
Chiropractic Treatment for Migraine Pain in El Paso, TX
Migraine headache pain can be characterized as a throbbing pain or a pulsing sensation of varying intensity, which is generally accompanied by nausea as well as extreme sensitivity to light and sound. According to the American Migraine Association, migraines affect about 36 million Americans, or approximately 12 percent of the population in the United States. Because the symptoms can often become very debilitating, many migraine sufferers will have tried everything to attempt to relieve their headache pain, including avoiding triggers and using drugs and/or medications to reduce the symptoms. However, research studies have found that one alternative treatment option can greatly benefit migraineurs: chiropractic care.
Chiropractor Treating Migraine Pain
Chiropractic care is a safe and effective alternative treatment option which focuses on the diagnosis, treatment and prevention of a variety of injuries and/or conditions associated with the musculoskeletal and nervous system. A doctor of chiropractic, or chiropractor, will commonly utilize a series of chiropractic methods and techniques, including spinal adjustments and manual manipulations, to carefully correct any spinal misalignment, or subluxation, located along the length of the spine. Although the true source of migraines is still misunderstood today, healthcare professionals believe that a misalignment of the cervical spine, or neck, may trigger migraine symptoms. By correcting the alignment of the spine, a chiropractor can release the pressure being placed against the spinal column which may be irritating and/or compressing the complex structures surrounding the spine, manifesting the well-known symptoms of migraines. Furthermore, chiropractic care can decrease muscle tension and increase circulation, eliminating stress in the body which is also known to be a factor behind migraines, promoting further relief.


The Efficacy of Chiropractic Spinal Manipulative Therapy (SMT) in the Treatment of Migraine
Abstract
- Objective: To test the efficacy of Chiropractic spinal manipulative therapy (SMT) in the treatment of migraine, using an uncontrolled clinical trial.
- Design: A clinical trial of six months duration. The trial consisted of 3 stages: two months of pre-treatment, two months of treatment, and two months post treatment. Comparison was made to initial baseline episodes of migraine preceding commencement of SMT.
- Setting: Chiropractic Research Centre of Macquarie University
- Participants: Thirty two volunteers, between the ages of 23 to 60 were recruited through media advertising. The diagnosis of migraine based on a detailed questionnaire, regarding self reported symptoms or signs, with minimum of one migraine with aura per month.
- Interventions: Two months of SMT provided by an experienced chiropractor at a university clinic.
- Main Outcome Measures: Participants completed diaries during the entire trial noting the frequency, intensity, duration, disability, associated symptoms and use of medication for each migraine episode. In addition, clinic records were compared to their diary entries of migraine episodes.
- Results: A total of fifty nine participants responded to the advertising, with twenty five being excluded or deciding not to continue in the trial. Two participants (5.9%) withdrew during the trial, one due to alteration in work situation and one following soreness after SMT. The Chiropractic SMT group showed statistically significant improvement (p < 0.05) in migraine frequency and duration, when compared to initial baseline levels. Only one participant (3.1%) reported that the migraine episodes were worse after the two months of SMT, and this was not sustained at the two month post treatment follow up period.
- Conclusion: The results of this study suggest that Chiropractic SMT is an effective treatment for migraine with aura. However, due to the cyclical nature of migraine with aura, and the finding that episodes usually reduce following any intervention, further research is required. A prospective randomised controlled trial utilising detuned EPT (interferential), a sham manipulation group and an SMT group is nearing conclusion. It is anticipated this trial will provide further information of the efficacy of Chiropractic SMT in the treatment of migraine with aura.
- Key Indexing Terms (MeSH): Migraine, chiropractic, spinal manipulation, clinical trial.
Dr. Alex Jimenez’s Insight
According to the American Chiropractic Association, a 2011 report published in the Journal of Manipulative and Physiological Therapeutics, or JMPT, found that chiropractic care, including spinal adjustments and manual manipulations, can improve migraine and cervicogenic headache symptoms. Healthcare professionals have associated primary headaches with stress and muscle tension. Chiropractic care can help decrease the frequency of migraines and manage its symptoms by carefully correcting any spinal misalignment, or subluxation, found along the spine. By restoring the proper alignment of the spine, chiropractic care can improve overall spinal function by alleviating pressure on the nervous system, increasing circulation and reducing muscle tension and stress which causes migraine pain.
