by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Integrative Functional Wellness, Integrative Medicine, Natural Health, Wellness
Conventional medicine is necessary to cure disease, but if you really want to stay healthy, you should incorporate treatments from the field of need to incorporate curing illness, but if you want to stay as healthy you should incorporate practices from the field known as integrative medicine as well, a top expert says.
“The field of integrative, or complementary, medicine, grew out of what used to be known as ‘alternative health,’ but the concepts we use today are based on scientific evidence,” Dr. Ashwin Mehta tells Newsmax Health.
Conventional medicine, known also as Western medicine, is a system in which medical doctors and other healthcare professionals treat symptoms and diseases using such means as drugs, radiation or surgery.
In contrast, the term “alternative medicine” describes a range of medical therapies that are not regarded as orthodox by the medical profession, such as herbalism, homeopathy, and acupuncture.
“In the 1970s, the alternative medicine gained traction in the U.S. as a pushback against the biochemical paradigm that was becoming associated with medicine,” says Mehta, medical director of integrative medicine at Memorial Healthcare System in Hollywood, Fla.
“But, on the other hand, the realization was growing that there might be something of value in these ancient healing traditions, and so we should scientifically evaluate them.”
When some alternative therapies were held up to this scrutiny, they were found to be baseless, says Mehta. On the other hand, others were found to be valuable. These have since been known as integrative, or complementary therapies, he adds.
“Integrative medicine uses only the therapies that have been found to have scientific validity,” says Mehta.
He likes to explain this concept by using an example in cancer treatment.
“If the body is a garden and cancer is an unwelcome weed, the job of the oncologists (cancer doctors) is pluck out the weed and our job is to make the soil of the garden inhospitable to the weed ever coming back,” he says.
One of the most valuable adjuncts that integrative medicine offers today’s patient is the ability of these therapies to reduce inflammation.
Inflammation is the same reddening process you see if you cut your finger. But there also is an invisible type of inflammation, known as “chronic bodily inflammation,” which occurs inside your body and cannot be seen.
Such inflammation is increasingly viewed as the culprit in the development of cardiovascular disease, diabetes, and cancer as well, notes Mehta.
“Today, we use the term ‘metabolic syndrome,” to describe a number of conditions, including high cholesterol, high blood sugars, high blood pressure and obesity, that increase the risk of cardiovascular disease, diabetes and cancer,” says Mehta.
What these conditions have in common is that they cause a “predominance of inflammation,” he adds.
To combat inflammation, follow these 5 principles of integrative medicine, he says:
Use food as medicine: Much of our medication, from aspirin to chemotherapy, has been derived from leafy plants, so it makes sense to use them in cooking. Green tea, turmeric and cinnamon have anti-inflammatory properties.
Use food to strengthen your immune system: The Mediterranean Diet is anti-inflammatory because it features a largely plant-based diet that focuses on vegetables, nuts and seeds, cold-water fish and healthy herbs and spices.
Get a good night’s sleep: During REM sleep, the body’s temperature dips slightly (about 1 ½ degrees) creating a cooling effect that helps reduce inflammation. If you have trouble sleeping, check your caffeine intake and turn of “screens,” in your room that can disrupt your melatonin levels. (Melatonin is the “sleep” hormone). This means TV’s, tables, and smart phones. Aromatherapy, the use of essential oils, can also create a restful environment.
Consider cxercise as medicine: A sedentary lifestyle impairs circulation over time, contributing to physical deconditioning that gives rise to obesity and osteoporosis and also increases the risk of high blood pressure and diabetes.
Practice meditation. A daily period of meditation has been found to strengthen the mind-body connection.
