A migraine is a neurological condition commonly characterized by an intense, debilitating headache. Approximately 12 percent of the population in the United States suffers from migraines. Other symptoms may include: nausea, vomiting, difficulty speaking, numbness or tingling, and sensitivity to light and sound. Several factors can trigger a migraine. These include: stress, lack of food or sleep, exposure to light, hormonal changes in women and anxiety. Although healthcare professionals have yet to understand the true source of migraines, doctors of chiropractic have concluded that a spinal misalignment, or subluxation, may be associated with different types of headaches. The purpose of the following article is to demonstrate the results of a case of chronic migraine remission after a 72-year-old woman with a 60-year history of migraine headaches received chiropractic care.
Contents
A Case of Chronic Migraine Remission After Chiropractic Care
Abstract
- Objective: To present a case study of migraine sufferer who had a dramatic improvement after chiropractic spinal manipulative therapy (CSMT).
- Clinical features: The case presented is a 72-year�old woman with a 60-year history of migraine headaches, which included nausea, vomiting, photophobia, and phonophobia.
- Intervention and outcome: The average frequency of migraine episodes before treatment was 1 to 2 per week, including nausea, vomiting, photophobia, and phonophobia; and the average duration of each episode was 1 to 3 days. The patient was treated with CSMT. She reported all episodes being eliminated after CSMT. The patient was certain there had been no other lifestyle changes that could have contributed to her improvement. She also noted that the use of her medication was reduced by 100%. A 7-year follow-up revealed that the person had still not had a single migraine episode in this period.
- Conclusion: This case highlights that a subgroup of migraine patients may respond favorably to CSMT. While a case study does not represent significant scientific evidence, in context with other studies conducted, this study suggests that a trial of CSMT should be considered for chronic, nonresponsive migraine headache, especially if migraine patients are nonresponsive to pharmaceuticals or prefer to use other treatment methods.
- Key indexing terms: Migraine, Chiropractic, Spinal manipulative therapy
Dr. Alex Jimenez’s Insight
Migraine is a prevalent and debilitating condition which affects about 12 percent of the population in the U.S.� Furthermore, migraine affects more women than men. While the causes and symptoms of migraine headache pain have been identified, many healthcare professionals believe that a spinal misalignment, or subluxation, may often lead to various types of headaches. Chiropractic care utilizes spinal adjustments and manual manipulations to carefully correct the alignment of the spine, restoring proper structure and function. According to the research study below, chiropractic can be an effective migraine headache treatment. Chiropractic care is a safe and effective alternative treatment option for patients with migraine who seek a natural method and technique to reduce their symptoms without the use of drugs and/or medications.
Introduction
Migraine remains a common and debilitating condition.[1,2] It has an estimated incidence of 6% in males and 18% in females.[2] A study in Australia found the cost to industry to be an estimated $750 million.[3] Lipton et al found that migraine is one of the most frequent reasons for consultations with general practitioners, affecting between 12 million and 18 million people each year in the United States.[4] The estimated cost in the United States is $25 billion in lost productivity due to 156 million full-time work days being lost each year.[5] Recent information has suggested that these older figures above are still current, but also underestimated, because of many sufferers not stating their problem because of a perceived poor social stigma.[6]
The Brain Foundation in Australia notes that 23% of households contain at least one migraine sufferer. Nearly all migraine sufferers and 60% of those with tension-type headache experience reductions in social activities and work capacity. The direct and indirect costs of migraine alone would be about $1 billion per annum.[3]
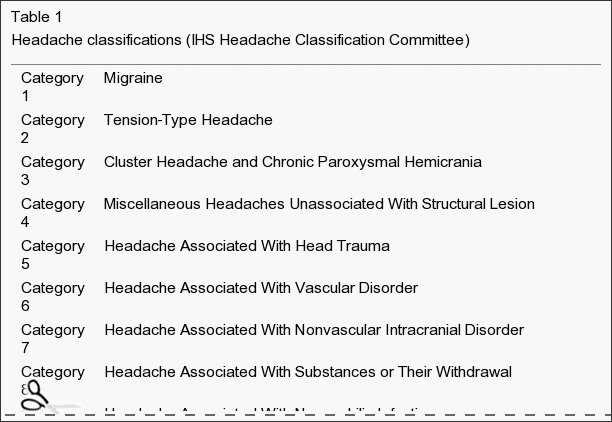
The Headache Classification Committee of the International Headache Society (IHS) defines migraines as having the following: unilateral location, pulsating quality, moderate or severe intensity, and aggravated by routine physical activity. During the headache, the person must also experience nausea and/or vomiting, photophobia, and/or phonophobia.[7] In addition, there is no suggestion either by history or by physical or neurologic examination that the person has a headache listed in groups 5 to 11 of their classification system.[7] Groups 5 to 11 of the classification system include headache associated with head trauma, vascular disorder, nonvascular intracranial disorder, substances or their withdrawal, noncephalic infection, or metabolic disorder, or with disorders of cranium, neck, eyes, nose, sinuses, teeth, mouth, or other facial or cranial structures.
