Psychological Therapy for Chronic Pain Management in El Paso, TX
Psychological therapy, also known as psychotherapy, refers to the use of psychological methods to help change an individual’s way of thinking as well as improve their coping skills in order for them to learn how to best deal with stress. Psychological therapies have widely been utilized as a part of the multidisciplinary management of chronic pain. Common psychotherapies include, cognitive-behavioral therapy, mindfulness-based stress reduction and even chiropractic care. The connection between the mind and the body in relation to disease and illness have long been discussed in many research studies.
Evidence-based research studies have demonstrated that proper stress management through the use of psychological therapy as well as mindfulness interventions can effectively benefit patients with chronic pain. By way of instance, chiropractic care can safely and effectively help reduce stress, anxiety and depression by correcting spinal misalignments, or subluxation. A balanced spine can improve mood and mental health. Chiropractic care can include lifestyle modifications, such as nutritional advice, physical activity and exercise recommendations, and promote better sleeping habits, to further enhance the benefits of the treatment. The purpose of the following article is to demonstrate how psychological therapies impact the management of chronic pain.

Contents
Psychological Therapies for the Management of Chronic Pain
Abstract
Pain is a complex stressor that presents a significant challenge to most aspects of functioning and contributes to substantial physical, psychological, occupational, and financial cost, particularly in its chronic form. As medical intervention frequently cannot resolve pain completely, there is a need for management approaches to chronic pain, including psychological intervention. Psychotherapy for chronic pain primarily targets improvements in physical, emotional, social, and occupational functioning rather than focusing on resolution of pain itself. However, psychological therapies for chronic pain differ in their scope, duration, and goals, and thus show distinct patterns of treatment efficacy. These therapies fall into four categories: operant-behavioral therapy, cognitive-behavioral therapy, mindfulness-based therapy, and acceptance and commitment therapy. The current article explores the theoretical distinctiveness, therapeutic targets, and effectiveness of these approaches as well as mechanisms and individual differences that factor into treatment response and pain-related dysfunction and distress. Implications for future research, dissemination of treatment, and the integration of psychological principles with other treatment modalities are also discussed.
Keywords: pain management, multidisciplinary pain treatment, psychological therapy
Dr. Alex Jimenez’s Insight
Chiropractic care is an alternative treatment option which utilizes spinal adjustments and manual manipulations to treat injuries and/or conditions associated with the musculoskeletal and nervous system. Chiropractic treatment primarily focuses on spinal health, however, because the spine is the root of the nervous system, chiropractic care can also be effectively used to treat a variety of mental health issues. As a chiropractor, I make sure to focus on the body as a whole, rather than treating the symptoms of a single injury and/or condition. The truth of the matter is, chiropractic treatment must also deal with the emotional component of each health issue in order to provide overall relief. Psychosomatic disorders, refers to a physical illness caused or aggravated by a mental factor, such as stress. Chiropractic care can be utilized as a psychological therapy, in which, a chiropractor may recommend a series of lifestyle modifications to help reduce stress, anxiety and depression, together with spinal adjustments and manual manipulations to reduce symptoms associated with mental health issues. Furthermore, the understanding of the connection between the mind and body is essential in chiropractic treatment towards overall health and wellness.
Introduction to the Non-Pharmacological Treatment of Pain
Pain is an essential biological function that signals disturbance or damage in the body, prevents further harm through overuse of the afflicted area, and promotes physiological homeostasis.[1] Whether through abnormal healing, additional bodily damage, or failed medical intervention, pain may become chronic. Chronic pain no longer signals damage to the body and is instead a detriment to the physical and psychological well-being of the sufferer. Unfortunately, medical intervention frequently cannot resolve chronic pain, resulting in increased need for management approaches to pain, as is the approach to other chronic medical conditions.[2] In recent years, the biopsychosocial model has informed research and intervention in pain psychology, wherein physical, cognitive, affective, and interpersonal factors are used to inform treatment.[2] Currently, psychological interventions for chronic pain target a variety of domains, including physical functioning, pain medication use, mood, cognitive patterns, and quality of life, while changes in pain intensity may be secondary.[3] As such, psychological interventions for pain are ideally suited as complementary treatments to medical treatment.[4] In order to articulate the distinct philosophies and effects of each psychological intervention, it is important to first consider the variety of ways that pain affects psychological functioning.
Psychological Reactions to Pain
Recurrent pain may contribute to development of maladaptive cognitions and behavior that worsen daily functioning, increase psychiatric distress, or prolong the experience of pain.[5] Individuals suffering from chronic pain tend to show increased vulnerability to a variety of psychiatric conditions, including depressive disorders,[6] anxiety disorders,[7] and posttraumatic stress disorder.[7] However, the relationship between depression and pain is likely bidirectional, as the presence of a major depressive disorder has been identified as a key risk factor in the transition from acute pain to chronic pain.[8] Additionally, individuals with pain may suffer from significant anxiety and depressive symptomatology that does not reach the severity of a clinical diagnosis.[9] Further, chronic pain negatively impacts quality of life[10] and contributes to higher levels of disability.[10] Individuals with chronic pain are also vulnerable to higher rates of obesity,[11] sleep disturbance,[12] and fatigue,[13] show greater rates of medical utilization,[10] and are vulnerable to problematic pain medication use.[14] Given the negative psychological consequences of chronic pain, it is worthwhile to consider three psychological mechanisms related to pain-related distress that have proven to be suitable targets for intervention: pain catastrophizing, fear of pain, and pain acceptance.