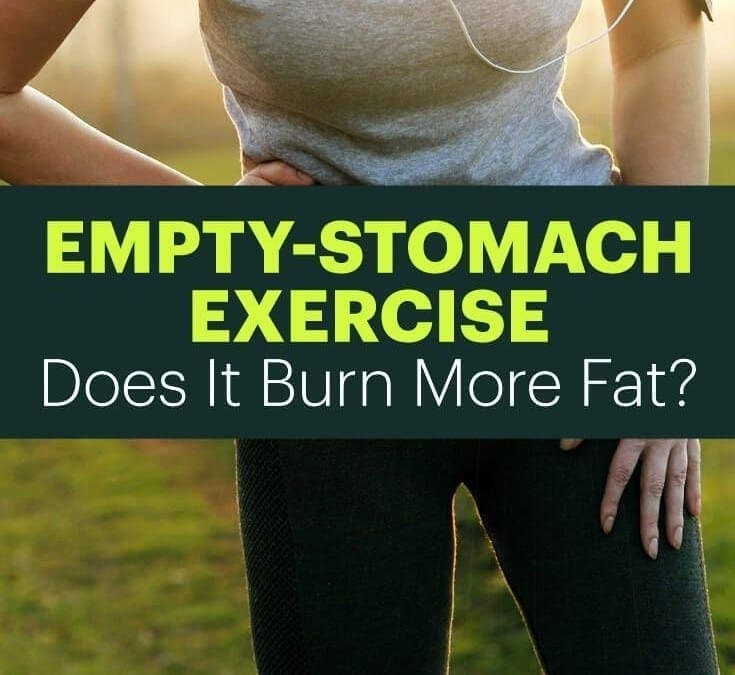
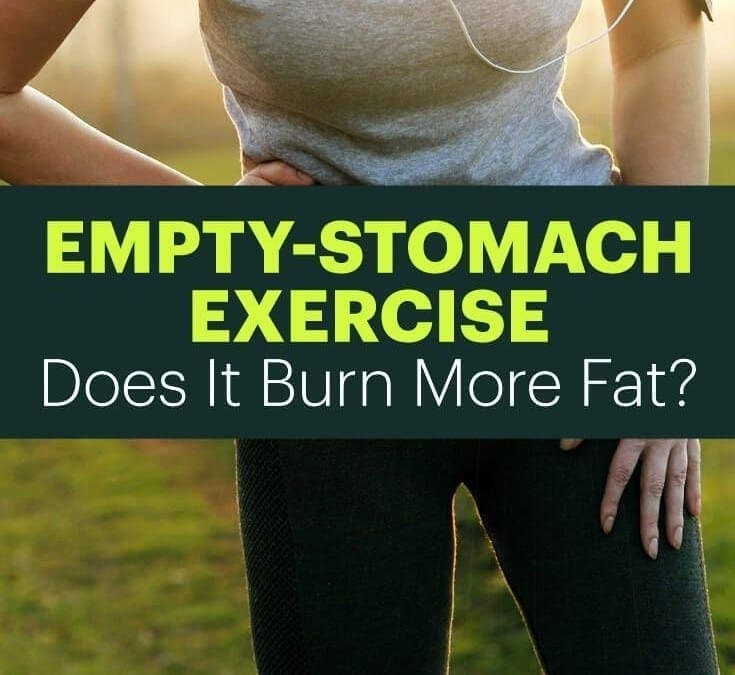
by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Fitness, Intermittent Fasting, Natural Health, Weight Loss, Wellness
El Paso, TX. Chiropractor Dr. Alex Jimenez examines working out on an empty stomach.
For a thing that should be simple, working out doesn�t consistently feel that way. There�s choosing the best fat-burning workout. There�s that pesky question of whether diet or exercise is essential for fat loss. And there�s a new one to throw into the mix: whether working out on an empty stomach can help you shed weight faster.
Bodybuilders swear by it while many people religiously enjoy their pre -workout protein shake. What exactly gives? Should you hitting the gym on an empty stomach and be forgoing food in the event you want to lose pounds?
Regrettably, like so much fitness guidance, this falls into the grey, �it depends� place. Let�s inquire.
Work Out On an Empty Stomach?
The theory behind exercising having an empty tummy is that when you squeeze before breakfast, your body burns fat faster.