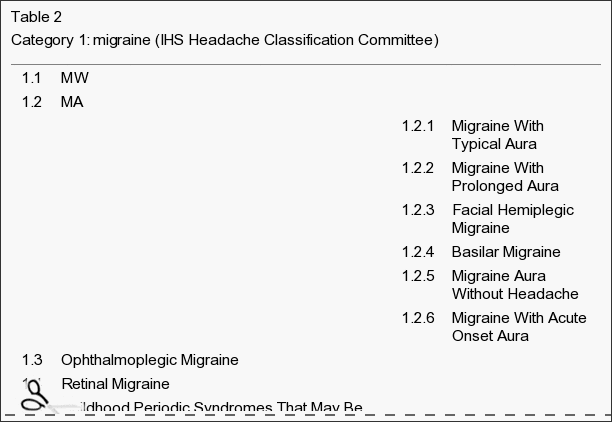
Some confusion relates to the �aura� feature that distinguishes migraine with aura (MA) and migraine without aura (MW). An aura usually consists of homonymous visual disturbances, unilateral paresthesias and/or numbness, unilateral weakness, aphasia, or unclassifiable speech difficulty.[7] Some migraineurs describe the aura as an opaque object, or a zigzag line around a cloud; even cases of tactile hallucinations have been recorded.[8] The new terms MA and MW replace the old terms classic migraine and common migraine, respectively.
The IHS diagnostic criteria for MA (category 1.2) is at least 3 of the following:
- 1) One or more fully reversible aura symptoms indicating focal cerebral cortex and/or brain stem dysfunction.
- 2) At least 1 aura symptom develops gradually over more than 4 minutes or 2 or more symptoms occurring in succession.
- 3) No aura symptom lasts more than 60 minutes.
- 4) Headache follows aura with a free interval of less than 60 minutes.
Migraine is often still nonresponsive to treatment.[9] However, several studies have demonstrated statistically significant reduction in migraines after chiropractic spinal manipulative therapy (CSMT).[10-15]
This article will discuss a patient presenting with MW and her response after CSMT. The discussion will also outline specific diagnostic criteria for migraine and other headaches relevant to chiropractors, osteopaths, or other health practitioners.
Case Report
A 72-year�old 61-kg white woman presented with migraine headaches that had commenced in early childhood (approximately 12 years old). The patient could not relate anything to the commencement of her migraines, although she believed there was a family history (father) of the condition. During the history, the patient stated that she suffered regular migraine headaches (1-2 per week) with which she also experienced nausea, vomiting, vertigo, and photophobia. She needed to cease activities to alleviate the symptoms, and she often required acetaminophen and codeine medication (25 mg) or sumatriptan succinate for pain relief. The patient was also taking verapamil (calcium ion antagonist, for essential hypertension), calcitriol (calcium uptake, for osteoporosis), pnuemenium on a daily basis, and carbamazipine (antiepileptic, neurotropic medication) twice daily.
The patient reported that an average episode lasted 1 to 3 days and that she could not perform activities of daily living for a minimum of 12 hours. In addition, a visual analogue scale score for an average episode was 8.5 out of a possible maximum score of 10, corresponding to a description of �terrible� pain. The patient noted that stress or tension would precipitate a migraine and that light and noise aggravated her condition. She described the migraine as a throbbing head pain located in the parietotemporal region and was always left-sided.
