The previous rehab masterclass on Lisfrancs injuries highlighted the pathogenesis of injuries, the midfoot joint’s relevant factors, and typical injury mechanisms were presented along with diagnostic findings. In this masterclass scientific specialist Dr. Alexander Jimenez discusses the management of Lisfranc injuries…
Contents
Management
After the initial injury, it may not be clear exactly what harm the foot has been done to by the athlete. Both athlete and sports medicine staff may confuse. The athlete with subtle stage 1-type injuries will try to ‘run off’ the pain. As they continue and fail to reevaluate they will stop training/competition.
When an injury into the Lisfranc is suspected, the first MTP joint ought to be assessed to exclude a ‘toe’ injury and the ankle checked to exclude an ankle injury. They crutches till they could be properly analyzed and remain non-weightbearing ideally with an Aircast boot and need to ice the foot aggressively.
Non-operative�Treatment of Lisfranc Injuries
A stage 1 accident that’s functionally secure could be handled with a non-weight posture boot or cast for a first two weeks. They can be analyzed for tenderness on palpation over the TMT joint at this time and follow-up x-rays will be required to exclude any latent diastasis of the second and first metatarsal space. If pain-free on palpation and x ray is normal, they could have the weight bearing status assessed using complete weight bearing foot flat and position is raised by a toe. If that is normal they can stay out of the boot using a custom made orthotic and rehabilitation and return to conditioning may begin.
Then the boot is reapplied, if the foot stays painful to palpate or if they neglect raise test and they stay non weight bearing to partial weight bearing for a further four weeks.
For pain along with weightbearing status they’re reassessed in the stage. If these are uneventful then the rehabilitation and reconditioning stream is moved to by the athlete. If problematic they need to be assessed for postponed stabilisation.
The time period to get a injury that is secure could be a month recovery until return to play.
Operative Treatment Lisfranc Injuries
Stage 2 and stage 3 accidents need to have the midfoot surgically stabilized since they’re generally unstable injuries. Interestingly, Hummell et al (2010) recently clarified a successful result in a point 3 football player with non-operative treatment. The objective of surgery is to acquire a fantastic reduction to optimize functional results. Virtually all expert opinions relating to Lisfranc injuries emphasize the importance of gaining as to avoid long- term morbidity from the midfoot.
Myerson et al (1986) identified some things that result in poor outcome for example residual angulation between the metatarsals, diastasis greater than 2mm between the first and second metatarsals. Correcting these defects is essential to avoid long-term complications like chronic functional disability , post-injury arthritis and instability with walking.
To obtain reduction of the TMT joints reduction is usually necessary to remove any tissue for example little bone fragments or ligaments. Reduction is supported with fluoroscopy. Nevertheless, in instances percutaneous fixation can be accomplished if the dislocation can be reduced by the surgeon under fluoroscopy and stabilize the joints together with wires and screws. However, most will require an open reduction to properly visualize and access of the joints that are tarsometarsal.
The choice of hardware for surgery is debatable surgeons the choices are:
1. Cannulated screws;
2. Solid, Non-cannulated screws;
3. K wires;
4. Bridge plates for tarsometatarsal joints.
At a thorough literature review, Stavlas et al (2010) found that injuries to the first few metatarsals (lateral and middle column) react well with screw fixation, whereas harms to the fourth and fifth metatarsals (lateral column) may respond well with K wire fixation.
Post-Operative Rehabilitation
This will often involve a non-weight- bearing cast or boot to get the first 3 weeks with a CAM/Aircast boot used for the subsequent three to five weeks so that the athlete is complete weight. Weight is slowly built around the eight to twelve months post-operative interval so that in a custom-made orthotic the athlete can weight bear by 3 months that.
The hardware is often removed at 12-16 weeks post-op in lighter athletes and in heavier athletes (>200 lbs) it’s been suggested to take out the hardware in 24 weeks (Nunley and Verullo 2002).
Post-surgery the results are generally favourable. Nunley and Vertullo (2002) discovered that in stable stage 1 harms, great outcome was found with conservative treatment with athletes back to game at 11-18 weeks post-injury. Athletes with stage 2 injuries had good outcomes with ORIF and returned to play 12-20 weeks. Period 3 accidents were not described.
