Physicians, neurologists, and other healthcare professionals may often run a cranial nerve examination as part of a neurological evaluation to analyze the operation of the cranial nerves. This involves a highly formalized series of tests that evaluate the status of each cranial nerve. A cranial nerve test begins with observation of the patient partly due to the fact that cranial nerve lesions may ultimately affect the symmetry of the face or eyes, among other signs and symptoms.
The visual fields for neural lesions or nystagmus�are tested via an evaluation of particular eye movements. The sensation of the face is tested by asking patients to execute different facial movements, like puffing out their cheeks. Hearing is tested through voice and tuning forks. The position of the individual’s uvula is also examined because asymmetry in its placement could indicate a lesion of the glossopharyngeal nerve. After the capability of the individual to use their shoulder to test the accessory nerve (XI), the patient’s tongue operation is generally assessed by detecting various tongue movements.
Contents
Damage or Injury of the Cranial Nerves
Compression
Cranial nerves may be compressed due to increased intracranial pressure, a profound effect of an intracerebral haemorrhage, or tumour which presses against the cranial nerves and interferes with the communication of impulses along the length of a nerve. In some instances, a loss of functionality of one cranial nerve may on occasion be the first symptom of an intracranial or skull base cancer.
An increase in intracranial pressure can lead to dysfunction of the optic nerves (II) because of the compression of the surrounding veins and capillaries, resulting in swelling of the eyeball, known as papilloedema. A cancer, such as an optic glioma, can also affect the optic nerve (II). A pituitary tumour can compress the optic tracts or the optic chiasm of the optic nerve (II), causing visual field loss. A pituitary tumour may also extend into the cavernous sinus, compressing the oculuomotor nerve (III), the trochlear nerve (IV) and the abducens nerve (VI), often leading to double-vision and strabismus. These cranial nerves may also be impacted by herniation of the temporal lobes of the brain via the falx cerebri.
The cause of trigeminal neuralgia, where one side of the face experiences painful signs and symptoms, is believed to be due to the compression of a cranial nerve by an artery as the nerve exits from the brain stem. An acoustic neuroma, especially at the junction between the pons and medulla, may compress the facial nerve (VII) and the vestibulocochlear nerve (VIII), resulting in hearing and sensory loss on the affected side.
Stroke
Occlusion of blood vessels which supply the cranial nerves or their nuclei, or an ischemic stroke, might cause specific signs and symptoms which could localize where the occlusion happened. A clot in a blood vessel draining the cavernous sinus, also known as the cavernous sinus thrombosis, may affect the oculomotor (III), the trochlear (IV), and the opthalamic branch of the trigeminal nerve (V1) and the abducens nerve (VI).
Inflammation
Inflammation caused by an infection may impair the operation of any of the cranial nerves. Infection of the facial nerve (VII), for instance, can result in Bell’s palsy. Multiple sclerosis, an inflammatory process which can produce a loss of the myelin sheathes that encircle the cranial nerves, may cause a variety of shifting signs and symptoms which can ultimately affect multiple cranial nerves.
Other
Trauma to the skull, bone disease like Paget’s disease, and damage or injury to the cranial nerves through neurosurgery, by way of instance, through tumor removal, are other potential causes of cranial nerve health issues.

Dr. Alex Jimenez’s Insight
There are 12 pairs of cranial nerves which exit the brain, one in each side. These cranial nerves are named and numbered (I-XII) according to their location in the brain as well as their specific function in the body. Common conditions, such as multiple sclerosis, may affect one or more of the cranial nerves, resulting in dysfunction of the specific regions innervated by them. Signs and symptoms associated with health issues affecting specific cranial nerves can help healthcare professionals determine the source of the problem. Testing the cranial nerves involves a number of steps in order to be certain which function of the human body has been ultimately affected.
Clinical Significance of the Cranial Nerves
Most commonly, humans are believed to have twelve pairs of cranial nerves which have been assigned Roman numerals I-XII for identification. The numbering of the cranial nerves is based on the order in which they emerge from the brain, or from the front to the back of the brainstem. These include: the olfactory nerve (I), the optic nerve (II), the oculomotor nerve (III), the trochlear nerve (IV), the trigeminal nerve (V), the abducens nerve (VI), the facial nerve (VII), the vestibulocochlear nerve (VIII), the glossopharyngeal nerve (IX), the vagus nerve (X), the accessory nerve (XI), and the hypoglossal nerve (XII). Below we will narrow down the clinical significance of the cranial nerves.
