- Long periods of sitting/standing
- Forward bending
- Body maneuvers that increase pressure in intervertebral discs
- Coughing
- Sneezing
- Characterize the activities leading up to when the symptoms first presented
- Location of the pain
- Associated factors that reduce and worsen the pain
- Medical history

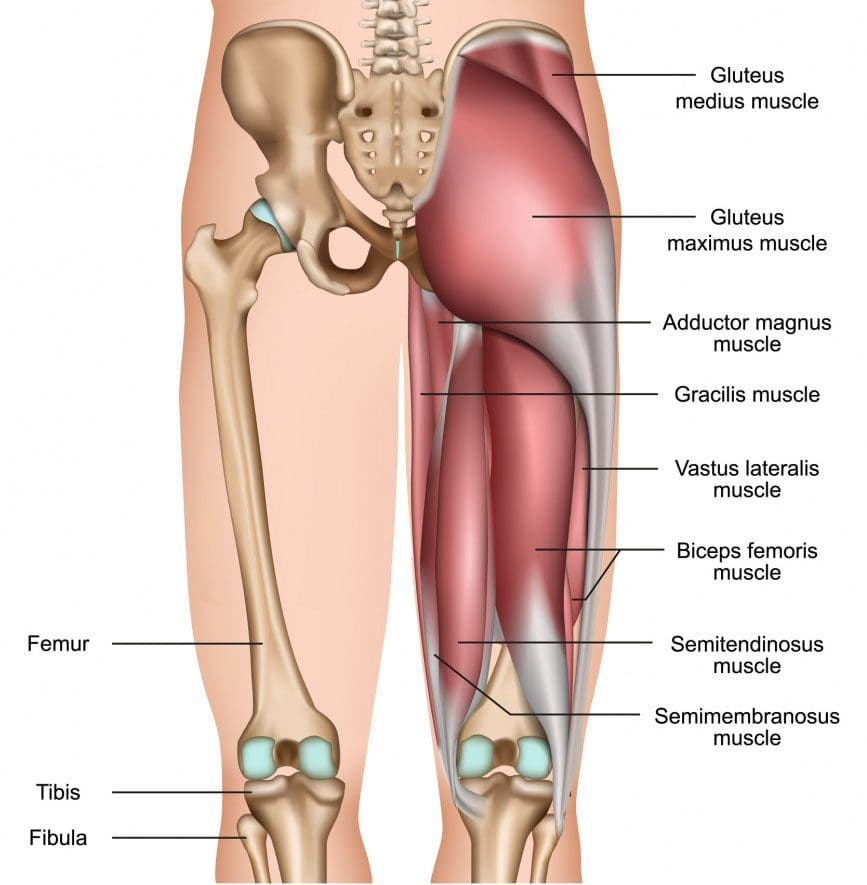
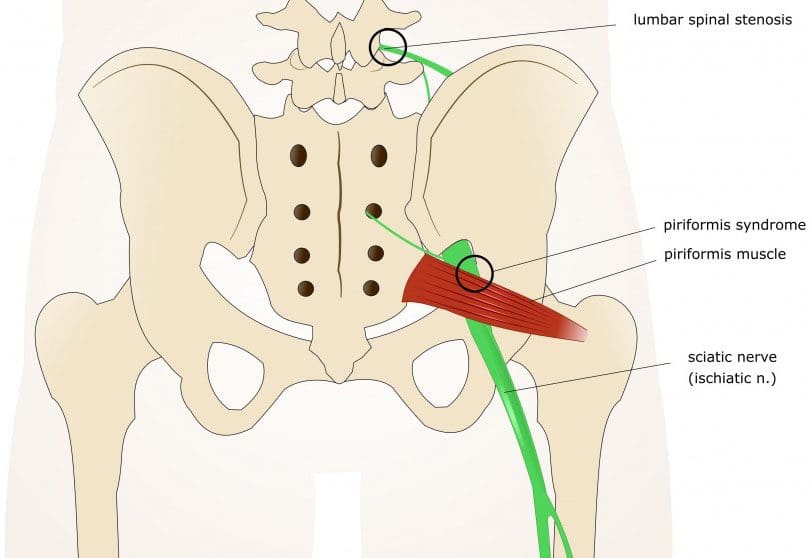
- The way the sciatic nerve runs through the lower body. It starts in the lower lumbar and upper sacral nerve roots. It exits through the pelvis and runs down the back of the thigh to the knee where it branches out into nerves that provide the motor and sensory functions to the legs and feet.
