Origin: The most common cause of�migraines/headaches�can relate to neck complications. From spending excessive time looking down at a laptop, desktop, iPad, and even from constant texting, an incorrect posture for extended periods of time can begin to place pressure on the neck and upper back leading to problems that can cause headaches. The majority of these type of headaches occurs as a result of tightness between the shoulder blades, which in turn causes the muscles on the top of the shoulders to also tighten and radiate pain into the head.
Contents
Origin Of Head Pain
- Arises from pain sensitive structures in the head
- Small diameter fibers (pain/temp) innervate
- Meninges
- Blood vessels
- Extracranial structures
- TMJ
- Eyes
- Sinuses
- Neck muscles and ligaments
- Dental structures
- The brain has no pain receptors
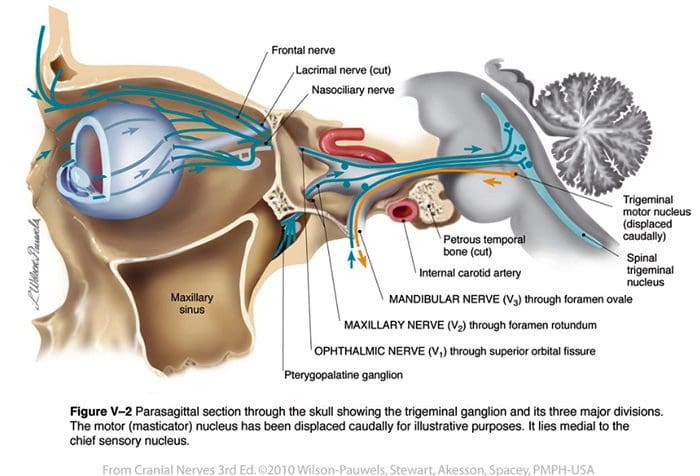
Spinal Trigeminal Nucleus
- Trigeminal nerve
- Facial nerve
- Glossopharyngeal nerve
- Vagus nerve
- C2 nerve (Greater occipital nerve)
Occipital Nerves
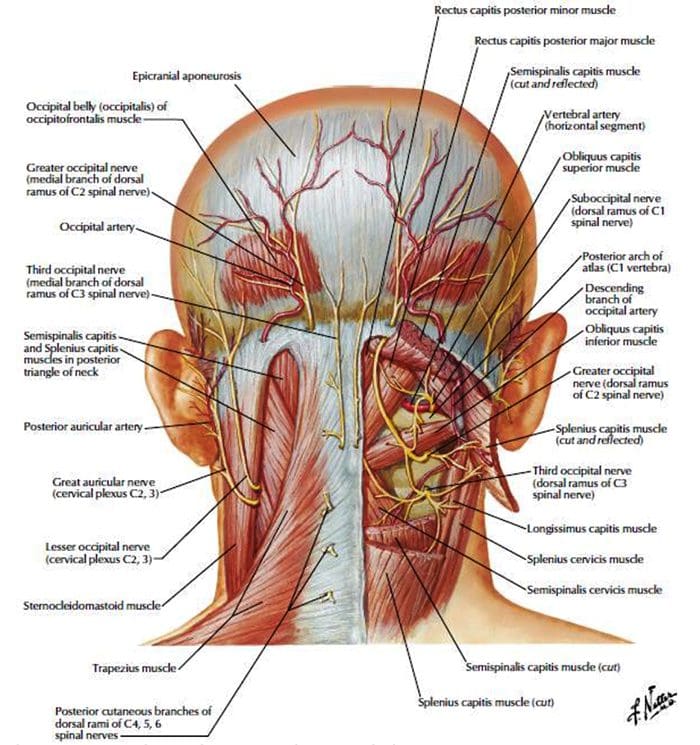 http://dailymedfact.com/neck-anatomy-the-suboccipital-triangle/
http://dailymedfact.com/neck-anatomy-the-suboccipital-triangle/
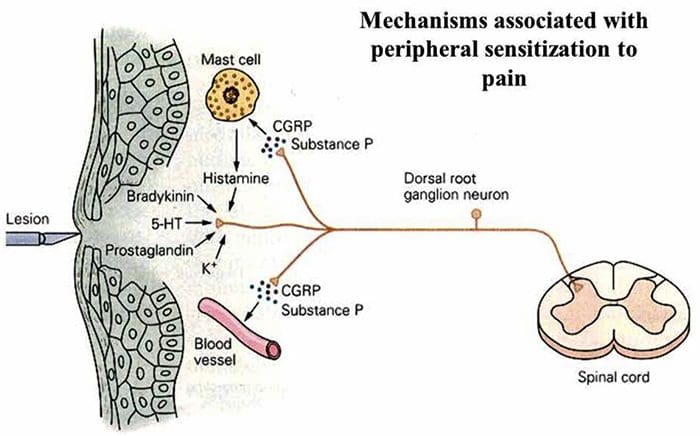
Sensitization Of Nociceptors
- Results in allodynia and hyperalgesia
Headache Types
Sinister:
- Meningeal irritation
- Intracranial mass lesions
- Vascular headaches
- Cervical fracture or malformation
- Metabolic
- Glaucoma
Benign:
- Migraine
- Cluster headaches
- Neuralgias
- Tension headache
- Secondary headaches
- Post-traumatic/post-concussion
- “Analgesic rebound” headache�
- Psychiatric
HA Due To Extracranial Lesions
- Sinuses (infection, tumor)
- Cervical spine disease
- Dental problems
- Temporomandibular joint
- Ear infections, etc.