Olfactory Nerve (I)
The olfactory nerve (I) communicates the sensation of smell to the brain. Lesions resulting in anosmia, or loss of the sense of smell, have been previously described to occur through trauma, damage or injury to the head, especially in the instance that a patient hits the back of their head. In addition, frontal lobe masses, tumors, and SOL have also been associated with the loss of the sense of smell. Healthcare professionals have previously identified that the loss of the sense of smell is one of the first symptoms seen in Alzheimer’s and early dementia patients.
Healthcare professionals may test the function of the olfactory nerve (I) by having the patient close their eyes and cover one nostril at a time in order to have them breathe out through their nose while placing a scent under the nostril and having them breathe in. The doctor will ask the patient, “do you smell anything?”, and record the findings. This tests whether the nerve is operating appropriately. If the patient says yes, the doctor will then ask the patient to identify the scent. This tests whether the processing pathway, known as the temporal lobe, is functioning accordingly.
Optic Nerve (II)
The optic nerve (I) communicates visual information to the retina. Lesions to this cranial nerve can be the result of CNS disease, such as MS, or CNS tumors and SOL. Most health issues associated with the visual system emerge from direct trauma, metabolic or vascular diseases. FOV lost in the periphery can also indicate that SOL may be affecting the optic chiasm, including a pituitary tumor.
A healthcare professional will often test the function of the optic nerve (II) by asking whether the patient can see. If the patient describes having vision in each eye, the optic nerve is functional. Doctors may also perform visual acuity testing using the Snellen chart, first one eye at a time, then the two eyes together, or they may perform distance vision testing. Near vision testing will often involve the Rosenbaum chart, first one eye at a time, then the two eyes together. Additional associated testing for the visual system can include, the ophthalmoscopic or funduscopic exam, which assess the A/V ratio and vein/artery health as well as assess cup to disc ratio of the visual system. Other testing methods include field of vision testing, intraoccular pressure testing and the iris shadow test.
Oculomotor Nerve (III), Trochlear Nerve (IV), and Abducens Nerve (VI)
The oculomotor nerve (III), the trochlear nerve (IV), the abducens nerve (VI) and the ophthalmic division of the trigeminal nerve (V1) travel through the cavernous sinus to the superior orbital fissure, passing out of the skull into the orbit. These cranial nerves control the tiny muscles that move the eye and also offer sensory innervation to the eye and orbit.
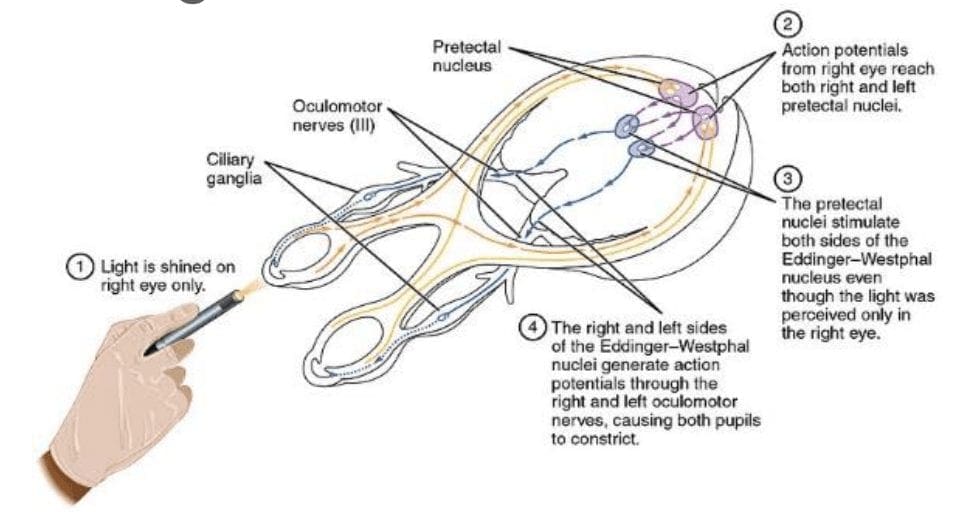
The clinical significance of the oculomotor nerve (III) includes diplopia, lateral strabismus (unopposed lateral rectus m.), head rotation away from the side of the lesion, a dilated pupil (unopposed dilator pupillae m.), and ptosis of the eyelid (loss of function of the levator palpebrae superioris m.). Lesions to the oculomotor nerve (III) can occur due to inflammatory diseases, such as syphilitic and tuberculous meningitis, aneurysms of the posterior cerebral or superior cebellar aa., and SOL in the cavernous sinus or displacing the cerebral peduncle to the opposite side. Testing this cranial nerve is performed by moving a light in front of the patient’s pupil from the lateral side and hold for 6 seconds. The doctor should watch for direct (ispilateral eye) and consensual (contralateral eye) pupillary constriction in order to distinguish dysfunction of the oculomotor nerve (III).
