Facet hypertrophy is an incurable, chronic disease that affects the facet joints in the spine. Can recognizing symptoms, help in diagnosis, and treatment?
Contents
Facet Hypertrophy
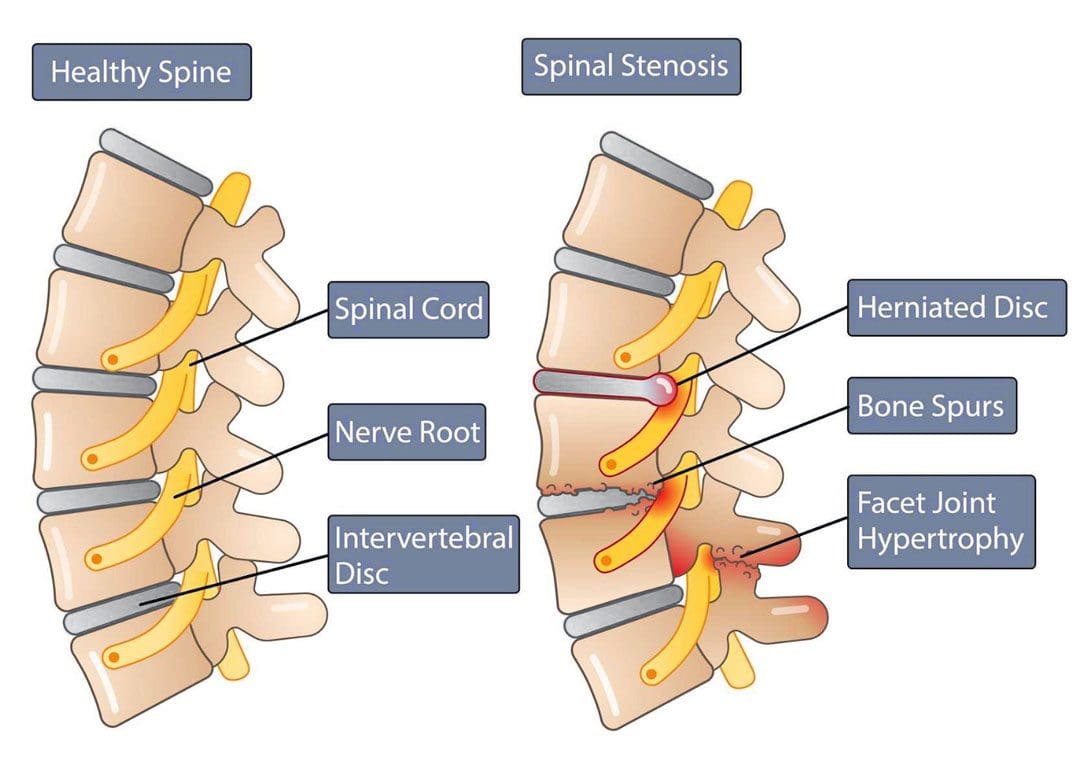
Facet hypertrophy causes the facet joints in the spine to enlarge. They are found where the vertebrae come into contact on the back of the vertebrae that form the backbone. These joints stabilize the spine when twisting and bending. Hypertrophy results when damage wears down the cartilage that cushions the bones that meet in the joint. This can include:
- Aging
- Wear and tear
- Arthritis
- Other joint diseases can damage facet joints.
Swelling, new bone growth, and bone spurs can occur as the joint tries to repair the damaged cartilage. The swelling and new bone growth can narrow the spinal canal and compress surrounding nerves, causing pain and other sensation symptoms. This ailment does not have a cure and worsens over time. The objective of treatment is to manage the pain symptoms and slow down the disease’s progress.
Types
Facet hypertrophy can be described as unilateral or bilateral.
- Unilateral – the pain is felt on one side.
- Bilateral – the pain is felt on both sides
On the following areas: (Romain Perolat et al., 2018)
- Buttocks
- Sides of the groin
- Thighs
Symptoms
Symptoms can have a wide range of intensity, from a dull ache to chronic, disabling pain. The location of symptoms depends on the affected joint and the nerves involved, Pain manifests when the enlarged joints and new bone growth compresses the nearby nerves. The result leads to nerve damage and the following symptoms: (Weill Cornell Medicine Brain & Spine Center. 2023) (Cedars Sinai. 2022)
- Stiffness, especially when standing up or getting out of a chair.
- Inability to stand straight when walking.
- Inability to look up to the left or right without turning the whole body.
- Reduced range of motion and mobility.
- Numbness or a tingling sensation of pins and needles.
- Muscle spasms
- Muscle weakness
- Burning pain
The following symptoms are specific to the location of the affected joint (Weill Cornell Medicine Brain & Spine Center. 2023) (Cedars Sinai. 2022)
- Radiating pain from the affected joint into the buttocks, hips, and upper thigh when the affected joint/s are in the lower back.
- Radiating pain from the affected joint into the shoulder, neck, and back of the head when the affected joint/s are in the upper back.
- Headaches when the affected joint is in the neck.
Causes
A common cause is the age-related degeneration of the joints, called spondylosis. Research indicates that more than 80% of individuals who are 40 or older have radiologic evidence of spondylosis, even though they may not have symptoms. (The University of Toledo Medical Center. N.D.) The following conditions can also increase the risk of facet hypertrophy (Weill Cornell Medicine Brain & Spine Center. 2023)
- Unhealthy posture
- Being overweight or obese
- Sedentary lifestyle
- Injury or trauma to the spine
- Inflammatory conditions like rheumatoid arthritis or ankylosing spondylitis
- Osteoarthritis
- Genetic predisposition to the condition
Diagnosis
Diagnosis can be challenging when neck or back pain is the main complaint, as symptoms can mimic conditions such as sciatica from a herniated disc or hip arthritis. (Weill Cornell Medicine Brain & Spine Center. 2023)
- A healthcare provider will conduct a complete physical examination, medical history, and discussion of symptoms.
