by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chiropractic, Health
Have you ever wondered how many years your treating chiropractic doctor went to school for or how their education compares to that of other health care professionals? Knowing your doctor’s educational background and additional certifications is often essential to helping you choose the health care provider that is right for you. While the word�”doctor” automatically implies an extensive academic curriculum, each health care specialist has a unique and individualized educational program to complete prior to practicing in the field. Our doctors�have designed this article to help you understand your chiropractor�s educational background and how it may affect your care.
Chiropractors Educational Requirements?
As with many professionals, the specific requirements outlined often vary from state to state. Typically, chiropractors are required to have completed undergraduate pre-medical studies and obtained a bachelor�s degree prior to admission to a post graduate chiropractic college. Each chiropractic college has undergone a meticulous evaluation process to become certified by the Department of Education as an accredited educational institution.
The amount of time that your chiropractic doctor spends at a specific chiropractic academic institution is impressive. In fact, your chiropractor has spent a minimum of 4,200 hours at a chiropractic college prior to receiving his diploma. This time is spent in the classroom, laboratory, and clinic learning about the various aspects of the chiropractic profession and health care in general.
In the classroom, your doctor focuses his studies on the subjects of anatomy, physiology, diagnosis, pathology, biochemistry, neuromuscular and orthopedic evaluation, pediatric and geriatric care, microbiology, nutrition, immunology, radiology, philosophy, and clinical research. While this may seem like a lot, all of this information is assimilated and tested prior to advancement to clinical work. Once the student has completed his academic work, he will typically spend a minimum of 1,000 hours at a campus clinic under the guidance of a clinic doctor. During this time he will learn hands on how to diagnosis and treat patients in real clinical situations.
During your chiropractors education they will be tested through a number of different evaluations. Not only is your doctor subject to evaluation by their chiropractic college, they must also pass a series of national board examinations. Chiropractors practicing in the United States are required to have passed a series of four national board exams which evaluate them on their understanding of the basic sciences, clinical sciences, physiological therapeutics, diagnostic imaging, case management, and clinical competency. In addition to these requirements, following graduation and completion of national board examinations, each chiropractor must become certified by their state licensing agency.
The completion of these standards is not the end of the educational journey for chiropractic doctors. Depending on the state, each chiropractor is required to complete additional approved course work at designated times following their licensure. For example, Wisconsin requires a minimum of 40 hours of continuing education every two years following graduation.
Chiropractors Education In Comparison To Other Health Care Professionals?
After reading the above information, I feel it is safe to say that your chiropractic doctor knows far more about your health than just treating your back. To help understand this it is useful to compare a chiropractor�s education to other members of the health care community. Since many people are familiar with a medical doctor, we will compare their educational background with that of a chiropractic doctor. For starters, the typical chiropractic student will have completed a total of approximately 2,419 hours of academic work prior to the initiation of clinical studies. In comparison, the majority of medical students will have completed somewhere around 2,047 hours of study. Further, while each health care discipline has its strengths, chiropractic students undergo more hours of study in the fields of anatomy, embryology, physiology, biochemistry, diagnosis, x-ray, and orthopedics. In contrast, medical practitioners have had more classroom hours studying the subjects of pathology, psychology, and obstetrics.
When analyzing these numbers it is important to understand that while differences exist, each of your doctors has undertaken and completed a similar core education. In addition, it is important to remember that each of your doctors (even in the same health care discipline) possess various strengths to compensate for other health care professionals’ weaknesses and utilize a different approach to healing the body. In the end, finding the doctor that understands your needs and has the tools to provide you with the most appropriate care is what is important.