Pain catastrophizing is defined as a negative cognitive and affective mental set related to expected or actual pain experience.[15] Pain catastrophizing is characterized by magnification of the negative effects of pain, rumination about pain, and feelings of helplessness in coping with pain.[16] Pain catastrophizing has been associated with various forms of dysfunction, including increased rates of depression[17] and anxiety,[16] greater functional impairment and disability due to pain,[17] and lower overall quality of life.[18] Individuals who catastrophize about their pain report lower levels of perceived control over pain,[19] poorer emotional and social functioning,[20] and poorer responses to medical intervention.[21] Pain catastrophizing also contributes to poorer pain coping and overall functioning, making pain catastrophizing a viable target for psychological intervention. Addressing catastrophic thoughts about pain improves physical and psychological functioning in the short term[22] and improves the likelihood of returning to work despite the presence of persistent pain.[23]
Pain-related fear is another psychological mechanism that has significant implications for physical and psychological functioning in chronic pain. Pain-related fear reflects a fear of injury or worsening of one�s physical condition through activities that may trigger pain.[24] Pain-related fear is associated with increased pain intensity[25] and increased disability.[26] Pain-related fear contributes to disability by fostering passive or avoidant pain-coping behaviors that contribute to physical deconditioning and pain.[27] If left unaddressed, fear of pain can impair gains in physical rehabilitation settings.[28] Evidence suggests that pain catastrophizing precedes pain-related fear,[24] but both of these mechanisms uniquely contribute to pain and physical disability.[5,29]
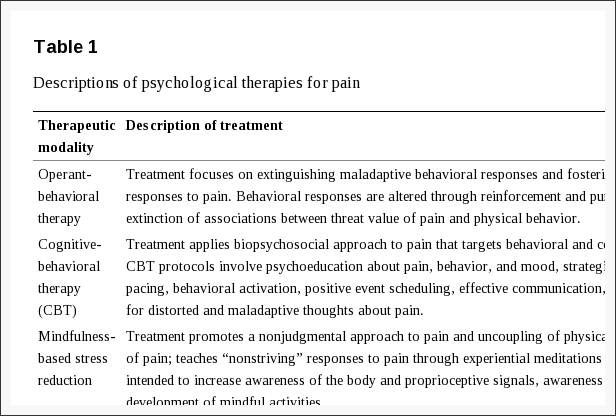
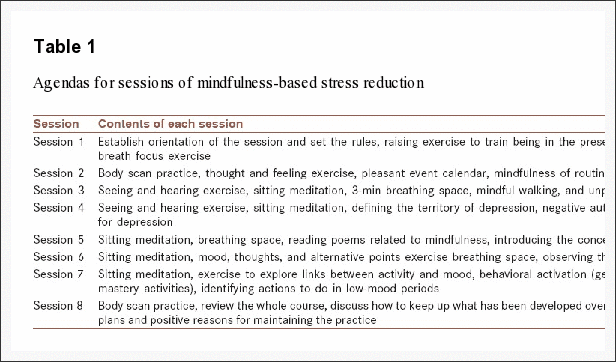
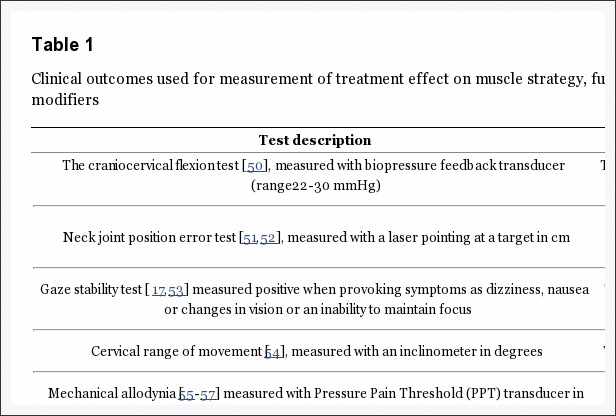
Recently, there has been increased attention to the psychological flexibility model, which extends the fear-avoidance model of chronic pain and proposes to improve treatment outcomes through fostering of accepting attitudes towards pain.[30] Psychological flexibility has been defined as an ability to engage in the present moment in a way that allows the individual to either maintain or adjust his or her behavior in the way that is most consistent with internally held goals and values;[31] this idea is especially important in times of greater pain, given the narrowing of focus that is common during times of pain.[32] Similar to psychological acceptance, which fosters a nonjudgmental approach to distressing thoughts and emotions, pain acceptance is defined as a process of nonjudgmentally acknowledging pain, stopping maladaptive attempts to control pain, and learning to live a richer life in spite of pain.[33] Pain acceptance influences emotional functioning through two distinct mechanisms: a willingness to experience pain, which buffers against negative emotional reactions to pain, and continued engagement in valued activities despite the presence of pain, which bolsters positive emotions.[34] Acceptance of pain is theorized to uncouple the occurrence of catastrophic thoughts about pain from subsequent emotional suffering[35] and reduces reliance on control- or avoidance-based coping,[36] thereby freeing cognitive and emotional resources for more meaningful pursuits.[33] Pain acceptance has demonstrated positive associations with cognitive, emotional, social, and occupational functioning in chronic pain populations.[36] Acceptance of pain predicts lower levels of pain catastrophizing[37] and greater levels of positive affect, which in turn reduce the association between pain intensity and negative emotions.[38] Pain acceptance is a particularly salient target for intervention in mindfulness- and acceptance-based therapies for chronic pain, which will be discussed later (see Table 1).