Introduction
Some studies appear to have demonstrated significant reduction in migraines following chiropractic intervention (1-8). However, this reduction may in part have been due to inaccurate diagnosis or overlapping symptoms (4,9,10). Many different conditions of the cervical spine, including mechanical and joint pathology, have been reported to cause headache (10-16). Sjaastad (17) used the term �cervicogenic headache� to describe a type of the chronic paroxysmal unilateral headache, which is accompanied by autonomic symptoms and provacated by movements of the head and neck. Sjaastad proposed that entrapment of the occipital nerve or a C2-C3 rhizopathy may produce this headache (18).
There are a number of aetiologies of migraines proposed in the literature. These include: vascular (19-21); autonomic (22); biochemical/cellular/immunological (23- 27); psychophysiological (28,29); neurogenic (9,15,25,30) and somatic (1-9,31,32). This has made a common treatment regime difficult. One early medical model was vascular cause of migraine, where a migrainous attack is initiated by a decreased blood flow to the cerebral vasculature or a cerebrovascular spasm, but characterized by extracranial vasodilation during the headache phase (19,20). However, later aetiological models have demonstrated more complex vascular changes with associated neurological changes (9).
Many practitioners involved in the treatment of migraine would, however, accept that a number of aetiological factors are involved and that there is substantial overlap in both aetiology or diagnosis (9,15,26,33,34). In addition, no single model appears to explain all the possible symptoms associated with migraine.
One possible aetiological factor is cervical spondylosis with associated neck pain and stiffness (34). Anthony states �when this is recognised, appropriate treatment can give impressive results…the aim is to relieve pressure on nerve roots in the upper neck thereby reducing activation of the spinal tract of the trigeminal nerve, which is part of the pain centre in the head and neck� (34). Surgical decompression of the lower cervical nerve�roots as carried out by Ghavamian (36) showed relief of migraine symptoms. He proposed that irritation and compression of the deep sympathetic fibres incited such symptomatology.
Vernon (7), proposed a vertebrogenic model which involves components from the different categories previously stated. One part involves lesions in the low cervical/upper thoracic spine and the upper cervical spine. The low cervical spine/upper thoracic spine (C7-T4) model proposed that dysfunction (i.e. somatic dysfunction) at these vertebral levels causes joint fixation and pain. This pain alters the neural messages received, and therefore sent, by the Central Nervous System (CNS). The Autonomic Nervous System which controls, amongst other functions, blood supply, is thus also affected. It is proposed that when certain threshold levels of transient cerebral ischaemia (due to vasoconstriction caused by the above mechanism) are reached, a migraine cascade of symptomatology may be precipitated.
A second part involves somatic dysfunction in the upper cervical spine (Occiput-C2), which produces local pain and fixation leading to increased neural input to the CNS. This results in a reduction in descending pain-inhibiting impulses from the CNS and consequently increases activity within the spinal trigeminal tract (which transmits the majority of sensory afferents and pain signals from the upper cervical region to the brain). Having exceeded a threshold level, this excessive afferent input to the CNS will trigger focal, and spreading vasoconstriction within the intracerebral vasculature. This will in turn promote extra-carotid vasodilation and cranial pain which is mediated by the ipsilateral trigeminal nerve (7).
Another model contends that irritation of the vertebral nerve by cervical lesions can produce a sympathetic syndrome, giving symptoms of headache, vertigo, visual disturbances and tinnitus. However, this model has not been well substantiated and appears more likely a cause of vascular headache as opposed to migraine (11). The source of pain in migraines is found in the intra- and extracranial blood vessels. The blood vessel walls are pain sensitive to distension, traction or displacement. The idiopathic dilation of cranial blood vessels, together with an increase in a pain threshold lowering substance, result in headache of migraine type (26).
Migraine has a well established symptomatology that has been outlined in various studies (4,12,15). The debilitating and frequent nature of symptoms that include head pain, nausea, vomiting, phonophobia, and photophobia, costs our society both socially and economically (4,12,15,20). As such, effective treatment has long been sought, therefore justifying study in this area. However, there is substantial overlap of symptoms between migraine and cervicogenic�headache, and some authors believe elements of the migraine headache continuum involve cervical headache (9,10).
