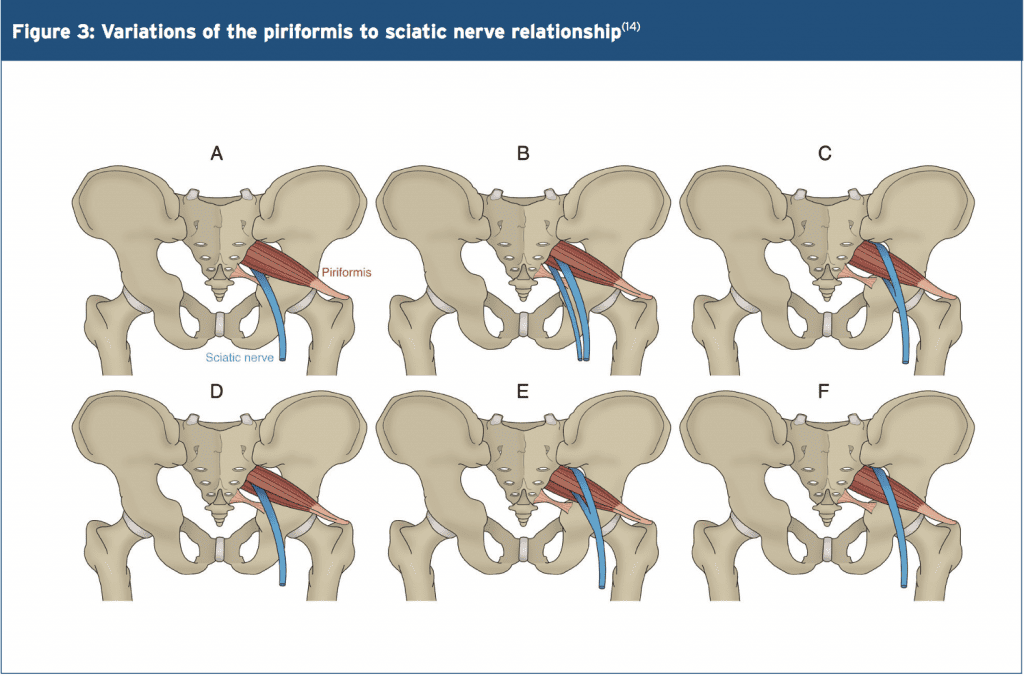
 Trigger Points & Massage
Trigger Points & Massage