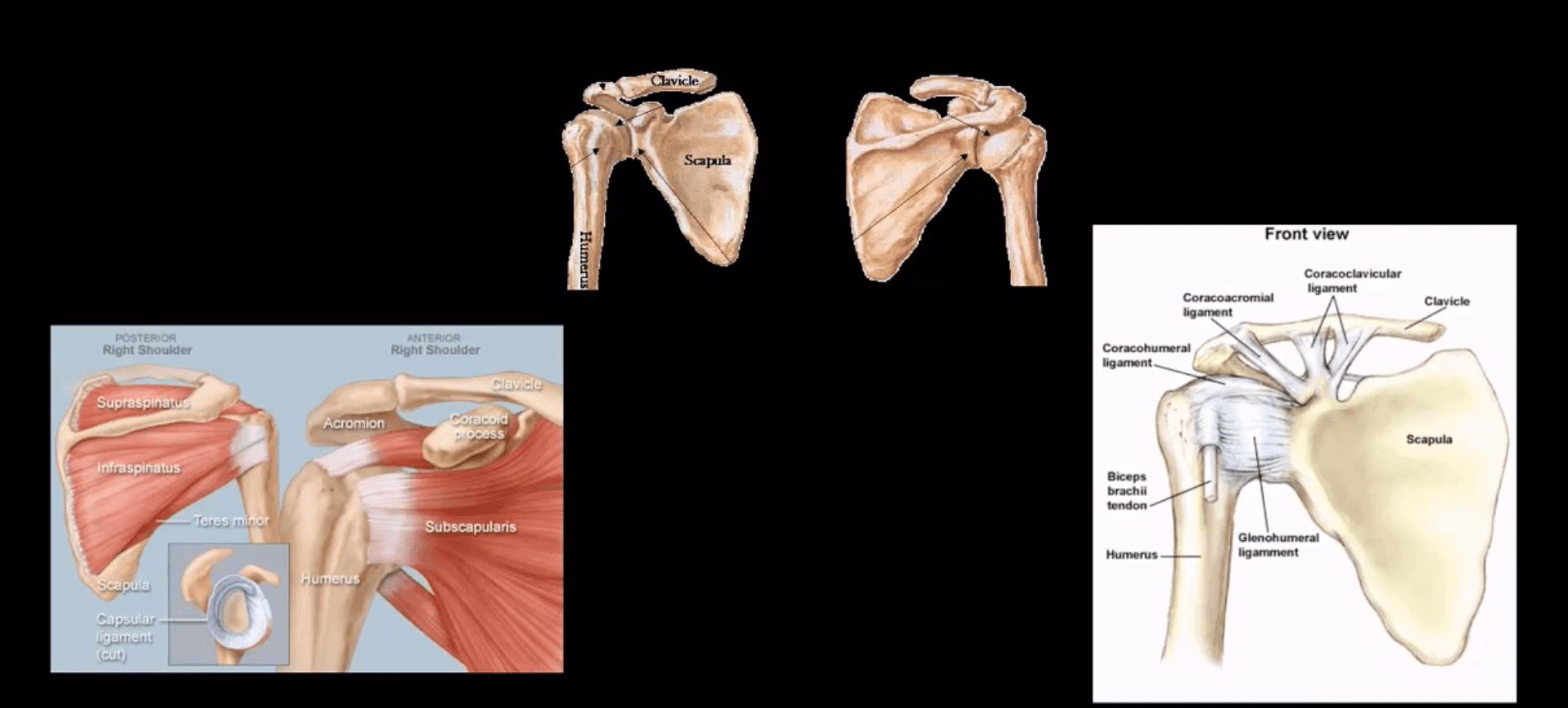
Overview of Shoulder Anatomy
Contents
Acute Trauma
- Proximal humeral Fx account for 4-6% of all Fxs. Osteoporotic (OSP) Fx in >60 y.o associated with minimal trauma with F: M 2:1 ratio. In young patients, acute high energy trauma predominates.
- Complications: AVN humeral head, Axillary N paralysis.
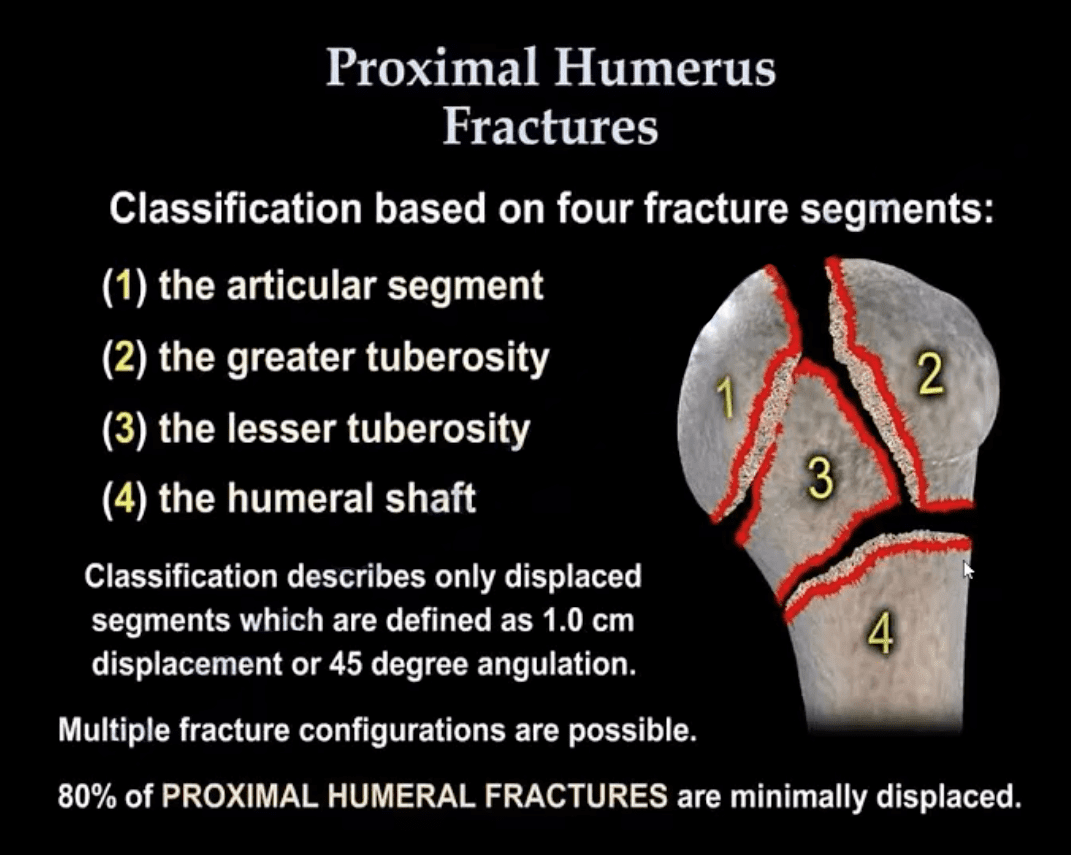
- Neer Classification: considers fractures along 4-anatomical lines with or w/o displacement >1-cm & 45-degree angulation
- One part Neer Fx- no displacement or very minimal <1-cm/45-degree. Can affect 1-4 lines and M/C at greater tuberosity. 80% of proximal humeral Fx are one-part Neer.
- Two-part Fx: 1-part is displaced >1-cm/45-degrees. m/c involves the surgical neck
- Three-part Fx: 2-parts are displaced >1-cm/45-degrees.
- Four-part Fx: all 4-parts can be displaced. Uncommon <1%
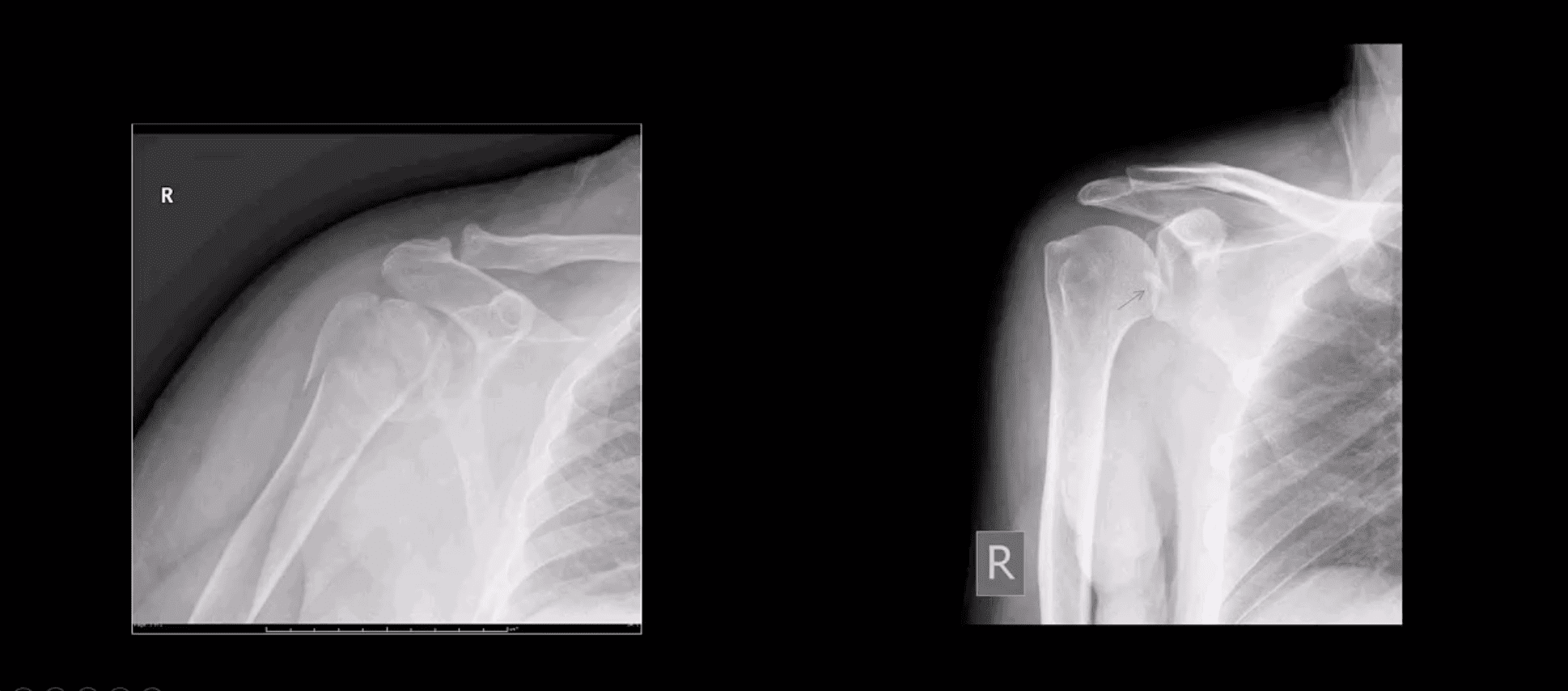
- Imaging: 1st step-radiography, CT may be used in more complex cases. Orthopedic referral
- Management: Neer one-part Fx is treated with Sling Immobilisation and progressive rehab
- The vast majority of Fx in the elderly are treated non-operatively
- Younger patients (40-65) may occasionally require hemiarthroplasty if 3 or 4-part Neer Fx present. Greater risk of AVN
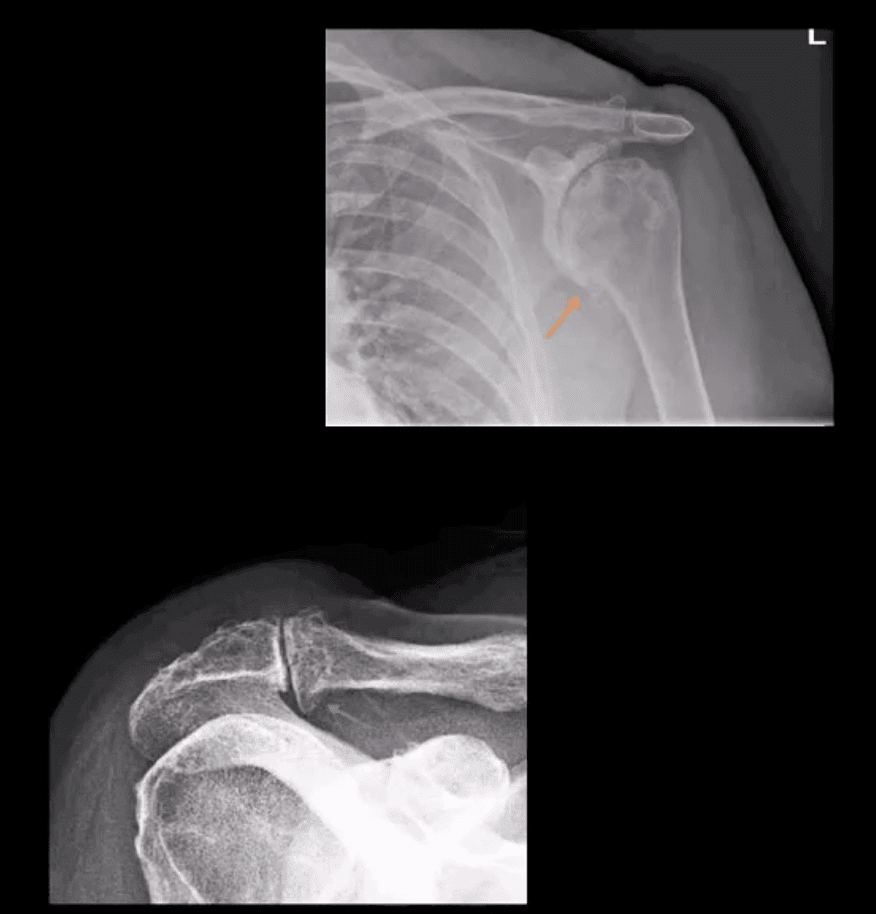
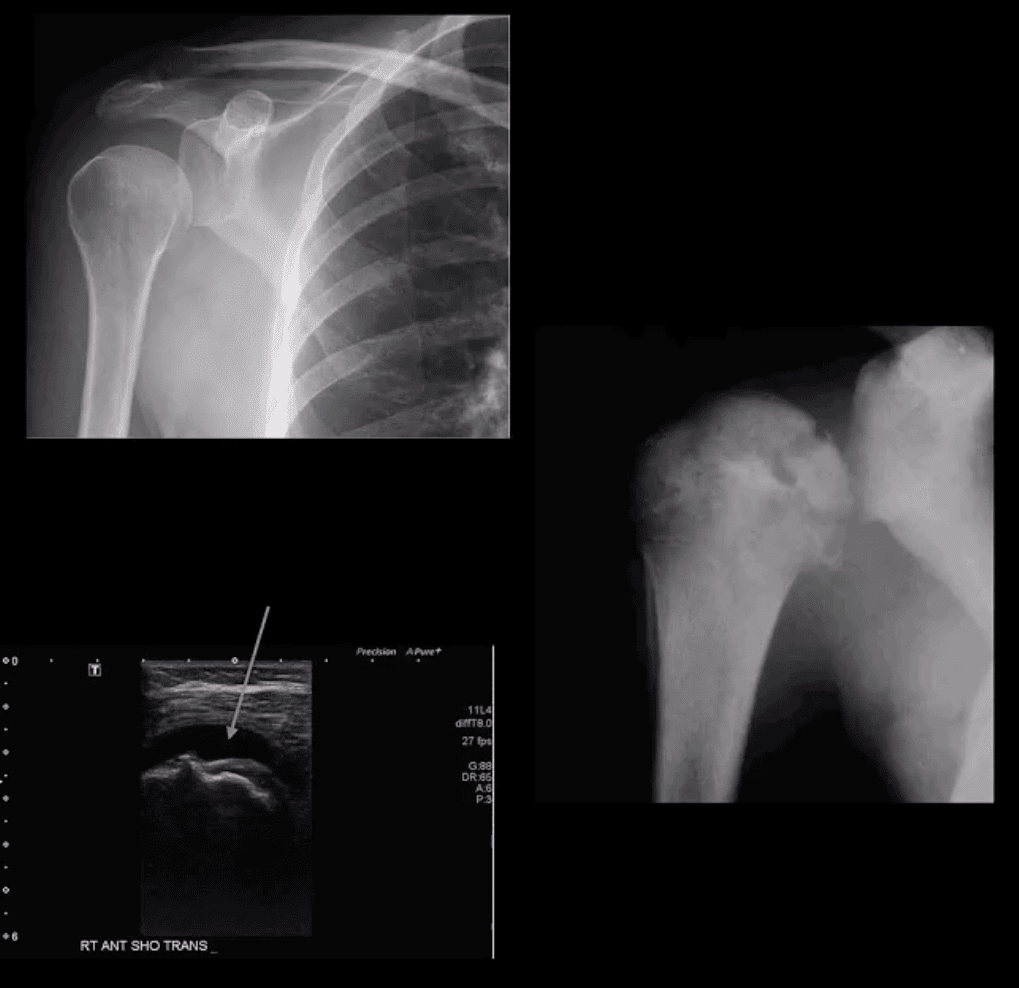
Proximal Humerus Fractures