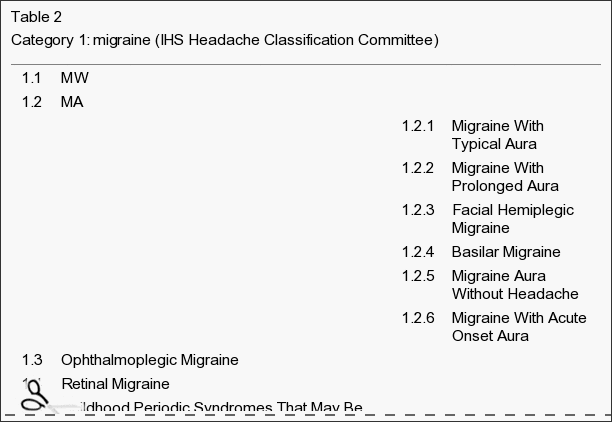
The Headache Classification Committee of the International Headaches Society, has discarded the former terms classical migraine and common migraine in favour of migraine with aura and migraine without aura. In migraine with aura (MA), this condition is defined as recurrent, periodic, unilateral headache which is preceded or accompanied by transient visual, sensory, motor, or other focal neurological symptoms which localise to the cerebral cortex or brainstem. Migraine without aura, (MWA) is defined as a vascular headache without striking prodromal or associated symptoms of cerebral dysfunction (37).
The incidence of migraine in Australia is estimated at 12%, with the cost to industry an estimated $250 million (38). In the USA approximately 8% of headaches diagnosed by medical practitioners are called migraine headaches (39). Migraine, in its various forms, affects an estimated 5-20% of people throughout the world (40).
A review of the literature appears to indicate that migraine is an associated feature of cervical dysfunction. This paper will evaluate chiropractic spinal manipulative treatment directed towards improving vertebral function, and its role in the management of the migraines.
Methodology
Chiropractic spinal manipulative therapy (SMT) is defined as a passive manual manoeuvre during which the three joint complex is carried beyond the normal physiological range of movement without exceeding the boundaries of anatomical integrity (41). SMT requires a dynamic force in a specific direction, usually with a short amplitude, to correct a problem of reduced vertebral motion or positional fault.
The study design was based on a previous study which involved 82 subjects who received either chiropractic SMT, physiotherapy manipulation, or a control treatment of medical mobilization (1). Parker et al, concluded that manipulation was not found to be more effective than mobilisation, and chiropractic treatment not more effective than the other two groups (3). However, much criticism was received over the study, especially the statistical analysis (42).
People with migraines were advertised for participation in the study via the radio and newspapers within a local region of Sydney. All applicants completed a questionnaire, developed from Vernon (12), which contains over 25 sections, including details of the initial�history, frequency, severity, location and reaction to the pain, associated symptoms, precipitating or aggravating factors, relieving factors, past treatment for migraines, medical history including medications and other diagnostic tests.
The participants to take part in the trial were selected according to responses in the questionnaire of specific symptoms. The criteria for migraine diagnosis was compliance with at least 5 out of the following indicators: reaction to pain requiring cessation of activities or the need to seek a quiet dark area; pain located around the temples; pain described as throbbing; associated symptoms of nausea, vomiting, aura, photophobia or phonophobia; migraine precipitated by weather changes; migraine aggravated by head or neck movements; previous diagnosis of migraine by a specialist; and a family history of migraine.
Participants also had to experience migraine at least once a month, but not daily, and the migraines could not have been initiated by trauma. Participants were excluded from the study if there were contra-indications to SMT, such as meningitis or cerebral aneurysm. In addition, participants with temporal arteritis, benign intracranial hypertension or space occupying lesions, were also excluded due to safety aspects.
Participants were informed that they were involved in a trial of manipulative therapy for migraine, and that they may be randomly assigned to a control group which would receive a placebo (non effective) treatment, or to an intervention group which would receive Chiropractic SMT. However, because of the small numbers of participants that were involved in the trial, a control group was not used. Participants were also informed that a thorough physical examination would be performed prior to commencement of treatment to assess any physical problems precluding them receiving SMT. Patients were blinded, by believing that they may or may not receive an effective treatment. In addition, practitioners were not aware of ongoing treatment results, therefore they were also �blinded� to the stage of progress of the patients condition or response to treatment.
The trial was conducted over six months, and consisted of 3 stages: two months pretreatment, two months treatment, and two months post treatment. Participants completed diaries during the entire trial noting the frequency, intensity, duration, disability, associated symptoms and use of medication for each migraine episode. In addition, clinic records were compared to their diary entries of migraine episodes. Concurrently, the subjects were contacted by telephone by the author every month and asked to describe the migraine episodes for comparison to their diaries.
