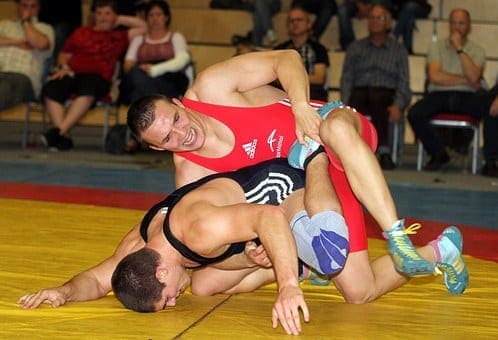
In the first part of the 2-part article on femoro-acetabular impingement (FAI), chiropractor, Dr. Alexander Jimenez discussed FAI and how it can lead to insidious onset abdominal pain and damage the hip joint labrum, leading to early arthritic changes. Given that conservative management generally fails in young athletes and needs operation, part two describes the post-operative rehabilitation period required to take an athlete back to full competition.
The post-operative rehabilitation period is highly dependent on the magnitude of pathology and the subsequent procedure; weight-bearing development is consequently variably reported in the literature.
If the labrum is surgically repaired, then protected weight bearing is encouraged to allow the repair site in order to be protected during the early healing phase. Also, avoiding extremes of flexion (beyond 60�) and also internal/external rotation for the initial 4 to 6 weeks is important to safeguard the repaired labrum. Any positions that possibly create an impingement and boost inflammation ought to be prevented. These include:
- Deep squatting
- Prolonged sitting
- Low couch sitting
- Lifting off the ground
- Pivoting on a fixed foot
These positions are more safely tolerated following the six week post-operative period. But on account of the selection of hip flexion limitations imposed in the initial six months, usual activities of daily living are rather restricted, making yield to work and daily chores challenging if not impossible from the first few weeks following surgery. Therefore, the post- surgical patient does have to make substantial lifestyle changes and they need assistance in the first six weeks following surgery.
Special precautions in certain types of FAI processes. Reshaping of the femoral head- neck junction can weaken the rectal neck so particular care must be taken in this post- operative period. Fracture of the femoral neck is an unlikely but potentially serious complication after a reshaping process. The athlete may be allowed to bear full weight, but crutches are needed to avoid twisting movements during the initial four weeks after surgery. High impact pursuits and high torsion moves should be prevented in the first 3 months, as bone grafting requires around three weeks to attain full structural integrity.
Furthermore, if microfracture of this femoral head is also done for femoral head cartilage defects, then the athlete ought to be restricted to partial weight- bearing for two weeks so as to optimize the premature maturation of the fibrocartilaginous healing response.
Contents
Key points
1. Weight bearing status is dependent on the kind of reshaping procedure, whether the labrum was repaired, and also what the surgeon favors
2. Steer clear of hip flexion beyond 60� in the first 4-6 Weeks
3. Avoid extremes of rotation
Post-Surgical Rehab
Rehabilitation protocols provided in the literature have a tendency to be quite generic in their own advice and at best explain broad transitional phases during the rehab process. They usually describe the transition in weight bearing status, the development of gait through walking into jogging, and give general guidelines as to how to and when to progress activity based on a time dependant strategy.
They then progress describing transitions into twisting and affect actions — usually explained as beginning at 3 weeks following surgery — and generally the guidance is that the speed with which the athlete progresses is variable and might need yet another 1 to 3 months to get full return based on the game. Trainers are usually advised that return to sports after surgical correction of FAI can require 4 to 6 weeks. However it’s critical that progression through rehabilitation phases is driven more by subjective and objective measures during the transition phases. This allows the athlete and therapist to track load (type and quantity) and ascertain whether the joint arrangements are able to withstand changes in load securely.