- Note: Left image: Fx involving the anatomical neck and the greater tuberosity with minimal displacement <1-cm/45-degree thus Dx as one-part Fx. Right image: Small avulsion Fx of the greater tuberosity with significant displacement (>45-degrees & 1-cm) thus Dx as two-part Fx
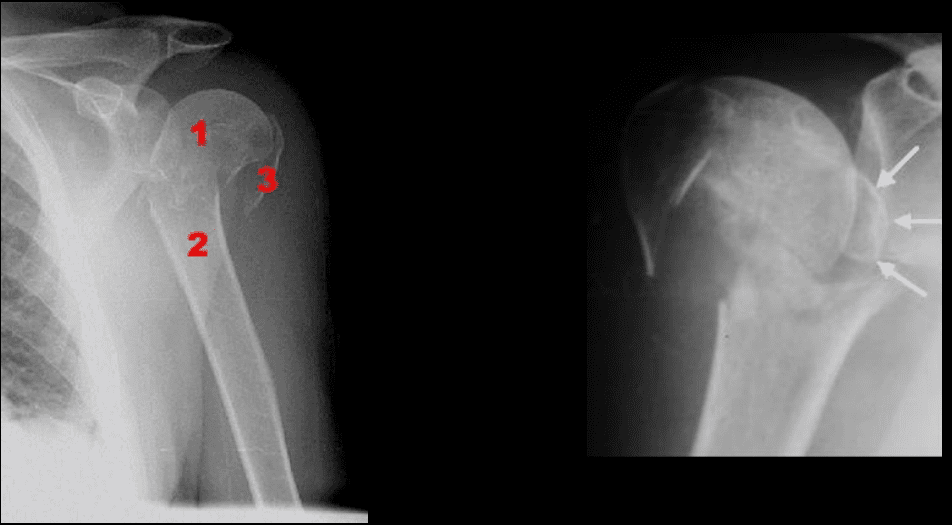
- Note: three-part Neer Fx (left) and four-part Neer Fx (right)> Management: operative in most cases in younger (40-65) patients
Shoulder Dislocation aka Glenohumeral Joint dislocation (GHJD)
- Refers to complete separation of the humerus from scapula glenoid. In 20-40s M: F 9:1 ratio, in60-80S M: F 3:1
- Anatomy: Shoulder stability is sacrificed for mobility, and overall GHJD is the m/c among large joints in the body
- Protective falls (e.g., FOOSH) and MVA are m/c causes. GHJ is most vulnerable in abduction, extension and external rotation. Anatomical factors: shallow glenoid, laxed ant-inferior capsule and GH ligaments. GHJD will induce severe tearing of major GHJ restraints. Associated osseous and labral injuries are common and may lead to chronic instability, DJD,�and functional changes
- 3-types: Anterior GHJD (95%)
- Posterior GHJD (4%) especially associated with epileptic seizures, electrocution and can occur b/l
- Inferior GHJD aka Laxatio Erecta (<1%) associated with severe trauma
- Clinically: AGHJD presents with severe pain, the arm is externally rotated and adducted, severe limitation of movement. GHJD may persist as chronic dislocation.