Call Today!
by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Fitness, Intermittent Fasting, Natural Health, Weight Loss, Wellness
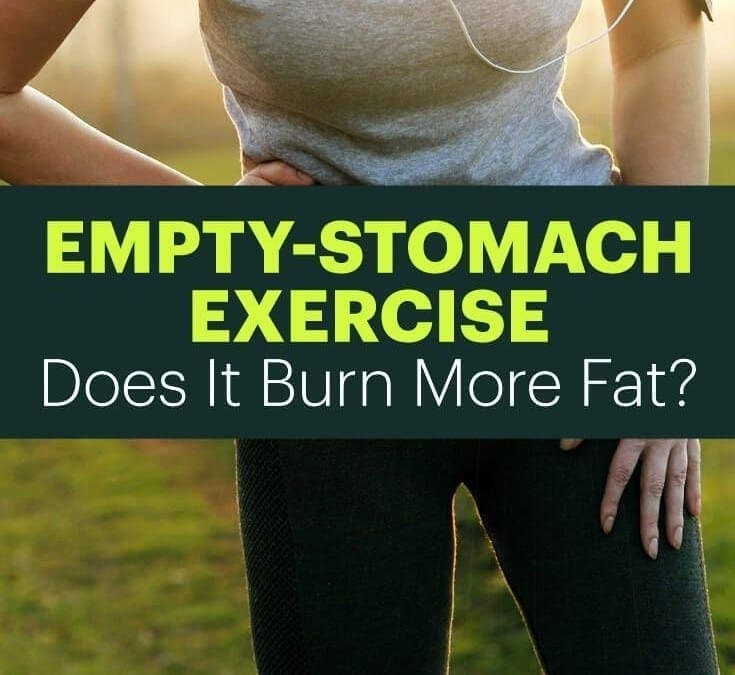
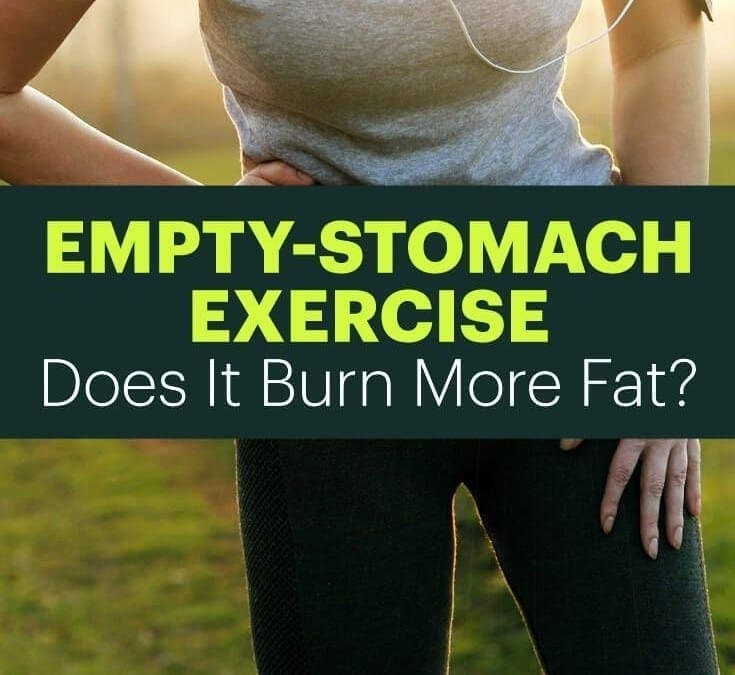
El Paso, TX. Chiropractor Dr. Alex Jimenez examines working out on an empty stomach.
For a thing that should be simple, working out doesn�t consistently feel that way. There�s choosing the best fat-burning workout. There�s that pesky question of whether diet or exercise is essential for fat loss. And there�s a new one to throw into the mix: whether working out on an empty stomach can help you shed weight faster.
Bodybuilders swear by it while many people religiously enjoy their pre -workout protein shake. What exactly gives? Should you hitting the gym on an empty stomach and be forgoing food in the event you want to lose pounds?
Regrettably, like so much fitness guidance, this falls into the grey, �it depends� place. Let�s inquire.
Work Out On an Empty Stomach?
The theory behind exercising having an empty tummy is that when you squeeze before breakfast, your body burns fat faster.
