by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Functional Medicine, Gut and Intestinal Health, Health, Wellness
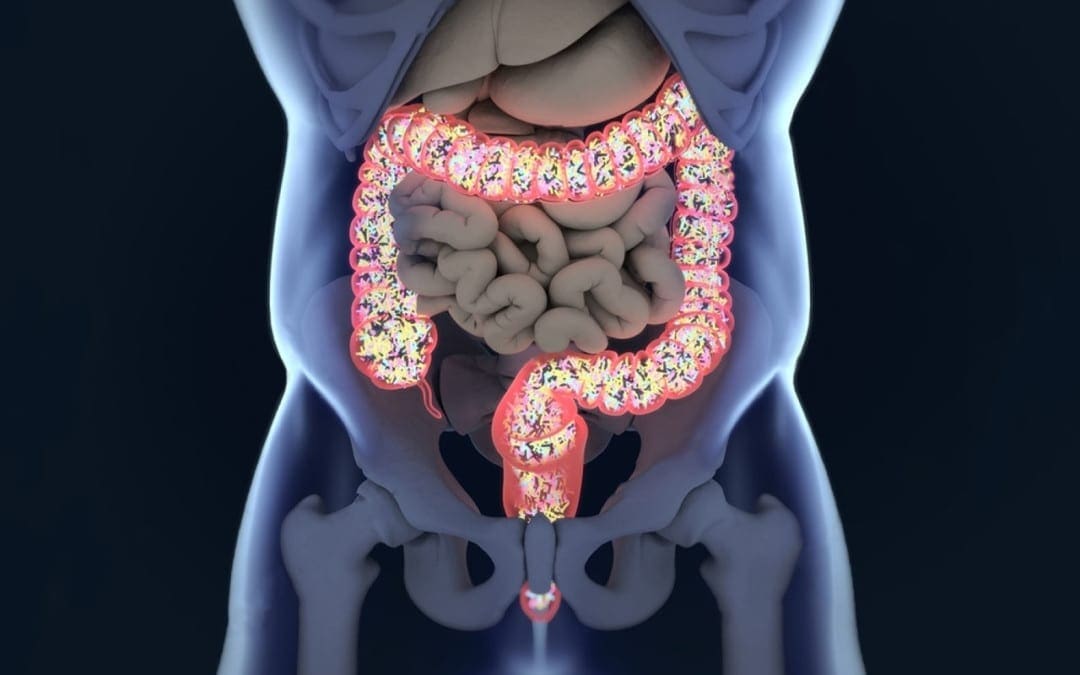
With the last article, we talk about how our gut system actually works. With the many microbes that inhabit our intestines, we do try to our best to lead a healthier lifestyle. Here at Injury Medical, local chiropractors and health coaches inform our patients about functional medicine as well as helping them to prevent a leaky gut. Here we will talk more about what the microbiomes in our intestines do when we are exposed to harsh environments.
The Microbiome
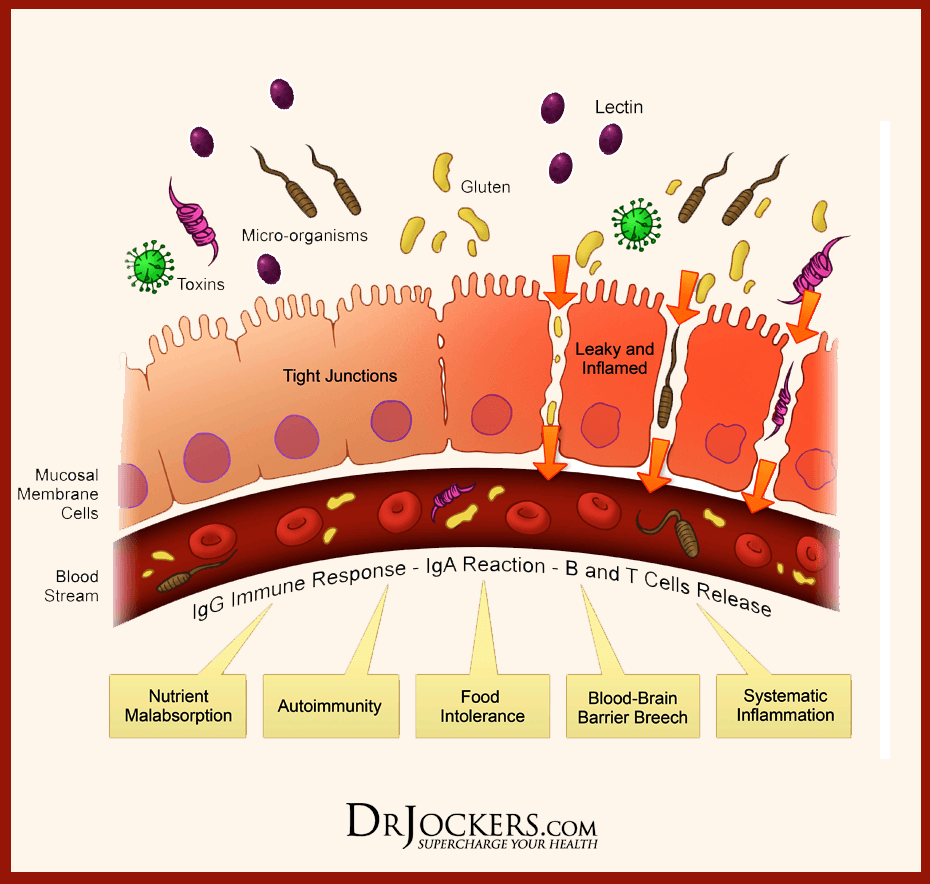
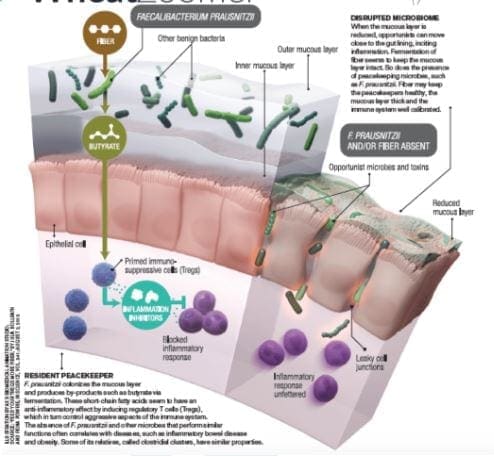
The significant role of the microbiome in the epithelial barrier integrity and breakdown. However, we can�t have a conversation with patients about intestinal permeability and food sensitivities without telling them about the role the microbiome plays.