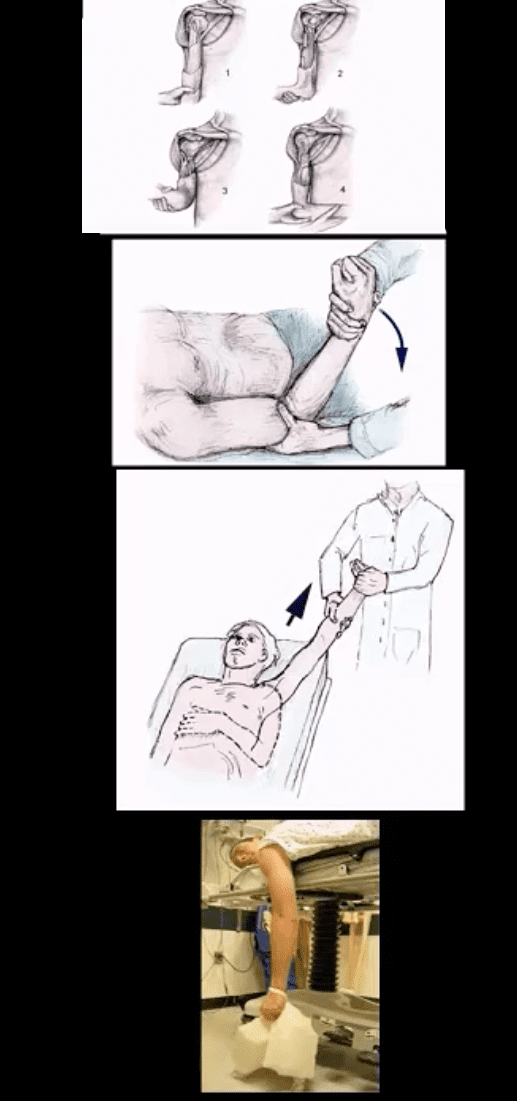
- Management: prompt reduction in ED under anesthesia or heavy sedation with Kocher technique top image (not used), External rotation method (middle) or Milch technique (can be used w/o anesthesia) and a few other methods. Delay in reduction correlates with greater risk of immediate and long-term�complications
Diagnostic Imaging Approach
- Shoulder series x-radiography is sufficient. Additional Imaging with CT scanning and MRI may be helpful to Dx osseous, cartilage, labral/ligaments pathology
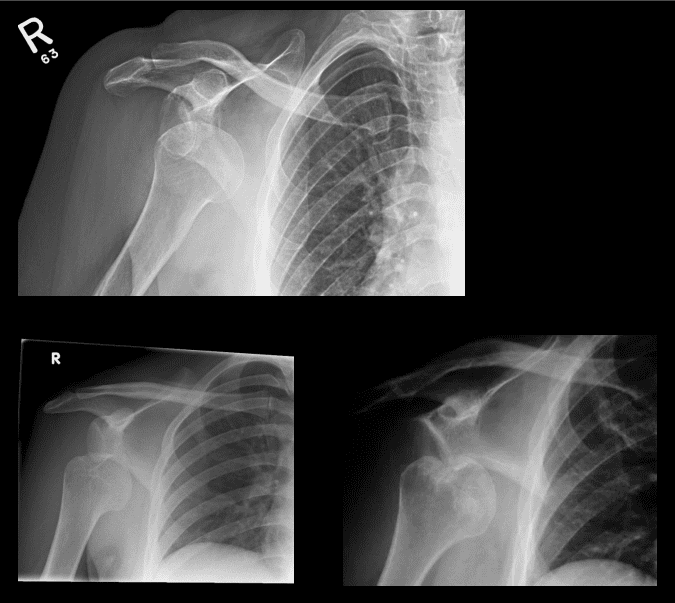
- Anterior GHJD (95%). Subcoracoid position(top right) of the humerus is the m/c
- Anterior GHJD may also occur as subglenoid(bottom left)and infrequently as subclavicular
- Key to radiographic search is to evaluate associated Bankart and Hill-Sachs injuries
Bankart Lesion
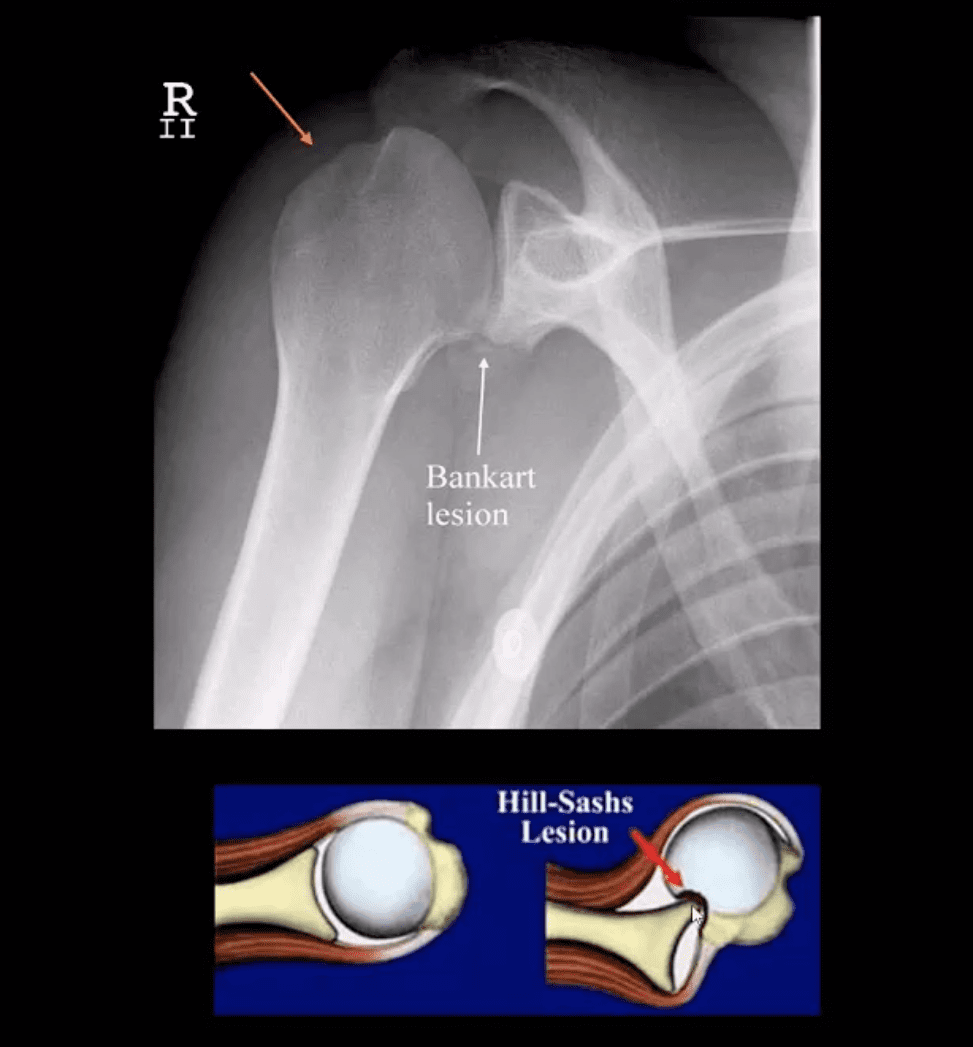
- Occurs during anterior GHJD d/t impaction of the head into anterior-inferior glenoid. Variations exist (see next slide). BonyBankart can be seen on x-rays. So-called soft tissue Bankart requires MRI. Cartilage (soft)Bankart is the m/c.
- Hill-Sachs aka Hatchet deformity (arrow postreduction)occurs during the same mechanism as Bankart, i.e., compression and impaction of posterolateral aspect of the head against the glenoid producing wedge-shape Fx. Hill-Sachs lesion may predispose to recurrent/chronic GHJD.
- Bankart lesion may heal, but operative suture anchors are needed sometimes
- CT arthrogram and MRI may be helpful
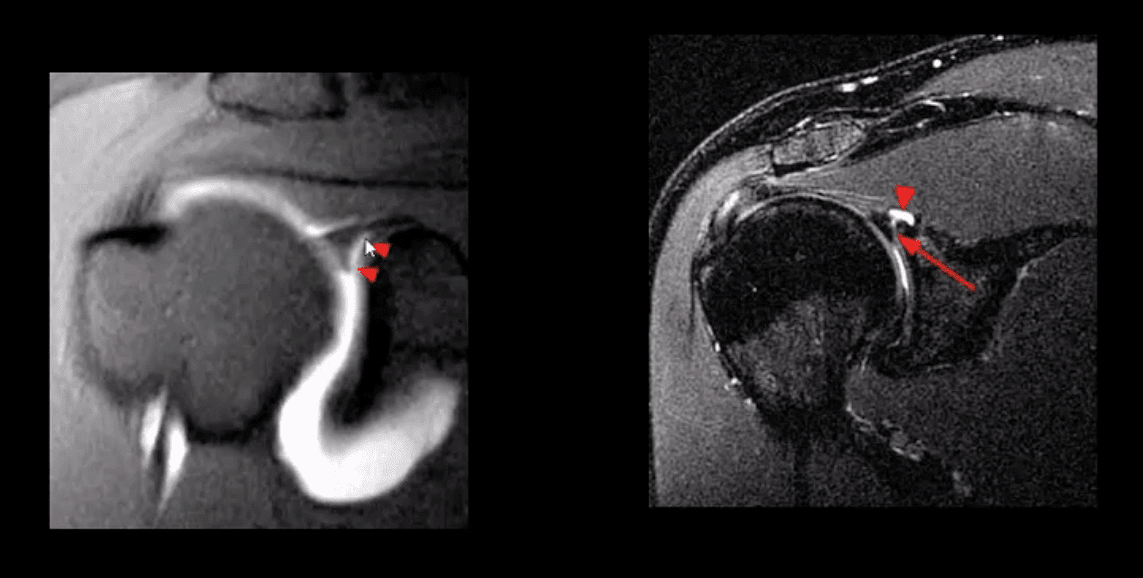
Types of Bankart Lesion
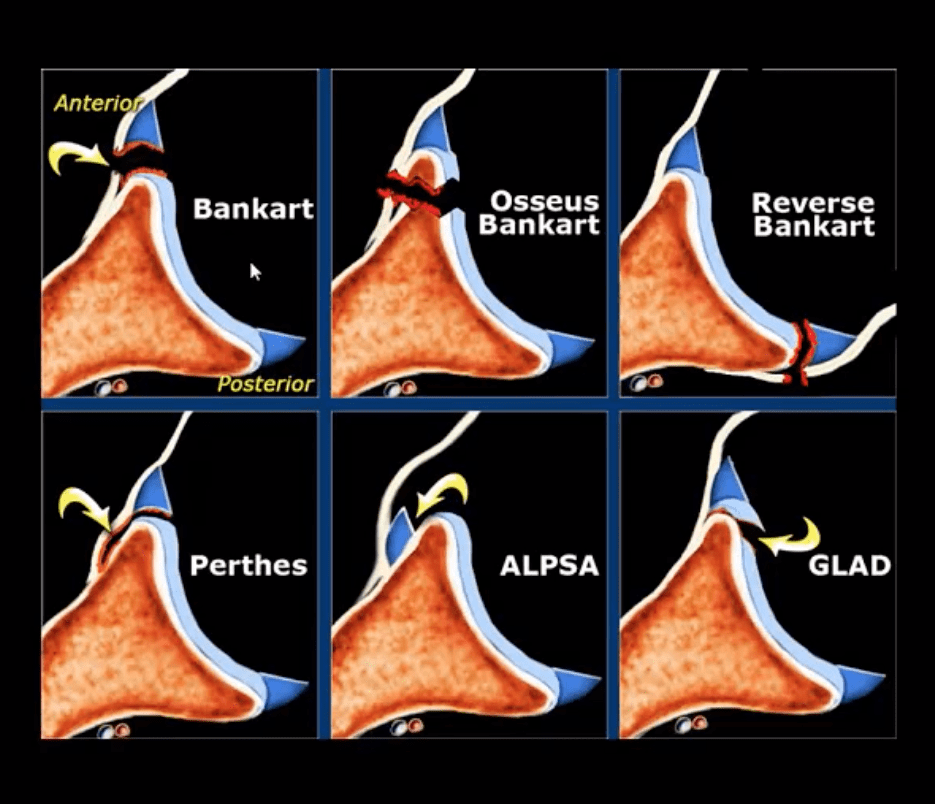
- Note different types of Bankart lesion. Onlyosseous Bankart can be seen radiographically. Soft tissue Bankart requires MRI with and without intra-articular gadolinium(arthrogram).