- Eye (glaucoma, uveitis)
- Extracranial arteries
- Nerve lesions
HA Red Flags
Screen for red flags and consider dangerous HA types if present
Systemic symptoms:
- Weight loss
- Pain wakes them from sleep
- Fever
Neurologic symptoms or abnormal signs:
- Sudden or explosive onset
- New or Worsening HA type especially in older patients
- HA pain that is always in the same location
Previous headache history
- Is this the first HA you�ve ever had?
Is this the worst HA you�ve ever had?
Secondary risk factors:
- History of cancer, immunocompromised, etc.
Dangerous/Sinister Headaches
Meningeal irritation
- Subarachnoid hemorrhage
- Meningitis and meningoencephalitis
Intracranial mass lesions
- Neoplasms
- Intracerebral hemorrhage
- Subdural or epidural hemorrhage
- Abscess
- Acute hydrocephalus
Vascular headaches
- Temporal arteritis
- Hypertensive encephalopathy (e.g., malignant hypertension, pheochromocytoma)
- Arteriovenous malformations and expanding aneurysms
- Lupus cerebritis
- Venous sinus thrombosis
Cervical fracture or malformation
- Fracture or dislocation
- Occipital neuralgia
- Vertebral artery dissection
- Chiari malformation
Metabolic
- Hypoglycemia
- Hypercapnea
- Carbon monoxide
- Anoxia
- Anemia
- Vitamin A toxicity
Glaucoma
Subarachnoid Hemorrhage
- Usually due to ruptured aneurysm
- Sudden onset of severe pain
- Often vomiting
- Patient appears ill
- Often nuchal rigidity
- Refer for CT and possibly lumbar puncture
Meningitis
- Patient appears ill
- Fever
- Nuchal rigidity (except in elderly and young children)
- Refer for lumbar puncture – diagnostic
Neoplasms
- Unlikely cause of HA in average patient population
- Mild and nonspecific head pain
- Worse in the morning
- May be elicited by vigorous head shaking
- If focal symptoms, seizures, focal neurologic signs, or evidence of increased intracranial pressure are present rule our neoplasm
Subdural Or Epidural Hemorrhage
- Due to hypertension, trauma or defects in coagulation
- Most often occurs in the context of acute head trauma
- Onset of symptoms may be weeks or months after an injury
- Differentiate from the common post-concussion headache
- Post-Concussive HA may persist for weeks or months after an injury and be accompanied by dizziness or vertigo and mild mental changes, which will all subside
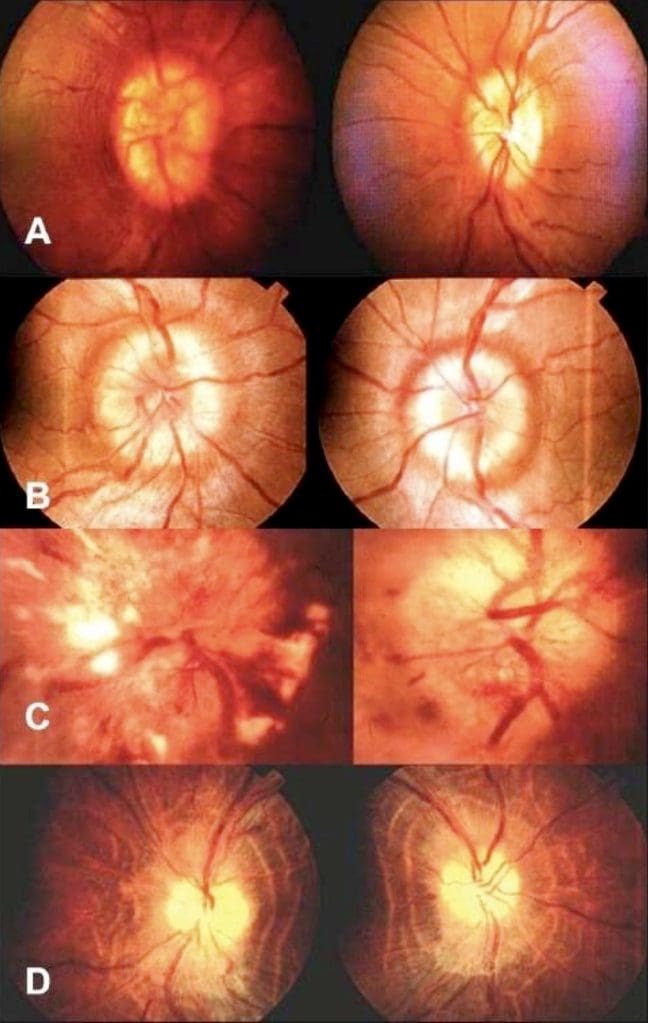
Increase Intracranial Pressure
- Papilledema
- May cause visual changes
Temporal (Giant-Cell) Arteritis
- >50 years old
- Polymyalgia rheumatic
- Malaise
- Proximal joint pains
- Myalgia
- Nonspecific headaches
- Exquisite tenderness and/or swelling over the temporal or occipital arteries
- Evidence of arterial insufficiency in the distribution of branches of the cranial vessels
- High ESR
Cervical Region HA
- Neck trauma or with symptoms or signs of cervical root or cord compression
- Order MR or CT cord compression due to fracture or dislocation
- Cervical instability
- Order cervical spine x-rays lateral flexion and extension views
Ruling Out Dangerous HA
- Rule our history of serious head or neck injury, seizures or focal neurologic symptoms, and infections that may predispose to meningitis or brain abscess
