Athletes and physically active individuals who participate in activities, exercises, and sports that involve kicking, pivoting, and/or shifting directions can develop pelvis overuse injury of the pubic symphysis/joint at the front of the pelvis known as osteitis pubis. Can recognizing the symptoms and causes help in treatment and prevention?
Contents
Osteitis Pubis Injury
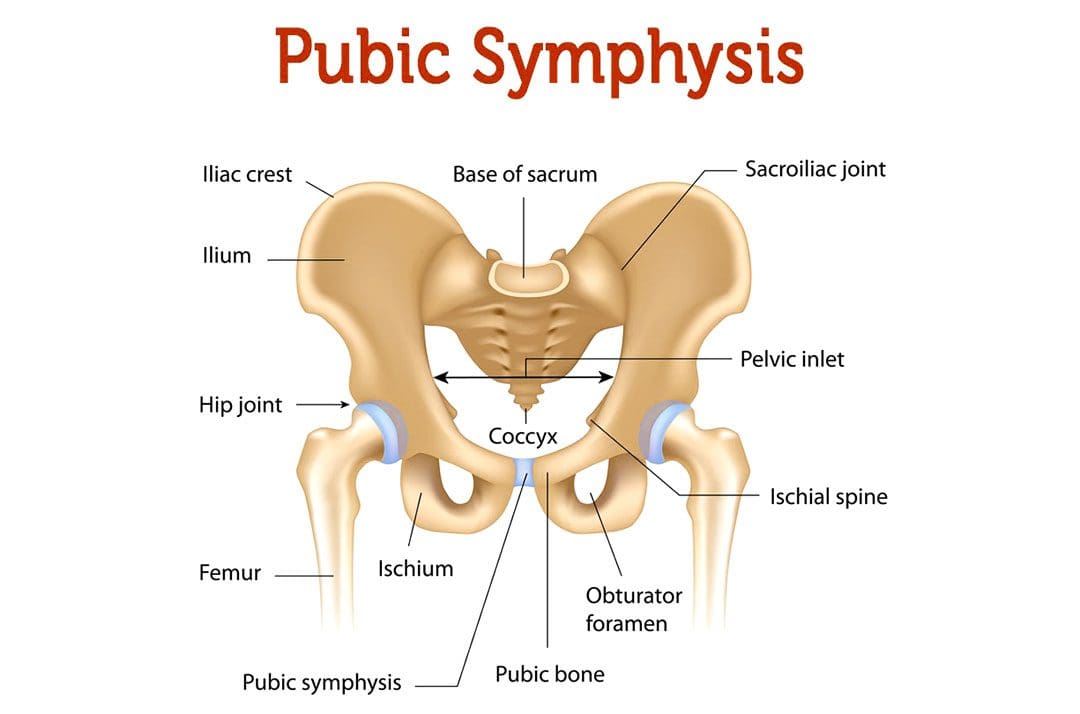
Osteitis pubis is the inflammation of the joint that connects the pelvic bones, called the pelvic symphysis, and the structures around it. The pubic symphysis is a joint in front of and below the bladder. It holds the two sides of the pelvis together in the front. The pubis symphysis has very little motion, but when abnormal or continued stress is placed on the joint, groin and pelvic pain can present. An osteitis pubis injury is a common overuse injury in physically active individuals and athletes but can also occur as the result of physical trauma, pregnancy, and/or childbirth.
Symptoms
The most common symptom is pain over the front of the pelvis. The pain is most often felt in the center, but one side may be more painful than the other. The pain typically radiates/spreads outward. Other signs and symptoms include: (Patrick Gomella, Patrick Mufarrij. 2017)
- Lower abdominal pain in the center of the pelvis
- Limping
- Hip and/or leg weakness
- Difficulty climbing stairs
- Pain when walking, running, and/or shifting directions
- Clicking or popping sounds with movement or when shifting directions
- Pain when lying down on the side
- Pain when sneezing or coughing
Osteitis pubis can be confused with other injuries, including a groin strain/groin pull, a direct inguinal hernia, ilioinguinal neuralgia, or a pelvic stress fracture.