Patients were instructed at the beginning of the study on the use of the diary and were given an instruction sheet to use throughout the course of the trial. The diary consisted of a table for entries of each of the outcome measures. This included noting the date of each episode, a number representing a visual analogue score, letters denoting associated symptoms, the length (in hours) of each migraine, the time (in hours) before the person could return to normal duties, type and use of medications and the overall relief from the medication. The diaries were modified from standard diaries used by the Brain Foundation of Australia.
A detailed history of the patient’s subjective pain features was taken during the initial consultation. This included the type of pain, duration, onset, severity, radiation, aggravating and relieving factors. The history also included medical features, a systems review for potential pathologies, previous treatments and its effects.
Factors for assessing subluxation included: orthopaedic and neurological testing, segmental springing, mobility measures such as visual estimation of range of motion, assessment of previous radiographs, specific chiropractic vertebral testing procedures, as well as response of the patient to SMT.
In addition, several vascular investigations were performed where indicated, which included: vertebral artery test, manipulative provocation test, blood pressure assessment, and abdominal aortic aneurysm screening.
During the treatment period, the subjects continued to record migraine episodes in their diary, and receive telephone calls from the authors. Treatment consisted of short amplitude, high velocity spinal manipulative thrusts, or areas of fixation determined by the physical examination. Patients were allowed a maximum of sixteen treatments, and the frequency of treatment was dependent on the clinicians opinion of the severity of the vertebral dysfunction. The majority of patients received a minimum of twelve treatments.
Comparison was made to initial baseline episodes of migraine preceding commencement of SMT. Statistical analysis involved comparing the effects of the different treatment regimes on the incidence, intensity, and duration of migraines throughout the trial. Statistical tests employed were a students t test to test for significant difference between each group and a one way analysis of variance (ANOVA) to test for changes for all groups. Statistical calculations were performed via a computer software program Minitab for Macintosh.
Results
A total of fifty nine participants responded to the�advertising, with twenty five being excluded or deciding not to continue in the trial. These included: six cases of infrequent recurrence of the migraines (less than one per month); two cases of contraindications to SMT; one case of cluster headache; one case of motor vehicle accident during pre treatment; one case of fear of SMT; fourteen cases where the university clinic was inconvenient or time constraints were too difficult for participants. Two participants (5.9%) withdrew during the trial, one due to alteration in work situation and one following soreness after SMT.
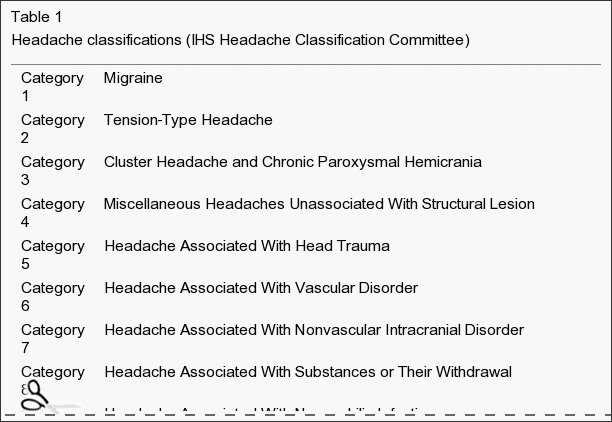
Thirty two participants, between the ages of 23 to 60, joined the study with there being 14 males and 18 females. Table 1 gives the comparative descriptive statistics for the group.
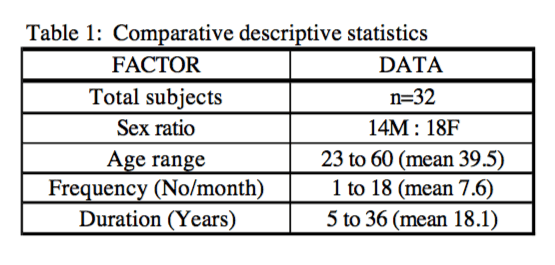
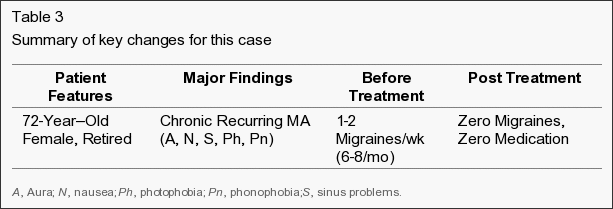
The Chiropractic SMT group showed statistically significant improvement (p < 0.05) in migraine severity (Figure 1), duration (Figure 2) and disability (Figure 3), when compared to initial baseline levels. Only one participant (3.1%) reported that their migraine episodes were worse after the two months of SMT, but this was not sustained at the two month post treatment follow up period. Table 2 demonstrates variate scores in each of the six diary categories for the three phases of the trial.