See, what occurs is that glycogen, a type of carbohydrate which our bodies shop, � runs out� overnight. When you wake up and hit the gym first thing in the morning, because your body is low on carbs, the notion is the body will really turn to fats next to obtain energy. (1)
Things do get tricky because if the body is completely from glycogen � you had an early dinner, got the full nighttime�s remainder and perhaps snoozed an extra hour or two � the body might bypass fat burning and head directly to muscle shops instead, chipping away at body definition.
�
Advantages of Working Out On an Empty Stomach
So what does the science say the huge benefits before working out to missing breakfast?
1. Burn Fat Quicker. One study followed 12 active males after breakfast who ran on the treadmill either or while they were still fasting from the night time before. (2) The men who hadn�t broken their fast, i.e. hadn�t had breakfast, burned up to 20 percent more body fat during the same work outs.
What�s especially fascinating is that the guys who jumped breakfast didn�t overeat after or attempt to otherwise make � for the early AM calories up they missed out on. So obtaining a head start on your fitness regimen pre-breakfast can help you lose more fat without making you sneak in extra calories later.
2. Improve Performance. There�s evidence that exercising when your carb levels are low, like when you�re on an empty stomach, actually helps improve functionality during �normal� workouts. The concept behind �train low, compete � that is high is that working out in a glycogen- low state helps the body become more efficient at burning off fat so at times when carb levels are quite high, the body is primed and raring to go. (3)
3. Time-Restricted Eating Can Help In Losing Weight. Work Out out on an empty stomach ties into the thought of time-limited eating. On this diet program, it is possible to eat as much as you want of anything you desire. The only caveat is that you just eat strictly between certain hours, with 12�16 hours of time where you don�t eat anything.
The notion is that when our bodies understand just when we�re going to be eating, our hormones react by burning fat and supporting weight reduction during the food-free hours. Scheduling workouts during fasting hours could encourage the body to burn more fat, particularly when you�re exercising first thing in the morning.
4. Improve Body’s Response To Insulin. When we eat, our bodies release insulin to consume all of the nutrients in the foods we�re enjoying. However, as soon as we�re eating way too many carbohydrates and sugar, our bodies become resistant to insulin � it�s unable to do its job at the same time.
All that insulin can bring in regards to an assortment of chronic illnesses and builds up. Among many health benefits of fasting, however, is reducing that susceptibility to insulin. Without continuous food, insulin isn�t so our bodies don�t become immune to the hormone, created often.
5. Inspiration To Work Out More.�Let�s confront it � we�re all super active. By working out each morning before stopping to make breakfast, having that cup of coffee or whatever it’s that might derail you in the mornings, you can get your calorie burning out of the way with no distractions that happen after.
In the event you have to be out of your house by 8 a.m., it�s a lot easier to hit the gym before eating as opposed to sitting down for breakfast, waiting to digest and then working out.
When It�s Not Wise To Work Out Without Any Food On Board
But working out on an empty stomach might not be the finest idea for everybody. For each study that says burning fat occurs more easily when you exercise before eating, there�s another one that says the opposite. An International Journal of Sport Nutrition and Exercise Metabolism study found that a pre-workout snack or light meal actually helps burn body fat. (4)
Plus study found no difference in weight reduction between women who ate a meal-replacement shake before exercising without eating and those that got directly in their workouts. (5)
Another problem is that without any fuel in your belly, you may well not be working out as hard as you could. A pre-workout snack that�s a mix of carbs, protein and healthy fats can give you the energy you need to push yourself harder.
That extra fire might be just things you must finish high-intensity interval workouts like Crossfit or Tabata, which actually help you burn off more calories in a briefer amount of time. These are intense work outs where you�re likely to need to max out your energy.
And when you�re training for endurance sports like long-distance racing or a triathlon, working out on an empty stomach might work for short distances, but you definitely wish to consume before longer work outs � depending on how much you�re going, you might even need to refuel during training.
Finally, if you�re someone who psychologically has to realize which you aren�t going to burn out mid way because you�ve eaten through exercising, it�s not a great day to work out on an empty stomach. Same goes for people who are diabetic or experience low blood sugar. Eating a small bite will make sure that you remain safe throughout your workout.