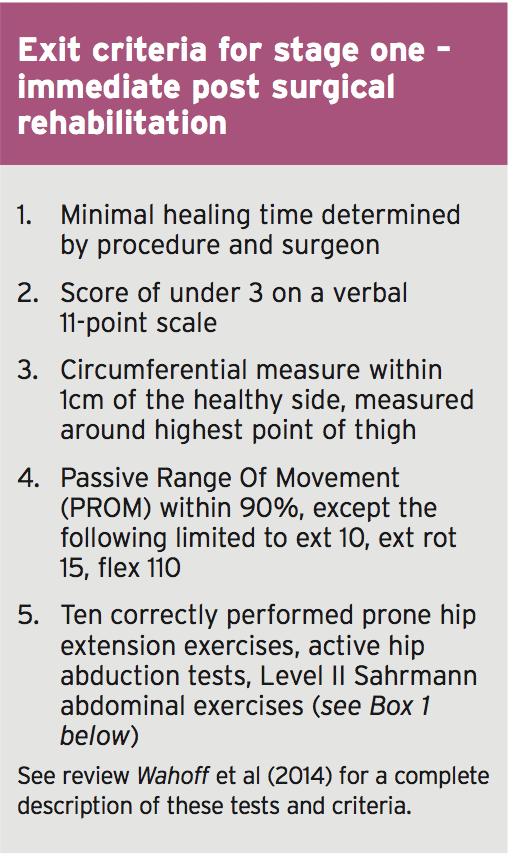
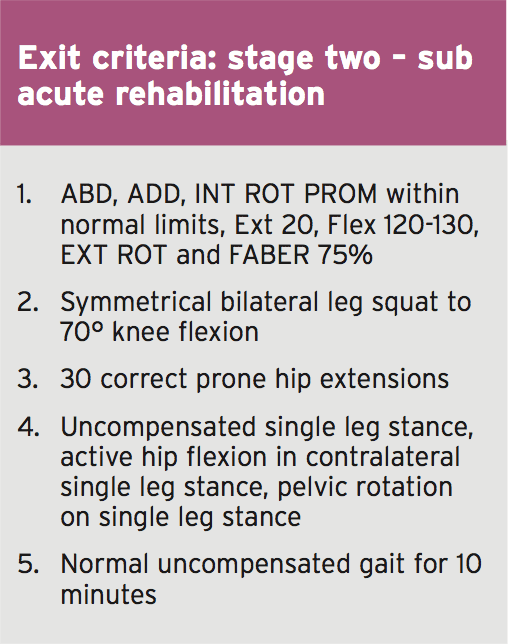
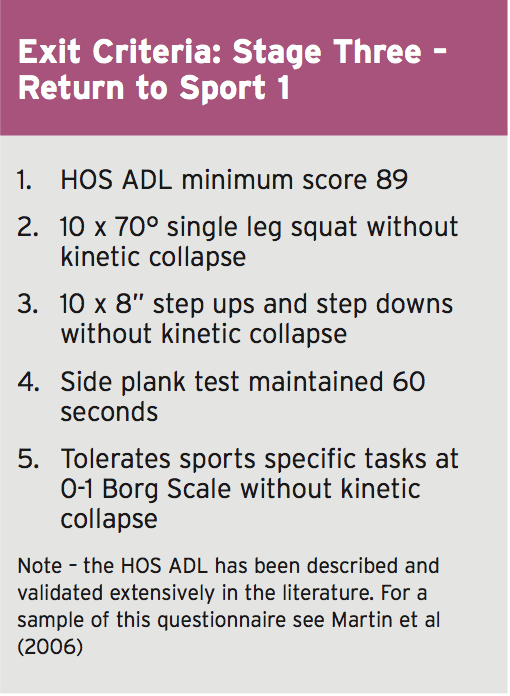
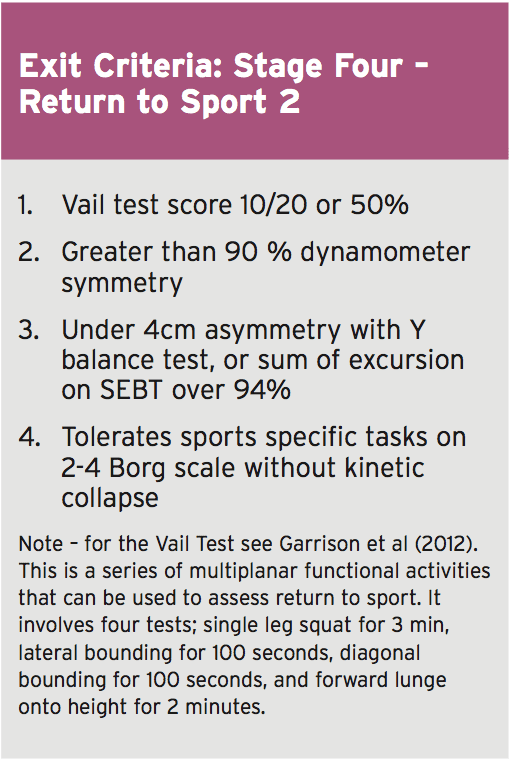
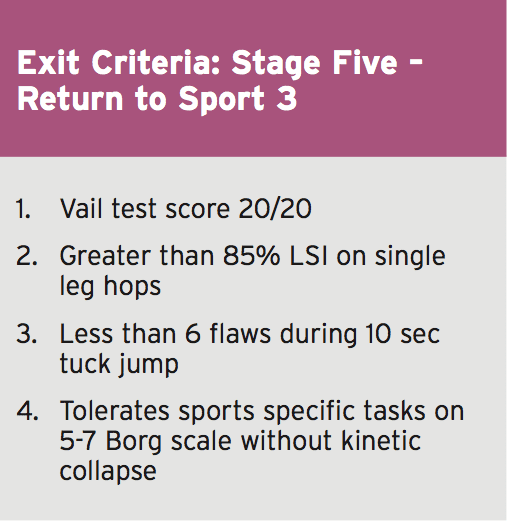
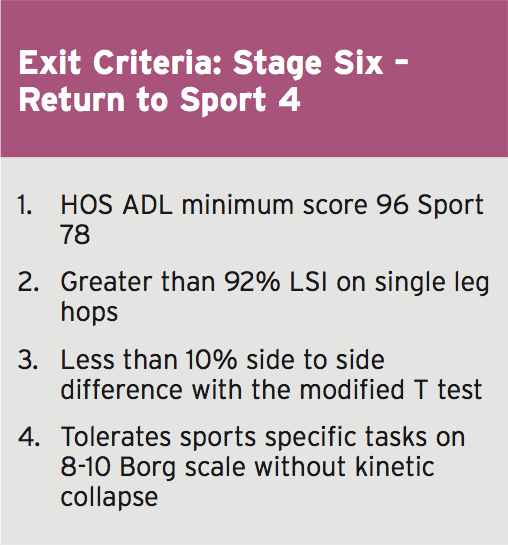
Wahoff et al (2014) have provided some standards which may be utilized to guide the transition from one point to the next(1). They describe their rationale and supply a complete description of all of the cited tests in their printed clinical comment. Essentially, the exit criteria they offer in each phase are as follows;
 So as to advance through the six clarified stages, the athlete may undergo extensive physiotherapy, focusing on hip range of movement exercises, manual therapy and trigger point releases, active stretching, potentially deloaded activities like hydrotherapy or Alta G walking/ running and strong hip rotator and gluteal strengthening exercises. Much of this will be ‘controlled’ and led by the wishes of the surgeon as they will provide the framework on if and what happens concerning loading.