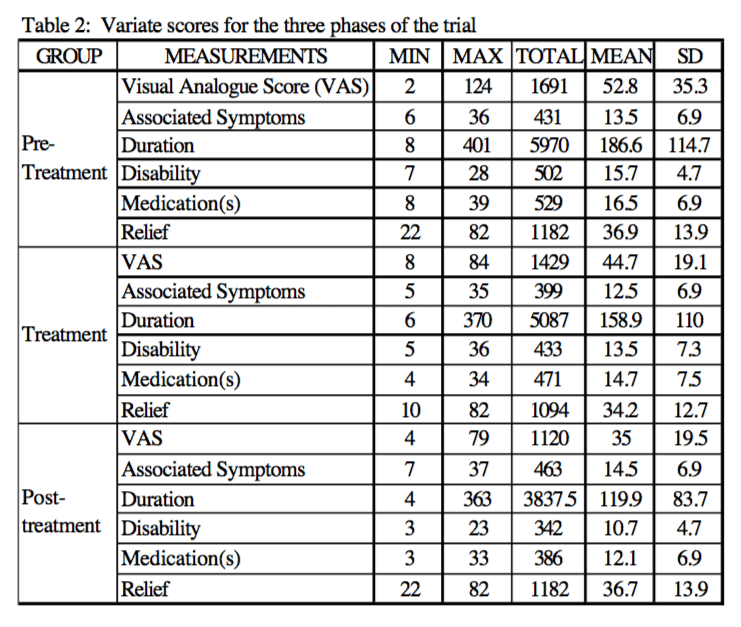
The greatest area for improvement was with disability scores (p < 0.01), where participants were asked to rate the time that elapsed before they could return to normal activities (Table 3). In addition, the duration of the migraine and the use of medication, reduced significantly following the SMT intervention (p < 0.05). Table 3 shows mean variate scores for the three phases of the trial�and statistical significance by analysis of variance (ANOVA).
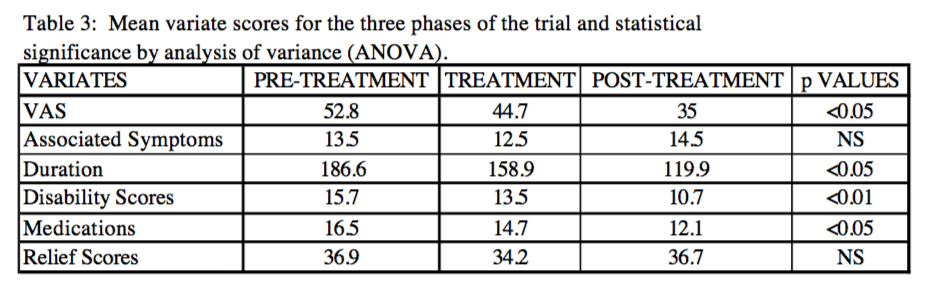
There was no apparent difference in the number of associated symptoms and the time taken for treatment to give relief of each migraine episode (Table 3). In addition, self reported possible trigger factors demonstrated no significant findings, predominantly due to the small sample size. Common trigger factors that were cited included stress, lack of sleep, work changes, or family situations. Most participants could not state a particular trigger factor.
Discussion
The majority of people who participated in this trial had chronic migraines that were severe and debilitating. However, the results have demonstrated a significant (p< 0.05) reduction in their�migraine episodes and their associated disability. The mean number of migraine per month reduced from 7.6 to 4.9 episodes.
This trial was conducted using a similar design to a previous study which demonstrated significant improvement in migraines following chiropractic SMT (1,3). The initial trial had limitations due to an inadequate control group, and this could also be a limitation with this study(2). However, the use of self reported, non treatment period as a control, allows flexibility regarding use of medication and any alteration during the trial.