Final�Thoughts
I wish I possibly could tell you that working out on an empty stomach will cause results that are better. But because numerous variables are at play � how fit you are, what type of exercise you�re doing and the way you workout best � it�s impossible.
What is vital is that you just remain hydrated before, during and following your workout. Drinking enough water will keep up energy levels. Drinking enough H2O can also keep pounds from increasing because thirst is, in addition, mistaken for hunger.
Maybe more notably than whether you eat before a workout is what you�re having later. A mix of protein and healthy carbs can help muscle tissue recover. Drinking a post-workout recovery shake or eating eggs with veggies in the first 45 minutes after exercise while your blood is circulating well is ideal. Take a look at my list of 43 greatest post-workout meals for quicker results � you�re certain to find something you�ll adore.
Eventually, whether you�re working out on an empty stomach or not, kudos to you for getting out there and taking control of your quality of life. Keep up the work outs!

Call Today!

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Diets, Fitness
Drinking 32 ounces of energy drink is associated with potentially harmful changes in blood pressure and heart function that are beyond those seen with caffeine alone, according to a new study.
There are more than 500 energy drink products on the market, and their increased popularity is matched by a significant rise in energy drink-associated emergency department visits and deaths.
Manufacturers and fans of these products claim they are as safe as caffeine, but there is little evidence to support that claim.
Caffeine in doses up to 400 mg (about five cups of coffee) is generally recognized as safe by the Food and Drug Administration. While energy drinks usually contain caffeine, little is known about the safety of some of their other ingredients the study team writes in the Journal of the American Heart Association.
To see what effects these other components have, researchers compared physical changes in a group of 18 healthy men and women after consuming a commercially available energy drink and after drinking another concoction with the same amount of caffeine but none of the other ingredients.
Besides 320 mg of caffeine – the amount in about four cups of coffee – the energy drink contained 4 ounces of sugar, several B vitamins and a proprietary “energy blend” of taurine and other ingredients that are often found drinks like Monster Energy, Red Bull and 5-Hour Energy.
Sachin A. Shah of David Grant Medical Center on Travis Air Force Base and University of the Pacific in Stockton, California, and colleagues measured the participants’ blood pressure and used an electrocardiogram (often called an ECG or EKG) to measure heart electrical activity for 24 hours after the subjects consumed the drinks.
An ECG change known as QTc prolongation and sometimes associated with life-threatening irregularities in the heartbeat was seen after drinking the energy drink, but not after drinking the caffeine beverage, the study team reports.
Several drugs have been withdrawn from the market just for causing ECG changes of a similar magnitude, the authors note.
Blood pressure increased by close to 5 points after drinking the energy drink, but by just under 1 point after drinking the caffeine beverage. Blood pressure also remained elevated six hours later.
These changes are by no means worrisome for healthy individuals, the researchers say, but patients with certain heart conditions might need to exercise caution consuming energy drinks.
Larger studies are needed to evaluate the safety of the noncaffeine ingredients contained in energy drinks, they conclude.
“The energy drink industry claims that their products are safe because they have no more caffeine than a premium coffee house coffee,” said Dr. Jennifer L. Harris from University of Connecticut’s Rudd Center for Food Policy and Obesity in Storrs, who wasn’t involved in the study.
“However, energy drinks also contain a proprietary ‘energy blend,’ which typically consists of stimulants and other additives. Some of these ingredients (including taurine and guarana) have not been FDA-approved as safe in the food supply, and few studies have tested the effects of caffeine consumption together with these ‘novelty’ ingredients,” she said by email.
“On top of that, energy drinks are highly marketed to adolescent boys in ways that encourage risky behavior, including rapid and excessive consumption,” she said. “As a result, emergency room visits by young people in connection with energy drinks are rising.”
Any research that compares the effects of consuming energy drinks versus caffeine alone provides important evidence for public health advocates who have urged the energy drink companies to stop targeting youth with these potentially harmful products, Harris added.
by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chiropractic, Natural Health
El Paso, TX. Chiropractor Dr. Alex Jimenez focuses on the rise in opioid use among older adults.
