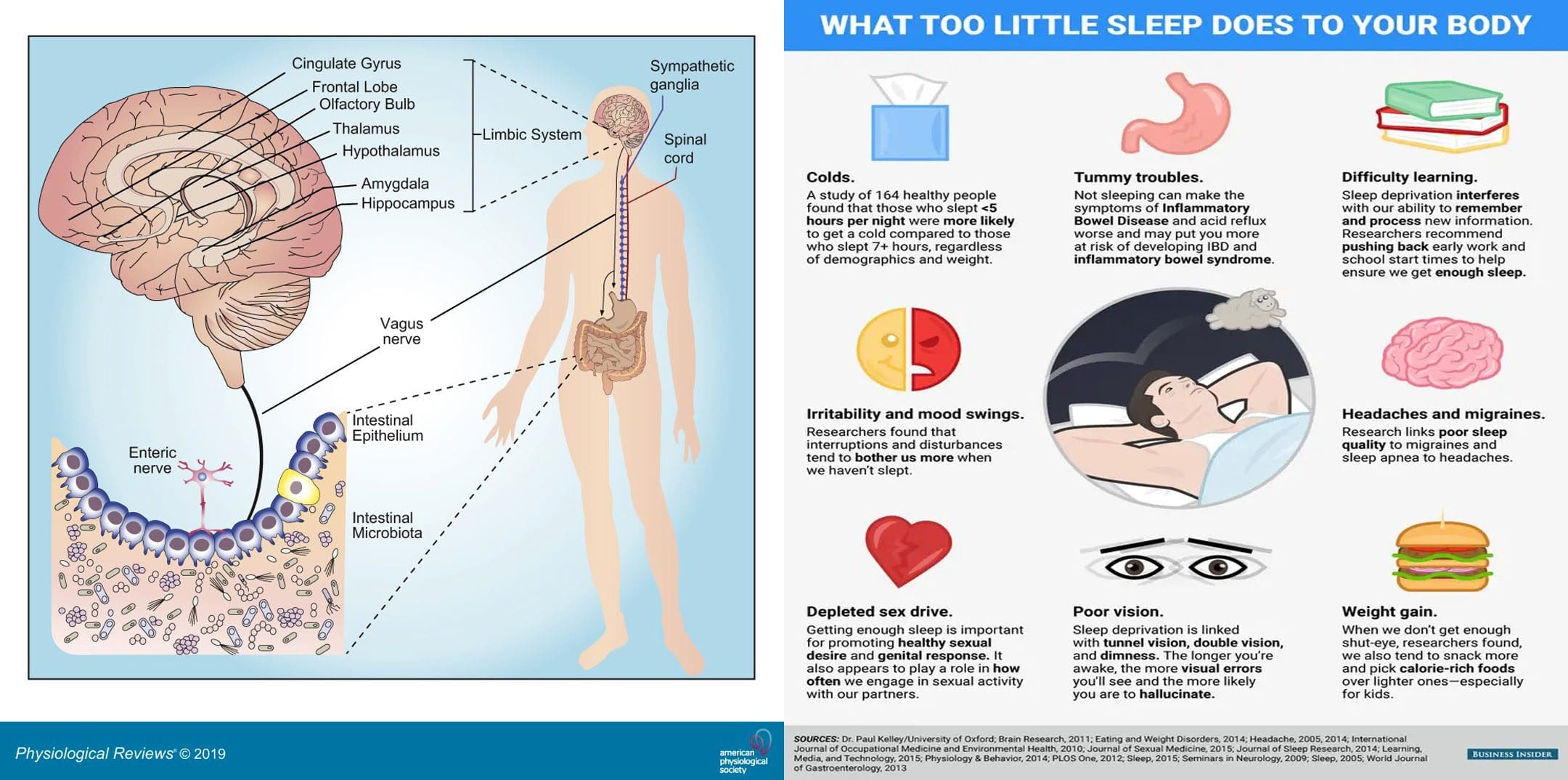
Viruses, bacteria, fungi, and protozoa are the microorganisms that naturally live in the digestive tract. Sleep affects gut health and vice versa. A healthy gut microbiota consists of all kinds of microorganisms that produce thousands of compounds and coexist harmoniously. A healthy diet and lifestyle are the biggest factors influencing bacteria variety, and maintaining a varied diet preserves microbiota diversity. Everybody’s gut microbiome is different; the more diverse the gut microbiome, the healthier sleep will be. The Injury Medical Chiropractic and Functional Medicine Clinic Team can develop a personalized nutritional plan to improve gut health and sleep patterns.