- Non-spinal sciatica causes. Non-spinal causes usually are the result of irritation of the nerve itself. The most common ways to irritate the nerve is compression, traction, or injury.
- Symptoms perceived as sciatica may not be related to the nerve at all. Injury/s to structures close to the nerve, like the hip, can copy symptoms caused by irritation of the nerve.
Contents
Hip joint disorders can emulate sciatica symptoms
Because the sciatic nerve is close to the hip joint, an injury to the hip could resemble symptoms of sciatica. Whatever the cause of the hip injury, those with hip pathology often report pain in the groin, upper thigh, and buttocks. The pain gets worse with activity, specifically bending, and rotation of the hip. Leg pain that turns into a limp when walking means that more likely the hip, and not the lower back, is the cause of the leg pain. X-rays and if necessary MRIs of the hip can help in determining if the hip is the cause of leg pain. An example of hip pathology that mimics spine-related sciatica:Hip Osteoarthritis
This is characterized by the loss of cartilage. This results in the narrowing of the ball and socket joint. Individuals with arthritis of the spine and hip, a doctor could use a steroid injection as a therapeutic providing pain relief and a diagnostic to help identify the root cause/pain generator.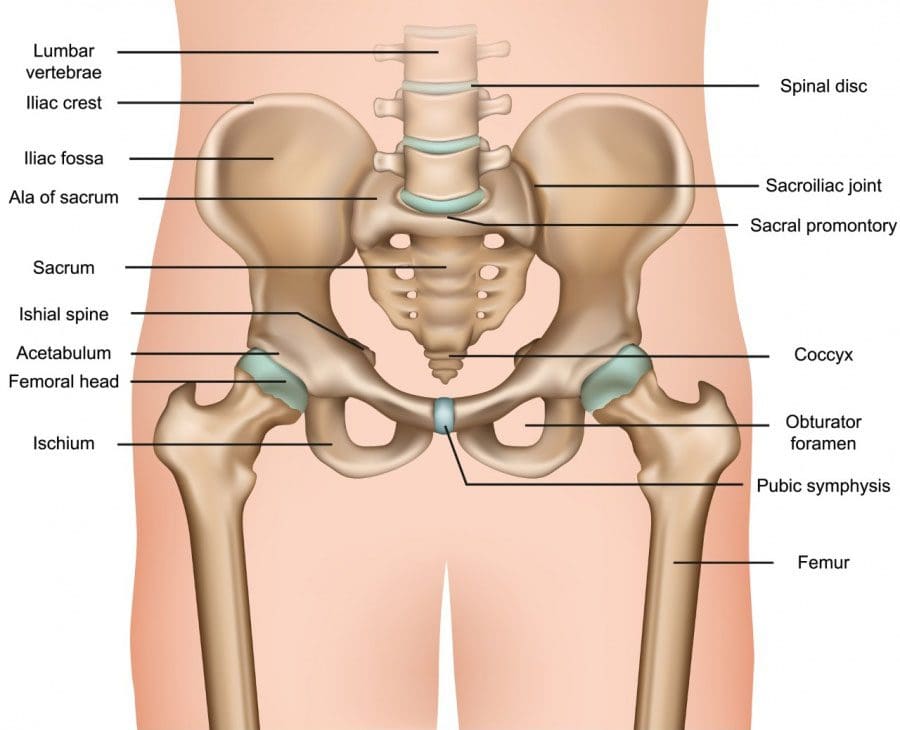
