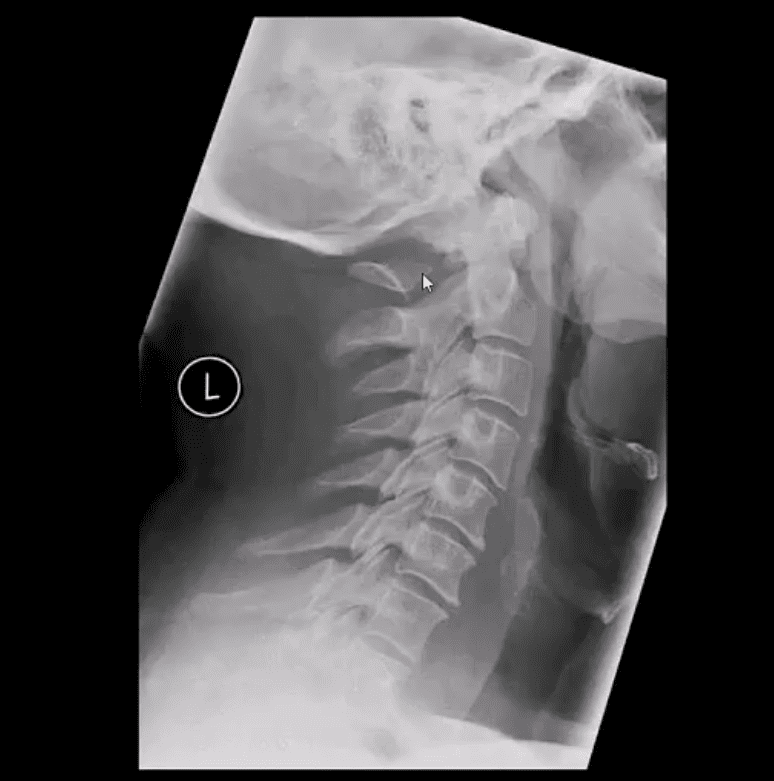
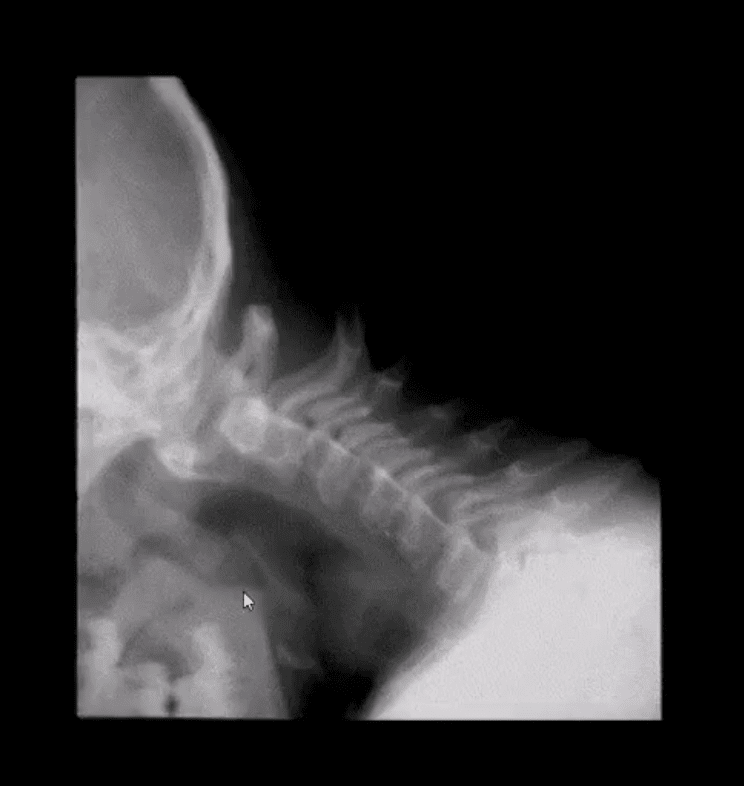
Hyperextension Injury
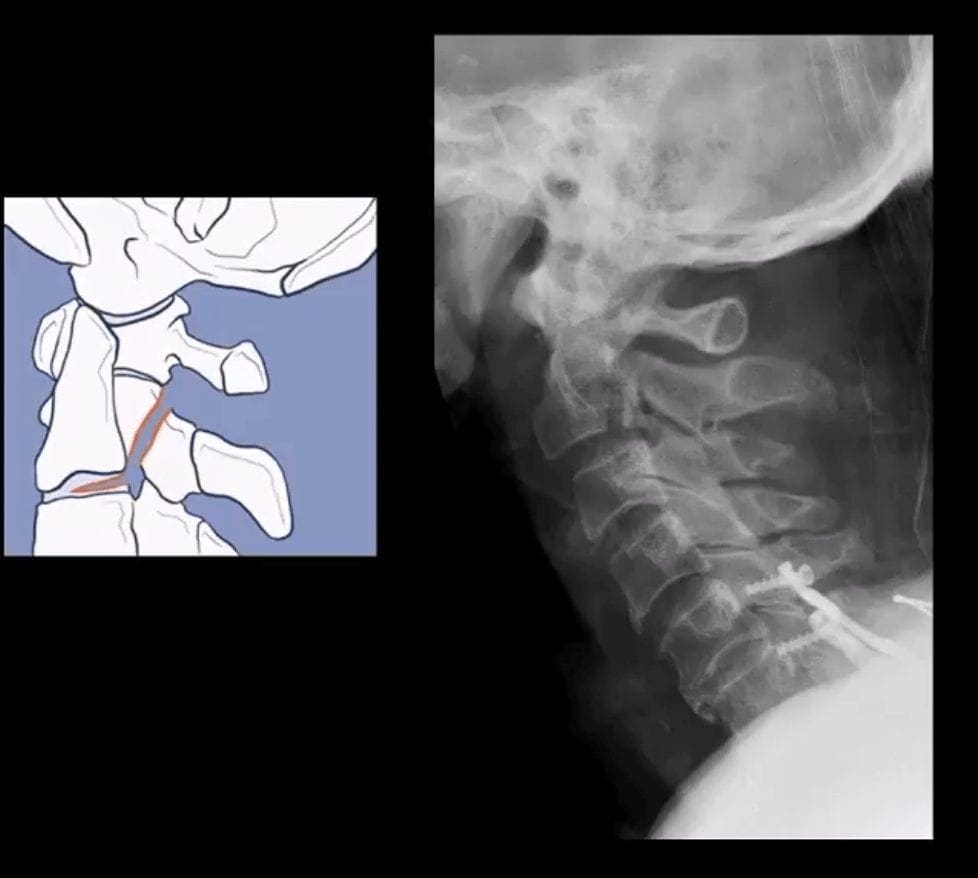
- Hangman’s Fx aka traumatic spondylolisthesis of C2 with a fracture of pars interarticularis or pedicles (unstable)
- MVA is the most common cause
- Mechanism: acute hyperextension of upper C/S similar to judicial hanging (never actually seen and most deaths are due to asphyxiation)
- Secondary flexion may tear PLL and disc
- Associated injuries: 30% have other c-spine fx especially Extension teardrop at C2 or C3 due to avulsion by ALL
- Cord paralysis may only present in 25% due to bony fragments dissociation and canal widening
- Hangman fx and extension teardrop
- Cervical degeneration and previous fusion is a key predisposing factor due to the lack of mobility and suppleness, rendering C/S easy to fracture
