Have you ever experienced low back pain? If you haven’t already, there’s a high probability you will present at least one case of back pain sometime during your lifetime. Back pain is one of the most prevalent spine health issues reported among the population of the United States, affecting up to 80 percent of Americans at some point in their lives. Back pain is not a specific disease, rather it is a symptom which may develop as a result of a variety of injuries and/or conditions.�Although most cases typically resolve on their own, the effective treatment of acute low back pain is essential towards preventing chronic low back pain.
Chiropractors and physical therapists frequently utilize a similar series of treatment methods, such as spinal adjustments and manual manipulations as well as massage and physical therapy, to help treat symptoms of back and low back pain. Many healthcare professionals, however, have started using the McKenzie method to manage acute back pain. The purpose of the following article is to educate patients on the effectiveness of the McKenzie method for acute non-specific low back pain.
Contents
The McKenzie Method for the Management of Acute Non-Specific Low Back Pain: Design of a Randomised Controlled Trial
Abstract
Background
Low back pain (LBP) is a major health problem. Effective treatment of acute LBP is important because it prevents patients from developing chronic LBP, the stage of LBP that requires costly and more complex treatment.
Physiotherapists commonly use a system of diagnosis and exercise prescription called the McKenzie Method to manage patients with LBP. However, there is insufficient evidence to support the use of the McKenzie Method for these patients. We have designed a randomised controlled trial to evaluate whether the addition of the McKenzie Method to general practitioner care results in better outcomes than general practitioner care alone for patients with acute LBP.
Methods/Design
This paper describes the protocol for a trial examining the effects of the McKenzie Method in the treatment of acute non-specific LBP. One hundred and forty eight participants who present to general medical practitioners with a new episode of acute non-specific LBP will be randomised to receive general practitioner care or general practitioner care plus a program of care based on the McKenzie Method. The primary outcomes are average pain during week 1, pain at week 1 and 3 and global perceived effect at week 3.
Discussion
This trial will provide the first rigorous test of the effectiveness of the McKenzie Method for acute non-specific LBP.
Background
In Australia, low back pain (LBP) is the most frequently seen musculoskeletal condition in general practice and the seventh most frequent reason for consulting a physician[1,2]. According to the Australian National Health Survey, 21% of Australians reported back pain in 2001; additionally, the Australian Bureau of Statistic’s 1998 Survey of Disability, Ageing and Carers estimated that over one million Australians suffer from some form of disability associated with back problems[1].
LBP poses an enormous economic burden to society in countries such as the USA, UK and The Netherlands[3]. In the largest state in Australia, New South Wales, back injuries account for 30% of the cost of workplace injuries, with a gross incurred cost of $229 million in 2002/03[4]. It is expected that most people with an acute episode of LBP will improve rapidly, but a proportion of patients will develop persistent lower levels of pain and disability[5,6]. Those patients with chronic complaints are responsible for most of the costs[6]. Effective treatment of acute LBP is important because it prevents patients from developing chronic LBP, the stage of LBP that requires costly and more complex treatment.
There is a growing concern about effectiveness of treatments for LBP, as reflected in the large number of systematic reviews published in the last 5 years addressing this issue. [7-12]. Despite the large amount of evidence regarding LBP management, a definitive conclusion on which is the most appropriate intervention is not yet available. A comparison of 11 international clinical practice guidelines for the management of LBP showed that the provision of advice and information, together with analgesics and NSAIDs, is the approach consistently recommended for patients with an acute episode[13]. Most guidelines do not recommend specific exercises for acute LBP because trials to date have concluded that it is not more effective than other active treatments, or than inactive or placebo treatments[8]. However, some authors have suggested that the negative results observed in trials of exercises are a consequence of applying the same exercise therapy to heterogeneous groups of patients. [14-16]. This hypothesis has some support from a recent high-quality randomised trial in which treatment based on a diagnostic classification system led to larger reductions in disability and promoted faster return to work in patients with acute LBP than the therapy recommended by the clinical guidelines[17].