Osteonecrosis
The femoral head can collapse from a lack of blood flow. Risk factors include:- Alcohol abuse
- Sickle cell disease
- Chronic steroid use
- Femoral neck fracture
- Hip dislocation
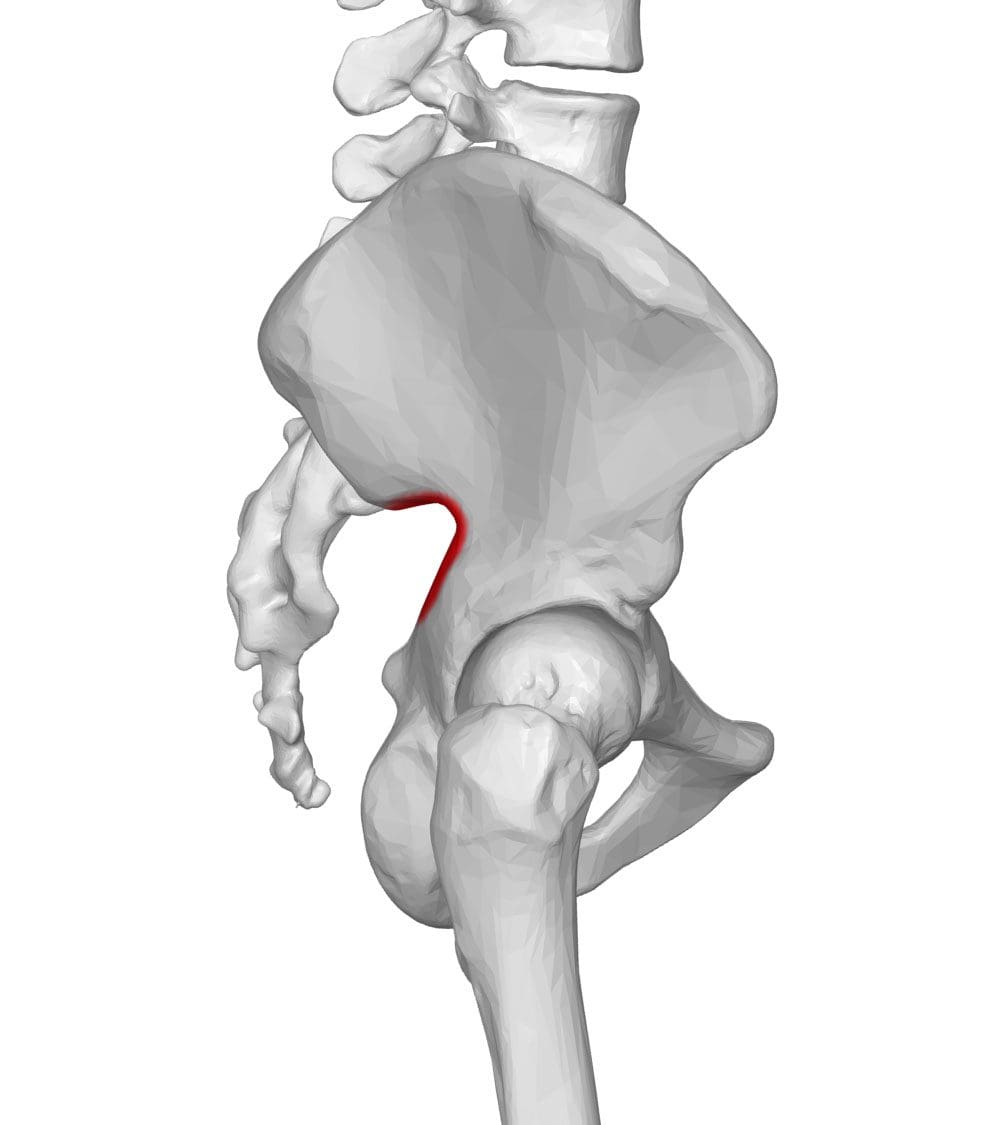
Femoroacetabular Impingement
This can stem from constant abnormal rubbing between the femoral neck and acetabulum from a bone deformity of the femur, or the acetabulum. Hip impingement at the joint can start the onset of arthritis along with tears of the labrum. This is cartilage that surrounds the hip joint and provides stability.Trochanteric Bursitis
There are fluid-filled sacs called bursas/bursae that help decrease friction between the bones, surrounding tendons, and muscles. They are at multiple locations on the body. Bursitis means that the bursa is inflamed and can be quite painful. The greater trochanter is a bony outward bump that extends from the femur. Trochanteric bursitis refers to inflammation of the bursa that separates the greater trochanter with the muscles and tendons of the thigh. Common symptoms are pain on the outside of the thigh that worsens by pressing on the area and can interfere with proper sleep when lying on the affected side.Femoral Neck Stress Fracture