- Imaging: initial x-radiography then CT that helps to delineate another injury such as facet/pedicle Fx further. MRI may help if complicated by Vertebral A. damage
- Management: if type 1 injury then closed reduction and rigid collar for 4-6 weeks, halo bracing if type 2 (>3-5mm displacement) Fx/instability, anterior or posterior spinal fusion at C2-3 if type 3 Fx (>5-mm displacement)
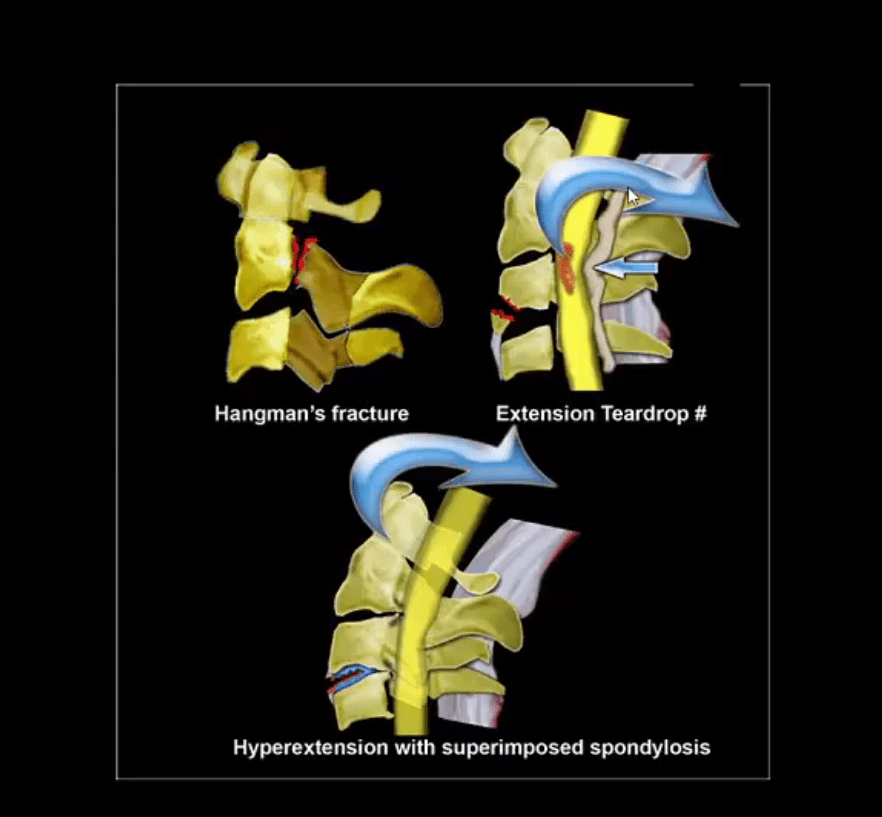
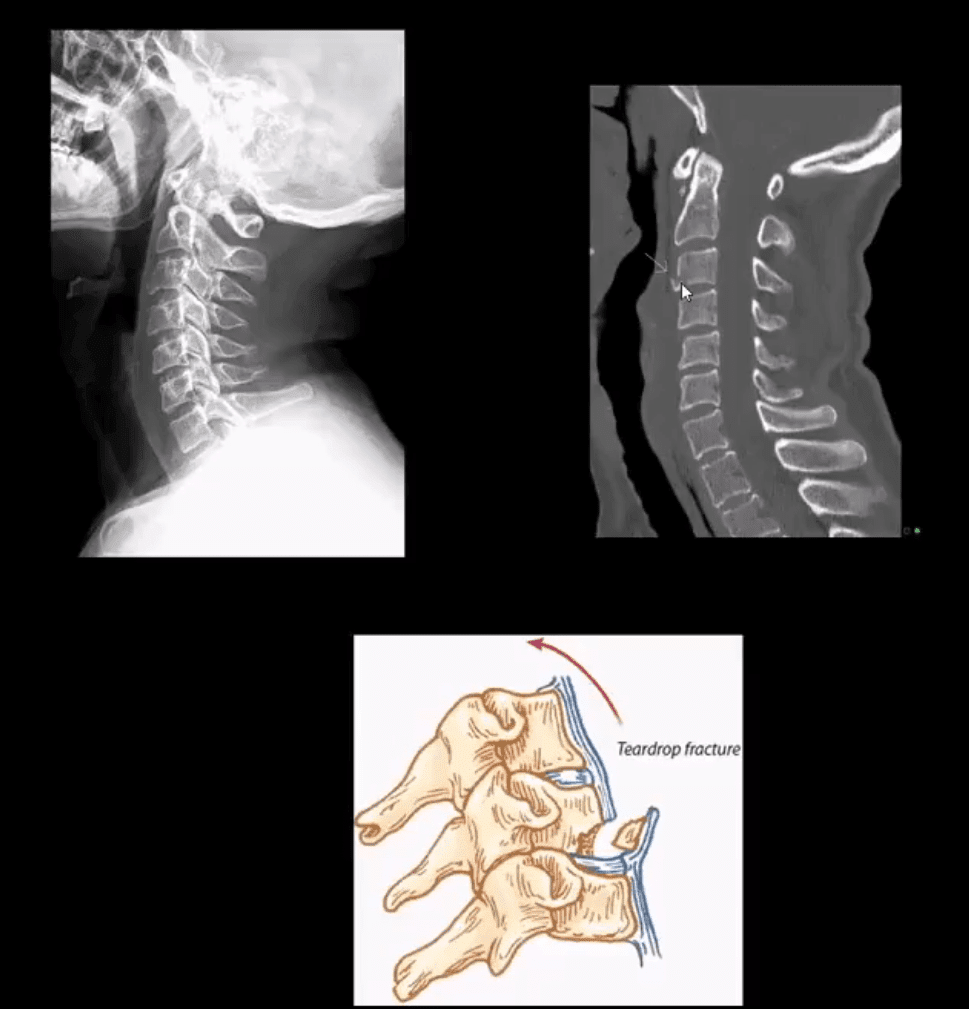
- Extension teardrop Fx (stable) potentially unstable if put in extension
- Avulsion of an inferior anterior body by ALL. More seen in elderly with superimposed C/S spondylosis
- Key radiography: a smaller anterior-inferior body corner, no disruption of ligamentous alignment. Typically at C2 or C3 due to sudden hyperextension and ALL avulsion