See, what occurs is that glycogen, a type of carbohydrate which our bodies shop, � runs out� overnight. When you wake up and hit the gym first thing in the morning, because your body is low on carbs, the notion is the body will really turn to fats next to obtain energy. (1)
Things do get tricky because if the body is completely from glycogen � you had an early dinner, got the full nighttime�s remainder and perhaps snoozed an extra hour or two � the body might bypass fat burning and head directly to muscle shops instead, chipping away at body definition.
�
Advantages of Working Out On an Empty Stomach
So what does the science say the huge benefits before working out to missing breakfast?
1. Burn Fat Quicker. One study followed 12 active males after breakfast who ran on the treadmill either or while they were still fasting from the night time before. (2) The men who hadn�t broken their fast, i.e. hadn�t had breakfast, burned up to 20 percent more body fat during the same work outs.
What�s especially fascinating is that the guys who jumped breakfast didn�t overeat after or attempt to otherwise make � for the early AM calories up they missed out on. So obtaining a head start on your fitness regimen pre-breakfast can help you lose more fat without making you sneak in extra calories later.
2. Improve Performance. There�s evidence that exercising when your carb levels are low, like when you�re on an empty stomach, actually helps improve functionality during �normal� workouts. The concept behind �train low, compete � that is high is that working out in a glycogen- low state helps the body become more efficient at burning off fat so at times when carb levels are quite high, the body is primed and raring to go. (3)
3. Time-Restricted Eating Can Help In Losing Weight. Work Out out on an empty stomach ties into the thought of time-limited eating. On this diet program, it is possible to eat as much as you want of anything you desire. The only caveat is that you just eat strictly between certain hours, with 12�16 hours of time where you don�t eat anything.
The notion is that when our bodies understand just when we�re going to be eating, our hormones react by burning fat and supporting weight reduction during the food-free hours. Scheduling workouts during fasting hours could encourage the body to burn more fat, particularly when you�re exercising first thing in the morning.
4. Improve Body’s Response To Insulin. When we eat, our bodies release insulin to consume all of the nutrients in the foods we�re enjoying. However, as soon as we�re eating way too many carbohydrates and sugar, our bodies become resistant to insulin � it�s unable to do its job at the same time.
All that insulin can bring in regards to an assortment of chronic illnesses and builds up. Among many health benefits of fasting, however, is reducing that susceptibility to insulin. Without continuous food, insulin isn�t so our bodies don�t become immune to the hormone, created often.
5. Inspiration To Work Out More.�Let�s confront it � we�re all super active. By working out each morning before stopping to make breakfast, having that cup of coffee or whatever it’s that might derail you in the mornings, you can get your calorie burning out of the way with no distractions that happen after.
In the event you have to be out of your house by 8 a.m., it�s a lot easier to hit the gym before eating as opposed to sitting down for breakfast, waiting to digest and then working out.
When It�s Not Wise To Work Out Without Any Food On Board
But working out on an empty stomach might not be the finest idea for everybody. For each study that says burning fat occurs more easily when you exercise before eating, there�s another one that says the opposite. An International Journal of Sport Nutrition and Exercise Metabolism study found that a pre-workout snack or light meal actually helps burn body fat. (4)
Plus study found no difference in weight reduction between women who ate a meal-replacement shake before exercising without eating and those that got directly in their workouts. (5)
Another problem is that without any fuel in your belly, you may well not be working out as hard as you could. A pre-workout snack that�s a mix of carbs, protein and healthy fats can give you the energy you need to push yourself harder.
That extra fire might be just things you must finish high-intensity interval workouts like Crossfit or Tabata, which actually help you burn off more calories in a briefer amount of time. These are intense work outs where you�re likely to need to max out your energy.
And when you�re training for endurance sports like long-distance racing or a triathlon, working out on an empty stomach might work for short distances, but you definitely wish to consume before longer work outs � depending on how much you�re going, you might even need to refuel during training.
Finally, if you�re someone who psychologically has to realize which you aren�t going to burn out mid way because you�ve eaten through exercising, it�s not a great day to work out on an empty stomach. Same goes for people who are diabetic or experience low blood sugar. Eating a small bite will make sure that you remain safe throughout your workout.