Physiotherapy
The athlete will see that the physiotherapist athletic coach weekly to regain mobility. Interventions will be necessary in addition to direct mobilizations to restore the accessory movements.
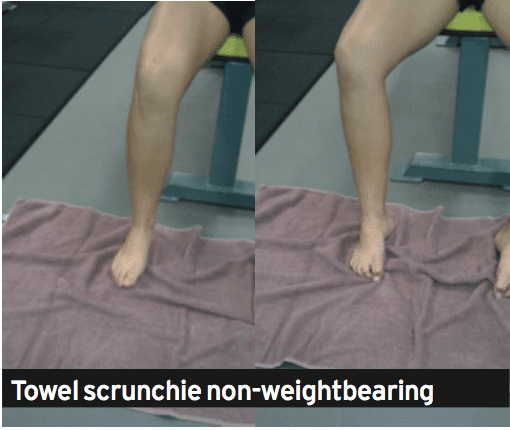
The therapist can also start intrinsic foot muscle exercises at approximately 8-10 weeks post-operative using the weight bearing exercises being postponed until week 12 post-operative. These exercises are designed to retrain the arch to be controlled by the foot muscles. Exercises that will satisfy this are towel scrunchies, cup drop, matt equilibrium and lunge exercises (see below).
The movement can be measured by the therapist regularly with knee.
1. Towel scrunchies. These have been used by therapists to strengthen the muscles that support the foot’s arch.
A. Place a towel onto a tiled or wooden floor (carpet will not work.
B. set the foot relaxed on the towel with all the foot in line with the knee and hip. The feet should be pointing directly ahead.
C. Initiate the movement by attempting to firstly raise the arch. Think about drawing the ball of the foot to the heel. You will see that the arch is going to lift.
D. Next use all the feet to loosen the towel under the foot.
E. Relax the foot and start again.
F. This exercise doesn’t cause any soreness the next day; the muscles should start to fatigue.
G. The development is seated, to standing on one leg and standing on two legs.


2. The cup drop. This can be an interesting and innovative way to integrate inherent arch muscle function and anti- pronator muscle function that is extrinsic using hip muscles that are hip, in particular the gluteus maximus and medius. During weight bearing, the hip is prevented by the gluteus medius muscle from rotating and adducting, and this action works well with the arch muscles preventing excess pronation.
A. Place a few small objects like marbles about one foot in front of your body.
B. Reach forward with the foot and also pick up the masonry with the feet. Of clawing at the masonry this activity will trigger the muscles.
C. Whilst holding the marble in the feet, circle the hip outwards into both sides of the body then behind the body and set the marble at a cup placed at 45 degrees to the cool.
D. It is necessary that the foot stays turned outwards as this retains the gluteus active.

3. The mat balance. This exercise incorporates these together with the arch muscles and adds contraction of the calf muscles both the gastrocnemius and soleus. The drill is done on a gentle matt, to create the exercise challenging. The mat surface generates an unstable situation, and there is mounting evidence that indicates that by incorporating a component of balance control to a rehab exercise may be necessary since the perturbations in movement excite all of the position feedback nerve endings which control proprioception. The nerve endings feedback to the muscle control system and also this potentiates the stimulation of their control muscles.
A.Place a soft mat in addition to a 6mm piece of timber or hard rubber mat. The thicker the mat that the harder the exercise.
B. Stand on the mat but just with the third, fourth and fifth feet connected with the matt. The first and second feet should be hanging unsupported from the mat.
C. This position of the foot makes a scenario whereby the foot wishes to turn in under gravity’s effect. The long pronation muscles in the shin and the muscles need to control the interior of the foot to keep it up and of the floor.
D. Attempting to keep equilibrium (and this will be hard when the matt is too soft), marginally boost the heel to participate the calf muscles.