Causes
An osteitis pubis injury usually occurs when the symphysis joint is exposed to excessive, continued, directional stress and overuse of the hip and leg muscles. Causes include: (Patrick Gomella, Patrick Mufarrij. 2017)
- Sports activities
- Exercising
- Pregnancy and childbirth
- Pelvic injury like a severe fall
Diagnosis
The injury is diagnosed based on a physical examination and imaging tests. Other tests may be used to rule out other possible causes.
- The physical exam will involve manipulation of the hip to place tension on the rectus abdominis trunk muscle and adductor thigh muscle groups.
- Pain during the manipulation is a common sign of the condition.
- Individuals may be asked to walk to look for irregularities in gait patterns or to see if symptoms occur with certain movements.
- X-rays will typically reveal joint irregularities as well as sclerosis/thickening of the pubic symphysis.
- Magnetic resonance imaging – MRI may reveal joint and surrounding bone inflammation.
- Some cases will show no signs of injury on an X-ray or MRI.
Treatment
Effective treatment can take several months or longer. Because inflammation is the underlying cause of symptoms, the treatment will often involve: (Tricia Beatty. 2012)
Rest
- Allows the acute inflammation to subside.
- During recovery, sleeping flat on the back may be recommended to reduce pain.
Ice and Heat Applications
- Ice packs help reduce inflammation.
- The heat helps ease pain after the initial swelling has gone down.
Physical Therapy
- Physical therapy can be extremely helpful in treating the condition to help regain strength and flexibility. (Alessio Giai Via, et al., 2019)
Anti-inflammatory Medication
- Over-the-counter nonsteroidal anti-inflammatory medications – NSAIDs like ibuprofen and naproxen can reduce pain and inflammation.
Assistive Walking Devices
- If the symptoms are severe, crutches or a cane may be recommended to reduce stress on the pelvis.
Cortisone
- There have been attempts to treat the condition with cortisone injections, but the evidence supporting its use is limited and needs further research. (Alessio Giai Via, et al., 2019)
Prognosis
Once diagnosed, the prognosis for full recovery is optimal but can take time. It can take some individuals six months or more to return to pre-injury level of function, but most return by around three months. If conservative treatment fails to provide relief after six months, surgery could be recommended. (Michael Dirkx, Christopher Vitale. 2023)
Sports Injuries Rehabilitation
References
Gomella, P., & Mufarrij, P. (2017). Osteitis pubis: A rare cause of suprapubic pain. Reviews in urology, 19(3), 156–163. doi.org/10.3909/riu0767
Beatty T. (2012). Osteitis pubis in athletes. Current sports medicine reports, 11(2), 96–98. doi.org/10.1249/JSR.0b013e318249c32b
Via, A. G., Frizziero, A., Finotti, P., Oliva, F., Randelli, F., & Maffulli, N. (2018). Management of osteitis pubis in athletes: rehabilitation and return to training – a review of the most recent literature. Open access journal of sports medicine, 10, 1–10. doi.org/10.2147/OAJSM.S155077
Dirkx M, Vitale C. Osteitis Pubis. [Updated 2022 Dec 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: www.ncbi.nlm.nih.gov/books/NBK556168/
Professional Scope of Practice *
The information herein on "Comprehensive Guide to Recovery from Osteitis Pubis Injury" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Our information scope is limited to Chiropractic, musculoskeletal, physical medicines, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somatovisceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and/or functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez, DC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, RN*, CCST, IFMCP*, CIFM*, ATN*
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807, New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Florida
Florida License RN License # RN9617241 (Control No. 3558029)
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Dr. Alex Jimenez DC, MSACP, RN* CIFM*, IFMCP*, ATN*, CCST
My Digital Business Card