- Complication: central cord syndrome (m/c incomplete cord injury) esp. in superimposed spondylosis and canal stenosis by the laxity of ligamentum flavum and osteophytes
- Management: hard collar isolation
Contents
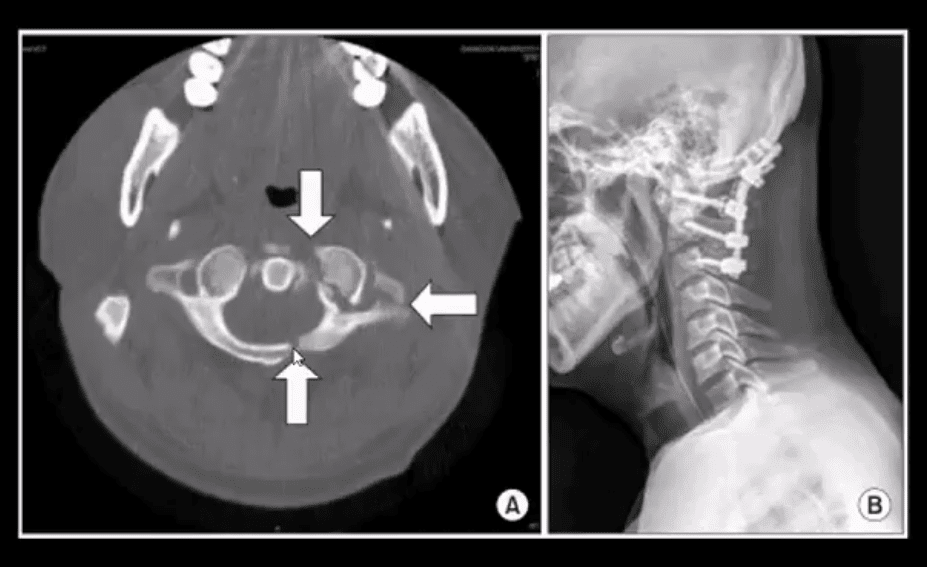
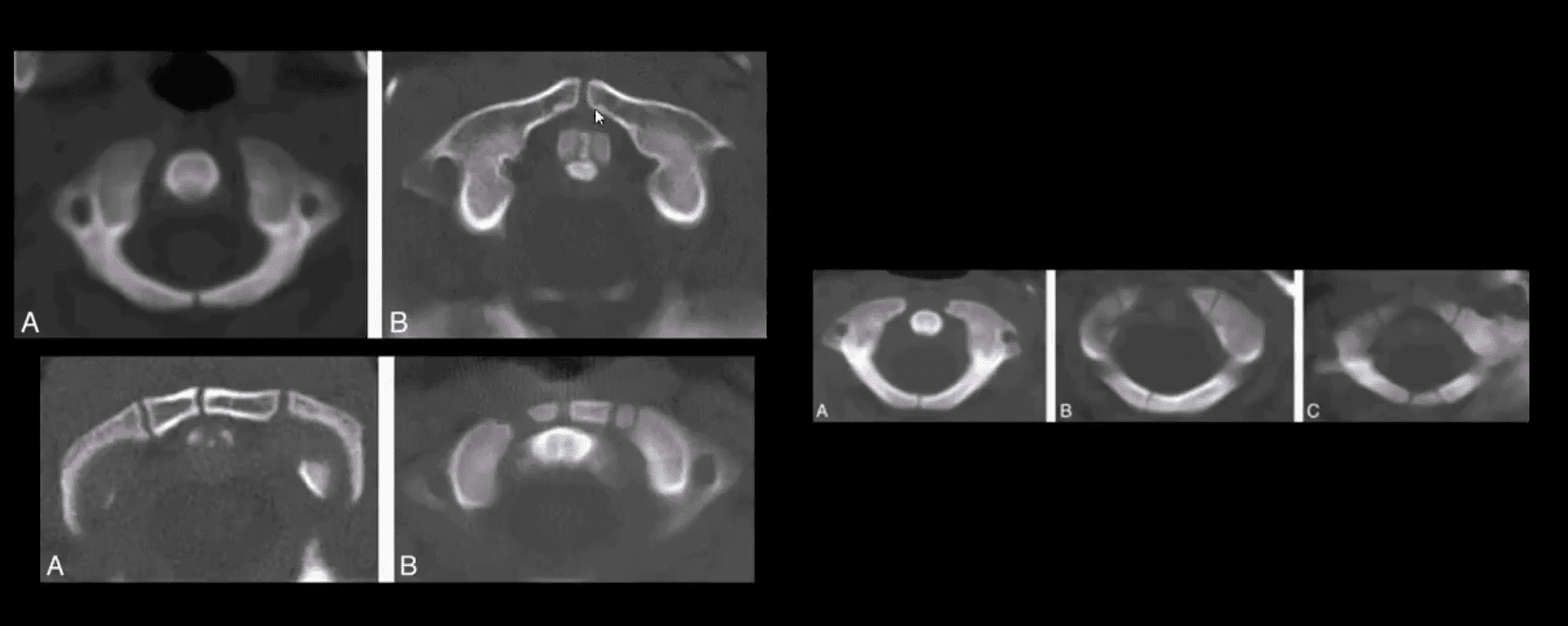
Vertical (axial) Compression Injury
- Jefferson Fx (named after British neurosurgeon who defined it) (unstable but neurologically intact Fx) 7% of all C/S injuries. Stability is dependent if the transverse ligament is intact or torn, which can be noted by overhanging of C1 lateral masses over C2 >5-mm combined (left image)
- Mechanism: C1 compression (e.g., diving into shallow waters) causing burst Fx-classically 4-parts of the anterior and posterior arch of C1. Variations exist.