Posterior Dislocation
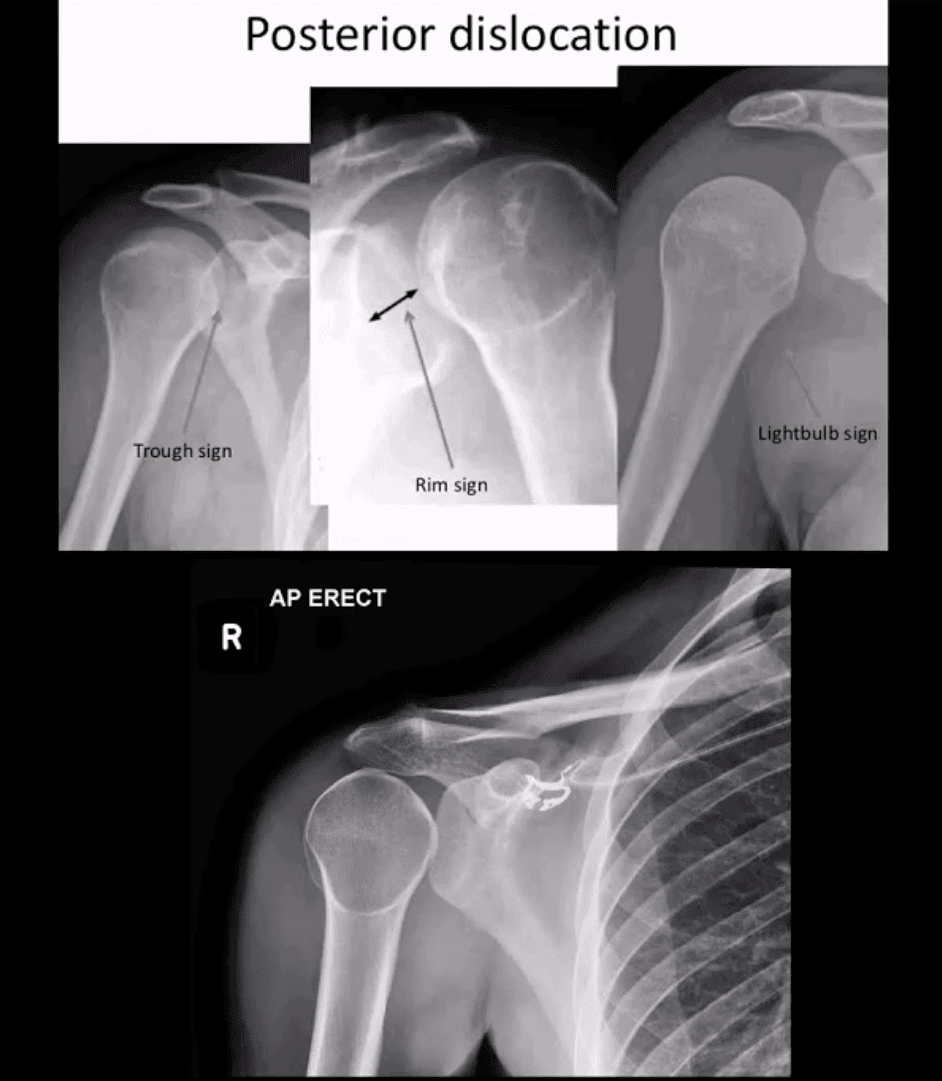
- Note: posterior GHJD with its characteristic signs:
- Trough sign aka reverse Hill-Sachs. Occurs d/t anterolateral head impaction Fx
- Rim sign: only occurs in the PGHJD d/t posterior position of the head and anterior glenoid-to humeral head distance 6-mm or greater
- Light-bulb sign: d/t acute internal rotation of the humerus (head)
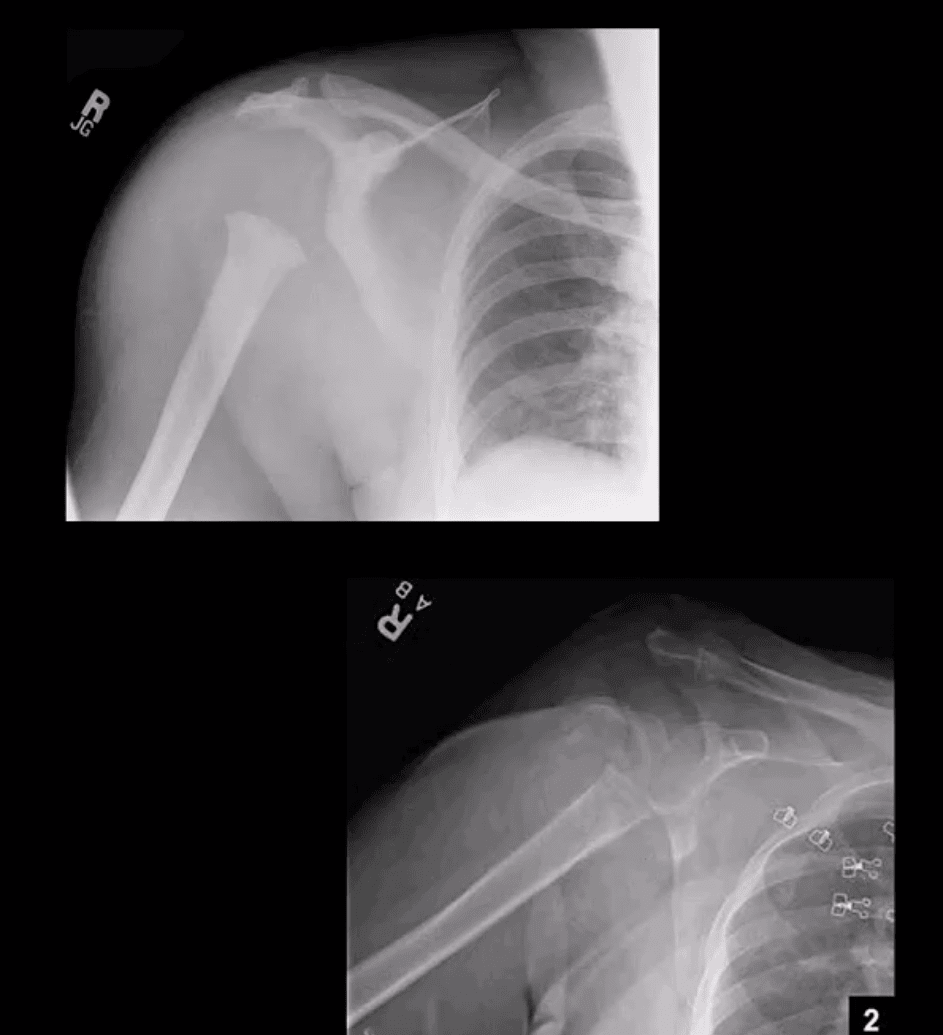
Inferior GHJD

- Inferior GHJD aka Laxatio Erecta
- Severe hyperabduction and inferior displacement of the humerus. Greater chances of severe neurovascular injury and acromial Fx
- The dislocated arm is hyperabducted and fixed with the elbow flexed and the arm above the head
ACJ Dislocation (ACJD)
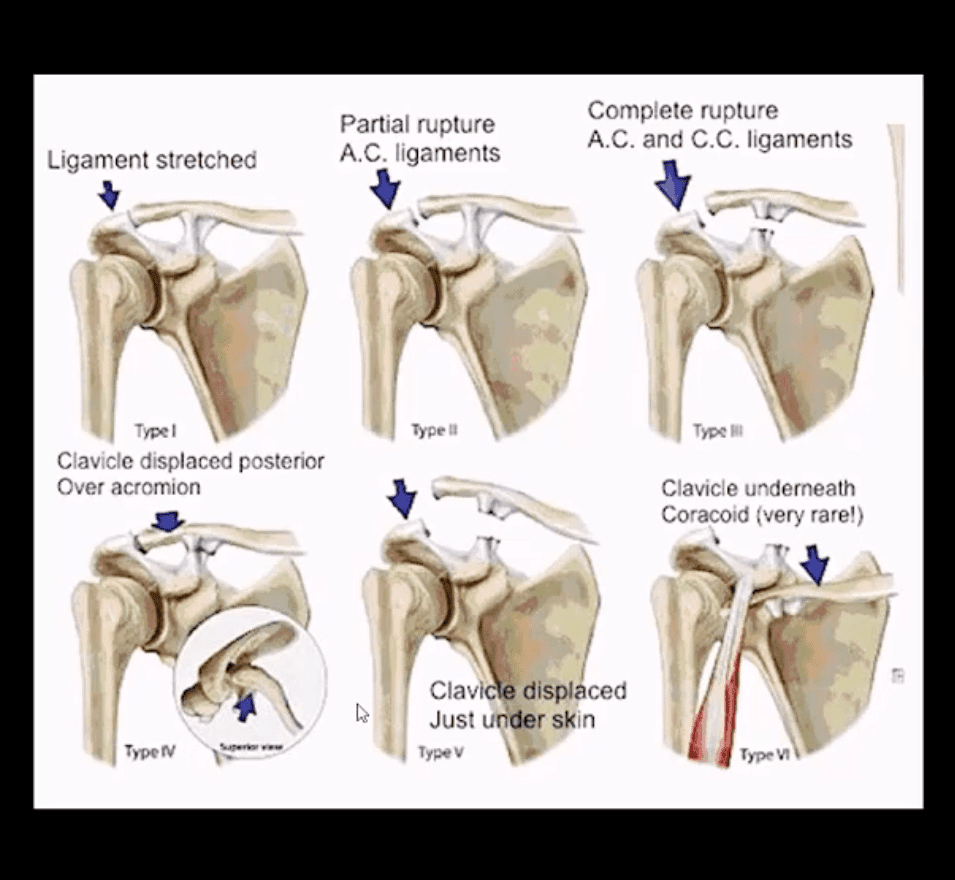
- ACJD: common injury, 9% of shoulder girdle injuries esp. in male athletes by a direct blow
- Rockwood classification (left) evaluates tearing of AC and CC ligaments and regional muscles
- Type1, 2, 3 among the m/c
- Type 1: sprain of ACL w/o tearing
- Type 2: tear of ACL and sprain of CCL
- Type 3: tear of AC & CCL. The clavicle is elevated above the acromion. If <2-cm good results with conservative Rx.