Contents
Sleep Affects Gut Health
Not having a diverse gut microbiome has been linked to autoimmune diseases, Parkinson’s disease, and mental health issues like anxiety and depression. Not getting healthy sleep is associated with many diseases and disorders, including:
- Gastrointestinal disorders
- Infections
- Diabetes
- Cardiovascular disease
- Neurological disorders
- Anxiety
- Depression
- Cancer
Changes in sleep patterns influence the central nervous system and the immune system, which affect different organ systems. For example, studies have shown some gastrointestinal disorders, like irritable bowel syndrome – IBS could be associated with increased REM sleep or the fourth part of the sleep cycle when vivid dreaming occurs. In Crohn’s disease or ulcerative colitis, long-term immune response activation can result in poor sleep, insufficient quality sleep, or other sleep problems. The deepest stages of sleep are when the brain and gut communicate to repair the body, restore nutrients, and remove and release toxins.
Sleep Cycle
During sleep, the immune system produces proteins called cytokines that perform functions during the inflammatory response, either by increasing or blocking inflammation, depending on the body’s needs. Cytokines help promote sleep, fight infection, or stop inflammation in chronic inflammatory diseases like Crohn’s disease or ulcerative colitis.
- Insufficient sleep significantly alters cytokine production, and infection-fighting cells decrease in numbers when sleep deprived, making it harder for the body to fight infections and lessening protection. This increases the inflammatory response and keeps the immune system on.
- Chronic or long-term immune response activation can result in sleep disturbances or disorders.
- Some disorders include small intestinal bacterial overgrowth and inflammation caused by microbiome abnormalities or dysbiosis.
- The gut barrier function begins to malfunction, leading to bacteria and pathogens leaking into blood circulation/leaky gut, triggering immune responses.
Ways to Improve Sleep
One of the main ways to improve sleep quality and gut microbiome health is to practice healthy sleep hygiene. According to the National Sleep Foundation, individuals should:
Nap Smart
- Naps can be a great way to refresh the mind and body and replenish energy levels during the day.
- Naps don’t make up for little sleep at night.
- Keep naps to 20-30 minutes for optimal benefits without disrupting nighttime sleep.
Optimal Sleep Environment
- Comfortable ergonomic mattress and pillows.
- Blackout curtains.
- Temperature between 60 and 67 degrees.
Quit Electronics Before Bed
- The bright lights from phones and screens can make it difficult to fall asleep fully.
- Use an alarm clock with a soft night light and keep the bedroom tech-free.
Create Sleep Routine
- Take a warm shower, read a book, or do light stretches.
- Create a wind-down routine to relax before bed to signal the body that it’s time for sleep.
Avoid Caffeine and Alcohol Before Bed
- These substances make it harder for the mind and body to fall or stay asleep.
Food As Medicine
References
Chabé, Magali et al. “Gut Protozoa: Friends or Foes of the Human Gut Microbiota?.” Trends in parasitology vol. 33,12 (2017): 925-934. doi:10.1016/j.pt.2017.08.005
Deng, Feilong, et al. “The gut microbiome of healthy long-living people.” Aging vol. 11,2 (2019): 289-290. doi:10.18632/aging.101771
Gut Bacteria Research: Physicians’ Committee for Responsible Medicine. (2019). “Gut Bacteria: Optimize Gut Health With a Plant-Based Diet,”
Ianiro, Gianluca, et al. “How the gut parasitome affects human health.” Therapeutic advances in gastroenterology vol. 15 17562848221091524. 30 Apr. 2022, doi:10.1177/17562848221091524
Lozupone, Catherine A et al. “Diversity, stability and resilience of the human gut microbiota.” Nature vol. 489,7415 (2012): 220-30. doi:10.1038/nature11550
Sleep and Gut Microbiome Study: PLoS One. (2019). “Gut microbiome diversity is associated with sleep physiology in humans.
Sleep Hygiene Information: National Sleep Foundation. (2019). “Sleep Hygiene.”
Vaishnavi, C. “Translocation of gut flora and its role in sepsis.” Indian journal of medical microbiology vol. 31,4 (2013): 334-42. doi:10.4103/0255-0857.118870
General Disclaimer, Licenses and Board Certifications *
Professional Scope of Practice *
The information herein on "Sleep Affects Gut Health: El Paso Back Clinic" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and on our family practice-based chiromed.com site, focusing on naturally restoring health for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez, DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card