- Complications: 50% show other C/S Fx, 40% show Odontoid C2 Fx esp. if extension and axial loading occur
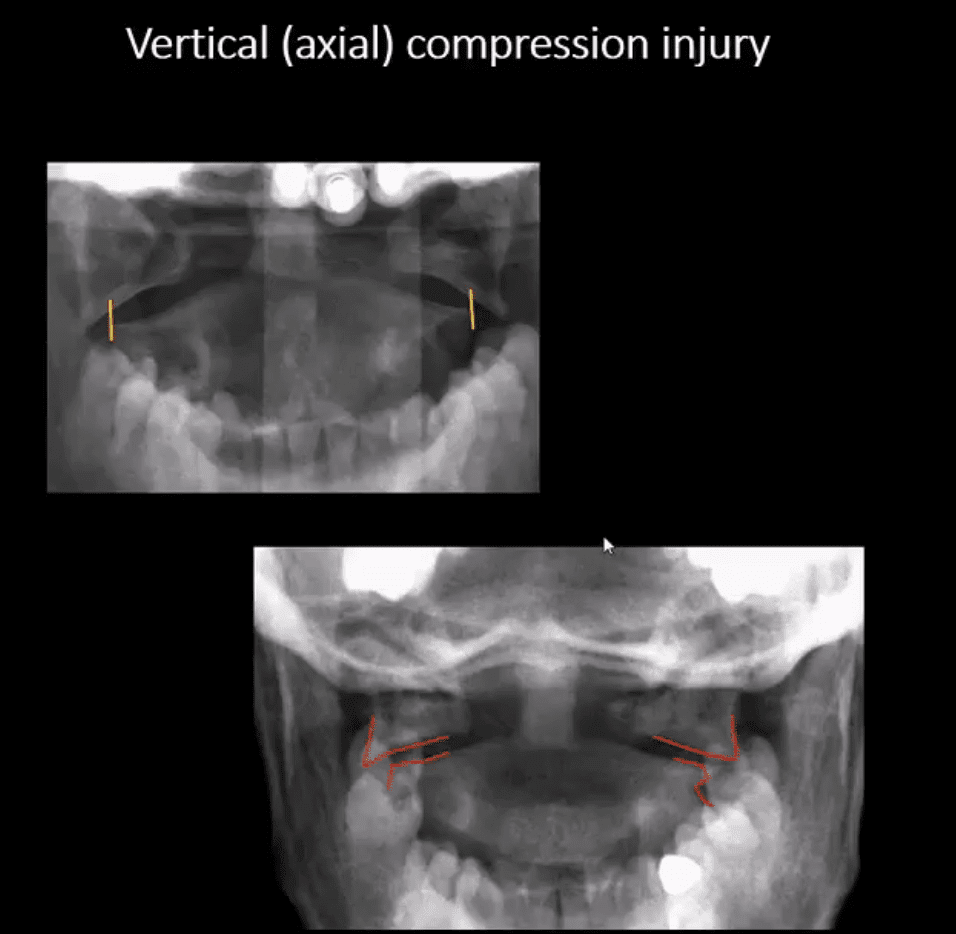
- Imaging: x-radiography followed by CT scanning to evaluate subaxial injury and complexity of C1 injury. Note Jefferson Fx with pillar and transverse foramina fx requiring posterior occipital-cervical fusion (below right image).
- Management: rigid collar immobilization if the transverse ligament is intact. Halo brace or fusion if the transverse ligament is ruptured
Cervical Injuries With Variable Mechanisms of Trauma
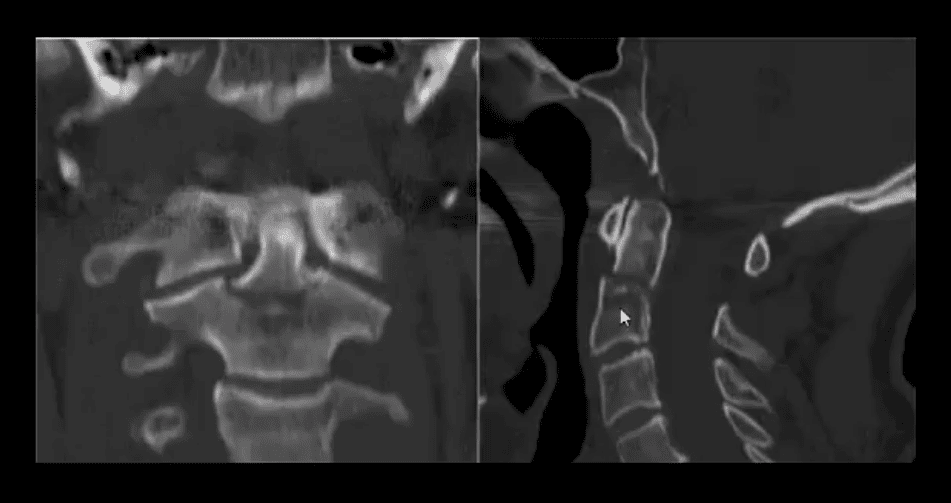
- Odontoid process fractures:
- These occur�with a variety of mechanisms, flexion, extension, lateral flexion. Elderly with superimposed spondylosis are at higher risk.