- Imaging: x-radiography with b/l ACJ views with and w/o weights to compare both ACJs. In complex cases CT scanning esp. if Fx is considered
- Management: Type 3 (>2-cm) & Types 4-6Operative
Type 3 ACJ Separation
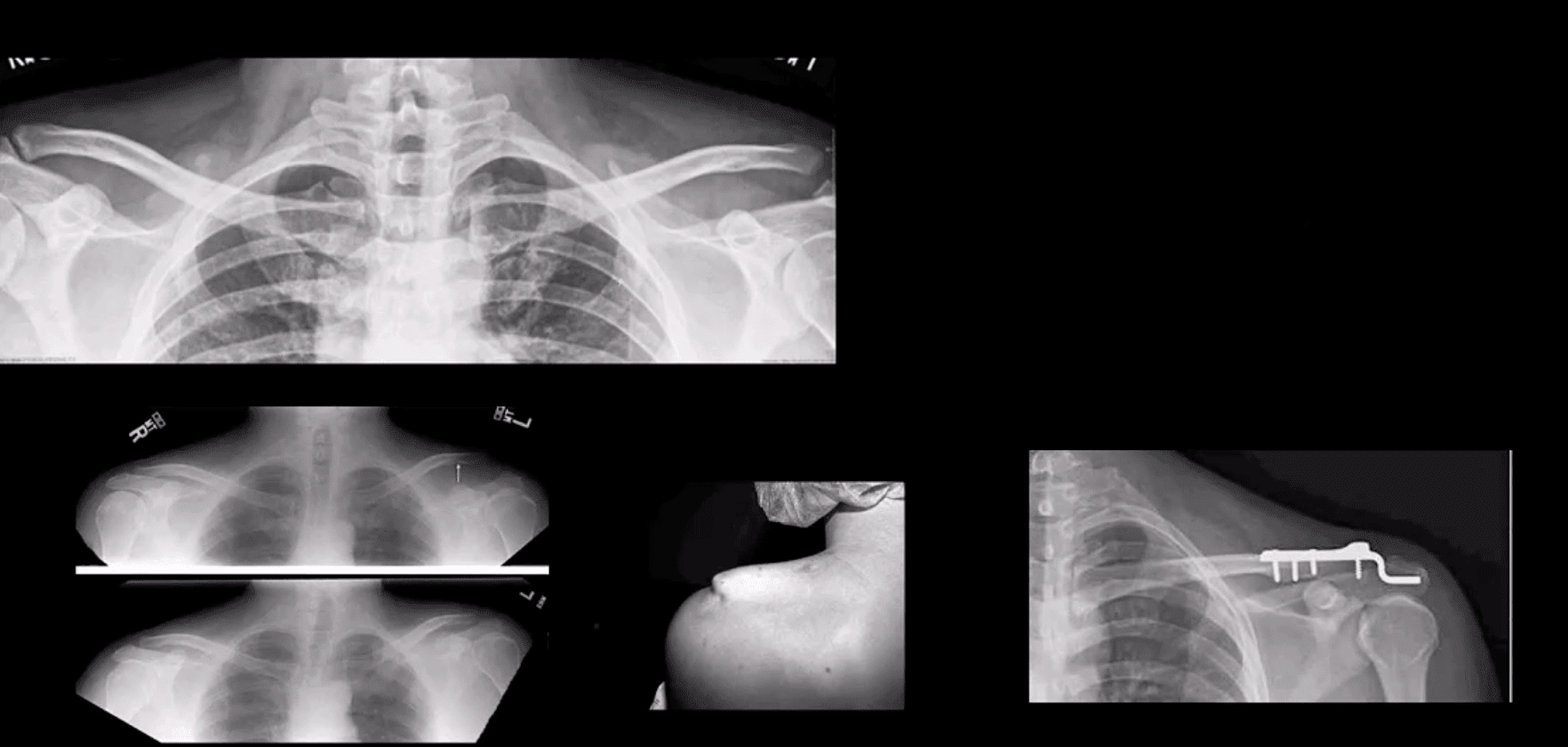
- Type 3 ACJ separation (top left)
- More significant ACJD (bottom images) with clinical sign of acromion under the skin and resultant ORIF
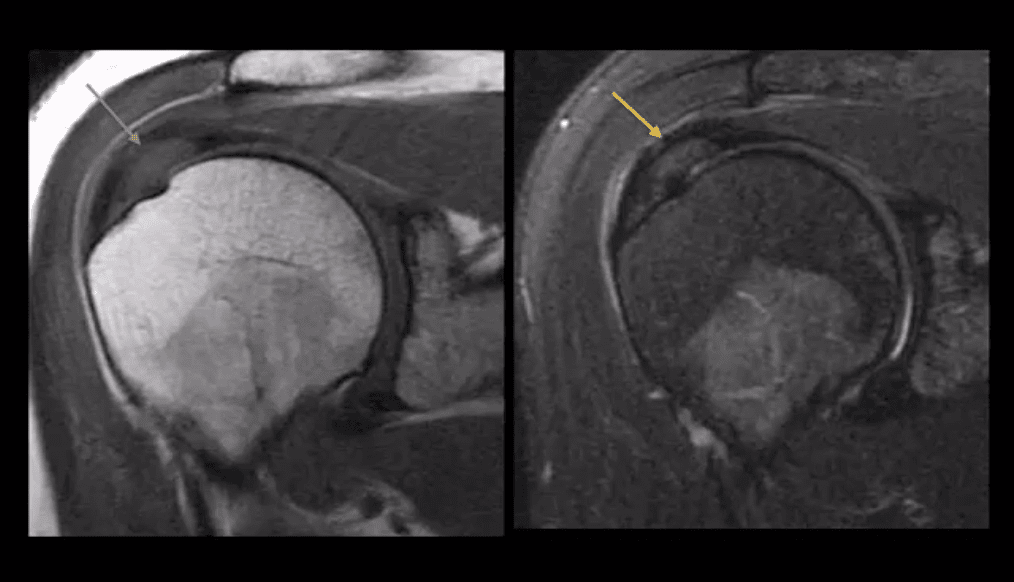
Rotator Cuff Muscles (RCM) Pathology
- RCM tendinopathy: collagenous degeneration of RCM particularly Supraspinatus M. tendon(SSMT) d/t overuse/degeneration-micro tearing with collagenous replacement. Impingement syndrome is a 2nd extrinsic cause. Presented clinically as pain and limited ROM
- Imaging Dx: MSK US can be as accurate as MRI and better in some cases d/t dynamic evaluation v. cost effective
- Key MRI clue is thickened inhomogeneous SSMTwith increased signal on all pulse sequences d/t fatty degeneration and inflammation (left images: T1 & T2 FS)
- MSKUS findings: thickening of the SSMTsubstance with a change�in normal echogenicity.MSKUS is good to DDx with SSMT tears. US advantages are that it allows dynamic evaluation of painful structures
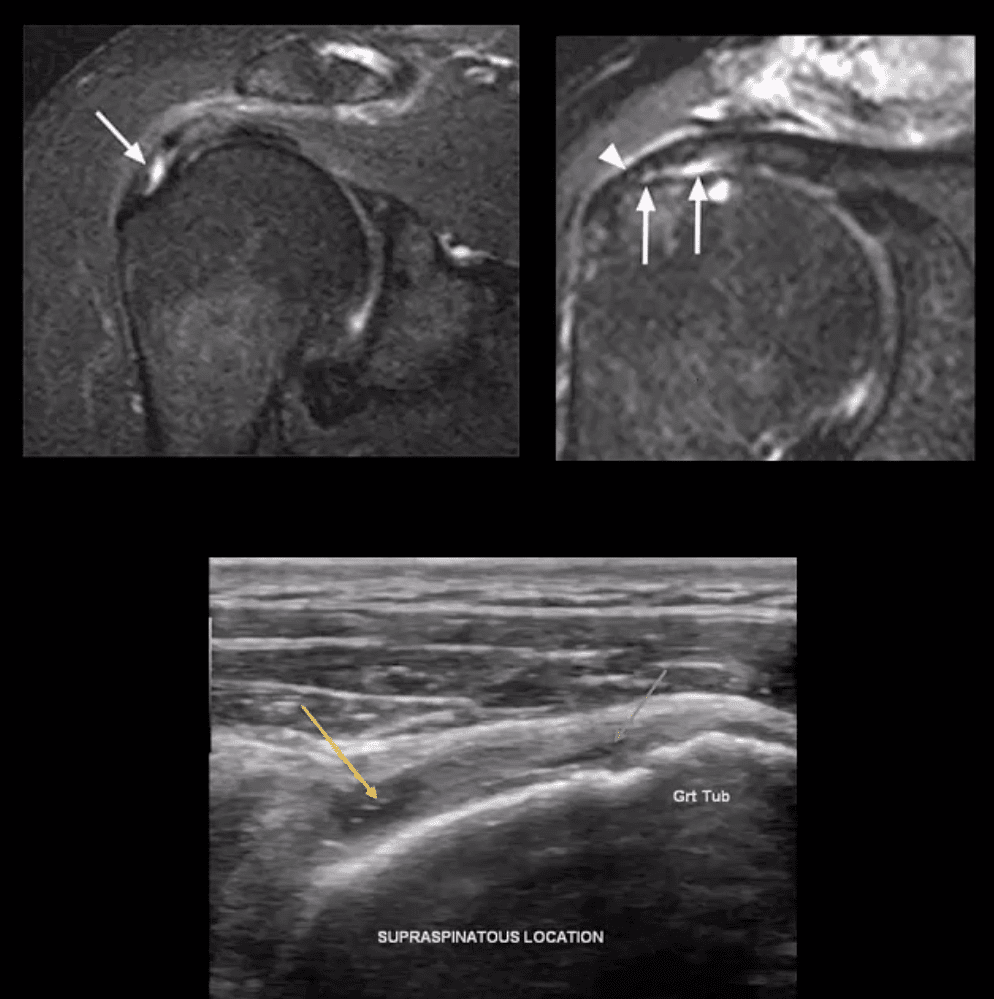
- Partial tear of SSMT: partial (incomplete) tear ofSSMT may occur at the bursal and articular surface or interstitial, i.e., intra-substance/noncommunicating. Etiology: sub-acromial impingement, acute strain, and chronic microtrauma tendinosis
- Clinically: pain on abd and flexion, impingement tests, Hawkins-Kennedy tests, etc. Pearls: partial tears can be more painful than complete tears
- Imaging Dx: MSKUS is as good as MRI (N.B.some studies indicated MSKUS is more superior to MRI). Key MRI findings: gap/incomplete tear of SSMT filled with joint fluid +/- granulation tissue
- MSKUS: decreased echogenicity of SSMT, thinning and partial tearing filled with fluid(anechoic areas arrows). Lost convexity of tendon bursal or articular interface.