So as to advance through the six clarified stages, the athlete may undergo extensive physiotherapy, focusing on hip range of movement exercises, manual therapy and trigger point releases, active stretching, potentially deloaded activities like hydrotherapy or Alta G walking/ running and strong hip rotator and gluteal strengthening exercises. Much of this will be ‘controlled’ and led by the wishes of the surgeon as they will provide the framework on if and what happens concerning loading.
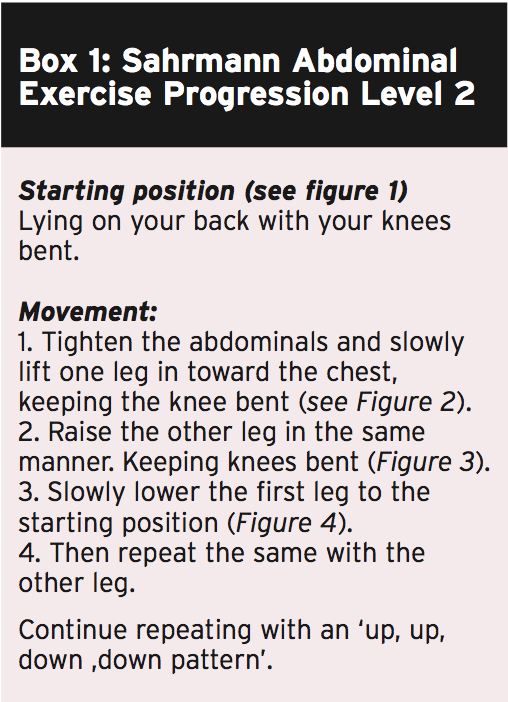
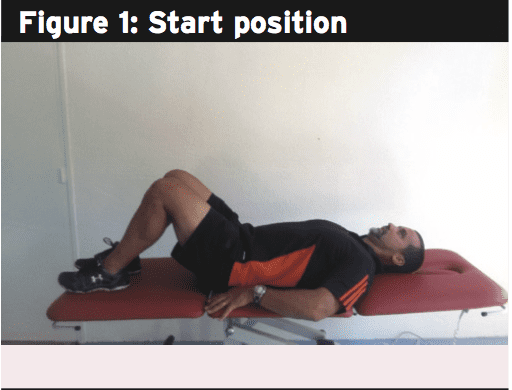