The clinical significance of the trochlear nerve (IV) is characterized where the patient presents diplopia and difficulty while maintaining a downward gaze, often complaining of having difficulties when walking down stairs, resulting in more frequent tripping and/or falling, followed by extortion of the affected eye (unopposed inferior oblique m.) and a head tilt to the unaffected side. Lesions to the trochlear nerve (IV) can commonly be the result of inflammatory diseases, aneurysms of the posterior cerebral or superior cerebellar aa., SOL in the cavernous sinus or superior orbital fissure and surgical damage during mesencephalon procedures. Head tilts in superior oblique palsy (CN IV failure) may also be identified.
The clinical significance of the abducens nerve (VI) includes diplopia, medial strabismus (unopposed medial rectus m.), and head rotation towards the side of the lesion. Lesions to this cranial nerve can be the result of aneurysms of the posterior inferior cerebellar or basilar aa., SOL in the cavernous sinus or 4th ventricle, such as a cerebellar tumor, fractures of the posterior cranial fossa, and increased intracranial pressure. Testing this cranial nerve is performed through the H-Pattern testing, where the healthcare professional will have the patient follow an object no bigger than 2 inches. It’s essential for the doctor to follow these specific guidelines as patient’s can have difficulties focusing on items that are too large, and it’s also important for the doctor not to hold the object too close to the patient. Convergence and accommodation testing is performed by bringing the object close to the bridge of the patient’s nose and back out at least 2 times. The physician must look for pupillary constriction response as well as convergence of the eyes.
Trigeminal Nerve (V)
The trigeminal nerve (V) is made up of three different parts: The . When put together, these nerves provide sensation to the skin of the face and also controls the muscles of mastication, or chewing. Cranial nerve dysfunction along any of the separate sections of the trigeminal nerve (V) can manifest as decreased bite strength on the ipsilateral side of the lesion, loss of sensation along the distribution of V1, V2, and V3, and loss of corneal reflex. Lesions to the trigeminal nerve (V) can be the result of aneurysms or SOL affecting the pons, particularly tumors at the cerebellopontine angle, skull fractures on the facial bones or damage to the foramen ovale, and Tic doloureux, most frequently referred to as trigeminal neuralgia, characterized by sharp pain along the distributions of the different parts of the trigeminal nerve (V). Physicians may utilize analgesic, anti-inflammatory or contralateral stimulation to control the signs and symptoms.
Testing the trigeminal nerve (V) includes pain & light touch testing along the ophthalmic (V1), the maxillary (V2), as well as the Mandibular (V3) nerves of the cranial nerve.�Testing is best done toward the more medial or proximal areas of
the face, where the V1, the V2 and the V3 are better delineated. A healthcare professional may also assess dysfunction along this cranial nerve using the blink/corneal reflex testing, performed by puffing air or doing a small tissue tap from the lateral side of the eye on the cornea. If normal, the patient blinks. The CN V provides the sensory (afferent) arc of this reflex. Bite strength may also be tested by having the patient bite down on a tongue depressor while the doctor tries to remove it. The jaw jerk/Masseter reflex may also be performed with the patient�s mouth slightly open, by placing the thumb on a patient�s chin and tapping the own thumb with a reflex hammer. Strong closure of the mouth indicates UMN lesion. CN V provides both the motor and sensory of this reflex.
Facial Nerve (VII) and Vestibulocochlear Nerve (VIII)
The facial nerve (VII) and the vestibulocochlear nerve (VIII) both input the inner auditory canal in the temporal bone. The facial nerve subsequently extends to the side of the face then distributes to control and reach all of the muscles in charge of facial expressions. The vestibulocochlear nerve reaches the organs which control equilibrium and hearing in the temporal bone.