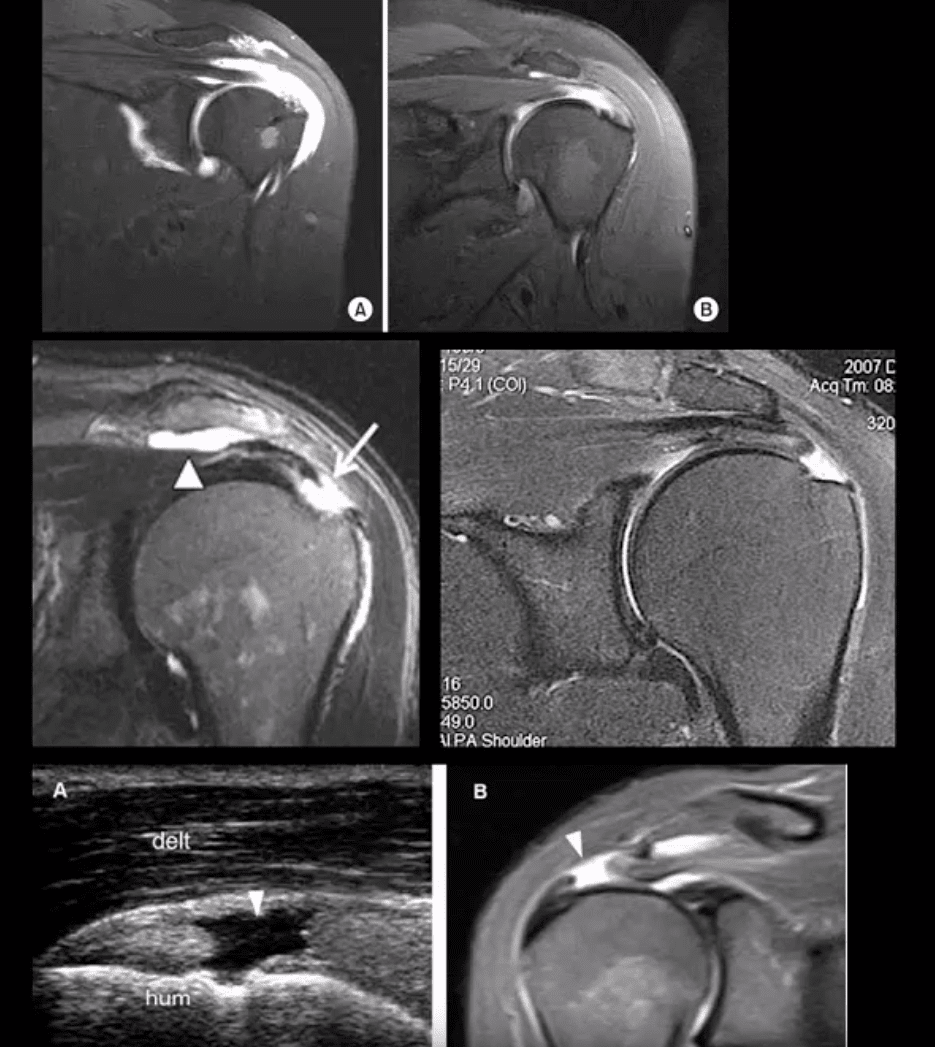
- Full Thickness SSMT (rot cuff) tear: degeneration/tearing of rot cuff. 2nd to impingement by Hooked acromion, overhead overuse or acute trauma. 7-25% of shoulder pain in the general population. Clinically: pain on impingement tests.
- Imaging Dx: MSKUS is as good as MRI.Limitations: poor Dx of labral pathology. Key USDx: focal tendon interruption, an anechoic gap (fluid filled), hypoechoic tendon, tendon retraction, uncovered cartilage sign (bottom left, A: US B: MRI)
- MRI: key Dx: insertional tear extending through entire SSMT crescent, retraction with fatty degeneration of SSMT and the muscle. If retraction is at 12 o�clock or greater (top images), it may not be anchored operatively
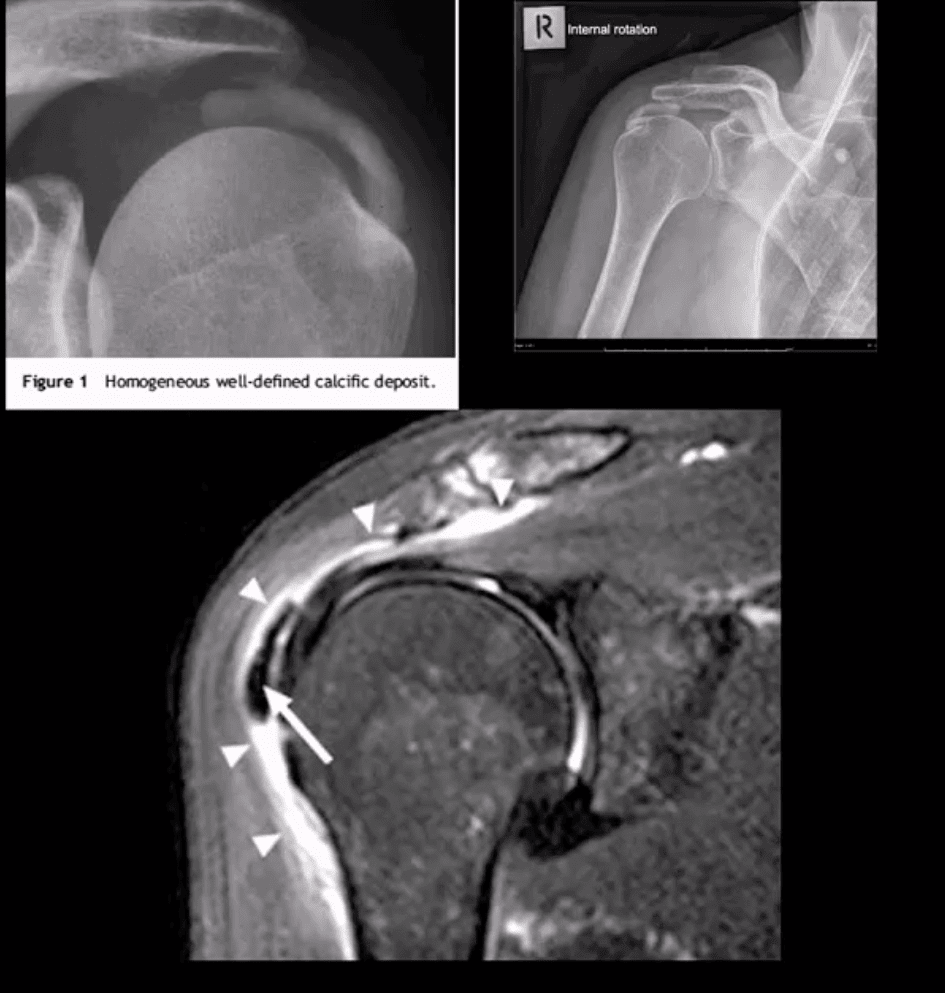
- Rotator Cuff (RTC) Calcific Tendinitis: usually d/t calcium HADD crystals. Middle-aged women are most affected. Ranges from asymptomatic imaging finding to severe destructive arthropathy or Milwaukee shoulder(infrequent)
- HADD has 3-pathological phases: formation resting-resorption.Mild-to-moderate pain esp. in resting phase.
- Imaging: x-radiography: homogenous ovoid mineralization within RTCMT, m/c in SSMT. MRI: ovoid/globular decreased signal on all pulse sequences often with surrounding edema (bottom left)
- Rx: self-resolution occurs. Advanced cases: operative aspiration etc.
Superior Labrum Anterior to Posterior (SLAP) Lesions/Tears
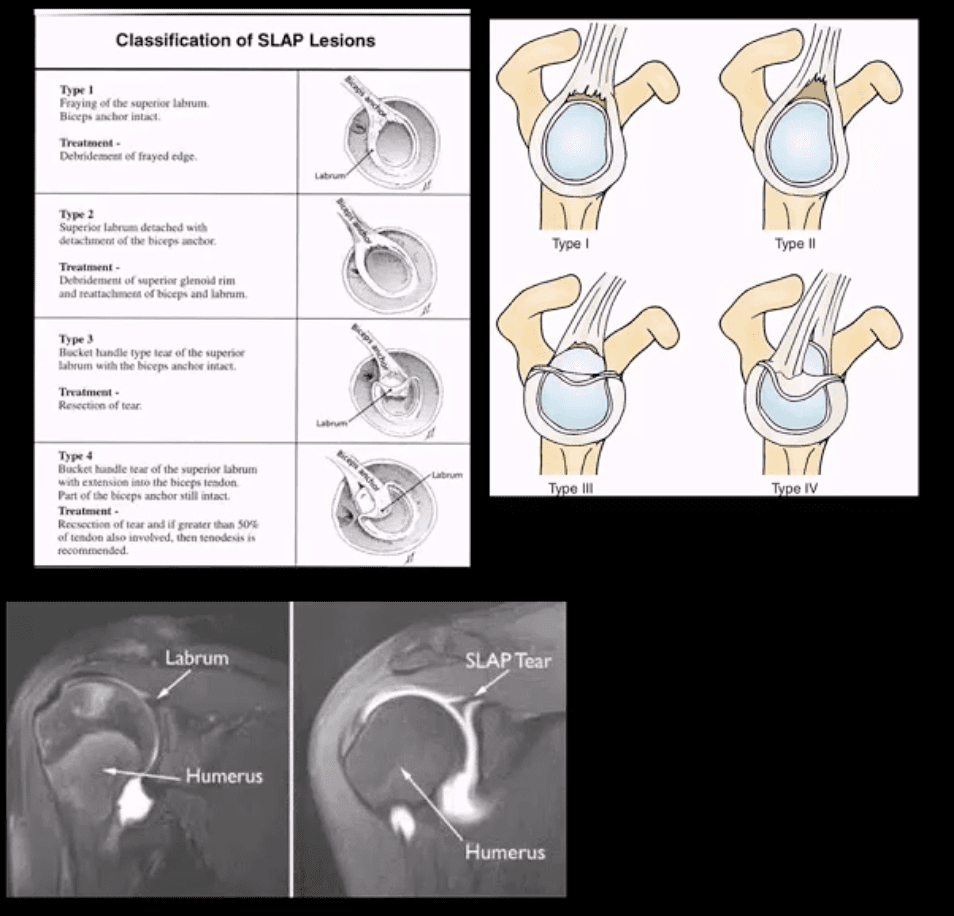
- SLAP tears: FOOSH and throwing sports or chronic shoulder instability aka Multidirectional shoulder instability (in 20%). Type 1-9 exist but the M/C areType 1-4
- In all 4-types superior labrum is affected with or w/oLHBMT anchor tear (see pictures). Clinically: pain, limitation of AROM with active compression tests, typically non-specific findings mimicking RTCpathology
- Imaging is crucial: best imaging is MRI arthrography. Key signs: hyperintense linear fluid signal within superior labrum +/- extending along the LHBT on fat-suppressed fluid sensitive imaging and FS T1 arthrogram. Best observed on coronal slices.