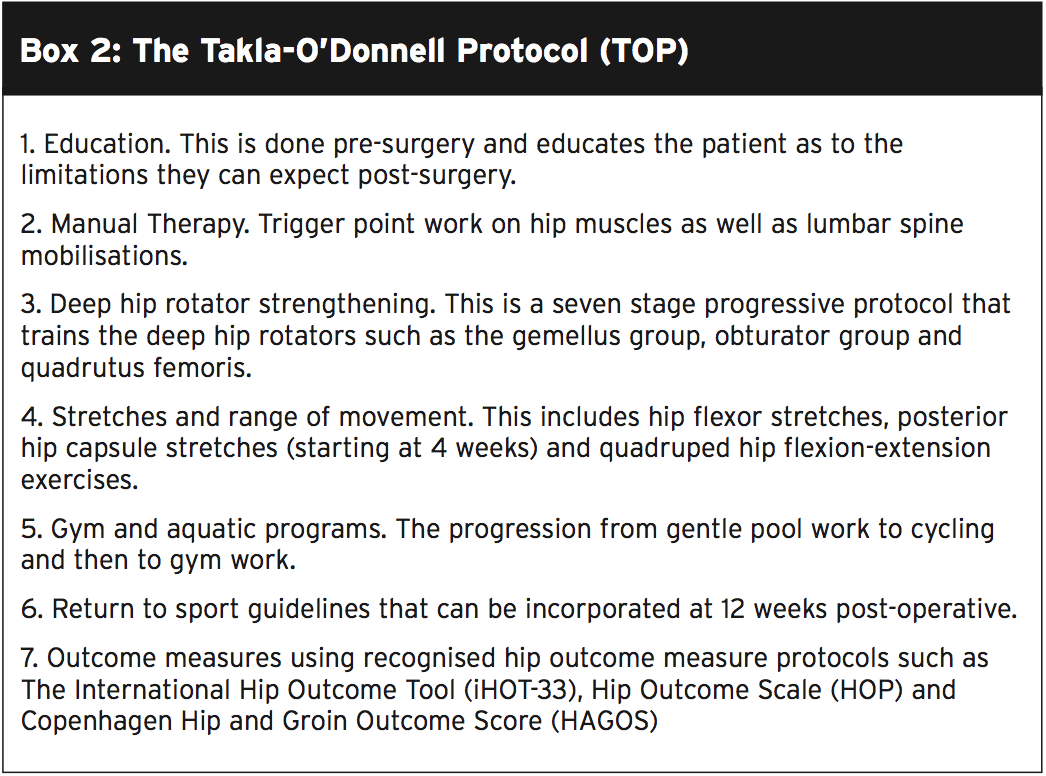
But more direct physiotherapy Interventions have been devised to direct the physiotherapist through the rehabilitation protocol. The Takla-O�Donnell Protocol (TOP) is a validated physiotherapy intervention program which may be utilized to induce the arthroscopically handled FAI patient (Bennel et al)(2).)