Psychological Intervention as an Approach to Pain Management
Operant Behavioral Approaches
Fordyce[39] proposed a behavioral model of pain adaptation in which maladaptive behavioral responses to pain develop through contingent relief from pain or pain-related fear. According to this theory, a behavioral drive to avoid pain leads individuals to avoid behaviors that are painful but maintain their physical and emotional health; this avoidance contributes to the development and maintenance of pain chronicity, deconditioning, and depression.[40] Operant therapy for chronic pain utilizes reinforcement and punishment contingencies to reduce pain-related behaviors and foster more adaptive behaviors, including graded patterns of activity, activity pacing, and time-contingent medication management.[40] Behavioral therapy for pain has shown positive effects on a variety of domains, including pain experience, mood, negative cognitive appraisals, and functioning in social roles.[3]
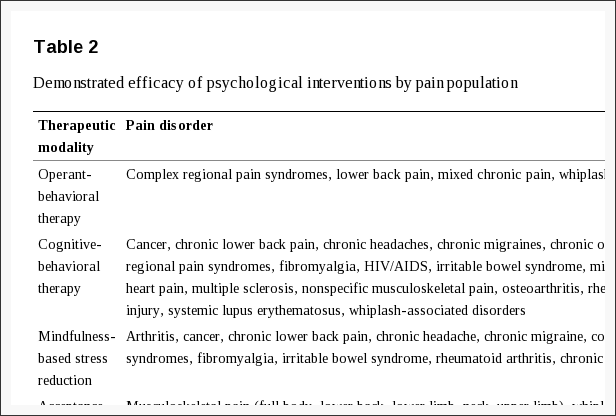
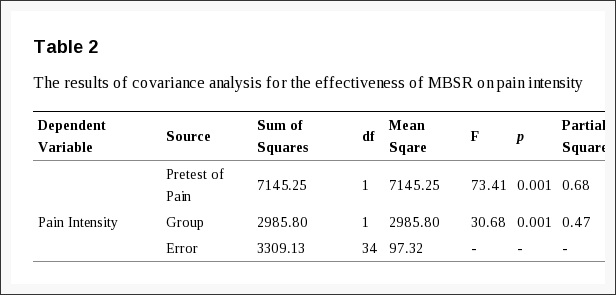
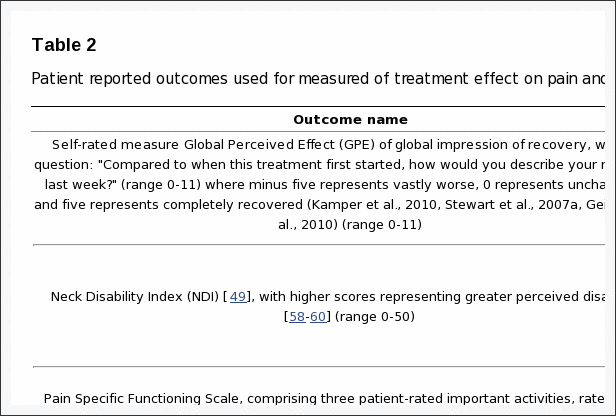
A recent application of learning theory to chronic pain involves in vivo exposure treatment for pain-related fear, which focuses on decreasing the perceived harmfulness of physical activity.[41] Learning theory posits that the aversive signal of pain may be passed to neutral stimuli (like physical movement behaviors), which contributes to avoidant behavior. In vivo exposure therapy extinguishes threat, fear, and behavioral avoidance through progressively increasing engagement in painful behaviors in the absence of catastrophic outcomes; when these behaviors are performed without serious negative consequences, patients may realize that their expectations about the consequences of physical movement and pain are unrealistic.[24,42] Consistent with exposure treatments for phobias and other anxiety disorders, in vivo exposure treatment for fear of pain involves development of a personalized, graded hierarchy of activities that elicit a fearful response, psychoeducation related to pain, fear, and behavior, and ultimately slow and systematic exposure to activities related to the individual�s fear hierarchy.[41] In vivo exposure treatment for pain-related fear has demonstrated efficacy in improving pain, pain catastrophizing, and functional disability,[41] and in decreasing pain-related fear and anxiety, depression, and anxiety.[43] Exclusively behavioral approaches to pain have been less prevalent in recent years but have demonstrated efficacy in lower back pain samples, among others (see Table 2). The effects of in vivo exposure on functional disability appear to be mediated by decreased catastrophizing and perceived harmfulness of activity[41] but may be differentially effective for patients of differing baseline levels of functionality.[40]
Cognitive-Behavioral Therapy