Incomplete fracture/s of the femoral neck typically occur in individuals that walk or run long distances regularly like runners and soldiers. The pain is usually focused around the groin and can be subtle when it presents. Walking or running makes the pain worse.Sacroiliac joints and fractures
The sacroiliac joints connect the spine to the pelvis. There are two joints, one on either side of the sacrum. While they are relatively immobile, they go through tremendous force doing routine daily activities. Sacroiliac joint pathology that can mimic spine-related sciatica include:Sacroiliitis
This is inflammation of the sacroiliac joints. The pain presents in a slow fashion with no obvious injury or cause. The pain is usually localized to the buttocks and can radiate down the back of the thigh. It is believed to be caused by irritation of the sciatic nerve by the inflammatory molecules in the sacroiliac joint or could present as referred pain from the joint. This is pain that is detected in a location other than the area of the pain generator. The pain reduces with light walking.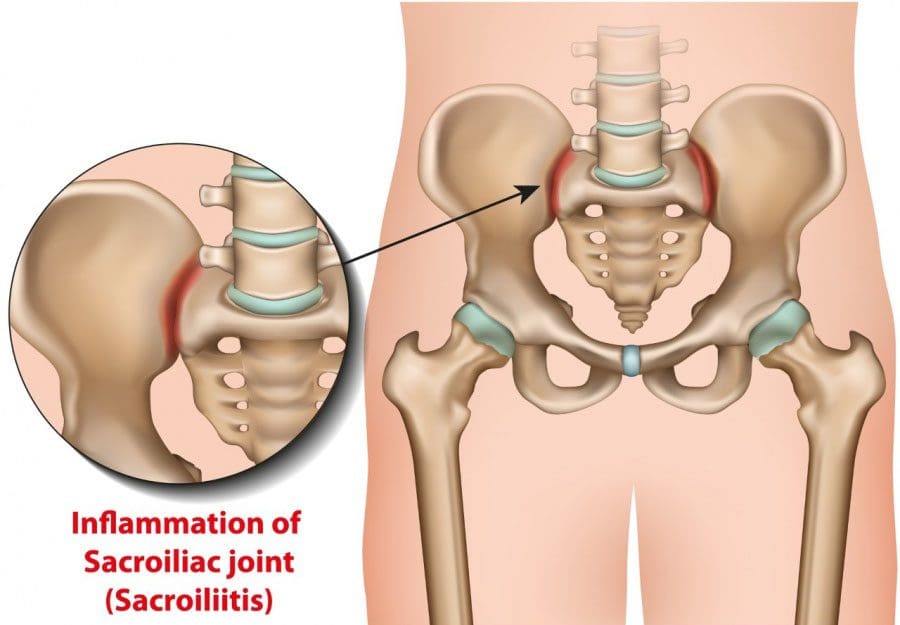
Sacral Fracture
A fracture of the sacrum can occur in those with a weakened bone after a minor injury and without trauma. Risk factors include:- Advanced age
- Osteoporosis
- Chronic steroid use
- Rheumatoid arthritis
- Vitamin D deficiency.