The patient had a previous history of a pulmonary embolism (2 years before treatment) and had a partial hysterectomy 4 years before treatment. She also stated she had hypertension that was controlled. She was a widow with 2 children, and she had never smoked. The patient had tried acupuncture, physiotherapy, substantial dental treatment, and numerous other medications; but nothing had changed her migraine pattern. She stated that she had never had previous chiropractic treatment. The patient also stated that she had been treated by a neurologist for �migraines� over many years.
On examination, she was found to have very sensitive suboccipital and upper cervical musculature and decreased range of motion at the joint between the occiput and first cervical vertebra (Occ-C1), coupled with pain on flexion and extension of the cervical spine. She also had significant reduction in thoracic spine motion and a marked increase in her thoracic kyphosis.
Blood pressure testing revealed she was hypertensive (178/94), which the patient reported was an average result (stage 2 hypertension using the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure 7 guidelines).
Based on the IHS Headache Classification Committee classification and diagnostic criteria, the patient had an MW�category 1.1, previously called common migraine (Table 1). This appeared secondary to moderate cervical segmental dysfunction with mild to moderate suboccipital and cervical paraspinal myofibrosis.
The patient received CSMT (diversified chiropractic �adjustments�) to her Occ-C1 joint, upper thoracic spine (T2 through T7), and the affected hypertonic musculature. Hypertonic muscles were released through gentle massage and stretching. An initial course of 8 treatments was conducted at a frequency of twice a week for 4 weeks. The treatment program also included recording several features for every migraine episode. This included frequency, visual analogue scores, episode duration, medication, and time before they could return to normal activities.
The patient reported a dramatic improvement after her first treatment and noticed a reduction in the intensity of her head and neck pain. This continued with the patient reporting having no migraines in the initial month course of treatment. Further treatment was recommended to increase her range of motion, increase muscle tone, and reduce suboccipital muscle tension. In addition, monitoring of her migraine symptoms was continued. A program of treatment at a frequency of once a week for a further 8 weeks was instigated. After the next phase of treatment, the patient noted much less neck tension, better movement, and no migraine. In addition, she no longer used pain-relieving medication (acetaminophen, codeine, and sumatriptan succinate) and noted that she did not experience nausea, vomiting, photophobia, or phonophobia (Table 2). The patient continued treatment at 2-weekly intervals and stated that, after 6 months, her migraine episodes had disappeared completely. In addition, she was no longer experiencing neck pain. Examination revealed no pain on active neck movement; however, a passive motion restriction at the C1-2 motion segment was still present.
The patient is currently having treatment every 4 weeks, and she still reports no return of her migraine episodes or neck pain. The patient has now not experienced any migraines for a period of more than 7 years since her last episode, which was immediately before her having her first chiropractic treatment.
Discussion
Case studies do not form high levels of scientific data. However, some cases do present significant findings. For example, cases with long (chronic) and/or severe symptomatology can highlight alternative treatment options. With case studies such as this, there is always a possibility that the symptoms spontaneously resolved, with no effective from the treatment. The case presented highlights a potential alternative treatment option. A 7-year follow-up revealed that the person had still not had a single migraine episode in this period. The patient was certain that there had been no other lifestyle changes that could have contributed to her improvement. She also noted that the migraines had stopped after her first treatment.
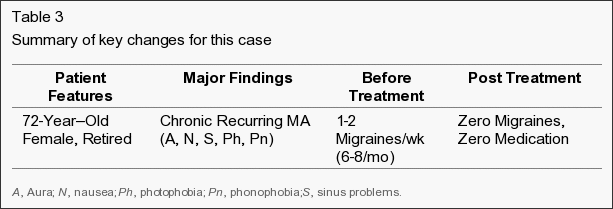
The average frequency of her migraines before treatment was 1 to 2 per week, with episodes that always included nausea, vomiting, photophobia, and phonophobia. In addition, the average duration of each episode was 1 to 3 days before her receiving CSMT. The person also noted that the use of her pain-relieving medication was also reduced by 100% (Table 3).