Cognitive-behavioral therapy (CBT) adopts a biopsychosocial approach to the treatment of chronic pain by targeting maladaptive behavioral and cognitive responses to pain and social and environmental contingencies that modify reactions to pain.[44] CBT principles have demonstrated efficacy for a variety of psychiatric disorders and physical illnesses, in addition to pain.[45] CBT for pain develops coping skills intended to manage pain and improve psychological functioning, including structured relaxation, behavioral activation and scheduling of pleasurable events, assertive communication, and pacing of behavior in order to avoid prolongation or exacerbation of pain flares. Unlike operant-behavioral approaches, CBT for pain also addresses maladaptive beliefs about pain and pain catastrophizing through formal use of cognitive restructuring: identification and replacement of unrealistic or unhelpful thoughts about pain with thoughts that are oriented towards adaptive behavior and positive functioning.[44] CBT for pain has been widely implemented as a standard treatment for pain and constitutes the current �gold standard� for psychological intervention for pain.[44]
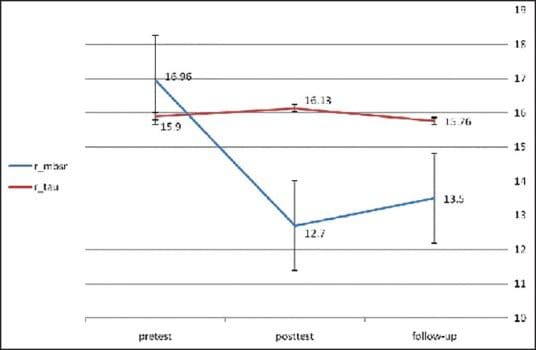
According to recent meta-analytic studies,[45] CBT for pain demonstrates small-to-medium effect sizes in a variety of domains and shows effects on pain and functioning comparable to standard medical care for pain.[3] CBT significantly improves disability and pain catastrophizing after treatment and yields longer-term improvements in disability, above and beyond the effects of usual medical care,[3] as well as smaller effects on pain, catastrophizing, and mood when compared to no treatment.[3] CBT-related changes in helplessness and catastrophizing are uniquely predictive of later changes in pain intensity and pain-related interference in daily functioning.[22] CBT is also a valuable adjunct treatment in physical rehabilitation programs.[46] The benefits of CBT for pain have been noted in many chronic pain populations (see Table 2) but may not be as robust in some populations, including fibromyalgia.[47] Further, some have suggested that the effects of CBT are at best moderately sized and not maintained long-term.[30] The intractable nature of chronic pain may make adaptation difficult as attempts to control pain may prove ineffectual, ultimately contributing to greater psychological distress.[36] Recent efforts have thus expanded the cognitive-behavioral model of pain intervention to address these issues, which has yielded two newer treatment modalities: mindfulness-based stress reduction (MBSR) and acceptance and commitment therapy (ACT). Unlike CBT, these approaches focus on fostering acceptance of chronic pain rather than emphasizing strategies for controlling pain, thereby improving emotional well-being and greater engagement in nonpain-related pursuits. Though these interventions both target acceptance of pain, they differ in their therapeutic implementation and approach to meditation and daily practice.
Mindfulness-Based Stress Reduction
Mindfulness-based interventions approach seeks to uncouple the sensory aspects of pain from the evaluative and emotional aspects of pain,[48] and promote detached awareness of the somatic and psychological sensations within the body.[48] As the chronic pain signal often cannot be extinguished, this detachment may enhance individual responses to chronic pain.[48] Through mindful awareness and meditation, thoughts about pain can be viewed as discrete events rather than an indication of an underlying problem that necessitates immediate and possibly maladaptive responses.[49] An individual may then recognize these sensations or thoughts as something familiar, which may serve to ameliorate emotional or maladaptive behavioral responses to pain.