In 1981, McKenzie proposed a classification system and a classification-based treatment for LBP labelled Mechanical Diagnosis and Treatment (MDT), or simply McKenzie Method[18]. Of the large number of classification schemes developed in the last 20 years [19-26], the McKenzie Method has the greatest empirical support (e.g. validity, reliability and generalisability) among the systems based on clinical features[27] and therefore seems to be the most promising classification system for implementation in clinical practice.
Physiotherapists commonly adopt the McKenzie Method for treating patients with LBP[28,29]. A survey of 293 physiotherapists in 1994 found that 85% of them perceived the McKenzie Method as moderately to very effective[28]. Nevertheless, a recent systematic review concluded that there is insufficient evidence to evaluate the effectiveness of the McKenzie Method for patients with LBP [30]. A critical concern is that most trials to date have not implemented the McKenzie Method appropriately. The most common flaw is that all trial participants are given the same intervention regardless of classification, an approach contradictory to the principles of McKenzie therapy.
The primary aim of this trial is to evaluate whether the addition of the McKenzie Method to general practitioner (GP) care results in better outcomes than GP care alone for patients with acute non-specific LBP when effect is measured in terms pain, disability, global perceived effect, and persistent symptoms.
Methods
The University of Sydney Human Research Ethics Committee granted approval for this study.
Study Sample
One hundred and forty eight participants with a new episode of acute non-specific LBP who present to GPs will be recruited for the study. A new episode of LBP will be defined as an episode of pain lasting longer than 24 hours, preceded by a period of at least one month without LBP and in which the patient did not consult a health care practitioner[31]. Participants will be screened for eligibility at their first appointment with the GP according to the inclusion and exclusion criteria.
Inclusion Criteria
To be eligible for inclusion, participants must have pain extending in an area between the twelfth rib and buttock crease (this may or may not be accompanied by leg pain); pain of at least 24 hours duration; pain of less than 6 weeks duration; and they need to be eligible for referral to private physiotherapy practice within 48 hours.
Exclusion Criteria
Participants will be excluded if they have one of the following conditions: nerve root compromise (defined as 2 positive tests out of sensation, power and reflexes for the same spinal nerve root); known or suspected serious spinal pathology; spinal surgery within the preceding 6 months; pregnancy; severe cardiovascular or metabolic disease; or inability to read and understand English.
Recruiting GPs will record the number of patients who are invited to participate, the number who decline to participate, and the number of screened patients who are ineligible and their reasons for declining participation or ineligibility. Written consent will be obtained for each participant.
Subjects who volunteer to participate and satisfy the eligibility criteria will receive baseline treatment and then be randomly allocated to one of the study groups. To ensure equal-sized treatment groups, random permuted blocks of 4�8 participants will be used[32]. Randomisation will be stratified by Workcover compensation status. The stratified random allocation schedule will be generated by a person not otherwise involved in recruitment, assessment or treatment of subjects and the randomisation sequence will be placed in sequentially numbered, sealed envelopes. The flow of participants through the study is detailed in Figure ?1.
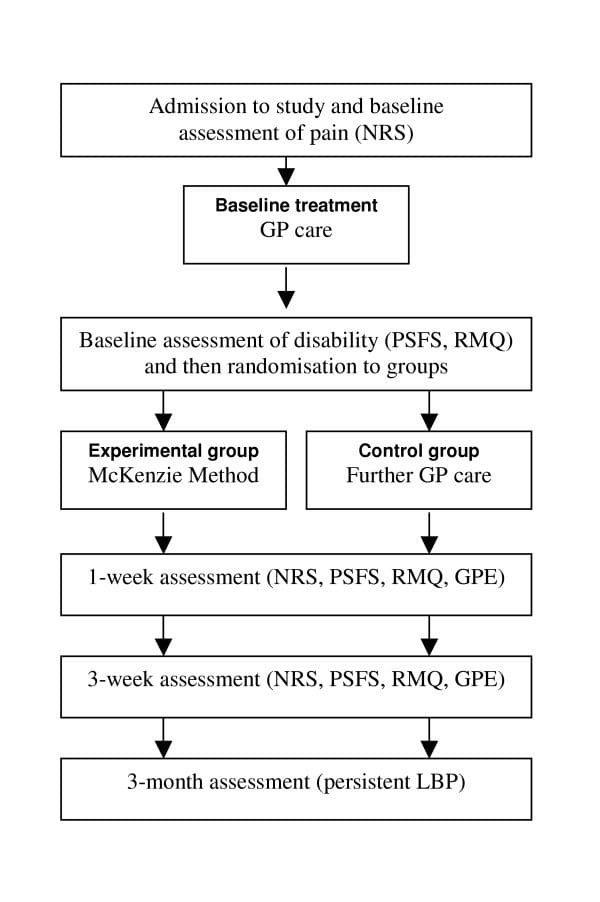
Figure 1: Flow of participants through the study. Legend: GP � General practitioner; NRS � Numeric pain rating scale; PSFS � Patient-specific functional scale; RMQ � Roland-Morris questionnaire; GPE � Global perceived effect; LBP � Low back pain.