- Check for fever
- Measure blood pressure (concern if diastolic >120)
- Ophthalmoscopic exam
- Check neck for rigidity
- Auscultate for cranial bruits.
- Complete neurologic examination
- If needed order complete blood cell count, ESR, cranial or cervical imaging
Episodic Or Chronic?
<15 days per month = Episodic
>15 days per month = Chronic
Migraine HA
Generally due to dilation or distension of cerebral vasculature
Serotonin In Migraine
- AKA 5-hydroxytryptamine (5-HT)
- Serotonin becomes depleted in migraine episodes
- IV 5-HT can stop or reduce severity
Migraine With Aura
History of at least 2 attacks fulfilling the following criteria
One of the following fully reversible aura symptoms:
- Visual
- Somatic sensory
- Speech or language difficulty
- Motor
- Brain stem
2 of the following 4 characteristics:
- 1 aura symptom spreads gradually over ?5 min, and/or 2 symptoms occur in succession
- Each individual aura symptom lasts 5-60 min
- 1 aura symptom is unilateral
- Aura accompanied or followed in <60 min by headache
- Not better accounted for by another ICHD-3 diagnosis, and TIA excluded
Migraine Without Aura
History of at least 5 attacks fulfilling the following criteria:
- Headache attacks lasting 4-72 h (untreated or unsuccessfully treated)
- Unilateral pain
- Pulsing/pounding quality
- Moderate to severe pain intensity
- Aggravation by or causing avoidance of routine physical activity
- During headache nausea and/or sensitivity to light and sound
- Not better accounted for by another ICHD-3 diagnosis
Cluster Headache
- Severe unilateral orbital, supraorbital and/or temporal pain
- �Like an ice pick stabbing me the eye�
- Pain lasts 15-180 minutes
At least one of the following on the side of headache:
- Conjunctival injection
- Facial sweating
- Lacrimation
- Miosis
- Nasal congestion
- Ptosis
- Rhinorrhea
- Eyelid edema
- History of similar headaches in the past
Tension Headache
Headache pain accompanied by two of the following:
- Pressing/tightening (non-pulsing) quality
- �Feels like a band around my head�
- Bilateral location
- Not aggravated by routine physical activity
Headache should be lacking:
- Nausea or vomiting
- Photophobia and phonophobia (one or the other may be present)
- History of similar headaches in the past
Rebound Headache
- Headache occurring on ?15 days a month in a patient with a pre-existing headache disorder
- Regular overuse for >3 months of one or more drugs that can be taken for acute and/or symptomatic treatment of headache
- Due to medication overuse/withdrawal
- Not better accounted for by another ICHD-3 diagnosis
Sources
Alexander G. Reeves, A. & Swenson, R. Disorders of the Nervous System. Dartmouth, 2004.
General Disclaimer, Licenses and Board Certifications *
Professional Scope of Practice *
The information herein on "Origin Of Head Pain | El Paso, TX." is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and on our family practice-based chiromed.com site, focusing on naturally restoring health for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez, DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card