Final�Thoughts
I wish I possibly could tell you that working out on an empty stomach will cause results that are better. But because numerous variables are at play � how fit you are, what type of exercise you�re doing and the way you workout best � it�s impossible.
What is vital is that you just remain hydrated before, during and following your workout. Drinking enough water will keep up energy levels. Drinking enough H2O can also keep pounds from increasing because thirst is, in addition, mistaken for hunger.
Maybe more notably than whether you eat before a workout is what you�re having later. A mix of protein and healthy carbs can help muscle tissue recover. Drinking a post-workout recovery shake or eating eggs with veggies in the first 45 minutes after exercise while your blood is circulating well is ideal. Take a look at my list of 43 greatest post-workout meals for quicker results � you�re certain to find something you�ll adore.
Eventually, whether you�re working out on an empty stomach or not, kudos to you for getting out there and taking control of your quality of life. Keep up the work outs!

Call Today!
by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chiropractic, Natural Health
El Paso, TX. Chiropractor Dr. Alex Jimenez focuses on the rise in opioid use among older adults.
SpineUniverse reported on a study that indicated a 10% increase in opioid addiction or dependency in patients prescribed such drugs to take care of postoperative pain. Although spine surgery was not among the forms of operations included in the research, it�s intriguing to see that 3% of the patients ages 55-years plus, disclosed addiction and opioid use.
Older adults as well as the elderly are part of about 100 million adults in the USA (US) affected by severe or chronic pain. Low back pain is neck pain, and among the most frequent causes of pain, followed by headache/ migraine pain. Spinal stenosis, spinal osteoarthritis, and degenerative disc disease are frequent investigations in elderly residents and our mature adult.
In a presentation by Sullivan in 2003 about chronic pain and prescription opioid abuse and dependence in mature adults, it had been reported that �the prevalence of pain increases with each decade of life Additionally, 80% were grown by pain criticisms in adults age 65 and older. Moreover, as the number of opioid prescriptions increased, so did use by older adults�but some medical studies regularly blown off addiction as temporary or rather rare.
Regulators React
Acknowledge and its particular bureaus and the government started to recognize opioid use and the potential risks in elderly Americans. In 2012, a study revealed that more than 700,000 adults (ages 45 to 84) were hospitalized particularly for opioid abuse. Mature adults as well as the elderly accounted for a five-time increase in hospitalizations for opioid abuse compared to younger Americans.
Adults of any age taking an opioid may experience drug unwanted effects that are possibly dangerous. But for mature adults or senior -aged individuals, the hazards are weightier. Why? Old people frequently take several medications simultaneously to treat different medical problems (eg, diabetes, hypertension). It may be a challenge for the patient to keep an eye on when to take a drug that is prescribed or remember if the medicine was taken, which may result in unintentional doses. An opioid drops, and introduces another tier of potential risks, including respiratory depression, lack of balance, confusion, dizziness, drowsiness, nausea.
In 2015, Congress introduced a Medicare-specific bill called �Ceasing Drug Exploitation and Shielding Seniors Act.� Now, we see changes dispensed, and monitored to prevent physician- shopping and other ways drugs could possibly be obtained and abused.

Managing Opioid Medications
Elderly patients or some adult live alone, in a household setting, receive home-health support, or reside in a assisted-living facility or alternative scenario. In some cases, the direction of the medication, including pain-relieving drug is managed by healthcare or nursing staff.
Many older adults and aged patients are quite capable of handling physician�s visits, their drugs, and everyday life. Then there are other people who want support. They might not realize they need help or may not ask. This is where friend, a family member or caregiver might help by being observant and step in to help. By way of example, does the patient take their medication as prescribed, but nevertheless look to be in pain? Does he /she stumble easily or fall, complain about feeling dizzy, confused, constipated, or have a few other criticisms?
Remember that people so do their needs for drugs and change with age. In unwanted effects and handling pain, the alternative can be an alternate kind of drug or a dose change. Considering many senior adults and aged men take multiple medications, it’s an excellent idea to bring OTC medication all prescription and nutritional supplements to each physician�s visit for review. This creates a superb chance for you and the individual to talk together with the doctor about new challenges and health changes.