Dr. Alex Jimenez’s Insight
In the management of low back pain, the attitudes, beliefs and treatment preferences of chiropractors, as well as that of physical therapists, can determine the most effective outcome measures in the care of patients with different types of spinal health issues. According to the following evidence-based research studies, the McKenzie method has been deemed to be one of the most useful treatment approaches for managing symptoms in patients with back and low back pain. Exercise and physical activity is also one of the most common treatment preferences for improving an individual’s strength, mobility and flexibility. Every healthcare professional varies in respect to their specific treatment preferences. These variations emphasize the need to identify the most effective treatment approach to guarantee proper treatment of LBP.
Outcome Measures
The McKenzie protocol is thought to promote rapid symptom improvement in patients with LBP[33,34] and this is one of the reasons that therapists choose this therapy. Therefore it is important to focus assessment on short-term outcomes. The primary outcomes will be:
- Usual pain intensity over last 24 hours recorded each morning in a pain diary over the first week. Pain will be measured on a 0�10 numerical rating scale (NRS). The unit of analysis will be the mean of the 7 measures[35];
- Usual pain intensity over last 24 hours (0�10 NRS) recorded at 1 and 3 weeks[35];
- Global perceived effect (0�10 GPE) recorded at 3 weeks.
The secondary outcomes will be:
- Global perceived effect (0�10 GPE) recorded at 1 week;
- Patient-generated measure of disability (Patient-Specific Functional Scale; PSFS) recorded at 1 and 3 weeks[36];
- Condition-specific measure of disability (Roland Morris Questionnaire; RMQ) recorded at 1 and 3 weeks[37];
- Number of patients reporting persistent back pain at 3 months.
Following the screening consultation in which the inclusion and exclusion criteria are assessed, the GP will supervise the baseline measurement of pain. All patients will then receive an assessment booklet and a pre-paid envelope in which all other self-assessed outcome measures are to be recorded and sealed. One member of the research team will contact patients by telephone within 24 hours of the consultation with the GP in order to give explanations regarding the appropriate form of filling in the assessment booklet. At this time, other baseline outcomes will be recorded and then the patient will be randomised to study groups. The patient will be advised to keep the booklet at home, to seal it into the pre-paid envelope after the final assessment and mail the sealed envelope to the research team. To ensure the proper use of the assessment booklet and to avoid loss of data due to non-returned booklets, a blinded assessor will contact all patients by telephone 9 and 22 days after the consultation with the GP to collect patient’s answers from the 1st week and 3rd week assessments, respectively.
The procedure for obtaining outcome data will be followed for all participants, regardless of compliance with trial protocols. At 3 months, data regarding the presence of persistent (chronic) symptoms will be collected by telephone. Participants will be asked to answer the following yes-no question: “During the past 3 months have you ever been completely free of low back pain? By this I mean no low back pain at all and would this pain-free period have lasted for a whole month”. Those answering no will be considered to have persistent LBP. Information on additional treatment and the direct costs with low back pain management will also be collected at 3 months.