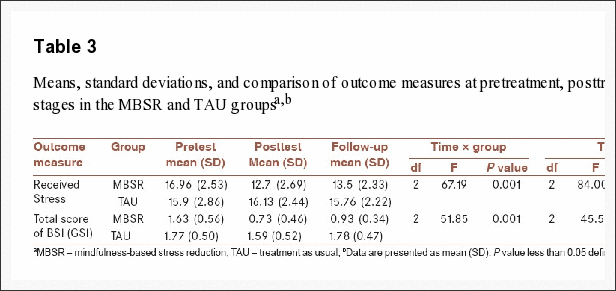
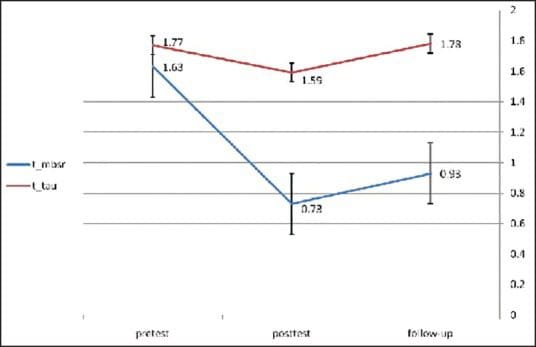
MBSR is a form of meditation developed in Eastern philosophy and later adapted to Western intervention that enhances awareness and acceptance of physical, cognitive, and emotional states and disconnects psychological reactions from the uncontrollable experience of pain flares.[44] MBSR interventions have traditionally been structured as 2-hour sessions occurring weekly over 10 weeks that develop awareness of the body and proprioceptive signals, awareness of the breath and physical sensations, and development of mindful activities (such as eating, walking, and standing).[48] MBSR promotes mindfulness through daily meditation, which is a requisite component of the treatment.[50] The mechanisms underlying effective MBSR intervention may be similar to desensitization to pain, as meditations involve motionless sitting practices that expose participants to painful sensations in the absence of catastrophic consequences.[48,50] In this way, MBSR interventions may function similarly to in vivo exposure for pain but serve the additional purpose of increasing tolerance for negative emotions, thereby fostering more adaptive responses to pain.[50] MBSR also reduces rumination[51] and interoception of distressing physical signals[52] and increases mindful awareness[51] and acceptance of pain.[53] MBSR necessitates cultivation of daily mindfulness practices,[48] yet compliance rates of MBSR have been found to compare favorably to behavioral pain management techniques.[54] However, evidence on the importance of daily practice is mixed; the amount of time devoted to these mindful activities correlates with symptom improvement in some studies,[55] yet compliance rates appear to correlate only modestly with improvement in others.[54] Unlike CBT, which identifies thoughts as distorted and in need of change, practitioners of mindfulness adopt a nonjudgmental approach to thoughts as �discrete events� that encourage emotional distance from thoughts.[44,50] Further, CBT is a goal-oriented treatment modality, targeting an increased relaxation response or an altered behavioral or thought response, whereas mindfulness does not prescribe specific goals, relying instead on nonjudgmental observation.[50] Further, mindfulness instructors are expected to engage in their own daily mindfulness practices, whereas CBT practitioners do not necessarily need daily practice in CBT to teach it effectively.[50]
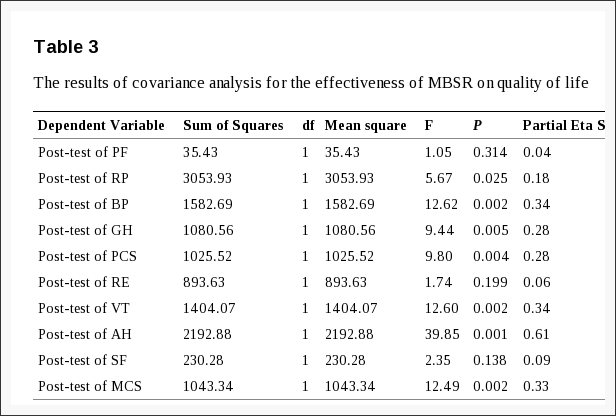
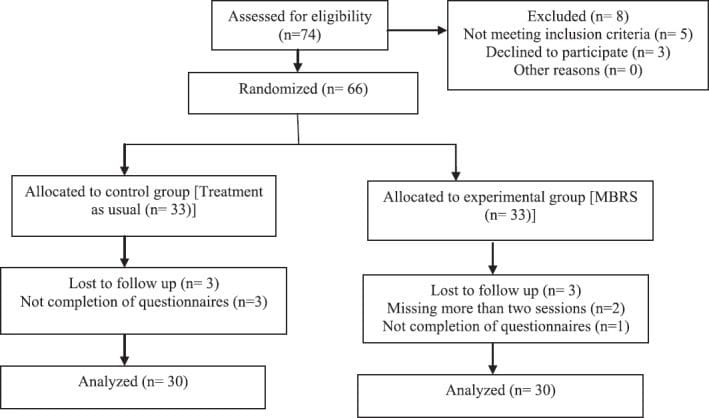
MBSR has demonstrated efficacy in addressing the severity of medical symptoms and psychological symptoms,[48] pain intensity,[56] and coping with stress and pain;[54] these treatment gains may last up to 4 years after intervention in many domains.[54] MBSR has been effective in diverse pain samples,[48,54,56] and in individuals with irritable bowel syndrome,[52] neck pain,[57] migraine,[57] fibromyalgia,[58] and chronic musculoskeletal pain.[59] Additionally, MBSR addresses co-occurring symptoms of depression in individuals with some chronic pain conditions like fibromyalgia[60] and enhances the effects of multidisciplinary treatment on disability, anxiety, depression, and catastrophizing.[61] Meta-analytic studies of MBSR in chronic pain have shown small to moderate effects of MBSR on anxiety, depression, and psychological distress in patients with chronic illnesses including pain,[62] and these benefits tend to be robust across studies.[63] However, as with CBT, MBSR may be differentially effective across populations; a recent longitudinal study noted greater improvements in pain, health-related quality of life, and psychological well-being for back or neck pain than in fibromyalgia, chronic migraine, or headache.[57]
Acceptance and Commitment Therapy
ACT adopts a theoretical approach that thoughts do not need to be targeted or changed; instead, responses to thoughts may be altered so that their negative consequences are minimized.[31] ACT interventions improve well-being through nonjudgmental and purposeful acknowledgment of mental events (ie, thoughts and emotions), fostering acceptance of these events, and increasing the ability of the individual to remain present and aware of personally relevant psychological and environmental factors; in doing so, individuals are able to adjust their behavior in a way that is consistent with their goals or values, rather than focusing on immediate relief from thoughts and emotions.[31] In the treatment of pain, ACT fosters purposeful awareness and acceptance of pain, thereby minimizing the focus on reducing pain or thought content and instead directing efforts towards fulfilling behavioral functioning.[44] ACT shares conceptual similarity with MBSR due to shared goals of promoting mindfulness and acceptance of pain but, unlike MBSR, ACT does not utilize daily mindful meditation and instead focuses on identification of the values and goals of the individual, which serve to direct behavior.[64] ACT-based interventions have demonstrated benefits on various aspects of mental health in chronic pain populations, including mental health quality of life, self-efficacy, depression, and anxiety.[65] Some studies of ACT interventions for chronic pain have reported medium or larger effect sizes for improvements in pain-related anxiety and distress, disability, number of medical visits, current work status, and physical performance,[66,67] with smaller effects of this intervention noted on pain and depression.[64] However, meta-analytic studies of acceptance-based therapies for pain have revealed that ACT does not show incrementally greater efficacy in comparison to other established psychological treatments for chronic pain.[64]