Call Today!

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Natural Health, Wellness
Pregnant women should get their blood pressure checked at each prenatal visit to screen for preeclampsia, a potentially fatal complication that can damage the kidneys, liver, eyes and brain, new U.S. guidelines say.
While many doctors already monitor blood pressure throughout pregnancy, the U.S. Preventive Services Task Force (USPSTF) updated its guidelines for the first time since 1996 to stress that screening at every visit can help doctors catch and treat preeclampsia before it escalates from a mild problem to a life-threatening one.
“Preeclampsia is one of the most serious health problems affecting pregnant women,” task force member Dr. Maureen Phipps, a women’s health researcher at Brown University in Providence, Rhode Island, said by email.
“Because this condition is common and critical, the Task Force offers two separate recommendations to help women lower the risk associated with preeclampsia – screening for preeclampsia is recommended for all pregnant women, and women at high risk of developing the condition can take low-dose aspirin to help prevent it,” Phipps added by email.
The screening recommendations, published on Tuesday in JAMA, apply to women without a history of preeclampsia or high blood pressure. Separate guidelines advise low-dose aspirin after the first 12 weeks of pregnancy for women with a history of elevated blood pressure. (http://bit.ly/2oIwP5B)
Preeclampsia can progress quickly, and typically develops after 20 weeks of pregnancy. Blood pressure screening earlier in pregnancy can show normal results for women who go on to develop preeclampsia.
In addition to elevated blood pressure, women with preeclampsia may also have excess amounts of protein in their urine, as well as swelling in the feet, legs and hands.
Women may suffer from stroke, seizures, organ failure and in rare cases, death. For babies, complications include slower growth inside the uterus, low birth weight and death.
Risks for preeclampsia include a history of obesity, diabetes, kidney disease, lupus or rheumatoid arthritis, as well as a mother or sister who has experienced the condition.
Because the risks of preeclampsia increase with age, women may be able to lower their chances of developing this complication by having babies sooner, said Dr. Dana Gossett, an obstetrics and gynecology researcher at the University of California, San Francisco, and co-author of an accompanying editorial in JAMA.
“Beyond that, it is also important to ensure that all health problems are well managed prior to pregnancy,” Gossett said by email. “High blood pressure should be under good control, other diseases like kidney disease or lupus should be well controlled, and women should try to be close to their ideal body weight prior to conception.”
Checking blood pressure at every prenatal visit can help prevent complications for mothers and babies alike, said Dr. Martha Gulati, chief of cardiology at the University of Arizona College of Medicine in Phoenix and author of a separate editorial in JAMA Cardiology.
“This is something that should be provided to every woman as part of preventive care,” Gulati said by email. “We will save lives and prevent complications and death in pregnant women with this simple, cost-effective” test that doesn’t take much time.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Chiropractic, Lower Back Pain, Natural Health
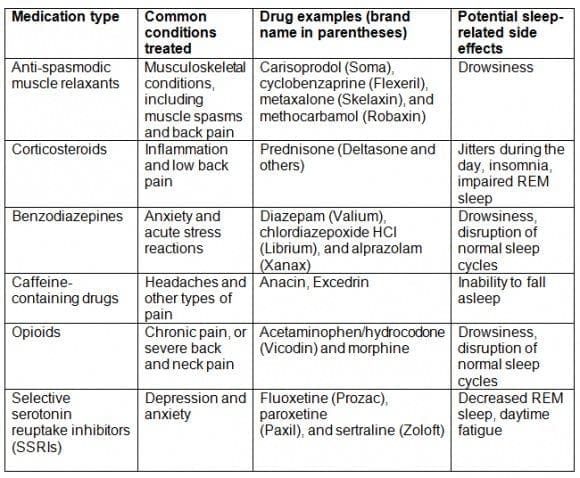
El Paso, TX. Chiropractor Dr. Alex Jimenez looks at back pain medications and their effect on sleep.
Can you relieve spine pain and get a good night�s rest? Sure some drugs get in the way.