E. Hold this position for 1-2 seconds and then slowly lower down to the beginning position.
F. Perform 3 sets of 10 repetitions.
4. Lunge with towel scrunchie. This workout is a high-level integration workout which combines gluteals and arch muscles whilst performing a exercise such as the lunge. This sort of exercise is done in late phase rehab prior to running as the muscle activation patterns more resemble what should happen in conducting concerning limb assistance — that is, the arch muscles control pronation, the quads control the knee and patella and the gluteus medius affirms the hip throughout foot strike.
A. Stand on a towel, very similar to Exercise 1 above.
B. Put some theratubing around a post and also wrapped round the upper tibia. The ring has to be guided to pull the tibia inwards, not outwards. This pulling in of the tibia can cause the top leg to follow along with this is imitating hip adduction and internal rotation. The goal of the exercise is to prevent it by maintaining the kneecap aligned with the next toes. The gluteals finally have to work to permit this to occur. Inwards and way would fall from the third toe, if they did not.
C. Gradually lower down into a lunge whilst keeping the monitoring of the kneecap over the next toe and also keeping the towel scrunched up under the foot.
D. Lift up to full knee extension. Rest. Start again.
Strength
The athlete will initially load throughout the foot with the foot impartial. Exercises such as split squat, high- foot leg press and posterior string movements such as deadlifts and stand pulls may start in the weight bearing phase. Exercises requiring more ankle dorsiflexion and so midfoot pronation will be delayed for a couple of weeks until strength and confidence improve (traditional one-leg squats, deadlifts and leg press).
Rehabilitation
The graded progressions for your athlete have been well summarized by Lorenz and Beauchamp (2013). The progression is a staged progression to gradually regain strength and confidence from landing and push-off positions. If the stage is pain free, the progressions could be made, the athlete could do selection and without compensations to the movement.
1. Bilateral heel raises
2. Heel raise,�single-leg eccentric lower
3. Single leg-heel raise from standing
4. Bilateral leaning heel raises
5.�Bilateral leaning heel raises, single leg�eccentric lower
6. Single-leg leaning heel raises
7. Single-leg triple extension heel raises
8. Mini-tramp low Impact exercises
A. Bilateral jumps in position
B. turns in place (two legs).
C. turns in place (two legs).
D. Jog in place
E. Three hops uninvolved, one hop involved
F. Two hops uninvolved, two hops involved
G. One hop uninvolved three hops involved
9. Agility ladder
A. Different frontal transverse plane designs
B. Hopscotch to involved negative (two to one)
10. Single-leg A/P jumps in place
11. Single leg M/L jumps in place
12. Single leg transverse jumps in position
13. Single leg hops in agility ladder
Return To Running
The choice as to when to remove the hardware will influences the choice. As a general rule, when the screws and wires are eliminated, the athlete will be permitted to attend and walk gym sessions to the elimination but running will probably be delayed.
The athlete is encouraged to walk a treadmill using a incline to promote the push. This can start at 12 weeks . The athlete may quickly advance into backward and forward running on grass and it’s expected they are doing so by week 14 depending on when the hardware was taken away. As they progress through running they could slowly begin to construct speed they reach sprint speed.
Gentle off-line running drills such as weaving, easy bypassing, stepping and caricoca drills would normally be started in around 16 weeks post-op and progressed into tougher single-leg and hard-cutting plyometrics as pain allowed. It would be expected that by 20 weeks post-op, the foot has sufficient strength, range of movement and confidence to start team- based ability function. Prior to this, the athlete can experience some frequent field hop tests like tests and single-leg triple jump to assess differences in abilities.
Functional Tests
A evaluation that is practical sports-specific is a test or field test that aims to mimic the movements. The use of practical tests aims to recognize imbalances and will boost confidence in both patient and the clinician the injured patient can return to play. It is effectively a way of reducing the hazard. The evaluation ought to be an objective, measurable and quantifiable test that includes a component of:
- Strength
- Agility
- Power
- Balance Neuromuscular status.
The aspects can be incorporated into practical tests such as agility and jumps/ movement evaluations.
The hop tests comprise:
1. Single jump
2. Triple hops
3. Crossover jump
4. 6m timed jump.