Future Directions and Remaining Questions
The extant literature suggests that each of the previously reviewed psychological interventions has retained value for the treatment of chronic pain. At present, there is little evidence of the superiority of any treatment approach, with one exception: CBT has demonstrated incrementally greater benefit in many areas than the effects of behavioral therapy.[3] As previously noted, however, operant-behavioral principles have been adopted for newer treatment approaches like in vivo exposure for fear of pain, which has demonstrated good benefit in multidisciplinary treatment with some pain populations.[41] Recent reviews have concluded that MBSR and ACT are promising but yield generally comparable effects to CBT, despite their distinct intervention methods.[64] The ability to draw conclusions regarding treatment superiority is further limited by the smaller number of high-quality studies of ACT or MBSR compared to the more robust CBT literature.[64]
Some critical questions remain regarding the comparative effectiveness of these interventions. First, the effects of CBT are significant in the short term but are not consistently maintained across time, possibly due to decreased adherence.[3] It is conceivable that acceptance-based approaches, which are predicated less on mechanistic coping strategies and instead foster accepting attitudes towards pain, may show greater rates of long-term adherence and longer-term benefits than CBT, though future study of this question is needed. Further, some pain disorders (such as fibromyalgia) have shown comparatively poorer treatment response to CBT than other pain disorders in some studies, which highlights the possible benefit of alternative interventions in such populations. Indeed, ACT and MBSR have also shown efficacy in fibromyalgia populations, though there remains a need to identify predictors of differential treatment response.[65]
Safety and Tolerability of Psychological Therapies
Psychological therapies for pain are presumed to be at low risk for adverse effects to the recipient; as a result, there is a dearth of empirical evidence regarding the risks of psychological interventions.[68] Some have suggested that patients who enter psychological treatment face risks of incorrect psychological diagnosis, psychological dependence, undermining of a patient�s ability to make their own decisions, or manipulation by the therapist to achieve nontherapeutic goals.[69,70] However, these concerns are alleviated through proper clinical and ethical training of practitioners and are not typically considered salient risks of psychological therapies when they are properly administered.[70] Recently, there has been a call for additional research to address the possibility of adverse psychotherapeutic effects[71] as well as a more systematic method of monitoring and identifying adverse events related to psychotherapy.[68] Though the rates of adverse effects of psychotherapy are still largely unknown, it is encouraging that recent studies have begun to specifically report the incidence of adverse events directly.[72]
Factors Affecting the Outcomes of Psychological Intervention
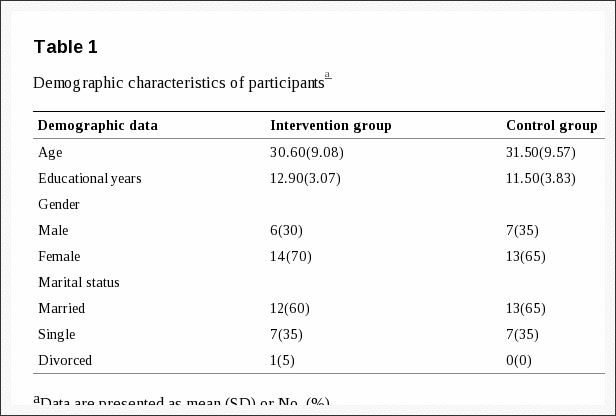
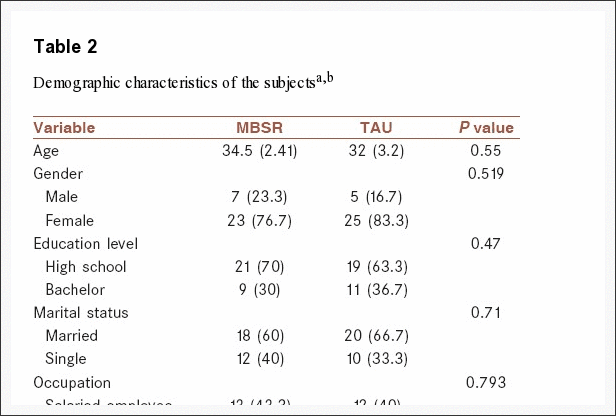
Practitioners should be cautioned against the assumption of homogeneity among patients with pain disorders, as a variety of factors may predict treatment response.[69,71] Turk[73] proposed that individuals coping with comparable levels of pain show distinct patterns of response that could be clustered into recognizable subclasses: �dysfunctional� patients, who report high levels of pain-related interference and distress; �interpersonally distressed� patients, who report lacking the support of loved ones in coping with their pain; and �adaptive copers,� who report notably higher levels of function and perceived social support and lower levels of pain-related dysfunction. Turk proposed that these patient subgroups respond differently to psychological intervention, and subsequent findings have supported this idea: �dysfunctional� patients have demonstrated greater response to interdisciplinary treatment involving psychological care than �interpersonally distressed� patients.[74] Identification of patient subgroups may be accomplished using instruments like the Multidisciplinary Pain Inventory[75] and through detailed assessment of chronic pain intensity and disability.[76] Additionally, patients� readiness to adopt a self-management approach to their own chronic pain appears to have significant implications for treatment response;[77] patients who are in the precontemplation stage of treatment readiness may benefit more from insight-focused therapy, versus those in an action stage, who may benefit more from establishing relaxation-based and other active coping strategies.[77] Patient readiness to self-manage pain may be assessed using the Pain Stages of Change Questionnaire.[77] Additionally, treatment response may be subject to patient beliefs about the importance of intervention-specific behaviors and about one�s own ability to perform these actions.[78]