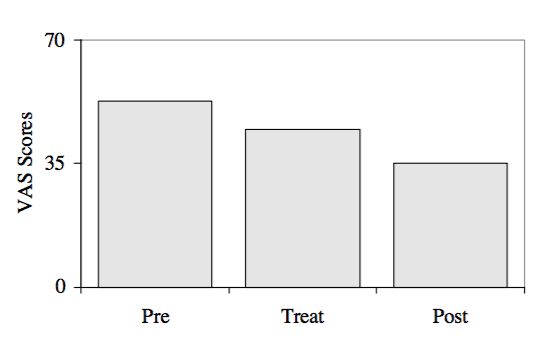
Figure 1: Comparison of visual analogue scores for pre-treatment, treatment and post-treatment group means.
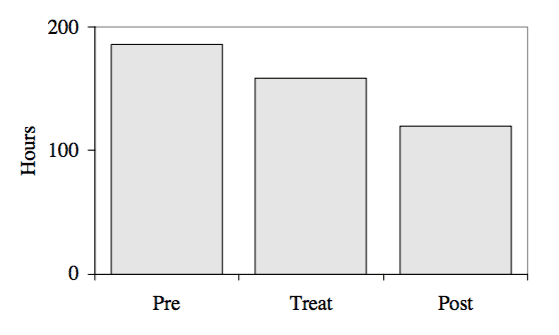
Figure 2: Comparison of duration time of migraine (hours) for pre-treatment, treatment and post-treatment group means.
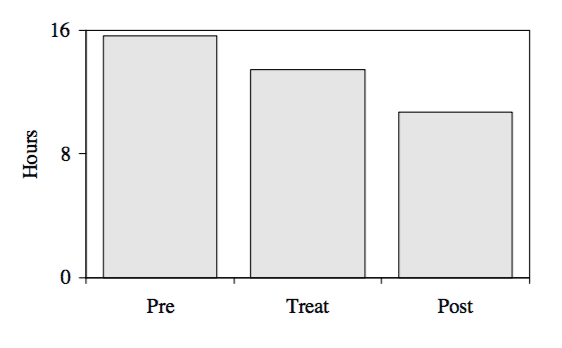
Figure 3: Comparison of disability time of migraine (hours) for pre-treatment, treatment and post-treatment group means.
A similar design to this study has also been used in a study of headache and SMT (14). The Boline study was a randomised controlled trial using two parallel groups, with a two week baseline, a six week treatment period and a four week post treatment period. The results of this study show that SMT was an effective method of treatment for tension type headaches, and that the benefit was sustained for the four weeks after cessation of the treatment.
The present study was conducted over a six month period which gives the results substantial significance because early criticisms of studies were that the length of the trial was too short to allow for the cyclical nature of migraines. However, the study is limited in the sample size and the fact that the trial was a pragmatic study which did not consider what aspects of chiropractic SMT had contributed to the improvement in the migraine episodes.
In addition, the study is limited due to the lack of a control group. However, the fact that the trial was conducted over a six month period, with two months pre-treatment, it could be argued that participants acted as their own form of control.
A further limitation of this study, as with other studies of migraine or headaches is that there is substantial overlap in diagnosis and classification of migraines. The questionnaire used in this study proved to have good reliability, however, there is strong suggestion that many headache sufferers may have more than one type of headache (12). An advantage with the design of this study is that regardless of the exact �diagnosis� of the migraine, self reported, non-treatment controls still allow assessment of the therapy in question.
The measurement used for relief scores proved to be poor, which was probably due in part to the small scale for response that participants were given. Future studies should address this issue. In addition, associated symptoms did not give a clear result because the study only measured the total number of associated symptoms, and the sample size was too small for a significant percentage breakdown. Future studies should also address this issue.
Conclusion
The results of this study suggest that Chiropractic SMT may be an effective treatment for migraine. However, due to the cyclical nature of migraine, and the finding that episodes usually reduce following any intervention, further research is required. A prospective randomised controlled trial utilising detuned EPT (interferential), a sham manipulation group and an SMT group is nearing�conclusion. It is anticipated this trial will provide further information of the efficacy of Chiropractic SMT in the treatment of migraine.