�This protocol is shown in box 2.
 Hip Muscle Control
Hip Muscle Control
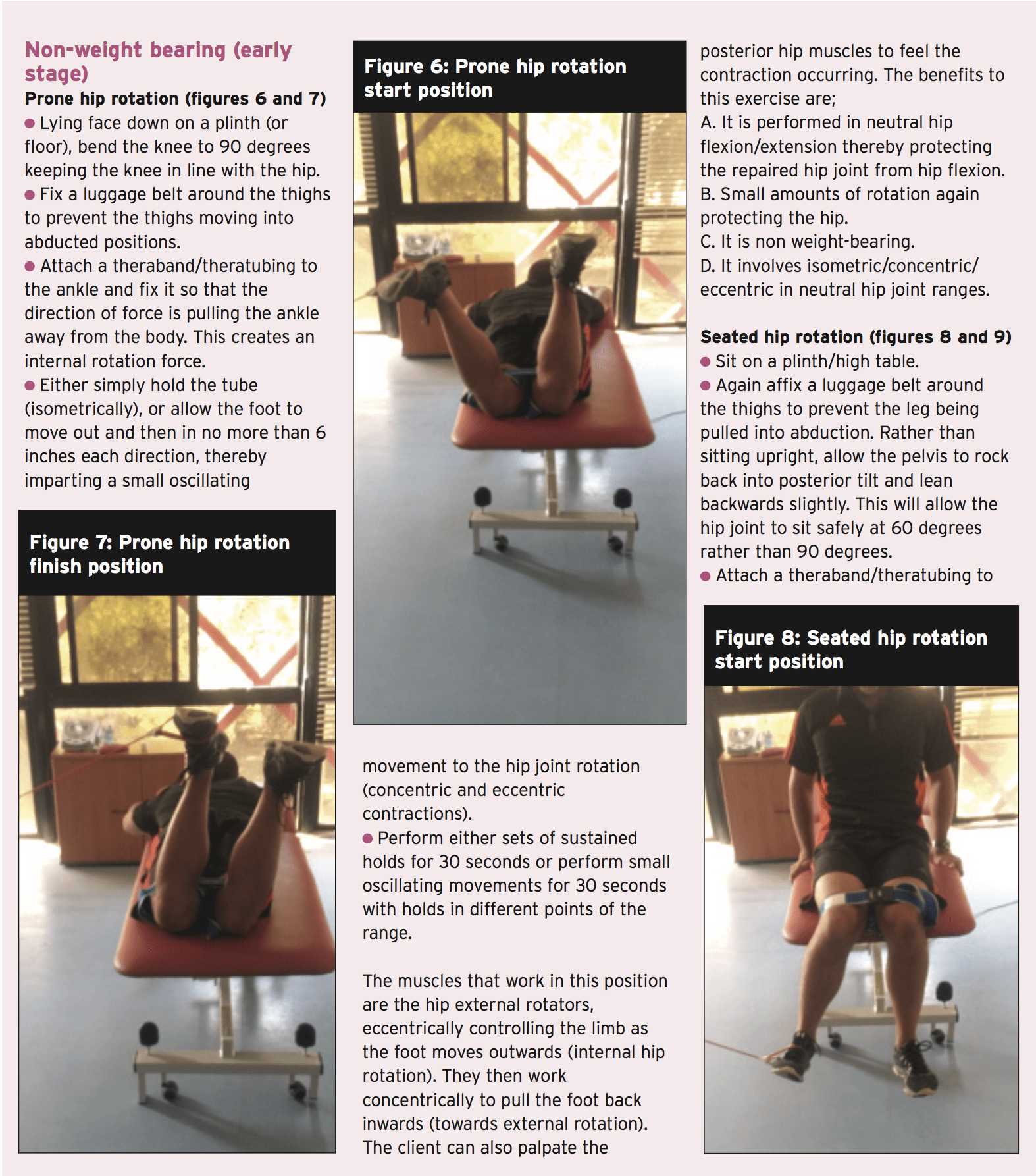
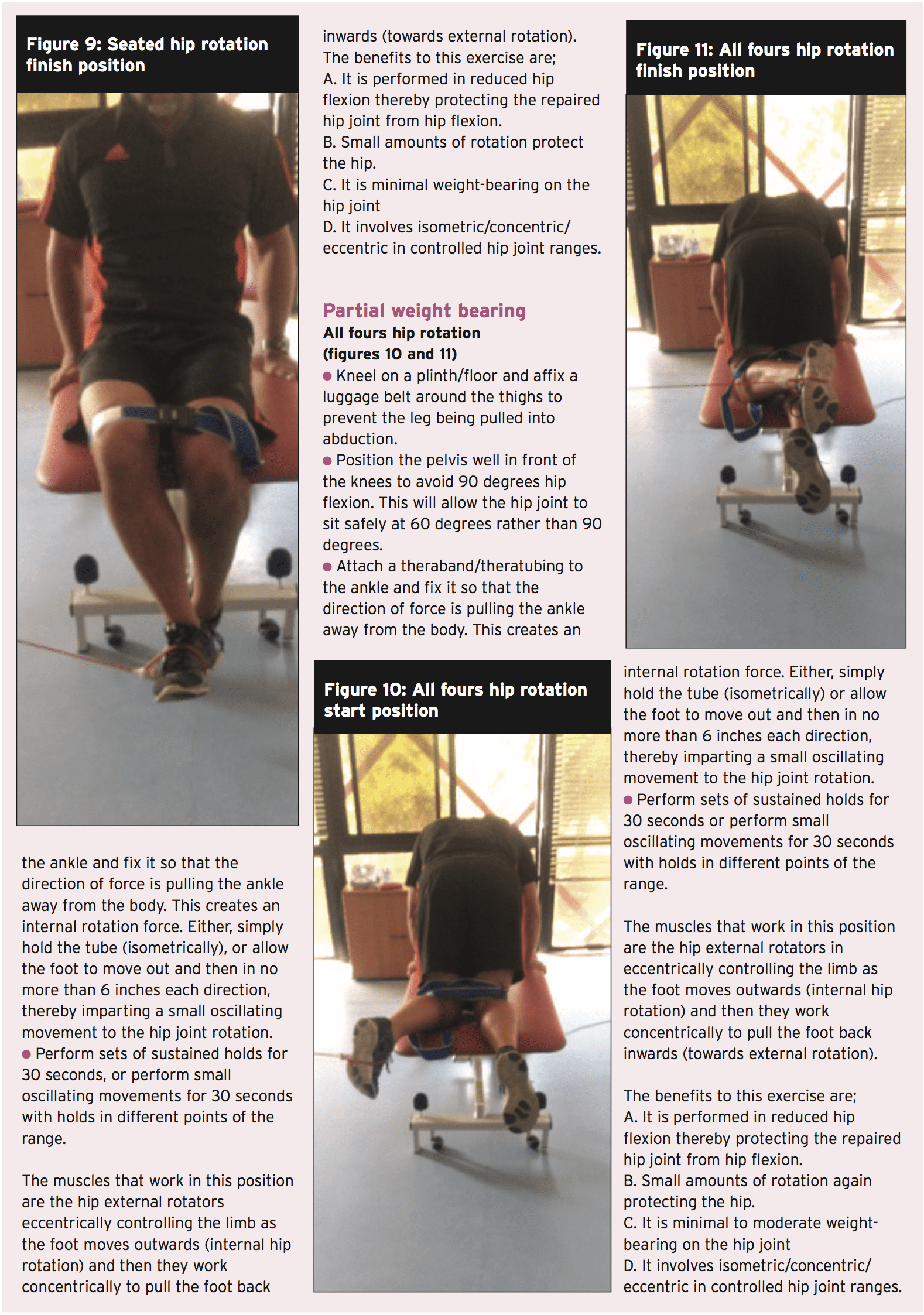
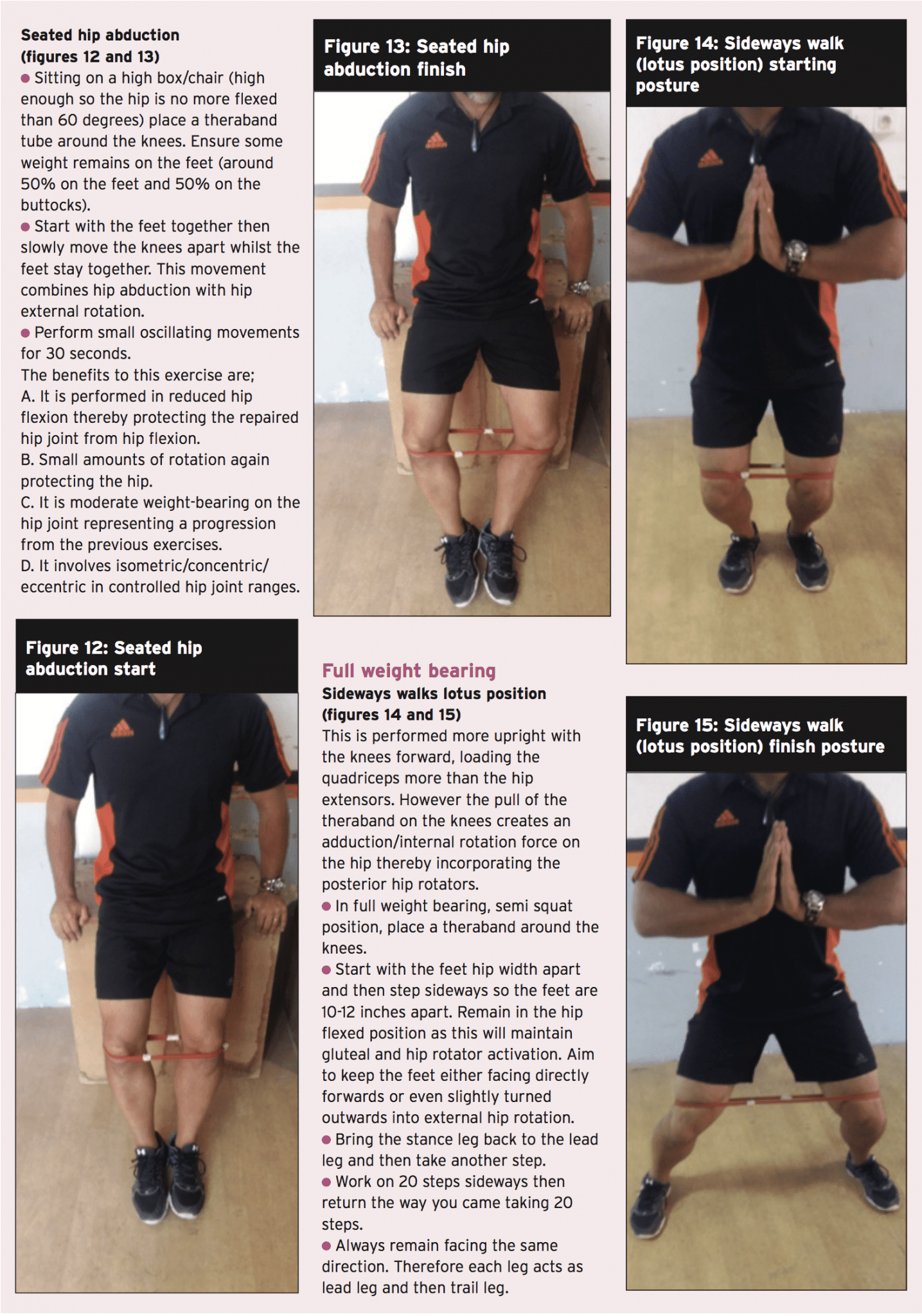
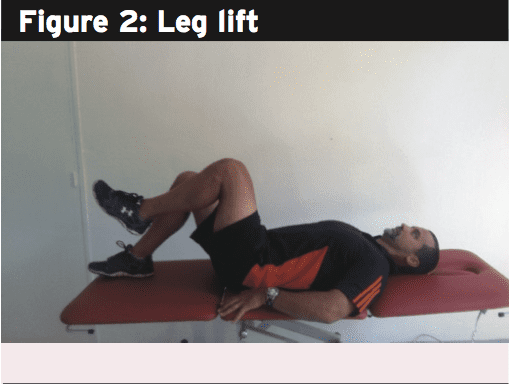
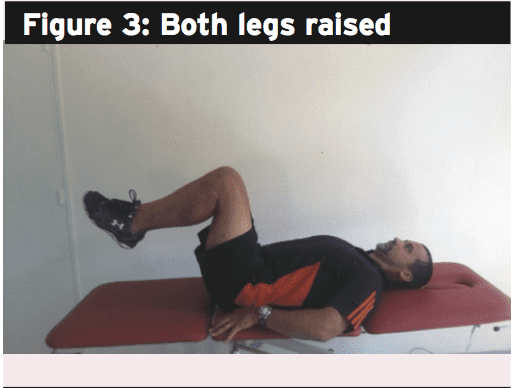