A secondary analysis will be performed on predictors of response to McKenzie treatment and prediction of chronicity. This will involve the measurement of participants’ expectation about the helpfulness of both treatments under investigation as well as information on the occurrence of the centralisation phenomenon. Expectation will be recorded prior to randomisation according to the procedures described by Kalauokalani et al[38].
Treatments
All participants will receive GP care as advocated by the NHMRC guideline for the management of acute musculoskeletal pain[2]. Guideline-based GP care consists of providing information on a favourable prognosis of acute LBP and advising patients to stay active, together with the prescription of paracetamol. Patients randomised to the experimental group will be referred to physiotherapy to receive the McKenzie Method. A research assistant not involved in the assessment or treatment of subjects will be responsible for the randomisation process and will contact therapists and patients to arrange the first physiotherapy session. The McKenzie treatment will be delivered by credentialed physiotherapists who will follow the treatment principles described in McKenzie’s text book[18]. All therapists will have completed the four basic courses taught by the McKenzie Institute International. To ensure the appropriate implementation of the McKenzie’s classification algorithm, a training session with a member of McKenzie’s educational program will be conducted prior to the commencement of the study. The treatment frequency will be at the discretion of the therapist with a maximum of 7 sessions over 3 weeks. We chose to restrict the McKenzie treatment to a maximum of 7 sessions based on the study of Werneke and colleagues[39], which concluded that further reductions in pain and function are not expected if favourable changes in pain location are not present until the seventh treatment visit. Treatment procedures from the McKenzie Method are summarised in the Appendix.
Participants randomised to the control group will continue their GP care as usual. All participants regardless of intervention group will be advised not to seek other treatments for their low back pain during the treatment period. Physiotherapists will be asked to withhold co-interventions during the course of the trial.
Several mechanisms will be used to ensure that the trial protocol is applied consistently. Protocol manuals will be developed and all involved researchers (GPs, physiotherapists, assessor, and statistician) will be trained to ensure that screening, assessment, random allocation and treatment procedures are conducted according to the protocol. A random sample of treatment sessions will be audited to check that treatment is being administered according to the protocol.

Data Analysis
Power was calculated based on the primary outcome measures (pain intensity and global perceived effect). A sample size of 148 participants will provide 80% power to detect a difference of 1 unit (15%) on a 0�10 pain scale (SD = 2.0) between the experimental and control groups, assuming alpha of 0.05. This allows for loss to follow-up of 15%. This sample size also allows the detection of a difference of 1.2 units (12%) on a 0�10 global perceived effect scale (SD = 2.4).
Data will be analysed by a research member blinded to group status. The primary analysis will be by intention-to-treat. In order to estimate treatment effects, between-group mean differences (95%CI) will be calculated for all outcome measures. In the primary analysis these will be calculated using linear models that include baseline values of outcome variables as covariates to maximise precision.
Discussion
We have presented the rationale and design of an RCT evaluating the effects of the McKenzie Method in the treatment of acute non-specific LBP. The results of this trial will be presented as soon as they are available.
Competing Interests
The author(s) declare that they have no competing interests.
Authors’ Contributions
LACM, CGM and RDH were responsible for the design of the study. HC was responsible for recruiting McKenzie therapists and she will also participate as a clinician in the trial. LACM and JMc will act as trial coordinators. All authors have read and approved the final manuscript.
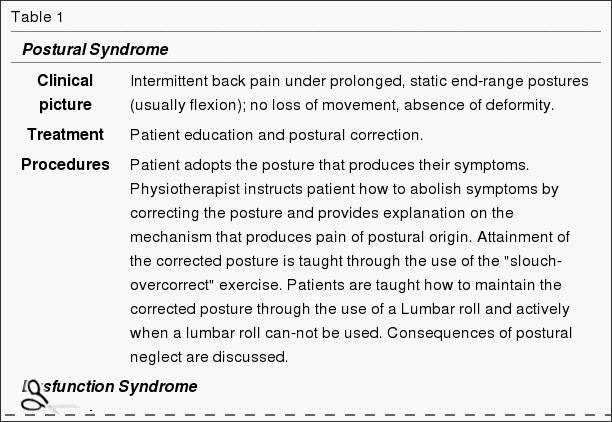
Appendix
Clinical picture and treatment principles according to the McKenzie Method
This table summarises the procedures involved in the McKenzie Method (Table 1). For detailed description of all procedures and progressions, refer to McKenzie’s text book. This is particularly important for Derangement syndrome since the treatment is extremely variable and complex and the full description of procedures would not be appropriate for the purposes of this paper.