- Anderson & D’Alonzo classification (below). Type 2 is the most common and most unstable. Type 3 has the best chance of healing d/t more massive bleed into C2 body and better healing potential.
- Imaging: x-radiography can miss some Fx. CT scanning is essential.
- On x-radiography note tilting of the Dens on lateral and APOM views. CT will reveal the injury and classify it.
- Complications: cord injury, non-union
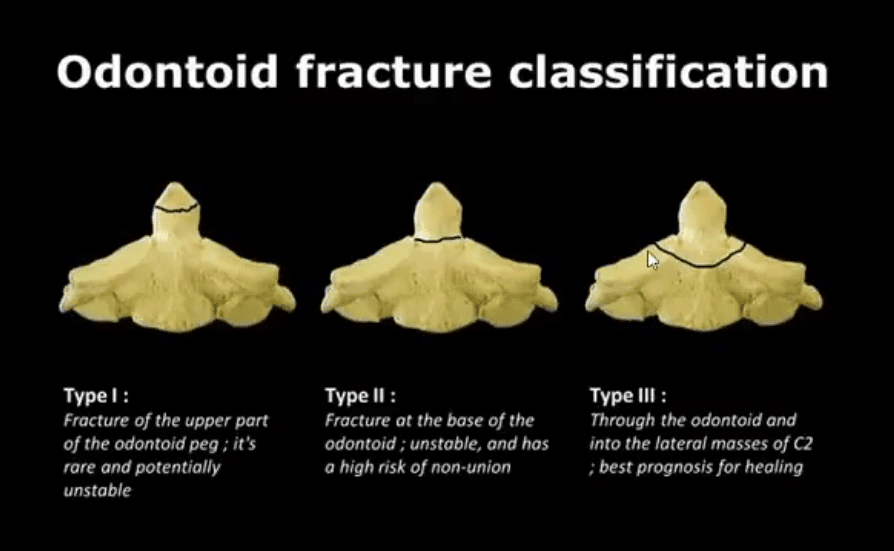
- CT scanning: type 2 odontoid fracture (unstable)
- Management: type 1 (alar ligament avulsion) most stable�observed and treated with rigid collar.
- In young patients, Halo brace is used to treat type 2
- Older patients do not tolerate Halo
- Operative C1-2 fusion if unstable is Dx and cord signs or other complicating factors are present
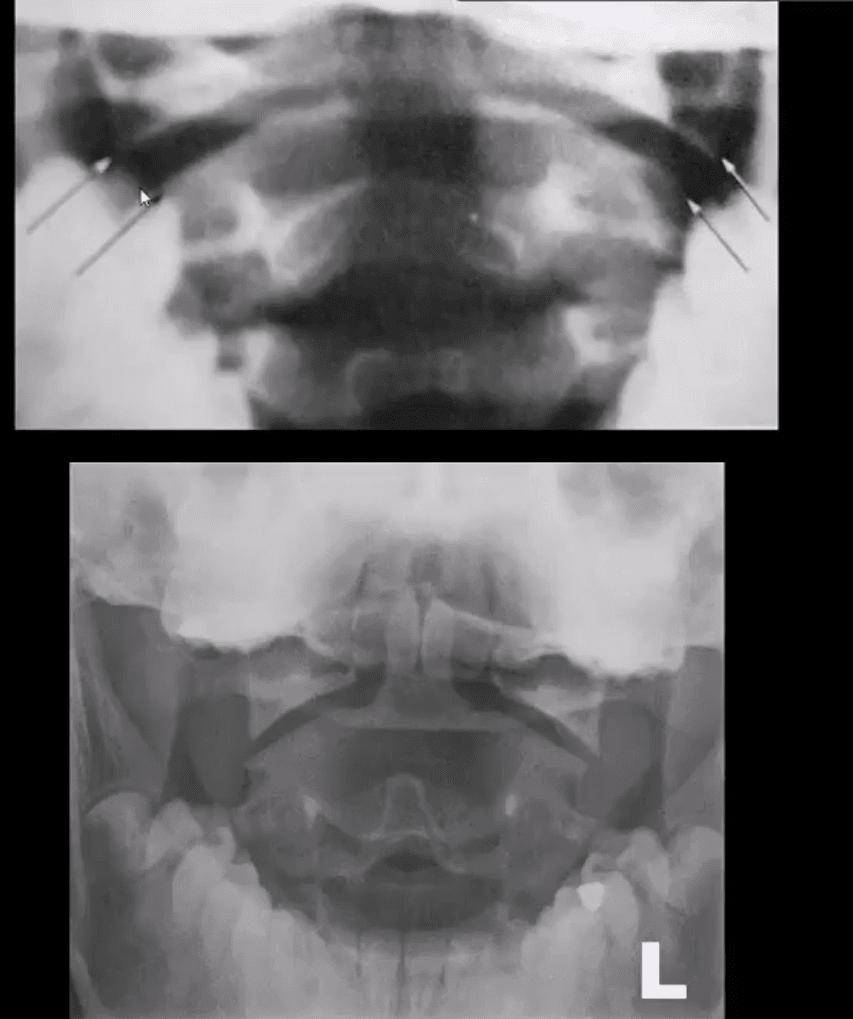
Normal Radiographic Variants & Anomalies Simulating Pathology
- Pediatric spine appears different especially in children younger than 10-years old.