As with all cranial nerves, signs and symptoms along the facial nerve (VII) describe the location of the lesion. Lesion in the lingual nerve will manifest as loss of taste, general sensation in the tongue and salivary secretion. Lesion proximal to the branching of the chorda tympani, such as in the facial canal, will result in the same signs and symptoms, without the loss of general sensation of the tongue, partly due because the V3 has not yet joined the facial nerve (VII). Corticobulbar innervation is asymmetric to the upper and lower parts of the facial motor nucleus. In the instance of an UMN lesion, or a lesion to the corticobulbar fibers, the patient will experience paralysis of the muscles in charge of facial expression in the contralateral lower quadrant. If there is an LMN lesion, or a lesion to the facial nerve itself, the patient will experience paralysis of the muscles of facial expression in the ipsilateral half of the face, otherwise known as Bell’s palsy.
A healthcare professional will test the facial nerve (VII) initially by asking the patient to mimic or follow specific instructions to make certain facial expressions. The doctor should make sure to evaluate all four quadrants of the face by asking the patient to raise their eyebrows, puff their cheeks, smile and then close their eyes tightly. Subsequently, the doctor will test the facial nerve (VII) by checking the strength of the buccinator muscle against resistance. The healthcare professional will achieve this by asking the patient to hold air in their cheeks as they press gently from the outside. The patient should be able to hold air in against the resistance.
Signs and symptoms of dysfunction in the vestibulocochlear nerve (VIII) often involve changes in hearing alone, most commonly as a result of infections in the otitis media and/or as a result of skull fractures. The most common lesion to this nerve is caused by an acoustic neuroma which affects the CN VII and the CN VIII, particularly the cochlear and vestibular divisions, as a result of proximity in the internal auditory meatus. Signs and symptoms of the health issue include nausea, vomiting, dizziness, hearing loss, tinnitus, and Bell’s palsy, etc.
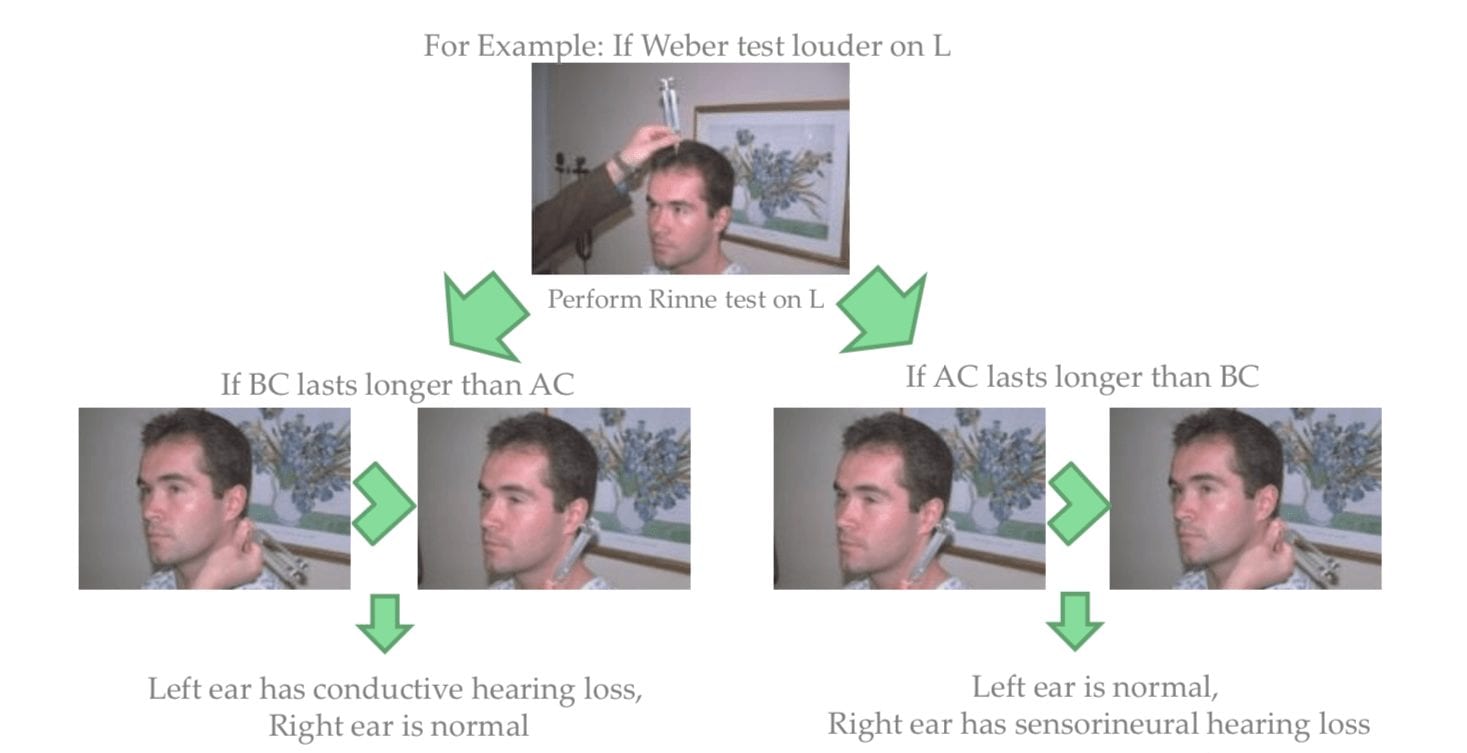
Testing the vestibulocochlear nerve (VIII) for dysfunction commonly involves an otoscopic exam, the scratch test, which determines whether a patient can hear equally on both sides, the Weber test, tests for lateralization, a 256 Hz tuning fork placed on top of the patient�s head in the center, which can help point out whether a patient hears it louder on one side than the other, and finally the Rinne test, which compares air conduction to bone conduction. Normally, air conduction should last twice as long as bone conduction.