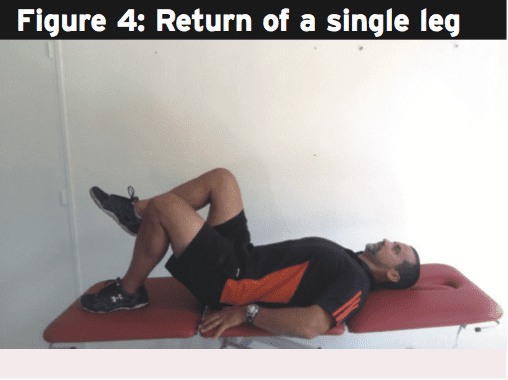
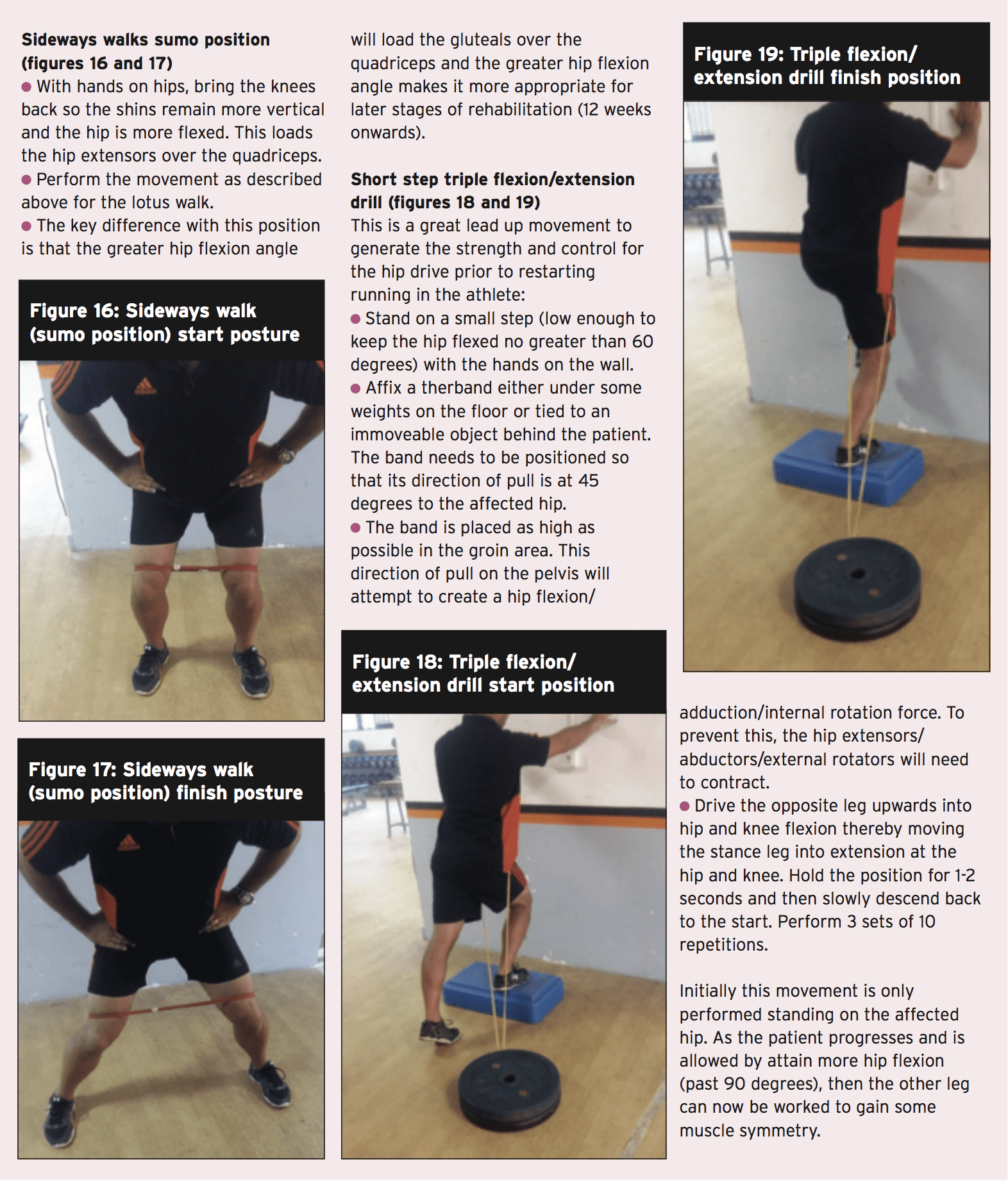
The focus of the rest of this article Will be to summarize some common yet powerful hip strengthening exercises which may be used to progress the hip muscle control throughout the rehabilitation phases.