SpineUniverse reported on a study that indicated a 10% increase in opioid addiction or dependency in patients prescribed such drugs to take care of postoperative pain. Although spine surgery was not among the forms of operations included in the research, it�s intriguing to see that 3% of the patients ages 55-years plus, disclosed addiction and opioid use.
Older adults as well as the elderly are part of about 100 million adults in the USA (US) affected by severe or chronic pain. Low back pain is neck pain, and among the most frequent causes of pain, followed by headache/ migraine pain. Spinal stenosis, spinal osteoarthritis, and degenerative disc disease are frequent investigations in elderly residents and our mature adult.
In a presentation by Sullivan in 2003 about chronic pain and prescription opioid abuse and dependence in mature adults, it had been reported that �the prevalence of pain increases with each decade of life Additionally, 80% were grown by pain criticisms in adults age 65 and older. Moreover, as the number of opioid prescriptions increased, so did use by older adults�but some medical studies regularly blown off addiction as temporary or rather rare.
Regulators React
Acknowledge and its particular bureaus and the government started to recognize opioid use and the potential risks in elderly Americans. In 2012, a study revealed that more than 700,000 adults (ages 45 to 84) were hospitalized particularly for opioid abuse. Mature adults as well as the elderly accounted for a five-time increase in hospitalizations for opioid abuse compared to younger Americans.
Adults of any age taking an opioid may experience drug unwanted effects that are possibly dangerous. But for mature adults or senior -aged individuals, the hazards are weightier. Why? Old people frequently take several medications simultaneously to treat different medical problems (eg, diabetes, hypertension). It may be a challenge for the patient to keep an eye on when to take a drug that is prescribed or remember if the medicine was taken, which may result in unintentional doses. An opioid drops, and introduces another tier of potential risks, including respiratory depression, lack of balance, confusion, dizziness, drowsiness, nausea.
In 2015, Congress introduced a Medicare-specific bill called �Ceasing Drug Exploitation and Shielding Seniors Act.� Now, we see changes dispensed, and monitored to prevent physician- shopping and other ways drugs could possibly be obtained and abused.

Managing Opioid Medications
Elderly patients or some adult live alone, in a household setting, receive home-health support, or reside in a assisted-living facility or alternative scenario. In some cases, the direction of the medication, including pain-relieving drug is managed by healthcare or nursing staff.
Many older adults and aged patients are quite capable of handling physician�s visits, their drugs, and everyday life. Then there are other people who want support. They might not realize they need help or may not ask. This is where friend, a family member or caregiver might help by being observant and step in to help. By way of example, does the patient take their medication as prescribed, but nevertheless look to be in pain? Does he /she stumble easily or fall, complain about feeling dizzy, confused, constipated, or have a few other criticisms?
Remember that people so do their needs for drugs and change with age. In unwanted effects and handling pain, the alternative can be an alternate kind of drug or a dose change. Considering many senior adults and aged men take multiple medications, it’s an excellent idea to bring OTC medication all prescription and nutritional supplements to each physician�s visit for review. This creates a superb chance for you and the individual to talk together with the doctor about new challenges and health changes.

Call Today!

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Exercise, Fitness, Weight Loss
The problem: When I gain weight, it goes straight to my middle
You know those squishy midsection lumps you can pinch? That’s subcutaneous fat, located just beneath the surface of your skin, says Ursula White, PhD, an obesity researcher at the Pennington Biomedical Research Center at Louisiana State University. Another type of fat, called visceral fat, sits deep within the abdominal area, surrounding the organs. This is the kind that’s considered especially harmful; research has found that excess amounts of visceral fat may put your at a higher risk of heart disease and type 2 diabetes.
Where we pack on flab may be determined by genetics, says White. But in general, notes Tara Collingwood, RDN, coauthor of Flat Belly Cookbook for Dummies ($23; amazon.com)�when people gain weight, it often increases their amount of visceral fat. That’s one reason a diet that’s too high in simple carbs is so problematic: “Eating too many low-fiber, high-sugar foods can spike levels of insulin, which then stores all those calories as fat,” explains Collingwood.