Glossopharyngeal Nerve (IX), Vagus Nerve (X) and Accessory Nerve (XI)
The glossopharyngeal (IX), the vagus nerve (X) and the accessory nerve (XI) all emerge from the skull to enter the neck. The glossopharyngeal nerve (IX) provides innervation to the upper throat and the back of the tongue, the vagus nerve (X) offers innervation to the muscles at the voicebox, and proceeds down to provide parasympathetic innervation to the chest and abdomen. The accessory nerve (XI) controls the trapezius and sternocleidomastoid muscles at the neck and shoulder.
The glossopharyngeal nerve (IX) is rarely damaged alone, due to it�s proximity to the CN X and XI. A healthcare professional should perform a test to look for signs of CN X & XI damage as well if CN IX involvement is suspected.
Patients with clinical signs and symptoms caused by vagus nerve (X) dysfunction may experience dysarthria, or difficulty speaking clearly, as well as dysphagia, or difficulty swallowing. These may present as food or liquid coming out of their nose or frequent chocking or coughing when eating and/or drinking. Further clinical presentations include hyperactivity of a visceral motor component, leading to the hypersecretion of gastric acid and resulting in ulcers. Hyper-stimulation of the general sensory component can cause coughing, fainting, vomiting and reflex visceral motor activity. The visceral sensory component of this nerve only provides general feelings of un-wellness but visceral pain may transfer on to the sympathetic nerves.
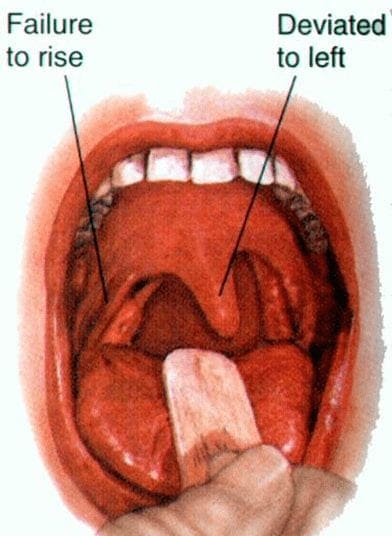
Testing for the glossopharyngeal nerve (IX) and the vagus nerve (X) can include the gag reflex, where the�CN IX provides the afferent (sensory) arc and the�CN X provides the efferent (motor) arc. Approximately 20 percent�of patients have a minimal or absent gag reflex. Other tests may include wwallowing, gargling, etc., as it requires CN X function. Healthcare professionals may also test palatal elevation because it requires CN X function. Furthermore, the doctor will see whether the palate elevates and uvula deviates
contralateral to damaged side. Finally, the healthcare professional will test the auscultation of the heart, since the R CN X innervates SA node (more rate regulation) and the L CN X the AV node (more rhythm regulation).