Regaining hip muscle power, particularly in the heavy hip external rotator group, is imperative from the FAI recovering athlete. Good muscle endurance and strength in those muscle groups will ensure adequate hip joint compression happens with motion to reduce any shearing effect between the head of femur and acetabulum(3). The muscle groups needing focus are (see figure 5):
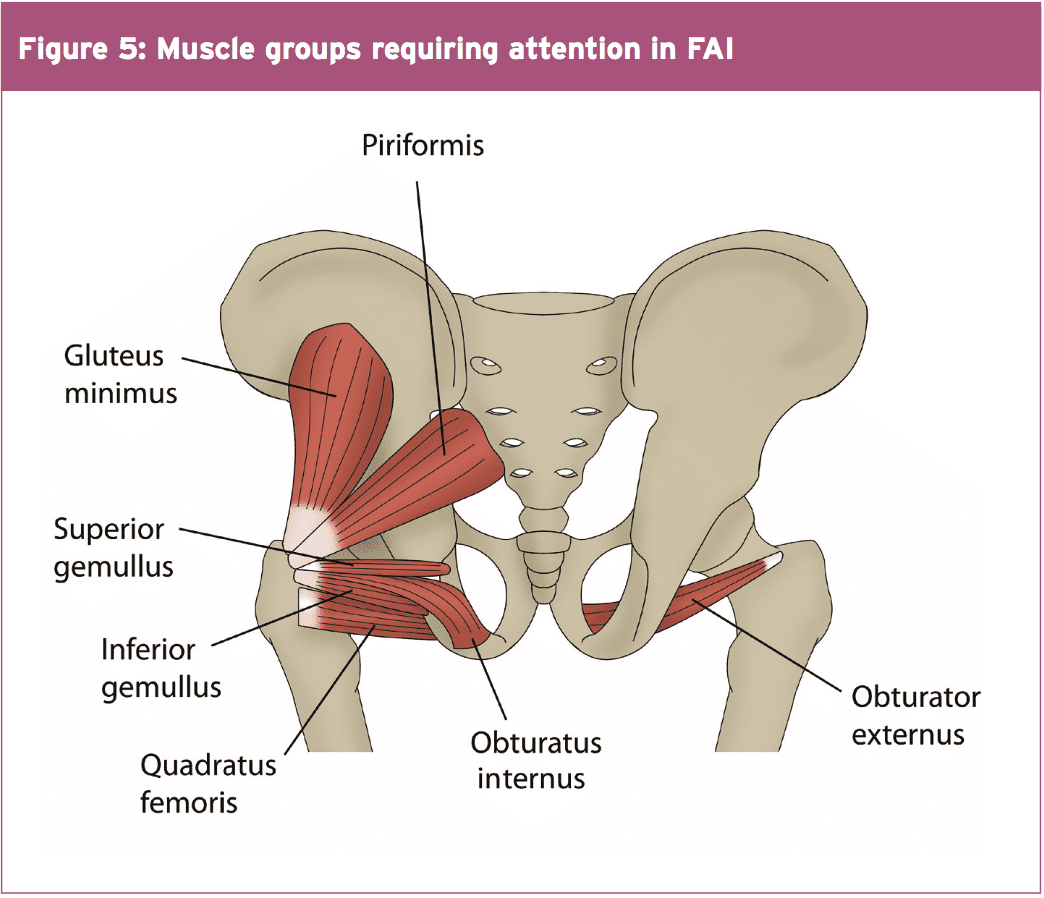
- Posterior fibres Gluteus Medius (PGMed)
- Gluteus minimus
- Superior and Inferior Gemellus
- Internal and External Obturator
- Quadratus Femoris
- Piriformis
There’s plenty of exercises that can be utilized to fortify the hip joint musculature. The chosen ones below are a sample of some effective exercises that can be used throughout the rehabilitation phases. However, the key requirements of the contained exercises include:
1. Performed in neutral stylish places to no more than 60 degrees hip flexion. This range of movement protects the hip joint from any possibly damaging impingement.
2. Minimal rotation of the hip, letting them be used in most stages of the rehabilitation process.
3. Performed isometrically or utilizing little oscillating concentric/eccentric contractions — to contract and hold to maintain the hip joint compacted and stable. This represents how these muscles work in individual function.
 Summary
Summary
In many ways. hip joint labral tears, capsule sprains, cartilage and muscle accidents and bony architectural issues like FAI can all lead to debilitating hip pain. FAI is a real concern for the athlete as the existence of a bone abnormality may lead to a painful hip impingement, damage to the acetabular labrum and premature onset degeneration. FAI’s don’t respond to conservative management. If the athlete suffers debilitating pain that affects competition then the options are either to cease competition all together or have the FAI surgically corrected. Once corrected by the surgeon, regaining complete motion and muscle strength and ultimate game related functional skills will require some time. Hip rotator muscle strengthening must shape the foundation of all handling post-surgical FAI issues.
References
1. International Journal of Sports Physical Therapy. 9(6); pp 813-826
2. Arthroscopy. 2006;22(12):1304-1311
3. Int J Sports Phys Ther. 2012;7(1):20-30.
General Disclaimer, Licenses and Board Certifications *
Professional Scope of Practice *
The information herein on "Hip Impingement Part II: Post Surgery" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and on our family practice-based chiromed.com site, focusing on naturally restoring health for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez, DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card