Single limb evaluations are necessary as study proves that dual limb and modified double limb tests don’t demonstrate any differences between groups since the uninvolved limb can mask deficits of the thoracic (Myer et al 2011). Single-leg hopping evaluations are sensitive enough to discover asymmetry, and specifically the crossover hop test at six months post-op is the most sensitive of these tests at predicting future function of the knee along with the 6m timed test is the most vulnerable and sensitive of under normal function at six months . (Logerstedt et al 2012).
Therefore isolated single-limb performance tests may provide a critical element to field-based operational performance testing to identify deficits in reduced limb performance, including deficits in force attenuation functional power and postural stability. The capability to maintain isolated single limb electricity is significant in sports that require significant control in stepping edge and cutting manoeuvres. This may require and ability to regenerate and divert and then to absorb force on one limb the motion.
Conclusion
Injuries are uncommon in athletes on account of the severe consequences they could have on athletic role, the sports medicine specialist has to be well versed in evaluation and initial management. They can be challenging injuries manage and to diagnose for the clinician.
Stable Lisfranc injuries with no instability can be handled conservatively stage 2 and 3 accidents involving diastasis of their second and first metatarsals requires consideration. This can be done usually using the open reduction and fixation with screws, K cables and/or plates
Rehabilitation after surgery will take no less than 12-16 weeks it’s typical for the return to sport to take in contact sport athletes. Successful return to competition time frames extend to the 20-24 week stage post-surgery and rehab will involve reduction of the entire limb kinetic chain but also not only the foot muscles.
References
1. Castro et al (2010) Lisfranc joint ligamentous complex: MRI with anatomic correlation in cadavers. AJR. 195; W447-455.
2. Chiodo CP and Myerson MS (2001) Developments and advances in the diagnosis and treatment of injuries to the
tarsometatarsal joint. Orthop Clin North America. 32(11); 11-20.
3. Garrick JG and Requa RK (1988) The epidemiology of foot and ankle injuries in sports. Clinical Sports Medicine. 7: 29-36.
4. Hummell et al (2010) Management of a stage 3 Lisfranc ligament injury in a collegiate football player. Athletic Training and Sports Health Care. 10(10); 1-5.
5. Logerstedt et al (2012) Single-legged hop tests as predictors of self reported knee function after ACL reconstruction. The Delaware-Oslo ACL cohort study. American Journal of Sports Med. 40(10); 2348-2356.
6. Lorenz and Beauchamp (2013) Case report. The functional progression and return to sport criteria for a high school football player following surgery for a Lisfranc injury. The International Journal of Sports Physical Therapy. 8(2); 162-171.
7. Myer GD, Schmitt LC, Brent JL, Ford KR, Barber KD, Scherer BJ, Heidt RS, Divine JG and Hewett TE (2011) Utilization of modified NFL combine testing to identify functional deficits in athletes following ACL reconstruction.
Journal of Sports Physical Therapy. 41(6); 377- 387.
8. Myers et al (1994) Midfoot sprains in collegiate football. American Journal of Sports Medicine. 21; 392-401.
9. Myerson et al (1986) Fracture dislocations of the tarsometatarsal joints: end results correlated with pathology and treatment. Foot and Ankle. 6(5); 225-242.
10. Nunley JA and Vertullo CJ (2002) Classification, investigation and management of midfoot sprains: Lisfranc injuries in the athlete. American Journal of Sports Medicine. 30(6); 871-878.
11. Ouzounian TJ and Sheriff MJ (1989) In vitro determination of midfoot motion. Foot and Ankle. 10; 140-146.
12. Rankine et al (2012) The diagnostic accuracy of radiographs in Lisfranc injury and the potential value of a craniocaudal projection. AJR. 198; W365-369.
13. Shapiro et al (1994) Rupture of the LisFranc�s ligament in athletes. American Journal of Sports Medicine. 22(5); 687-691.
14. Stavlas et al (2010) The role of reduction and internal fixation of Lisfranc fracturedislocation: a systematic review. International Orthopaedics. 34; 1083-1091.
General Disclaimer, Licenses and Board Certifications *
Professional Scope of Practice *
The information herein on "Managing Lisfranc Injuries: Scientific Outcomes" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and on our family practice-based chiromed.com site, focusing on naturally restoring health for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez, DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card