Lesions in the accessory nerve (XI)�may occur due to radical surgeries in the neck area, such as the removal of the laryngeal carcinomas. Testing for the accessory nerve (XI) may include the strength test SCM m. Patients with clinical signs and symptoms due to lesions in the accessory nerve (XI) will experience difficulties turning their head against the resistance of a healthcare professional, particularly toward the side opposite of the lesion. Testing for the accessory nerve (XI) may also include the strength test trapezius m. Patients with clinical signs and symptoms due to lesions in the accessory nerve (XI) will experience difficulties with shoulder elevation on the side of the lesion.
Hypoglossal Nerve (XII)
The hypoglossal nerve (XII) originates from the skull to reach the tongue in order to control essentially all of the muscles involved in the movements of the tongue. The clinical significance of health issues associated to the hypoglossal nerve (XII) can manifest as a deviating tongue towards the side of an inactive genioglossus m. upon tongue protrusion. This may often be contralateral to a corticobulbar, or UMN, lesion or from an ipsilateral to a hypoglossal n., or LMN, lesion.
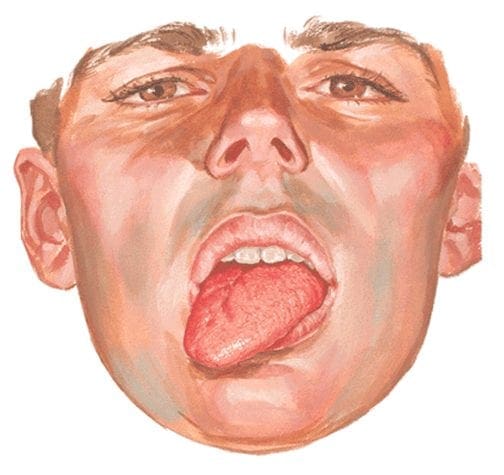
Testing for the hypoglossal nerve (XII) involves the healthcare professional asking a patient to stick out their tongue. The doctor will look for any deviation which may signal a health issue along the length of the hypoglossal nerve (XII). Another test the doctor may perform as a part of the evaluation may include the physician asking the patient to place their tongue inside their cheek and apply light resistance, one side at a time. The patient should be able to resist moving their tongue with pressure.
Clinical Examination of Cranial nerves I-VI
Clinical Examination of Cranial nerves VII-XII
The clinical significance of the signs and symptoms which manifest as a result of cranial nerve dysfunction are essential in order for the healthcare professional to properly diagnose the patient’s specific health issue. The clinical findings described above are often unique to the affected cranial nerve and the tests and evaluations for each can help confirm a diagnosis. Proper diagnosis is fundamental in order for the doctor to continue with the patient’s appropriate treatment. The scope of our information is limited to chiropractic as well as to spinal injuries and conditions. To discuss the subject matter, please feel free to ask Dr. Jimenez or contact us at 915-850-0900 .
Curated by Dr. Alex Jimenez
Additional Topics: Sciatica
Sciatica is medically referred to as a collection of symptoms, rather than a single injury and/or condition. Symptoms of sciatic nerve pain, or sciatica, can vary in frequency and intensity, however, it is most commonly described as a sudden, sharp (knife-like) or electrical pain that radiates from the low back down the buttocks, hips, thighs and legs into the foot. Other symptoms of sciatica may include, tingling or burning sensations, numbness and weakness along the length of the sciatic nerve. Sciatica most frequently affects individuals between the ages of 30 and 50 years. It may often develop as a result of the degeneration of the spine due to age, however, the compression and irritation of the sciatic nerve caused by a bulging or herniated disc, among other spinal health issues, may also cause sciatic nerve pain.

EXTRA IMPORTANT TOPIC: Chiropractor Sciatica Symptoms
MORE TOPICS: EXTRA EXTRA: El Paso Back Clinic | Back Pain Care & Treatments
General Disclaimer, Licenses and Board Certifications *
Professional Scope of Practice *
The information herein on "Testing the Function of the Cranial Nerves in El Paso, TX" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and on our family practice-based chiromed.com site, focusing on naturally restoring health for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez, DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card