- Normal variations; ADI 5-mm and may increase or decrease on flexed/extended views by 1-2-mm
- C2-3 may appear as pseudo-subluxation due to normal ligamentous laxity in children (below arrow)
- Pediatric vertebral bodies usually are narrower and anteriorly wedged due to the presence of cartilaginous tissue
- APOM view appears different in children, and some asymmetry of C1 articular masses is normal (below top image) and should not be confused with Jefferson Fx
- In adults, any asymmetry or “overhanging” of C1 articular masses is pathological and may indicate Jefferson fx
- Standard ossification centers of the Atlas synchondrosis in children should not be mistaken for fractures
- Persistent ossiculum terminal of Bergman is a typical variant/anomaly of tenacious un-united ossification center and should not be confused with type odontoid fx
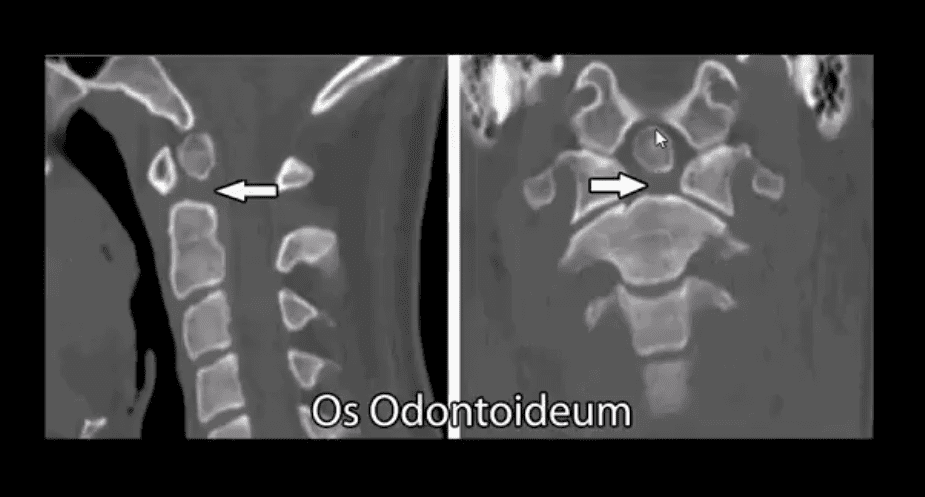
- Os odontoideum
- Un-united growth center that currently considered as an un-noticed injury that disturbed normal growth in a child younger than 5-years-old
- It may be a cause of C1-2 instability and should be evaluated with flexed and extended cervical views
- Should not be confused with type 2 Dens fracture because it typically more demonstrates greater mineralization of bone
- Incomplete bilateral agenesis of the C1 posterior arch
- Anomalous closure of C1 posterior arch
- Should not be confused with a fracture
- However, local or cord symptoms may develop after trauma in some cases
- Relatively rare anomaly developing due to failed chondrogenesis and ossification of posterior ossification centers of the Atlas