- As part of the examination, individuals may be asked to move into positions that cause pain and show where the pain is located. (Weill Cornell Medicine Brain & Spine Center. 2023)
- Imaging tests can show visible damage and inflammation and/or help rule out other injuries or conditions that may be causing the symptoms. (Romain Perolat et al., 2018) (Weill Cornell Medicine Brain & Spine Center. 2023)
- CT scans with or without myelogram – the use of contrast dye in the space around the spinal cord.
- MRI
- X-rays with or without a myelogram
A diagnosis is confirmed by injecting a diagnostic block that involves administering an anesthetic injection, sometimes with an anti-inflammatory like cortisone, into the joint or nerves near the affected joint. Two injections are given at different times to confirm the effect. (Romain Perolat et al., 2018)
- If immediate relief improves after each injection, the facet joint is confirmed as the source of the pain symptoms.
- If the block does not decrease the pain, the facet joint is probably not the source of the pain symptoms. (Brigham and Women’s Hospital. 2023)
Treatment
There is no cure for facet hypertrophy.
The goal of treatment is to make the pain more manageable.
Conservative treatment is usually successful in making a difference.
Conservative Treatment
First-line treatment involves utilizing conservative therapies (Romain Perolat et al., 2018)
- Massage therapy
- Physical therapy to strengthen the core muscles and spine.
- Targeted exercises to help maintain flexibility.
- Chiropractic adjustments to realign the spine.
- Healthy posture retraining.
- Non-surgical mechanical decompression.
- Bracing to stabilize the spine
- Acupuncture
- Nonsteroidal anti-inflammatory – aspirin, ibuprofen, and naproxen.
- Muscle relaxers – cyclobenzaprine or metaxalone.
- Steroid injection into the facet joints.
- Injection of platelet-rich plasma/PRP into the joints.
Medial Branch or Facet Block
- A medial branch block injects local anesthetic near the medial nerves that connect to an inflamed joint.
- Medial nerves are small nerves outside the joint space near the nerve that transmit signals and other impulses to the brain.
- A facet block injects the medication outside the joint space near the nerve that supplies the joint called the medial branch.
Neurolysis
Neurolysis, also known as rhizotomy or neurotomy, is a procedure that destroys affected nerve fibers to relieve pain, reduce disability, and reduce the need for analgesics. This treatment can relieve pain for six to 12 months until the nerve regenerates, where further treatments may be necessary. (Matthew Smuck et al., 2012) Neurolysis can be performed using one of the following techniques (Romain Perolat et al., 2018)
- Radiofrequency ablation RFA – the application of heat through radiofrequency.
- Cryoneurolysis – the application of cold temperatures to the targeted nerve.
- Chemical neurolysis – applying chemical agents, like a combination of phenol and alcohol.
- Severing the nerves with surgical instrumentation.
Surgery
When one or more facet joints are severely damaged, they can become nonfunctional and painful. Surgery may be recommended when symptoms are not relieved by other therapies. (Ali Fahir Ozer, et al., 2015)
Prognosis
Facet hypertrophy is a chronic condition that progresses with age and does not affect life expectancy. (Weill Cornell Medicine Brain & Spine Center. 2023) The disorder is incurable, but symptoms can be managed with conservative therapies
- A healthcare provider can help develop a treatment plan based on the extent and location of the joint affected.
- Early diagnosis and treatment can help individuals achieve the best results.
Maintaining an active lifestyle and healthy weight can help prevent further joint stress. Individuals may be recommended to do regular stretching and strengthening exercises to lower inflammation, reduce stress, and improve overall health.
Facet Syndrome Treatment
References
Perolat, R., Kastler, A., Nicot, B., Pellat, J. M., Tahon, F., Attye, A., Heck, O., Boubagra, K., Grand, S., & Krainik, A. (2018). Facet joint syndrome: from diagnosis to interventional management. Insights into imaging, 9(5), 773–789. https://doi.org/10.1007/s13244-018-0638-x
Weill Cornell Medicine Brain & Spine Center. (2023). Symptoms of facet syndrome.
Cedars Sinai. (2022). Facet joint syndrome.
The University of Toledo Medical Center. (N.D.). Spondylosis.
Weill Cornell Medicine Brain & Spine Center. (2023). Facet syndrome.
Weill Cornell Medicine Brain & Spine Center. (2023). Diagnosing and treating facet syndrome.
Brigham and Women’s Hospital. (2023). Facet and medial branch blocks.
Smuck, M., Crisostomo, R. A., Trivedi, K., & Agrawal, D. (2012). Success of initial and repeated medial branch neurotomy for zygapophysial joint pain: a systematic review. PM & R : the journal of injury, function, and rehabilitation, 4(9), 686–692. https://doi.org/10.1016/j.pmrj.2012.06.007
Ozer, A. F., Suzer, T., Sasani, M., Oktenoglu, T., Cezayirli, P., Marandi, H. J., & Erbulut, D. U. (2015). Simple facet joint repair with dynamic pedicular system: Technical note and case series. Journal of craniovertebral junction & spine, 6(2), 65–68. https://doi.org/10.4103/0974-8237.156049
General Disclaimer, Licenses and Board Certifications *
Professional Scope of Practice *
The information herein on "Managing Facet Hypertrophy Pain: A Guide" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and on our family practice-based chiromed.com site, focusing on naturally restoring health for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez, DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card