Trauma-related
Trauma to the pelvis or thigh can definitely cause sciatica pain and symptoms. With high-energy injuries, it is possible for the nerve roots of the sciatic nerve to get pulled or torn. More common causes include:- Posterior hip dislocation
- Pelvic fracture
Penetrating trauma
If some sharp object like a tool or shrapnel penetrates any area where the sciatic nerve is, it could cause sciatica by cutting the nerve. Or the object tears the nerve, known as a laceration. Most cases of trauma-induced sciatica result from a mild form of nerve injury known as neuropraxia. This is an injury that temporarily blocks nerve function. Neuropraxia can develop from the shock waves that surround the object as it travels through the tissue.Benign tumors and metastatic cancer
Discovering cancer during diagnosis for sciatica is rare. Symptoms that increase the possibility of cancer being the cause include:- Cancer in medical history
- 50 years and older
- Leg pain that goes on through the night
- No relief from lying on the back
- Night sweats
- Unexplained weight loss
- Nerve tumors include neurofibroma and schwannoma
- Surrounding fatty tissue called a lipoma
- Metastases from another source like lung cancer
Shingles
Shingles is a painful rash that occurs on one side of the body. It is caused by the varicella-zoster virus, which is the virus that causes chickenpox. The virus can lie dormant in nerve cells for years without causing any symptoms. Older individuals and individuals with underlying conditions in an immunocompromised state can cause the virus to activate. If the virus reactivates around the buttock and thigh, it can feel like sciatica. The presence of a red rash with blisters around the painful area is consistent with shingles.Childbirth and endometriosis
During pregnancy, the pelvis can become compressed between the growing baby and the bones in the pelvis. Also, having the hips and knees flexed and supported in stirrups too long can also cause sciatica. However, pregnancy-related sciatica is often temporary. A less common cause that occurs in women is endometriosis. Endometriosis is the growth of tissue somewhere other than the uterus, usually the ovaries and fallopian tubes. In some cases, this tissue can accumulate around the sciatic nerve or the nerve itself. As the tissue responds to the changes taking place during a normal menstrual cycle, recurrent sciatica pain can present.Vascular diagnoses
Arteries and veins in the pelvis and lower extremities that have become abnormal can cause sciatica. Either through compression or lack of oxygen from poor blood flow. An aneurysm can happen when the wall of the artery weakens and cannot withstand the pressure of the blood flowing through. This enlarges the artery and in some cases, the artery grows large enough to compress the nerve. Peripheral artery disease can cause sciatica when not enough blood is circulated from the heart to the muscles in the legs. If not enough oxygen is delivered to the muscles, leg pain and numbness can occur. It’s called claudication and is characterized by pain that is aggravated when walking and relieved when standing still. Risk factors for peripheral artery disease include:- Smokers both current and those who have quit
- High blood pressure
- High cholesterol
- Diabetic
Diabetes/high blood sugar
Diabetic peripheral neuropathy happens from nerve damage caused by high blood sugar. Nerves that are exposed to chronic high blood sugar can get damaged from the disruption of proper blood flow or from an alteration of the cellular structure of the nerve.Prescription meds
Nerve and muscle damage can happen as a side effect from prescription meds. Neuropathy and myopathy can cause symptoms that mimic sciatica brought on by disc herniation. Sometimes, if the medication is no longer taken the symptoms go away. The list of medications include:- Chemotherapy agents
- Antibiotics
- Statins medication to help lower cholesterol
Piriformis syndrome and back pocket wallets
Back pocket wallet
Also known as wallet neuritis, and wallet sciatica are terms that have been used to describe compression of the sciatic nerve by a heavy/bulky wallet in a back pocket. It is similar to symptoms of piriformis syndrome and presents in the buttocks and the same leg that can get aggravated from sitting. Usually, if the wallet is the sole cause, taking the wallet from the back pocket to another pocket or other storage option often brings pain relief.Conclusion non-spine related causes
While the majority of sciatica cases are caused by a back problem, injury, etc. There are various causes outside of the spinal column. Being able to describe the:- Location
- Pain severity
- Associated symptoms
- Factors that aggravate and alleviate the pain
Chiropractors & Sciatica Syndrome Expose
Dr. Alex Jimenez�s Blog Post Disclaimer
The scope of our information is limited to chiropractic, musculoskeletal, physical medicines, wellness, and sensitive health issues and/or functional medicine articles, topics, and discussions. We use functional health & wellness protocols to treat and support care for injuries or disorders of the musculoskeletal system. Our posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate and support directly or indirectly our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We also make copies of supporting research studies available to the board and or the public upon request. We understand that we cover matters that require an additional explanation as to how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. The provider(s) Licensed in Texas& New Mexico*General Disclaimer, Licenses and Board Certifications *
Professional Scope of Practice *
The information herein on "When Sciatica Is Not Spine Related" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and on our family practice-based chiromed.com site, focusing on naturally restoring health for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez, DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card