Pre-Publication History
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1471-2474/6/50/prepub
Acknowledgements
The authors thank the physiotherapists credentialed in the McKenzie Method for their participation in this project.
Managing Low Back Pain: Attitudes & Treatment Preferences of Physical Therapists & Chiropractors
Abstract
Background and Purpose:�Researchers surveyed physical therapists about their attitudes, beliefs, and treatment preferences in caring for patients with different types of low back pain problems.
Subjects and Methods: Questionnaires were mailed to all 71 therapists employed by a large health maintenance organization in western Washington and to a random sample of 331 other therapists licensed in the state of Washington.
Results: Responses were received from 293 (74%) of the therapists surveyed, and 186 of these claimed to be practicing in settings in which they treat patients who have back pain. Back pain was estimated to account for 45% of patient visits. The McKenzie method was deemed the most useful approach for managing patients with back pain, and education in body mechanics, stretching, strengthening exercises, and aerobic exercises were among the most common treatment preferences. There were significant variations among therapists in private practice, hospital-operated, and health maintenance organization settings with respect to treatment preferences, willingness to take advantage of the placebo effect, and mean number of visits for patients with back pain.
Conclusions and Discussion: These variations emphasize the need for more outcomes research to identify the most effective treatment approaches and to guide clinical practice.
In conclusion,�the effective treatment of acute low back pain is essential because it can potentially help prevent the development of chronic low back pain. A growing number of chiropractors and physical therapists, including other healthcare professionals, have utilized the McKenzie method to help manage acute non-specific low back pain in patients. According to the research study, further evidence is required to support the use of the McKenzie method for LBP, however, the outcome measures of the research study regarding the effectiveness of the McKenzie method for low back pain are promising. Information referenced from the National Center for Biotechnology Information (NCBI). The scope of our information is limited to chiropractic as well as to spinal injuries and conditions. To discuss the subject matter, please feel free to ask Dr. Jimenez or contact us at 915-850-0900 .
Curated by Dr. Alex Jimenez

Additional Topics: Sciatica
Sciatica is referred to as a collection of symptoms rather than a single type of injury or condition. The symptoms are characterized as radiating pain, numbness and tingling sensations from the sciatic nerve in the lower back, down the buttocks and thighs and through one or both legs and into the feet. Sciatica is commonly the result of irritation, inflammation or compression of the largest nerve in the human body, generally due to a herniated disc or bone spur.

IMPORTANT TOPIC: EXTRA EXTRA: Treating Sciatica Pain
Blank
References
- Australian Institute of Health and Welfare . Australia’s health 2004. 1st. Camberra , AIHW; 2004.
- Australian Acute Musculoskeletal Pain Guidelines Group Evidence-based management of acute musculoskeletal pain. . 2003. http://www.nhmrc.gov.au
- Maetzel A, Li L. The economic burden of low back pain: a review of studies published between 1996 and 2001. Best Pract Res Clin Rheumatol. 2002;16:23�30. doi: 10.1053/berh.2001.0204. [PubMed] [Cross Ref]
- WorkCover Authority NSW . Statistical Bulletin. NSW Workers Compensation 2002/03. Sydney , The WorkCover Authority NSW ; 2003.