Prescription medications are among the most recommended nonsurgical treatments for back and neck pain. While these drugs might help alleviate what ails your back, your sleep may suffer because of this. That�s a big deal, as sleep deprivation hurts your general wellbeing.
Unfortunately, back and neck pain medications can have side effects�and interfering with your sleep and ability to operate normally throughout the day are ones that are typical. Your medication may stop you from getting enough sleep or falling asleep. Or, your slumber quality suffers, although you might doze off readily. Plus, sleep-related side effects do n�t just affect you during the nighttime hours, as you may experience drowsiness or jitters during the day.
Sleep Science 101: Reconsidering Sedatives
Before delving into common back and neck pain drugs that may affect your slumber, it�s important to comprehend one of the biggest misconceptions about sleep medicines: the effect of sedation.
Many view sedatives as sleep aids due to the fact that they enable you to fall asleep fast. Nevertheless, this doesn�t tell the entire image, based on Steven A. King, MD, MS, who practices pain medicine in New York and is a clinical professor of Psychiatry at the New York University School of Medicine.
�When contemplating what�s good for sleep, it really is vital to not forget that sleep is just not a uniform activity through the entire span of the night, but rather, a succession of cycles involving different levels of wakefulness,� wrote Dr. King in a site for Psychiatric Times. �Merely because a medication may put one to sleep doesn�t mean restful slumber will be provided by it if it disrupts the normal sleep cycles.�
During a good night�s sleep, your brain will repeatedly cycle through five phases: stages 1, 2, 3, 4, and rapid eye movement (REM) sleep. You should spend about 25% of your total slumber and this is the cycle. As researchers believe it contributes to regulating your mood, learning, and saving memories having uninterrupted REM sleep is significant.
Monitor your sleep quality, if you�ve been prescribed a medicine with sedative effects, for example an opioid. It�s not about how fast you fall asleep but also how refreshed you feel the very next day. If you dazed and �re waking up groggy, talk to your doctor about possible alterations to your medication regimen.
Back &�Neck Pain Medications That May Disrupt Sleep
Below are drugs that treat spinal conditions and may likewise have sleep-associated side effects.
Note: The table below features common back and neck pain medications that could interfere with your sleep and daytime functioning; it is not an all inclusive list. Always discuss the potential side effects of your medications that are certain with your physician.
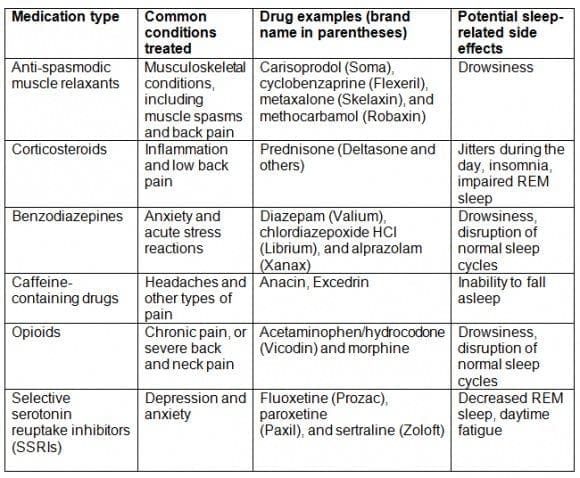
Talk To Your Doctor About Drug Alternatives For Better Sleep
The quality of your slumber shouldn�t suffer�as a result, although keeping your spine healthy is vital. If you�ve detected a decrease in quality or quantity of sleep since beginning your back or neck pain medicine, tell your physician. She or he might prescribe an alternative drug or treatment while addressing your spinal issue to restore healthful sleep.

Call Today!

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Natural Health, Wellness
Your tendency to indulge in chocolate, go heavy on salt, or eat veggies may be tied to certain gene variants, a new study suggests.
The study, of more than 800 adults, found links between several genes and people’s food likes and dislikes.
The gene variants were already known. One, for example, is linked to obesity risk; others are involved in hormone regulation.
It’s not yet clear what the new findings mean, the researchers said.
And they stressed that aversion to broccoli is not genetically determined: You might just need a better way of cooking it.