In conclusion,�chiropractic care is a safe and effective alternative treatment option which can be used to improve migraine symptoms as well as decrease their frequency. A chiropractor will utilize spinal adjustments and manual manipulations to correct spinal misalignments, or subluxations, releasing pressure being placed against the complex structures surrounding the spine, decreasing muscle tension and improving circulation to eliminate stress, ultimately benefitting migraine sufferers. Finally, the purpose of the article above was to demonstrate the efficacy of chiropractic spinal manipulative therapy, or SMT, in the treatment of migraine. Information referenced from the National Center for Biotechnology Information (NCBI). The scope of our information is limited to chiropractic as well as to spinal injuries and conditions. To discuss the subject matter, please feel free to ask Dr. Jimenez or contact us at 915-850-0900 .
Curated by Dr. Alex Jimenez
Additional Topics: Back Pain
According to statistics, approximately 80% of people will experience symptoms of back pain at least once throughout their lifetimes. Back pain is a common complaint which can result due to a variety of injuries and/or conditions. Often times, the natural degeneration of the spine with age can cause back pain. Herniated discs occur when the soft, gel-like center of an intervertebral disc pushes through a tear in its surrounding, outer ring of cartilage, compressing and irritating the nerve roots. Disc herniations most commonly occur along the lower back, or lumbar spine, but they may also occur along the cervical spine, or neck. The impingement of the nerves found in the low back due to injury and/or an aggravated condition can lead to symptoms of sciatica.

EXTRA IMPORTANT TOPIC:�Neck Pain Treatment El Paso, TX Chiropractor
MORE TOPICS: EXTRA EXTRA: El Paso, Tx | Athletes
Blank
References
1. Parker GB, Tupling H, Pryor DS. A controlled trial of cervical manipulation for migraine. Aust NZ J Med 1978; 8: 585-93.
2. Parker GB, Tupling H, Pryor DS. Letters to the editor: cervical manipulation for migraine. Aust NZ J Med 1979; 9: 341-2.
3. Parker GB, Tupling H, Pryor DS. Why does migraine improve during a clinical trial? Further results from a trial of cervical manipulation for migraine. Aust NZ J Med 1980; 10: 192-8.
4. Tuchin PJ, Bonello R. Classic migraine or not classic migraine, that is the question. Aust Chiro & Osteo 1996; 5: 66-74.
5. Whittingham W, Ellis WS, Molyneux TP. The effect of manipulation (Toggle recoil technique) for headaches with upper cervical joint dysfunction: a case study. J Manipulative Physiol Ther 1994; 17(6): 369-75.
6. Wight JS. Migraine: a statistical analysis of chiropractic treatment. J Am Chiro Assoc 1978; 12: 363-7.
7. Vernon H, Steiman I, Hagino C. Cervicogenic dysfunction in muscle contraction headache and migraine: a descriptive study. J Manipulative Physiol Ther 1992; 15: 418-29
8. Lenhart LJ. Chiropractic management of migraine without aura: a case study. JNMS 1995; 3: 20-6.
9. Nelson CF. The tension headache, migraine continuum: a hypothesis. J Manipulative Physiol Ther 1994; 17(3): 157-67.
10. Jull GA. Cervical headache: a review. In: Greive GP, ed. Modern manual therapy of the vertebral column. 2nd ed. Edinburgh: Churchill Livingstone, 1994: 333-46
11. Bogduk N. Cervical causes of headache and dizziness In: Greive GP, ed. Modern manual therapy of the vertebral column. 2nd ed. Edinburgh: Churchill Livingstone, 1994: 317-31.
12. Vernon H. ed. Upper cervical syndrome: cervical diagnosis and treatment. In: Differential diagnosis of headache. Baltimore: Williams & Wilkins. 1988: l46
13. Vernon HT. Spinal manipulation and headache of cervical origin. J Manipulative Physiol Ther 1989; 12: 455-68
14. Boline PD, Kassak K, Bronfort G, Nelson C, Anderson AV. Spinal manipulations vs. amitriptyline for the treatment of chronic tension-type headaches: a randomized clinical trial. J Manipulative Physiol Ther 1995; 18(3): 148-54.
15. Milne E. The mechanism and treatment of migraine and other disorders of cervical and postural dysfunction. Cephalgia 1989; 9 (suppl 10): 381-2.