The solution:�You can’t fight genetics�but you can make it harder for your body to store excess calories as fat by limiting your consumption of refined carbs. Eat more high-fiber foods instead, such as oats, beans, and sweet potatoes, suggests Leslie Bonci, RDN, owner of Active Eating Advice. Also, aim to eat three meals and one snack a day�and have them on a set schedule, recommends Bonci. One 2014 study found that eating erratically was linked to a bigger waist circumference than sticking to a schedule.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Natural Health, Wellness
Pregnant women should get their blood pressure checked at each prenatal visit to screen for preeclampsia, a potentially fatal complication that can damage the kidneys, liver, eyes and brain, new U.S. guidelines say.
While many doctors already monitor blood pressure throughout pregnancy, the U.S. Preventive Services Task Force (USPSTF) updated its guidelines for the first time since 1996 to stress that screening at every visit can help doctors catch and treat preeclampsia before it escalates from a mild problem to a life-threatening one.
“Preeclampsia is one of the most serious health problems affecting pregnant women,” task force member Dr. Maureen Phipps, a women’s health researcher at Brown University in Providence, Rhode Island, said by email.
“Because this condition is common and critical, the Task Force offers two separate recommendations to help women lower the risk associated with preeclampsia – screening for preeclampsia is recommended for all pregnant women, and women at high risk of developing the condition can take low-dose aspirin to help prevent it,” Phipps added by email.
The screening recommendations, published on Tuesday in JAMA, apply to women without a history of preeclampsia or high blood pressure. Separate guidelines advise low-dose aspirin after the first 12 weeks of pregnancy for women with a history of elevated blood pressure. (http://bit.ly/2oIwP5B)
Preeclampsia can progress quickly, and typically develops after 20 weeks of pregnancy. Blood pressure screening earlier in pregnancy can show normal results for women who go on to develop preeclampsia.
In addition to elevated blood pressure, women with preeclampsia may also have excess amounts of protein in their urine, as well as swelling in the feet, legs and hands.
Women may suffer from stroke, seizures, organ failure and in rare cases, death. For babies, complications include slower growth inside the uterus, low birth weight and death.
Risks for preeclampsia include a history of obesity, diabetes, kidney disease, lupus or rheumatoid arthritis, as well as a mother or sister who has experienced the condition.
Because the risks of preeclampsia increase with age, women may be able to lower their chances of developing this complication by having babies sooner, said Dr. Dana Gossett, an obstetrics and gynecology researcher at the University of California, San Francisco, and co-author of an accompanying editorial in JAMA.
“Beyond that, it is also important to ensure that all health problems are well managed prior to pregnancy,” Gossett said by email. “High blood pressure should be under good control, other diseases like kidney disease or lupus should be well controlled, and women should try to be close to their ideal body weight prior to conception.”
Checking blood pressure at every prenatal visit can help prevent complications for mothers and babies alike, said Dr. Martha Gulati, chief of cardiology at the University of Arizona College of Medicine in Phoenix and author of a separate editorial in JAMA Cardiology.
“This is something that should be provided to every woman as part of preventive care,” Gulati said by email. “We will save lives and prevent complications and death in pregnant women with this simple, cost-effective” test that doesn’t take much time.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chiropractic, Lower Back Pain, Natural Health
El Paso, TX. Chiropractor Dr. Alex Jimenez looks at back pain medications and their effect on sleep.
Can you relieve spine pain and get a good night�s rest? Sure some drugs get in the way.