- Rx: small tears may heal, but unstable tears require operative care.
- Key DDx: anatomical variants like Buford complex andSub-labral foramen
- SLAP tear with a paralabral cyst (bottom right)
- Normal variant DDx: sub labral foramen(bottom left) note: MR arthrography with contrast undercutting the labrum but w/o extending posteriorly to the LHBT
Shoulder Arthritis
- GHJ DJD: usually associated with a 2nd cause: trauma, instability, AVN, CPPD, etc. Presented with pain, crepitus and decreased ROM/function. Associated RTC disease may be present. Imaging; x-radiography is sufficient and provides grading/care planning.Major findings: joint narrowing, osteophytosis esp. at the inferior-medial head (orange arrow), subchondral sclerosis/cysts. Often noted superior head migration d/t RTC disease.
- ACJ OA: common and typically primary with aging. Presents with ACJ loss and osteophytes. Osteophytes along the undersurface of the ACJ �keel osteophytes�(blue arrow) may lead to RTC muscle tear. Regional bursitis is other clinical feature of ACJ arthrosis.
- Management: usually conservative depending on clinical signs/symptoms
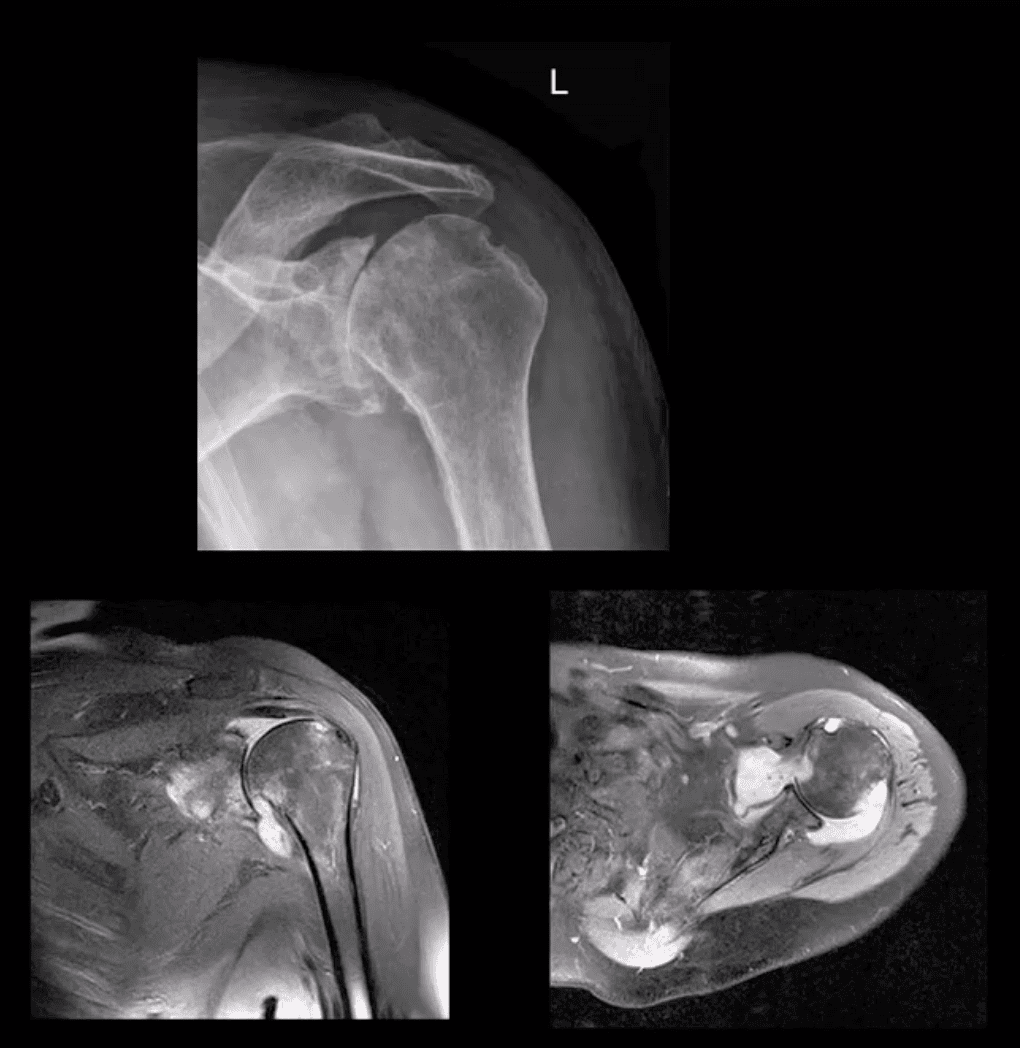
- Rheumatoid Arthritis GHJ: RA is a multisystem inflammatory disease affecting multiple joints lined by the synovium. GHJ RA is common (m/c large joints in RA knees/shoulders). Clinically: pain, limited ROM and instability, muscle weakness/wasting. Hands, feet,�and wrists are m/c affected. Imaging: x-radiography reveals periarticular erosions, uniform joint space loss, juxta-articular osteoporosis, subluxations,�and soft tissue swelling. MRI can help detect�commonly associated RTC tearing and instability. Early changes can be detected by MSKUS esp. with power Doppler use indicating hyperemia/inflammation.
- Note: L shoulder x-ray revealing cartilage destruction and symmetrical joint loss, multiple erosions, and likely loss of RTCM support with superior head migration, ST effusion present.
- Note: PDFS coronal and axial MRI slices of GHJ RA indicating marked inflammatory joint effusion, bone erosion/edema, synovial pannus formation and likely tear in RTC m. Management: Rheumatological referral and pharmacotherapy with DMARD. Operative care asRTCM repair. 10% of patients are disabled d/t RA
- Neuropathic Osteoarthropathy aka Charcot’s shoulder: d/t neurovascular and neural periarticular damage. Multiple causes exist.M/c develops in diabetics in midfoot. Shoulder Charcot is m/c in Syringomyelia (25%), trauma paralysis, MS, etc. Dx: clinical(50% pain/swelling 50% painless destruction). Imaging is crucial. X-radiography is sufficient in well-established cases, but early Dx is challenging. MRI may help with early Dx and delayed complications. Rad Dx: Shoulder Charcot is m/c presented as atrophic type destructive arthropathy with humeral head appearing as if surgically amputated along with intra-articular debris, density, distention, dislocation, and other key features
- Septic Shoulder: shoulder is the 3rd m/c followingknee>hips. Patients at risk: diabetics, RA pts, immunocompromised, I.V. drug users, indwelling catheters, etc. Routes: hematogenous (m/c), direct inoculation (iatrogenic, trauma etc.) adjacent spread(e.g. OM). Staph. Aureus (>50%) m/c.
- Clinically: joint pain and dec. ROM, fever 60% only, toxemia, inc. ESR/CRP. Dx: imaging and joint aspiration/culture. RadDx: early x-rays often unremarkable except ST effusion/fat planes obscuration, joint widening. Later7-12 days patchy osteopenia, moth-eaten/permeating bone resorption, articular destruction, joint narrowing. May progress to severe joint destruction and ankyloses. Early Dx & I.V. antibiotics are crucial even before culture. Operative irrigation and joint drainage in some cases. Complications are possible esp. if Rx is delayed. MSKUS with needle aspiration may help. Note: (top image) non-traumatic joint widening with inferolateral head displacement d/t septic A dx: by needle aspiration Staph. Aures.