- Patients with Down syndrome may suffer from increased ligamentous laxity and other abnormalities
- Increased risk of subluxation at C1-2
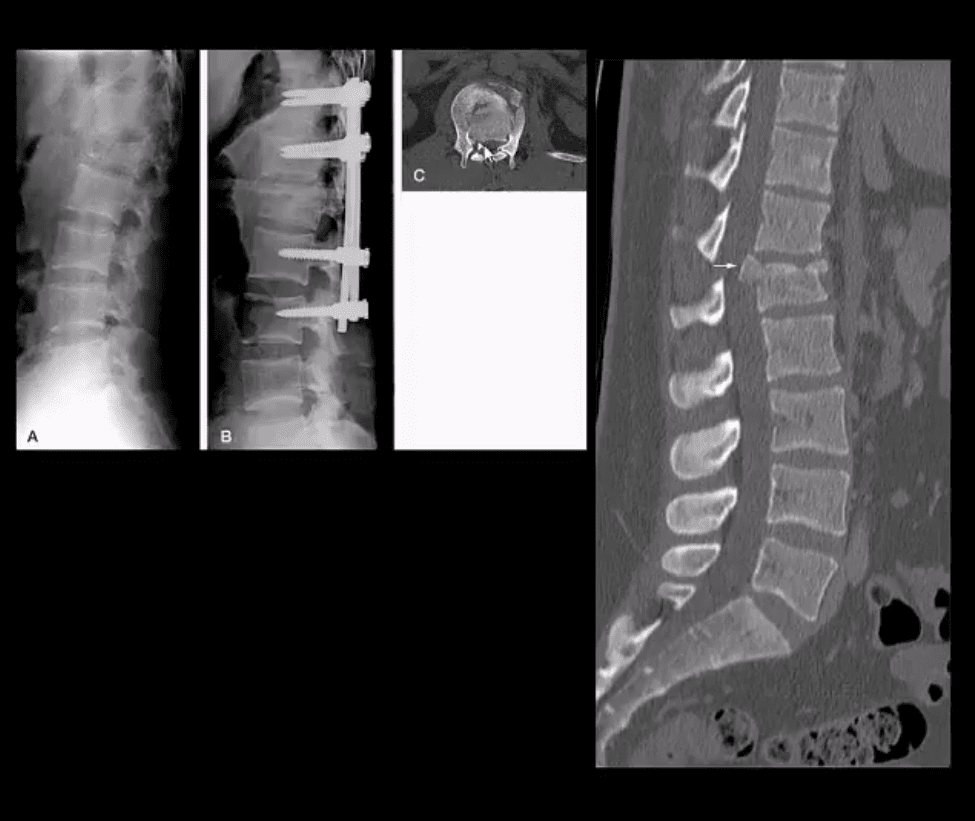
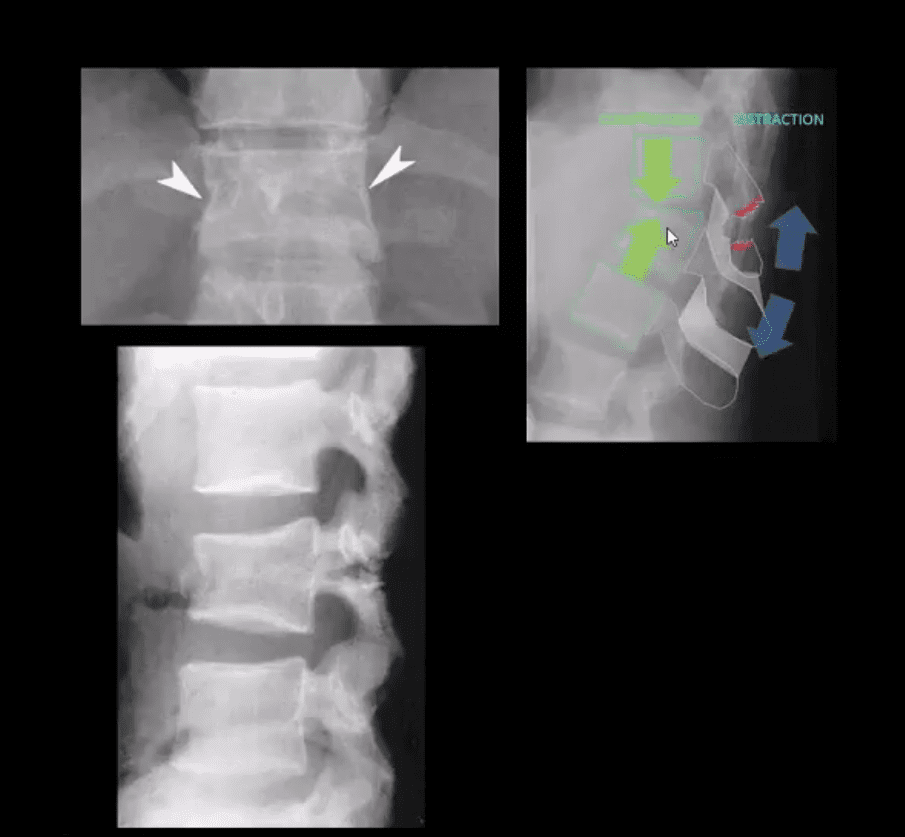
- Burst Fx (unstable) 2-columns are damaged
- Mechanism: axial loading with frequent flexion after falls and MVAs
- The thoracolumbar region is the most vulnerable due to the increased fulcrum of motion
- Key radiography: acute compression fracture and�collapse of body height, retropulsion of posterior body and acute kyphotic deformity on the lateral view
- On the frontal view: interpedicular widening (below yellow arrow), regional soft tissue swelling (below green arrow)
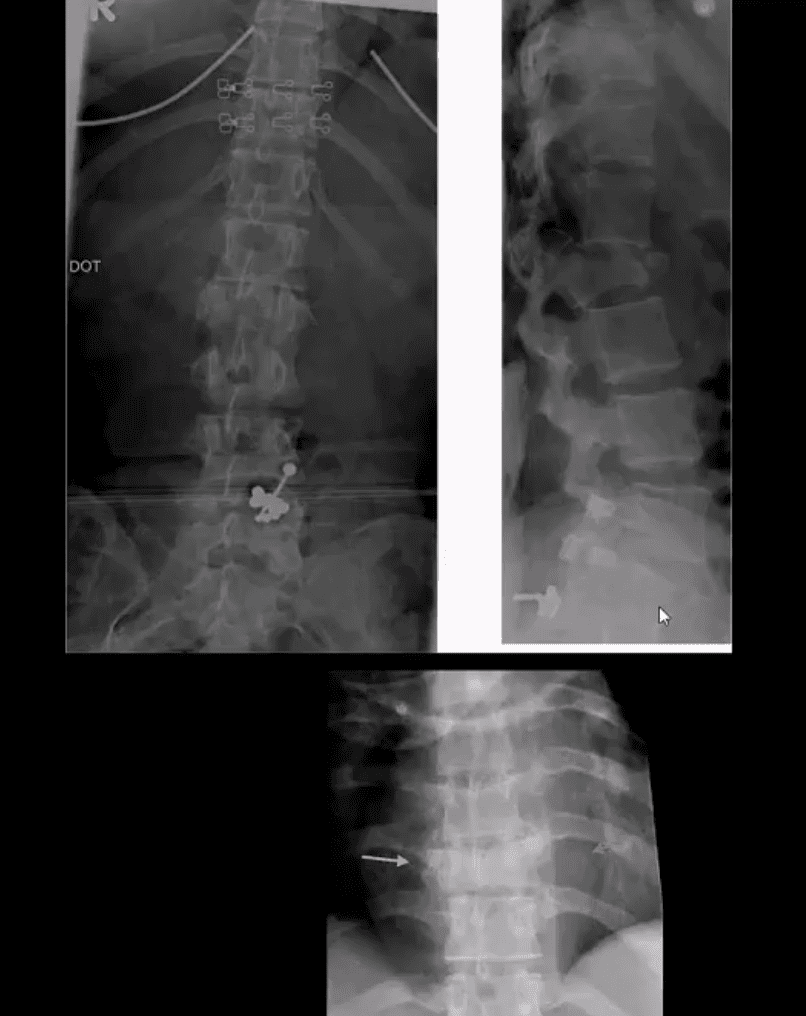
- Imaging: x-radiography should be followed by CT scanning w/o contrast
- MRI if neurologically unstable due to cord or conus injury
- Complications: cord damage by acutely retropulsed bone fragments
- Management: non-operative if neurologically intact and <50% body retropulsed with minimal kyphosis
- Operative (fusion) if 50% or more body retropulsed, laminar/pedicle Fx, neuro compromised
18-Year Old Female Following Trampoline Accident
- AP & lateral L/S views
- Note acute compression fracture, a vertebral body extending to posterior elements
- Widening of the inter-spinous distance between T11-T12 (below arrow)
- Radiolucent fracture line is seen through the T12 body on the AP projection
- CT scanning was performed
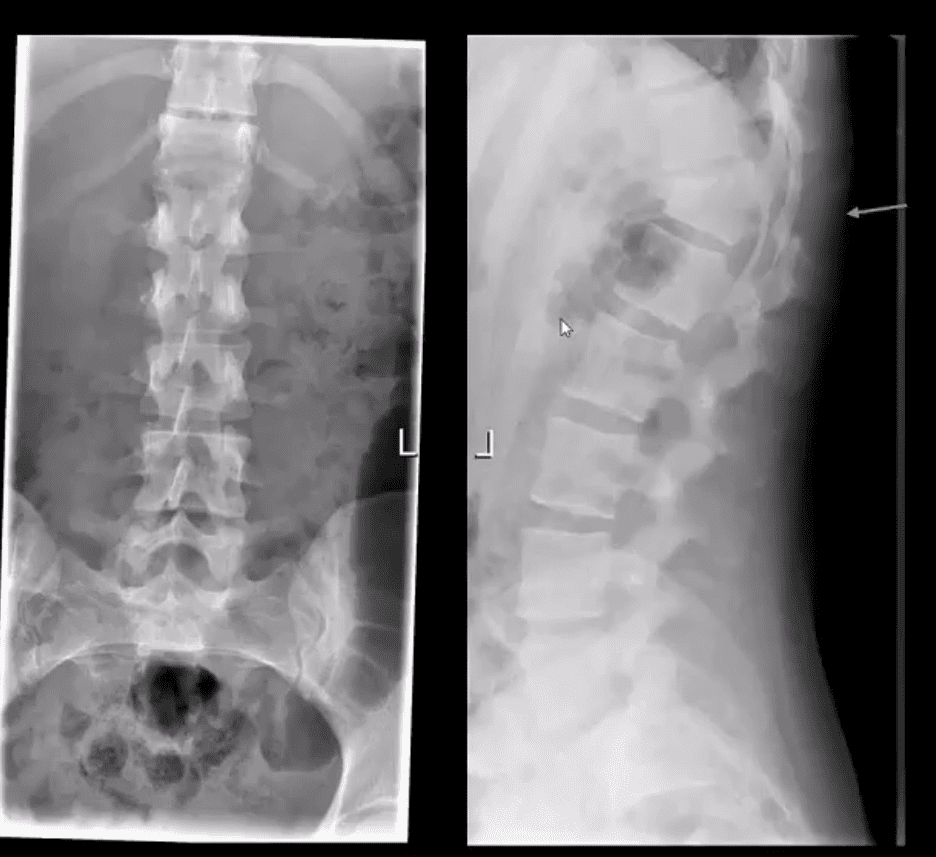
- Sagittal reconstructed Thoracic and Lumbar CT slices in bone window
- Note acute compression fracture, the T12 body extending into pedicle and lamin