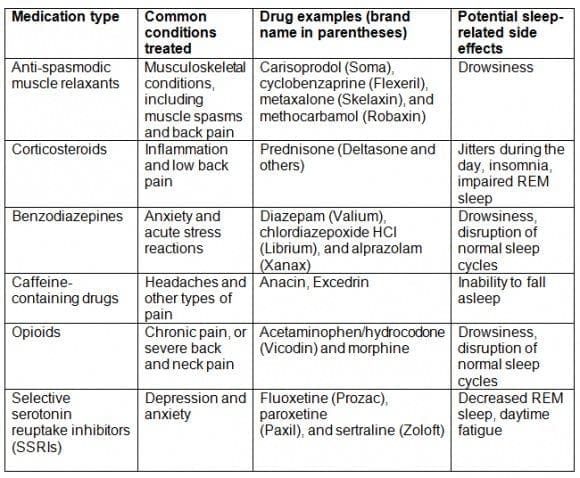
Prescription medications are among the most recommended nonsurgical treatments for back and neck pain. While these drugs might help alleviate what ails your back, your sleep may suffer because of this. That�s a big deal, as sleep deprivation hurts your general wellbeing.
Unfortunately, back and neck pain medications can have side effects�and interfering with your sleep and ability to operate normally throughout the day are ones that are typical. Your medication may stop you from getting enough sleep or falling asleep. Or, your slumber quality suffers, although you might doze off readily. Plus, sleep-related side effects do n�t just affect you during the nighttime hours, as you may experience drowsiness or jitters during the day.
Sleep Science 101: Reconsidering Sedatives
Before delving into common back and neck pain drugs that may affect your slumber, it�s important to comprehend one of the biggest misconceptions about sleep medicines: the effect of sedation.
Many view sedatives as sleep aids due to the fact that they enable you to fall asleep fast. Nevertheless, this doesn�t tell the entire image, based on Steven A. King, MD, MS, who practices pain medicine in New York and is a clinical professor of Psychiatry at the New York University School of Medicine.
�When contemplating what�s good for sleep, it really is vital to not forget that sleep is just not a uniform activity through the entire span of the night, but rather, a succession of cycles involving different levels of wakefulness,� wrote Dr. King in a site for Psychiatric Times. �Merely because a medication may put one to sleep doesn�t mean restful slumber will be provided by it if it disrupts the normal sleep cycles.�
During a good night�s sleep, your brain will repeatedly cycle through five phases: stages 1, 2, 3, 4, and rapid eye movement (REM) sleep. You should spend about 25% of your total slumber and this is the cycle. As researchers believe it contributes to regulating your mood, learning, and saving memories having uninterrupted REM sleep is significant.
Monitor your sleep quality, if you�ve been prescribed a medicine with sedative effects, for example an opioid. It�s not about how fast you fall asleep but also how refreshed you feel the very next day. If you dazed and �re waking up groggy, talk to your doctor about possible alterations to your medication regimen.
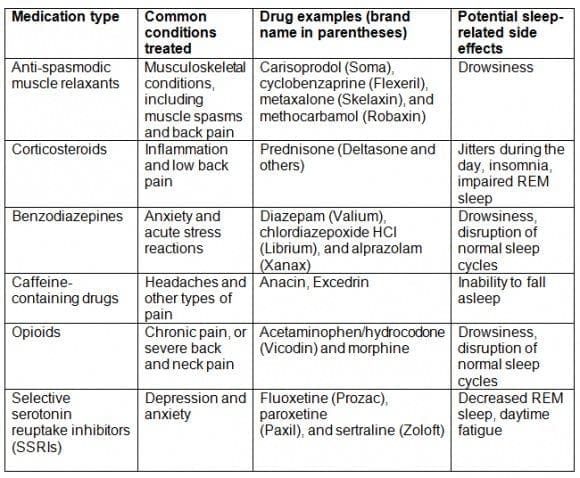
Back &�Neck Pain Medications That May Disrupt Sleep
Below are drugs that treat spinal conditions and may likewise have sleep-associated side effects.
Note: The table below features common back and neck pain medications that could interfere with your sleep and daytime functioning; it is not an all inclusive list. Always discuss the potential side effects of your medications that are certain with your physician.
Talk To Your Doctor About Drug Alternatives For Better Sleep
The quality of your slumber shouldn�t suffer�as a result, although keeping your spine healthy is vital. If you�ve detected a decrease in quality or quantity of sleep since beginning your back or neck pain medicine, tell your physician. She or he might prescribe an alternative drug or treatment while addressing your spinal issue to restore healthful sleep.

Call Today!