- Pengel LH, Herbert RD, Maher CG, Kathryn RM. Acute low back pain: Systematic review of its prognosis. BMJ. 2003;327:1�5. [PMC free article] [PubMed]
- Thomas E, Silman AJ, Croft PR, Papageorgiou AC, Jayson M, Macfarlane GJ. Predicting who develops chronic low back pain in primary care: a prospective study. BMJ. 1999;318:1662�1667. [PMC free article] [PubMed]
- Guzm�n J, Esmail R, Karjalainen K, Malmivaara A, Irvin E, Bombardier C. Multidisciplinary rehabilitation for chronic low back pain: systematic review. BMJ. 2001;322:1511�1516. doi: 10.1136/bmj.322.7301.1511. [PMC free article] [PubMed] [Cross Ref]
- van Tulder M, Malmivaara A, Esmail R, Koes B. Exercise therapy for low back pain. A systematic review within the framework of the Cochrane Collaboration Back Review Group. Spine. 2000;25:2784�2796. doi: 10.1097/00007632-200011010-00011. [PubMed] [Cross Ref]
- van Tulder M, Ostelo R, Vlaeyen JWS, Linton SJ, Morley SJ, Assendelft WJJ. Behavioral treatment for chronic low back pain. A systematic review within the framework of the Cochrane Back Review Group. Spine. 2000;25:2688�2699. doi: 10.1097/00007632-200010150-00024. [PubMed] [Cross Ref]
- Jellema P, van Tulder MW, van Poppel MN, Nachemson AL, Bouter LM. Lumbar supports for prevention and treatment of low back pain. A systematic review within the framework of the Cochrane Back Review Group. Spine. 2001;26:377�386. doi: 10.1097/00007632-200102150-00014. [PubMed] [Cross Ref]
- Ferreira ML, Ferreira PH, Latimer J, Herbert RD, Maher CG. Does spinal manipulative therapy help people with chronic low back pain? Aust J Physiother. 2002;48:277�284. [PubMed]
- Pengel HM, Maher CG, Refshauge KM. Systematic review of conservative interventions for subacute low back pain. Clin Rehabil. 2002;16:811�820. doi: 10.1191/0269215502cr562oa. [PubMed] [Cross Ref]
- Koes BW, van Tulder MW, Ostelo R, Burton K, Waddell G. Clinical guidelines for the management of low back pain in primary care: an international comparison. Spine. 2001;26:2504�2514. doi: 10.1097/00007632-200111150-00022. [PubMed] [Cross Ref]
- Borkan J, Koes B, Reis S, Cherkin DC. A report from the Second International Forum for Primary Care Research on low back pain: reexamining priorities. Spine. 1998;23:1992�1996. doi: 10.1097/00007632-199809150-00016. [PubMed] [Cross Ref]
- Bouter LM, van Tulder MW, Koes BW. Methodologic issues in low back pain research in primary care. Spine. 1998;23:2014�2020. doi: 10.1097/00007632-199809150-00019. [PubMed] [Cross Ref]
- Leboeuf-Yde C, Lauritsen JM, Lauritzen T. Why has the search for causes of low back pain largely been nonconclusive? Spine. 1997;22:877�881. doi: 10.1097/00007632-199704150-00010. [PubMed] [Cross Ref]
- Fritz JM, Delitto A, Erhard RE. Comparison of classification-based physical therapy with therapy based on clinical practice guidelines for patients with acute low back pain. Spine. 2003;28:1363�1372. doi: 10.1097/00007632-200307010-00003. [PubMed] [Cross Ref]
- McKenzie R, May S. The lumbar spine. Mechanical diagnosis & therapy. 2nd. Vol. 1. Waikanae , Spinal Publications New Zealand Ltd; 2003. p. 374.
- van Dillen LR, Sahrmann SA, Norton BJ, Caldwell CA, McDonnell MK, Bloom NJ. Movement system impairment-based categories for low back pain: stage 1 validation. J Orthop Sports Phys Ther. 2003;33:126�142. [PubMed]
- BenDebba M, Torgerson WS, Long DM. A validated, practical classification procedure for many persistent low back pain patients. Pain. 2000;87:89�97. doi: 10.1016/S0304-3959(00)00278-5. [PubMed] [Cross Ref]
- Delitto A, Erhard RE, Bowling RW, DeRosa CP, Greathouse DG. A treatment-based classification approach to low back syndrome: identifying and staging patients for conservative treatment. Phys Ther. 1995;75:470�485. [PubMed]
- Klapow JC, Slater MA, Patterson TL, Doctor JN, Atkinson JH, Garfin SR. An empirical evaluation of multidimensional clinical outcome in chronic low back pain patients. Pain. 1993;55:107�118. doi: 10.1016/0304-3959(93)90190-Z. [PubMed] [Cross Ref]
- Laslett M, van Wijmen P. Low back and referred pain: diagnosis and proposed new system of classification. N Z J Physiother. 1999;27:5�14.