- Dx: Chance fracture of T12
- MR imaging was performed

- T2 Wl sagittal MRI
- Findings: acute compression fracture T12 body extending to posterior elements causing rapture of interspinous and flavum ligaments
- Mild compression of the distal cord above the conus is noted with a minimal signal abnormality
- Dx: Chance fracture
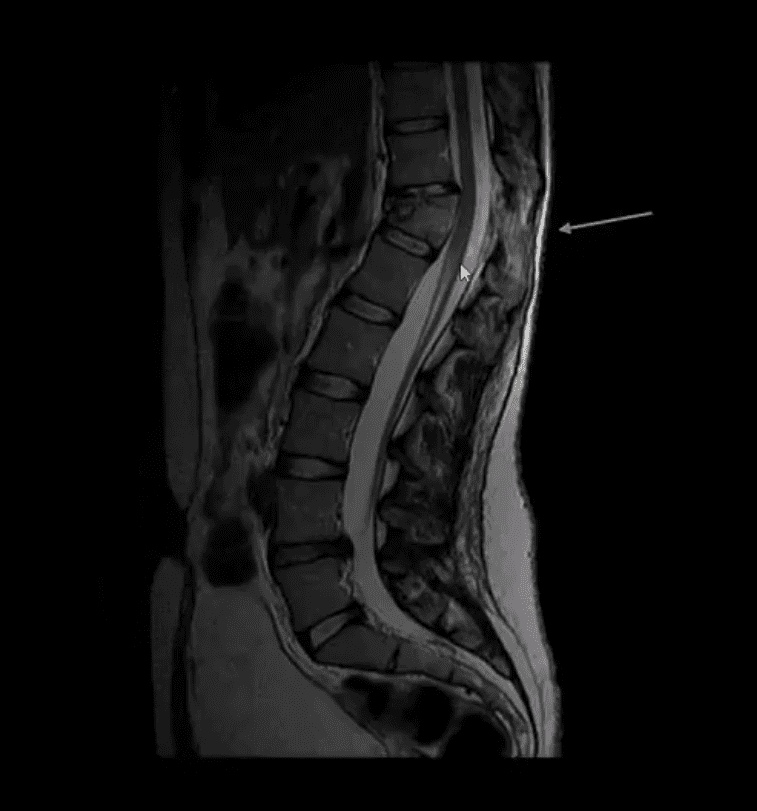
- Chance Fx aka (Seatbelt Fx) – is a flexion-distraction injury (unstable)
- M/C in lower thoracic-upper lumbar
- All 3-columns fail: column 3 torn by distraction, columns 1 and 2 fail on compression (Denis classification)
- Causes: MVA, falls
- Imaging: initial x-radiography should be followed by CT scanning w/o contrast to assess bone fragments retropulsion/canal compression. MRI may help to evaluate potential cord damage and ligaments tearing
- Management: non-operative immobilization if neuro intact
- Operative decompression and fusion
Spinal Trauma Imaging Approach
Resources:
- https://emedicine.medscape.com/article/824380-overview
- https://emedicine.medscape.com/article/248236-overview#a9
- https://emedicine.medscape.com/article/397896-overview#a3
- https://www.aafp.org/afp/1999/p331.html
General Disclaimer, Licenses and Board Certifications *
Professional Scope of Practice *
The information herein on "Spinal Trauma Imaging Approach to Diagnosis Part II" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and on our family practice-based chiromed.com site, focusing on naturally restoring health for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez, DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card