Additionally, there may be demographic, psychological, and medical differences among patients that are relevant to treatment response, including the etiology of pain conditions, socioeconomic status, and cultural and ethnic background; these factors require further empirical research in order to optimize clinical outcomes but have not yet received adequate attention in the clinical literature.[79] For example, baseline levels of physical functioning appear to predict response to certain psychological treatment modalities like in vivo exposure for fear of pain.[40] Further, baseline levels of pain, depression, and anxiety have been found to predict dropout rates in some samples,[80,81] though these effects are not apparent in all samples.[3] In addition to being an important mechanism of treatment, there is evidence that baseline levels of fear of pain may also predict differential treatment response; individuals more fearful of pain at the outset of a multidisciplinary pain treatment program showed greater responsiveness to in vivo exposure for this problem.[28] The presence of medical comorbidities that are likely to impact future functioning is also important to consider; recently, psychological interventions have been developed that address comorbid symptoms of sleep,[82] obesity,[29] and fatigue[83] that may accompany chronic pain. Hybrid treatments may be more important in independent clinical practice, where comorbidity is more common.[82] Notably, there is little evidence that personality variables factor significantly into treatment response; most of the connections between personality traits and variables relevant to psychological intervention for pain are theoretical and have not consistently emerged in empirical research.[84,85]
Patient age is also an important consideration in examining responses to interventions for pain. Older adults have increased risks of various ailments related to pain, including arthritis and osteoporosis, but may have poor tolerance to medications for these conditions.[86] Further, age may alter psychological reactions to pain; the emotional aspects of pain are more strongly correlated with pain catastrophizing in younger adults than older adults while sensory aspects of pain appear more strongly related to pain catastrophizing in older adults.[87] Additionally, treatment protocols may require accommodation for elderly populations; addressing an elderly patient�s fear of movement may be complicated by a fear of falling that is absent in younger populations.[88] As memory concerns are more common in older adulthood, treatment protocols may be improved if they minimize the demand for memorized tasks.[89] Unfortunately, research is lacking for specific psychological interventions in elderly populations.[86] In general, psychological interventions are presumed to be of low risk for older adults,[90] and CBT for pain has received comparatively greater empirical support for older adults.[88] Overall, the efficacy of psychological intervention for pain in older adults is an area that warrants additional study in the future.
Treatment availability is a key consideration for psychological intervention, especially for patients in poverty or living in remote geographical locations. Though it is beyond the scope of this paper to review ethnic and socioeconomic contributors to health, low socioeconomic status is a significant risk factor for the development of chronic pain and factors heavily into racial disparities in health outcomes.[91] As financial challenges may restrict access to traditional psychological interventions, the importance of alternative modalities for provision of mental health interventions for chronic pain is paramount. Teleinterventions[92] and Internet-based interventions[93] may be viable for psychological treatment of chronic pain; Internet-based programs delivering ACT,[94] CBT,[46] and mindfulness interventions[95] have demonstrated benefits in psychosocial functioning, mood, and pain coping. However, methodologically rigorous clinical trials and evidence for maximally effective and efficient implementation of these programs are needed, as many interventions have shown modest effects and comparatively high dropout rates.[96]
Combining psychological treatment modalities with one another and with other medical interventions may constitute the next logical step in enhancing treatment outcomes. Institution of a flexible, goal-oriented approach, akin to ACT, may enhance engagement and adherence in CBT.[97] Additionally, a combination of graded in vivo exposure and ACT may show incremental benefit in addressing pain-related fear and anxiety.[98] Effects of CBT may also be enhanced in conjunction with treatments like biofeedback[99] and hypnosis.[100] A word of caution: presentation of psychological treatment by nontraditional practitioners may show variable effectiveness unless treatment approaches are adjusted appropriately.[101] If trained properly, however, appropriately-designed cognitive-behavioral interventions can be effectively administered by physiotherapists,[102] physical therapists,[103] nurses, and occupational therapists.[104]
Conclusion
Psychotherapy constitutes a valuable modality for addressing the behavioral, cognitive, emotional, and social factors that both result from and contribute to pain-related dysfunction and distress through enhancement of self-management strategies. There are several distinct psychological interventions that differ in their theoretical approaches, therapeutic targets, and areas of efficacy, but CBT, ACT, MBSR, and operant behavioral approaches to pain may all play important roles for enhancing the self-management abilities of individuals with chronic pain. However, there remains a need to identify predictors of differential treatment response and salient patient subgroups to optimize treatment outcomes, as well as additional and alternative means to provision of psychological services for those who are unwilling or unable to engage in traditional psychotherapy. More empirical research into contributing factors of differential treatment response and the dissemination of psychological treatment for pain may result in significant savings to the physical, emotional, and financial costs of chronic pain.