16. Young K, Dharmi M. The efficacy of cervical manipulation as opposed to pharmocological therapeutics in the treatment of migraine patients. Transactions of the Consortium for Chiropractic Research. 1987
17. Sjaastad O, Saunte C, Hovdahl H, Breivok H, Gronback E. Cervical headache: an hypothesis. Cephalgia 1983; 3: 249-56.
18. Sjaastad O, Fredricksen TA, Stolt-Nielsen A. Cervicogenic headache, C2 rhizopathy, and occipital neuralgia: a connection. Cephalgia 1986; 6: 189-95.
19. Wolff�s Headache and other head pain. Revised by Dalessio DJ. 3rd ed. New York: Oxford University Press. 1972.
20. Selby G, Lance JW. Observations on 500 cases of migraine and allied vascular headache. J Neurol Neurosurg Psychiatry 1960; 23: 23-32.
21. Anderson A, Friberg L, Olsen T, Olsen J. Delayed hyperemia following hypoperfusion in classic migraine. Arch Neurol 1988; 45: 154-9.
22. Appel S, Kiritzky A, Zahavi I, et al. Evidence for instability of the autonomic nervous system in patients with migraine headache. Headache 1992; 32: 10-7.
23. Takasha T, Shimomura T, Kazuro T. Platelet activation in muscle contraction headache and migraine. Cephalgia 1987; 7: 239-43.
24. Lance J, Lambert G, Goadsby P, et al. 5-Hydroxytryptamine and its putative aetiological involvement in migraine. Cephalgia 1989; 9(Suppl 9): 7-13
25. Ferrari M, Odink J, Tapparelli C, et al. Serotonin metabolisminmigraine.Neurology1989;39:1239-42.
26. Dalassio D. The pathology of migraine. Clin J Pain 1990; 6: 235-9.
27. Stellar S, et al. Migraine prevention with timolol. JAMA 1984; 252(18): 2576-80.
28. Couch J, Hassanein R. Amitriptyline in migraine prophylaxis. Arch Neurol 1979; 36: 695-9.
29. Zeigler D, Hurwitz A, Hassanein R, et al. Migraine prophylaxis: a comparison of propranolol and amitriptyline. Arch Neurol 1987; 44: 486-9.
30. Anthony MN, Lance JW. Plasma serotonin in patients with chronic tension headache. J Neurol Neurosurg Psychiatry 1989; 52: 182-4.
31. Sjasstad 0, Fredricksen TA, Sand T. The localization of the initial pain of attack: a comparison between classic migraine and cervicogenic headache. Functional Neurololgy 1989; 4: 73-8
32. Commission of Enquiry Into Chiropractic. Chiropractic in New Zealand. 1979 NZ PD Hasselburg.
33. Marcus DA. Migraine and tension type headaches: the questionable validity of current classification systems. Pain 1992; 8: 28-36
34. Anthony M. Migraine and its management. Aust
Fam Phys 1986; 15(5): 643-9.
35. Grayham JR. Migraine headache: diagnosis and
management. Headache 1979; 19(3): 133-41.
36. Ghavamian T. Cervical discopathy and a new concept in the sympathetics of the cervical spine and
head. J Bone Joint Surg 1971; 53A: 1233.
37. Headache Classification Committee of the International Headache Society. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalgia 1988; 9 (Suppl
7): 1-93.
38. King J. Migraine in the workplace. Brainwaves. Australian Brain Foundation 1995 Hawthorn, Victoria.
39. Lipton RB, Stewart WE. Migraine in the United States: a review of epidemiology and health care use. Neurology 1993; 43(Suppl 3): S6-10.
40. Stewart WE, Lipton RB, Celentous DD, et al. Prevalence of migraine headache in the United States. JAMA 1992; 267: 64-9.
41. Brunarski DJ. Clinical trials of spinal manipulation: a critical appraisal and review of the literature. JMPT 1984; 7(4): 243-7.
42. Marosszeky JE. Letters to the editor: cervical manipulation for migraine. Aust NZ J Med 1979; 9: 339.



 Please Recommend Us: If you have enjoyed this video and/or we have helped you in any way please feel free to recommend us. Thank You.
Please Recommend Us: If you have enjoyed this video and/or we have helped you in any way please feel free to recommend us. Thank You.

 Please Recommend Us: If you have enjoyed this video and/or we have helped you in any way please feel free to recommend us. Thank You.
Please Recommend Us: If you have enjoyed this video and/or we have helped you in any way please feel free to recommend us. Thank You.