Migraines are a common and debilitating condition; yet because they have an uncertain etiology, the most appropriate treatment regime is often unclear.[16] Previous etiological models described vascular causes of migraine, where episodes seem to be initiated by a decreased blood flow to the cerebrum followed by extracranial vasodilation during the headache phase.[8] However, other etiological models seem connected with vascular changes related to neurologic changes and associated serotonergic disturbances.[9] Therefore, previous treatments have focused on pharmacological modification of blood flow or serotonin antagonist block.[17]
Studies examining the role of the cervical spine to headache (ie, �cervicogenic headache�) have been well described in the literature.[18-30] However, the relation of the cervical spine to migraine is less well documented.[10-15] Previous studies by this author have demonstrated an apparent reduction in migraines after CSMT.[10,11] In addition, other studies have suggested that CSMT may be an effective intervention for migraine.[14,15] Although, previous studies have some limitations (inaccurate diagnosis, overlapping symptoms, inadequate control groups), the level of evidence gives support for CSMT in migraine treatment.[11] However, practitioners need to be critically aware of potential overlap of diagnoses when reviewing migraine research or case studies on effectiveness of their treatment.[18-22] This is especially important in comparison of migraine patients who may be suitable for chiropractic manipulative therapy.[23-28]
Between 40% and 66% of patients with migraine, particularly those with severe or frequent migraine attacks, do not seek help from a physician.[29] Among those who do, many do not continue regular physician visits.[30] This may be due to patients’ perceived lack of empathy from the physician and a belief that physicians cannot effectively treat migraine. In a 1999 British survey, 17% of 9770 migraineurs had not consulted a physician because they believed their condition would not be taken seriously; and 8% had not seen a physician because they believed existing migraine medications were ineffective.[30] The most common reason for not seeking a physician’s advice (cited by 76% of patients) was the patients’ belief that they did not need a physician’s opinion to treat their migraine attacks.
The case was presented to assist practitioners making a more informed decision on the treatment of choice for migraines. The outcome of this case is also relevant in relation to other research that concludes that CSMT is a very effective treatment for some people. Practitioners could consider CSMT for migraine based on the following:
- 1) Limitation of passive neck movements.
- 2) Changes in neck muscle contour, texture, or response to active and passive stretching and contraction.
- 3) Abnormal tenderness of the suboccipital area.
- 4) Neck pain before or at the onset of the migraine.
- 5) Initial response to CSMT.
As with all case reports, results are limited in application to larger populations. Careful clinical decision making should be used when applying these results to other patients and clinical situations.
Conclusion
This case demonstrates that some migraine sufferers may respond well with manual therapies, which includes CSMT. Therefore, migraine patients who have not received a trial of CSMT should be encouraged to consider this treatment and assess any potential response. Where there are no contraindications to CSMT, an initial trial of treatment may be warranted. Following evidence-based medicine guidelines, medical practitioners should discuss CSMT with migraine patients as an option for treatment.[31,32] Subsequent studies should address this issue and the role that CSMT has in migraine management.
In conclusion, a�migraine is a debilitating and intense type of headache which is often accompanied by a variety of other symptoms. Although still misunderstood today, doctors of chiropractic have shown that a spinal misalignment, or subluxation may trigger migraine headaches. According to the article above, chiropractic care may effectively help individuals who suffer from migraine headaches. However, further research studies are required.�Information referenced from the National Center for Biotechnology Information (NCBI). The scope of our information is limited to chiropractic as well as to spinal injuries and conditions. To discuss the subject matter, please feel free to ask Dr. Jimenez or contact us at 915-850-0900 .
Curated by Dr. Alex Jimenez
Additional Topics: Back Pain
According to statistics, approximately 80% of people will experience symptoms of back pain at least once throughout their lifetimes. Back pain is a common complaint which can result due to a variety of injuries and/or conditions. Often times, the natural degeneration of the spine with age can cause back pain. Herniated discs occur when the soft, gel-like center of an intervertebral disc pushes through a tear in its surrounding, outer ring of cartilage, compressing and irritating the nerve roots. Disc herniations most commonly occur along the lower back, or lumbar spine, but they may also occur along the cervical spine, or neck. The impingement of the nerves found in the low back due to injury and/or an aggravated condition can lead to symptoms of sciatica.

EXTRA IMPORTANT TOPIC:�Neck Pain Treatment El Paso, TX Chiropractor
MORE TOPICS: EXTRA EXTRA: El Paso, Tx | Athletes
Blank
References
Close Accordion
General Disclaimer, Licenses and Board Certifications *
Professional Scope of Practice *
The information herein on "Migraine Headache Treatment in El Paso, TX" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and on our family practice-based chiromed.com site, focusing on naturally restoring health for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez, DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card