Footnotes
Disclosure:�The author reports no conflicts of interest in this work.
In conclusion, psychological therapies, such as cognitive-behavioral therapy, mindfulness-based stress reduction and even chiropractic care, have been demonstrated to effective help treat chronic pain, according to research studies. The connection between the mind and body has previously been referenced as a cause for a variety of health issues, including chronic pain. Finally, the article above demonstrated the effects of psychological therapy for chronic pain management. Information referenced from the National Center for Biotechnology Information (NCBI). The scope of our information is limited to chiropractic as well as to spinal injuries and conditions. To discuss the subject matter, please feel free to ask Dr. Jimenez or contact us at 915-850-0900 .
Curated by Dr. Alex Jimenez
Additional Topics: Back Pain
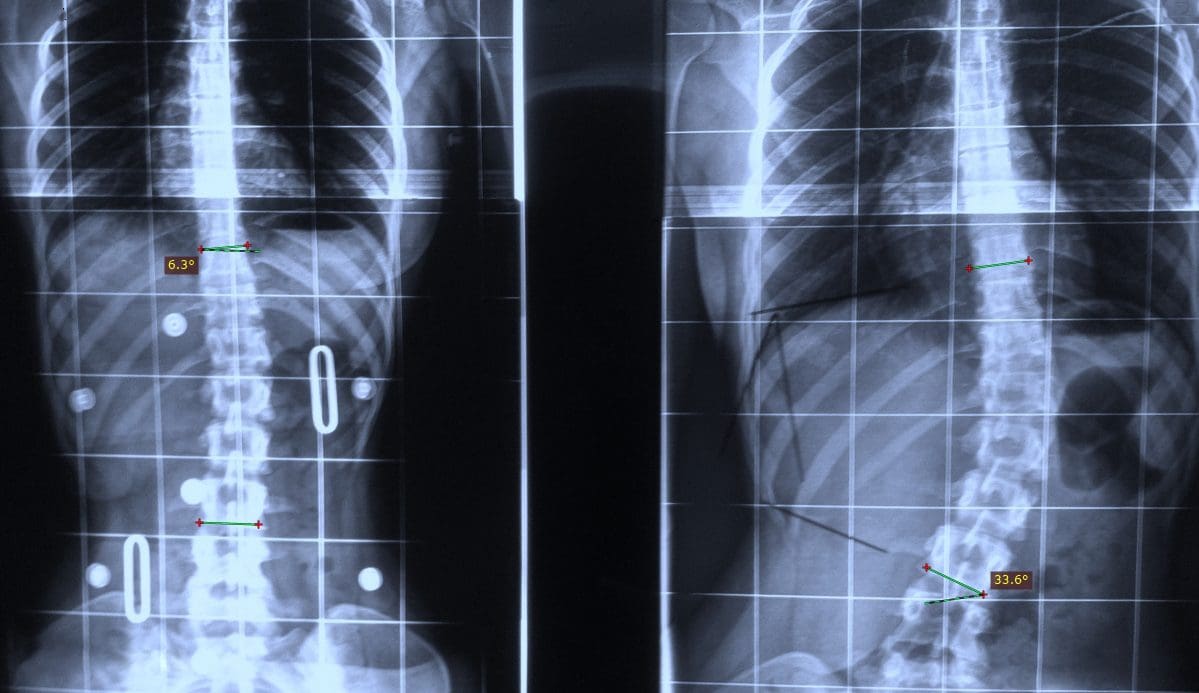
According to statistics, approximately 80% of people will experience symptoms of back pain at least once throughout their lifetimes. Back pain is a common complaint which can result due to a variety of injuries and/or conditions. Often times, the natural degeneration of the spine with age can cause back pain. Herniated discs occur when the soft, gel-like center of an intervertebral disc pushes through a tear in its surrounding, outer ring of cartilage, compressing and irritating the nerve roots. Disc herniations most commonly occur along the lower back, or lumbar spine, but they may also occur along the cervical spine, or neck. The impingement of the nerves found in the low back due to injury and/or an aggravated condition can lead to symptoms of sciatica.

EXTRA IMPORTANT TOPIC: Managing Workplace Stress
MORE IMPORTANT TOPICS: EXTRA EXTRA: Car Accident Injury Treatment El Paso, TX Chiropractor