- Maluf KS, Sahrmann SA, van Dillen LR. Use of a classification system to guide nonsurgical management of a patient with chronic low back pain. Phys Ther. 2000;80:1097�1111. [PubMed]
- Petersen T, Laslett M, Thorsen H, Manniche C, Ekdahl C, Jacobsen S. Diagnostic classification of non-specific low back pain. A new system integrating patho-anatomic and clinical categories. Physiother Theory Pract. 2003;19:213�237.
- Stiefel F, deJonge P, Huyse F, al INTERMED – An assessment and classification system for case complexity: Results in patients with low back pain. Spine. 1999;24:378�384. doi: 10.1097/00007632-199902150-00017. [PubMed] [Cross Ref]
- McCarthy CJ, Arnall FA, Strimpakos N, Freemont A, Oldham JA. The biopsychosocial classification of non-specific low back pain: a systematic review. Phys Ther Rev. 2004;9:17�30. doi: 10.1179/108331904225003955. [Cross Ref]
- Batti� MC, Cherkin DC, Dunn R, Ciol MA, Wheeler KJ. Managing low back pain: attitudes and treatment preferences of physical therapists. Phys Ther. 1994;74:219�226. [PubMed]
- Li LC, Bombardier C. Physical therapy management of low back pain: An exploratory survey of therapist approaches. Phys Ther. 2001;81:1018�1028. [PubMed]
- Machado LAC, de Souza MS, Ferreira PH, Ferreira ML. The McKenzie protocol for low back pain: a systematic review of the literature with a meta-analysis approach. Spine (in press) 2005. [PubMed]
- de Vet HCWPD, Heymans MWMS, Dunn KMMP, Pope DPPD, van der Beek AJPD, Macfarlane GJPD, Bouter LMPD, Croft PRPD. Episodes of Low Back Pain: A Proposal for Uniform Definitions to Be Used in Research. Spine. 2002;27:2409�2416. doi: 10.1097/00007632-200211010-00016. [PubMed] [Cross Ref]
- Pocock SJ. Clinical trials. A practical approach. 1st. Chichester , John Wiley & Sons; 1984.
- Delitto A, Cibulka MT, Erhard RE, Bowling RW, Tenhula JA. Evidence for use of an extension-mobilization category in acute low back syndrome: A prescriptive validation pilot study. Phys Ther. 1993;73:216�228. [PubMed]
- Schenk RJ, Jozefczyk C, Kopf A. A randomized trial comparing interventions in patients with lumbar posterior derangement. J Manual Manip Ther. 2003;11:95�102.
- Farrar J, Young J, LaMoreaux L, al Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94:149�158. doi: 10.1016/S0304-3959(01)00349-9. [PubMed] [Cross Ref]
- Stratford P, Gill C, Westaway M, Binkley J. Assessing disability and change on individual patients: a report of a patient specific measure. Physiother Can. 1995;47:258�263.
- Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine. 1983;8:141�144. [PubMed]
- Kalauokalani D, Cherkin D, Sherman K, Koepsell T, R D. Lessons from a trial of acupuncture and massage for low back pain. Spine. 2001;26:1418�1424. doi: 10.1097/00007632-200107010-00005. [PubMed] [Cross Ref]
- Werneke M, Hart DL, Cook D. A descriptive study of the centralization phenomenon. A prospective analysis. Spine. 1999;24:676�683. doi: 10.1097/00007632-199904010-00012. [PubMed] [Cross Ref]
Close Accordion
General Disclaimer, Licenses and Board Certifications *
Professional Scope of Practice *
The information herein on "McKenzie Therapy for Acute Non-Specific Low Back Pain" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and on our family practice-based chiromed.com site, focusing on naturally restoring health for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez, DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card