But the findings add to evidence that food preferences are partly related to genetic variation.
“Research is really beginning to look at the role of genes in food intake and nutrient use,” said Lauri Wright, a registered dietitian in Florida who was not involved in the study.
Some researchers believe that understanding the genetics behind food preferences will lead to more individualized diet advice. In fact, there’s a burgeoning field known as “nutrigenomics,” Wright noted.
For now, though, you are unlikely to have your DNA analyzed when you see a dietitian.
Nor do you need to, added Wright. She said dietitians already ask people about their food preferences — and a slew of other information — to help craft personalized diet plans.
Wright is a spokesperson for the Academy of Nutrition and Dietetics, and director of the doctorate in clinical nutrition program at the University of North Florida.
Past studies have found correlations between gene variations and people’s tastes for certain foods.
For the most part, they have looked at genes related to taste receptors, said Silvia Berciano, who led the current study.
Berciano said her team focused on certain genes that have been connected to behavioral and psychological traits (such as depression or addiction), to see if any are also related to eating habits.
To do that, the researchers analyzed variations in those genes, along with self-reported diet habits, among 818 white U.S. adults.
In general, the study found, there were associations between several genes and food preferences. Variations in a gene called FTO, which is related to obesity, were tied to vegetable and fiber consumption, for instance.
It’s possible that the FTO gene influences both obesity risk and people’s desire for veggies, said Berciano, a researcher at Tufts University in Boston.
Could the link exist simply because people prone to obesity are less likely to be vegetable lovers? Berciano said that’s unlikely: The FTO variation tied to vegetable/fiber intake is in a different place on the gene than the variant related to obesity.
In other findings, a gene called SLC6A2, which helps regulate hormones like norepinephrine, was related to fat intake.
Meanwhile, variations in a gene that helps regulate oxytocin — the so-called “love hormone” involved in bonding, mood and other behaviors — were related to chocolate intake, as well as heavier weight.
Oxytocin “enhances the brain’s reward system,” Berciano noted. On the other hand, she said, lower oxytocin levels could boost chocolate cravings as a way to get that same reward.
Berciano was scheduled to present the findings Sunday at the American Society for Nutrition’s annual meeting, in Chicago. The results should be considered preliminary until published in a peer-reviewed medical journal.
The study does not prove that any of those gene variants directly affect people’s food preferences, Wright pointed out.
And even if they have an influence, she said, diet habits are much more than a matter of genes. Economics, culture and a range of environmental factors are at play, she added.
And, with help, people can change even long-standing diet habits. “We don’t want people to think, ‘I can’t help bingeing on chocolate, it’s in my genes,’ ” Wright said.
Still, Berciano said an understanding of the genetics behind food preferences could eventually prove useful in the real world.
“Understanding how genetic differences affect neural regulation of eating behavior means that we’ll be able to predict the behavioral tendencies of the individual,” she said.
That, she added, could help in creating diet plans that are “easier for the individual to adhere to.”
For now, though, Wright said she is unsure how expensive genetic testing would enhance what dietitians already do. “We already look at the individual — not just their food preferences, but their other lifestyle habits and their economic and social situations,” she said.
That bigger context, Wright said, is critical in helping people make lasting diet changes.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Natural Health, Wellness
A new UK study has highlighted the importance of friendships in helping people get through the more stressful periods of life.
Carried out by Dr Rebecca Graber from the University of Brighton during her time at the University of Leeds, the preliminary study is the first to provide long-term statistical evidence on the huge benefit of friends, and in particular best friends, on coping with and developing resilience to stress.
The study included 185 adults, with 75 completing the study’s questionnaires and assessments on psychological resilience, best friendship quality, coping behaviors and self-esteem.
Participants then completed the same assessments again one year later, to see how the quality of best friend relationships had affected resilience to stress during this period.
The results showed that best friendships had a protective effect against stress, helping to develop psychological resilience in adults, although how still remains unclear.
The findings also support research published last year by Dr Graber, which found that best friendships can help develop resilience to stress in socioeconomically vulnerable children.