Ischemic Osteonecrosis
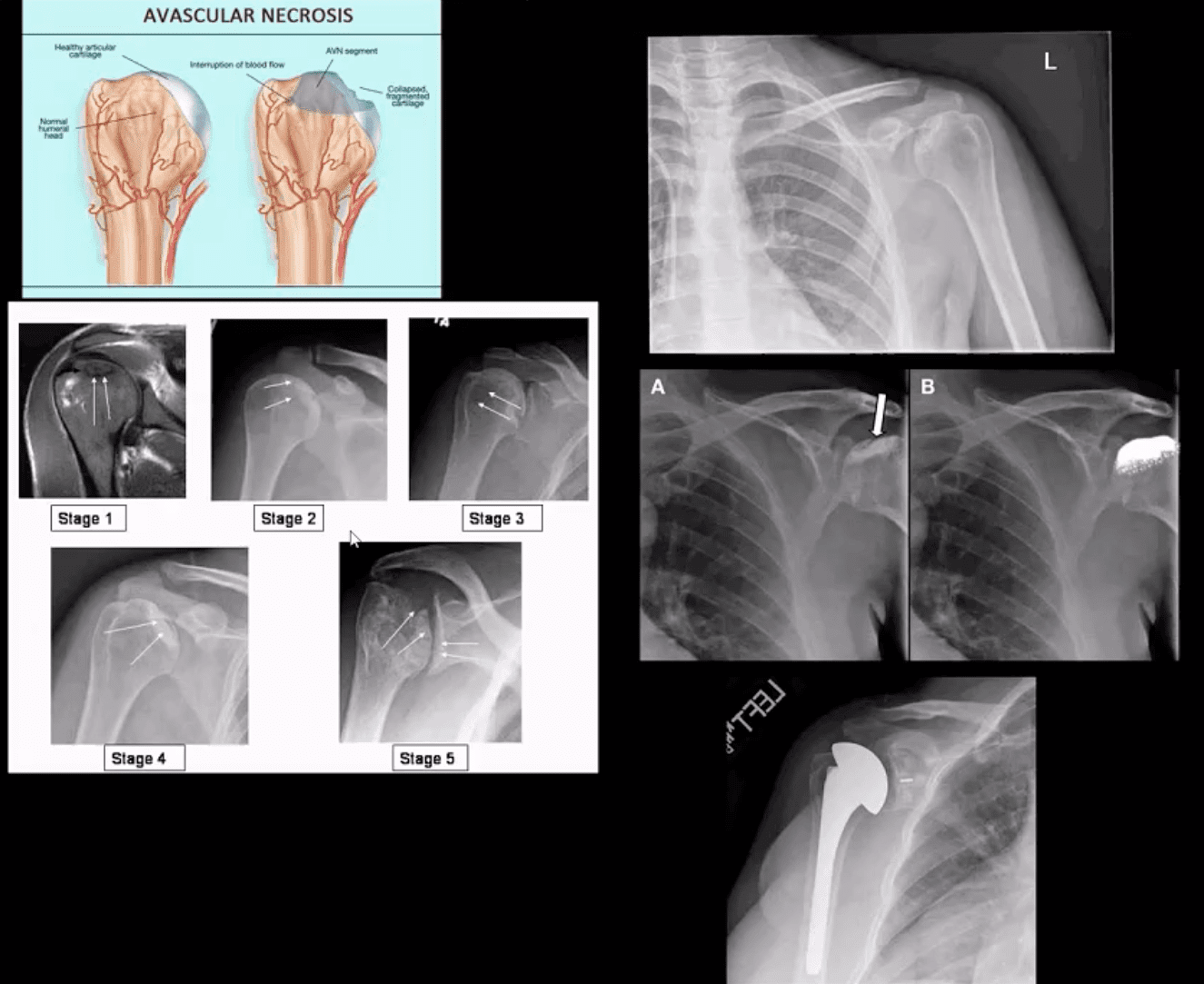
- Ischemic Osteonecrosis of the humeral head may occur d/t trauma (Neer four-part Fx), Steroids, Lupus, Sickle cell, Alcoholism, Diabetes,�and many other conditions. Imaging is crucial: MRI detects earliest changes as intraosseous edema. X-ray features are late, presented as a collapse of subchondral bone with sclerosis �snow cap� sign, fragmentation, and progressive severe DJD
- Management: orthopedic referral, core decompression in early cases, hemiarthroplasty in moderate and total arthroplasty in severe cases.
Shoulder Neoplasms
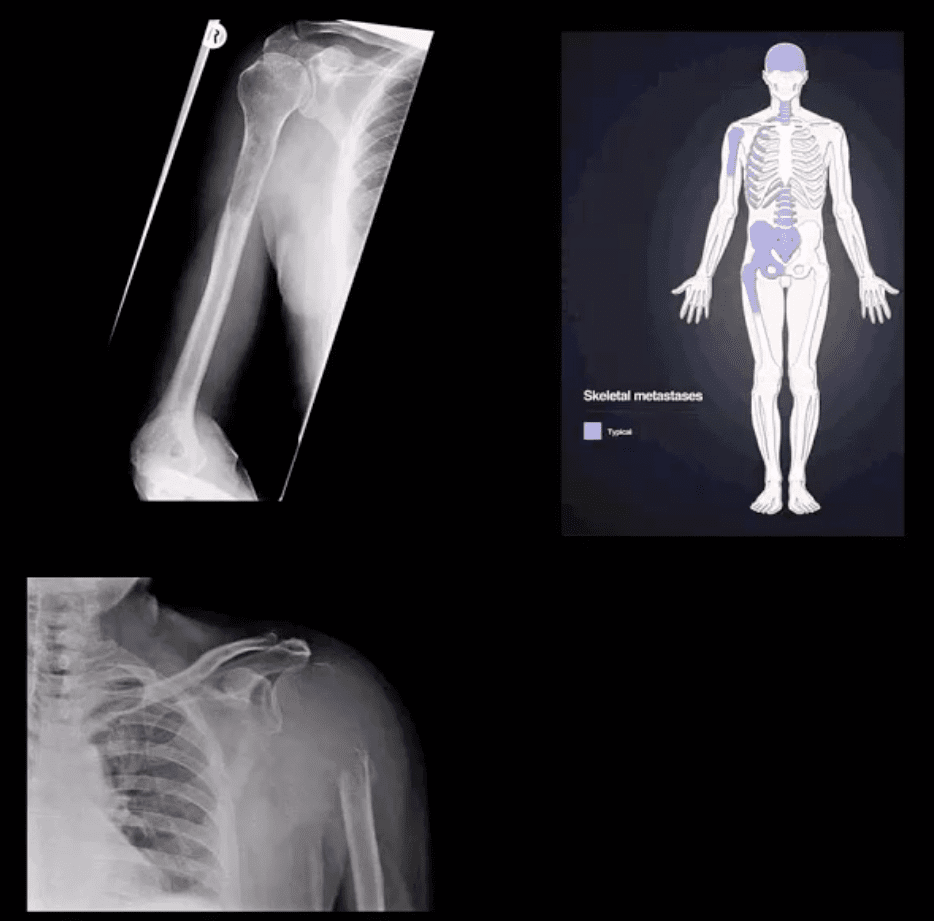
- In adults >40, bone Mets d/t lung, breast, renal cell, thyroid CA & prostate are the m/c causes. Clinically: may mimic pain resemblingRTC/joint changes. Should be evaluated carefully. Key to Dx: Hx, PE and Imaging esp.in pts with known primary
- Imaging: 1st step x-rays, MRI can help, Tc99bone scintigraphy helps to detect regional and distant disease. X-ray features: destructive lytic changes typically in prox humerus(red marrow) with or w/o path Fx. DDx: Mets, MM, lymphoma
- Clinically: night pain, pain at rest, etc. Lab tests: unrewarding, in severe cases hypercalcemia may be noted.
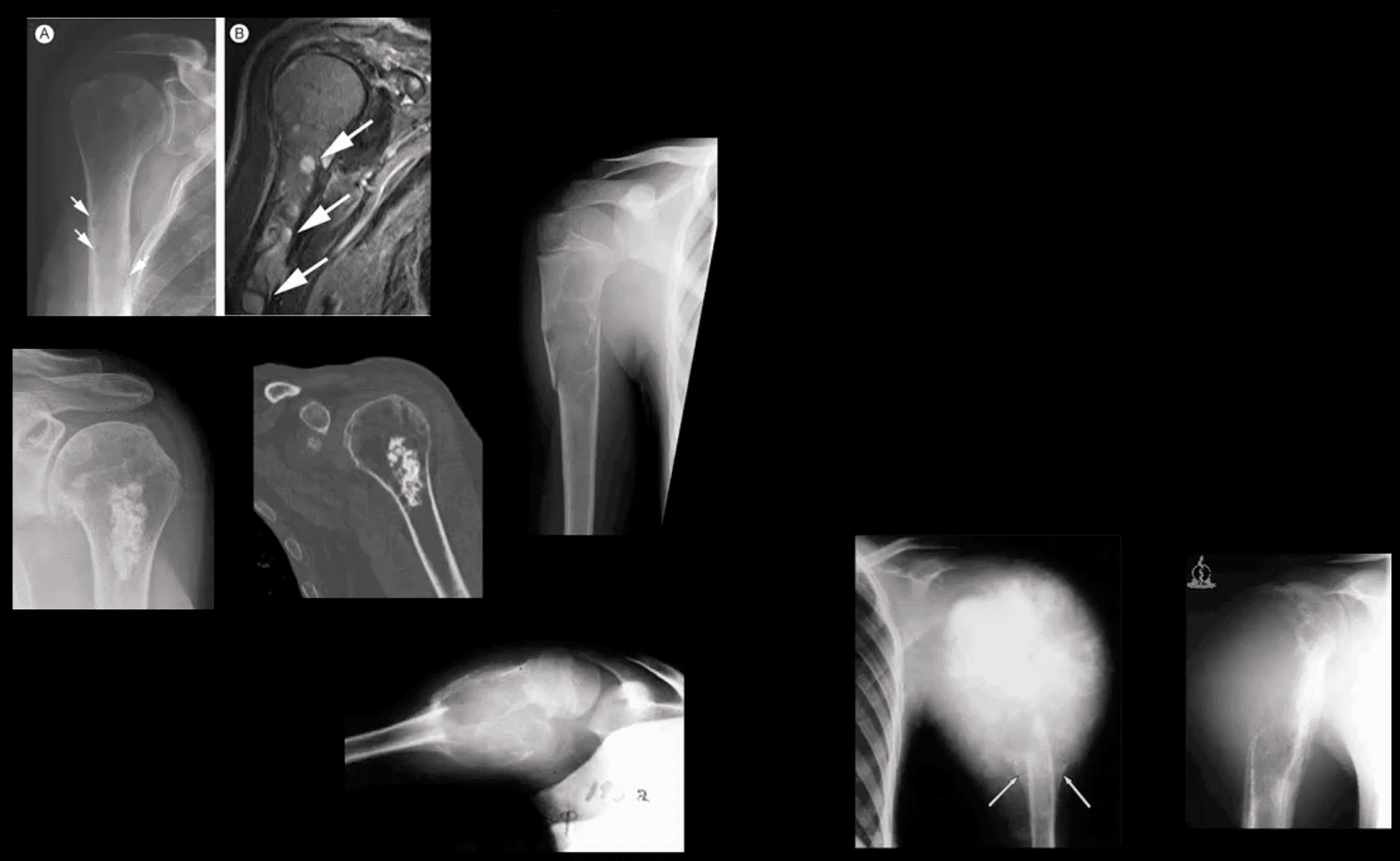
- Primary Malignant bone neoplasms (shoulder) Adults: M. Myeloma or Solitary plasmacytoma, Chondrosarcoma may transform from an enchondroma and some others. In children/teenagers: OSA vs. Ewing�s
- Primary benign bone neoplasms (shoulder). Adults: Enchondroma (patients in their 20-30s)GCT. In children: Simple bone cyst (Unicameral Bone cyst), Osteochondroma, Aneurysmal Bone Cyst, Chondroblastoma (rare)
- Imaging: 1st step x-radiography
- MRI is essential to Dx. Especially in cases of primary malignant neoplasms Evaluate extent, soft tissue invasion, preoperative planning, staging, etc.
General Disclaimer, Licenses and Board Certifications *
Professional Scope of Practice *
The information herein on "Shoulder Diagnostic Imaging Approach | El Paso, TX." is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and on our family practice-based chiromed.com site, focusing on naturally restoring health for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez, DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card