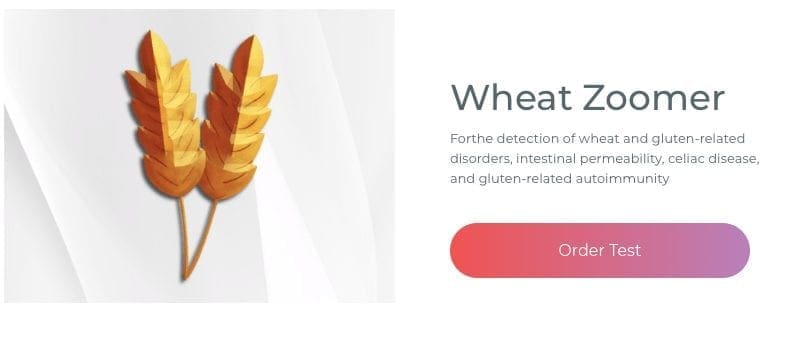
The Wheat zoomer is rich with data but adds the Gut zoomer with the patients; the results are more accurate.
Microbial Influence on our Intestines
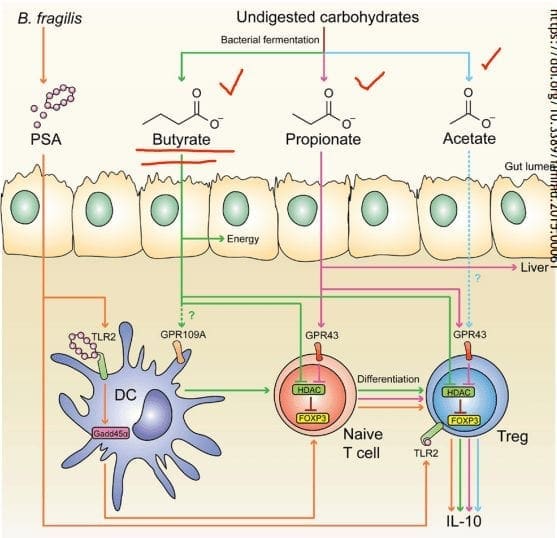
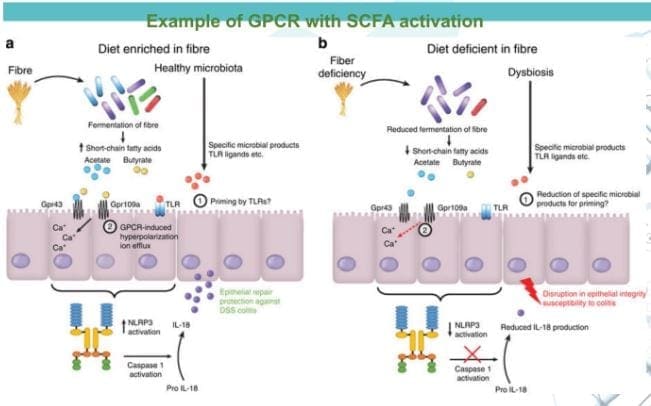
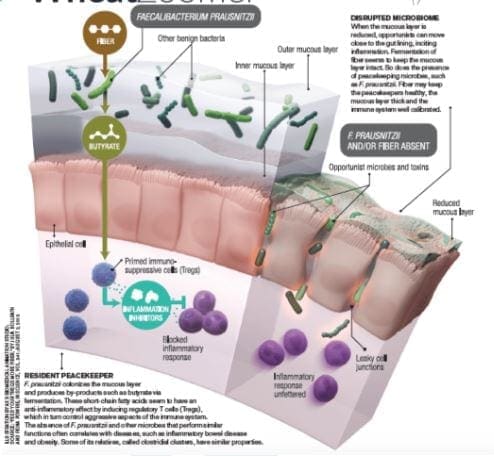
- Immune influence: One of the leading roles that microbiomes play in the immune system is that it generates byproducts of carbohydrates/fiber fermentation that will influence T-cell differentiation. Without the distinction, we will see an increase of being at high risk of autoimmune diseases, allergies, autism, and asthma.
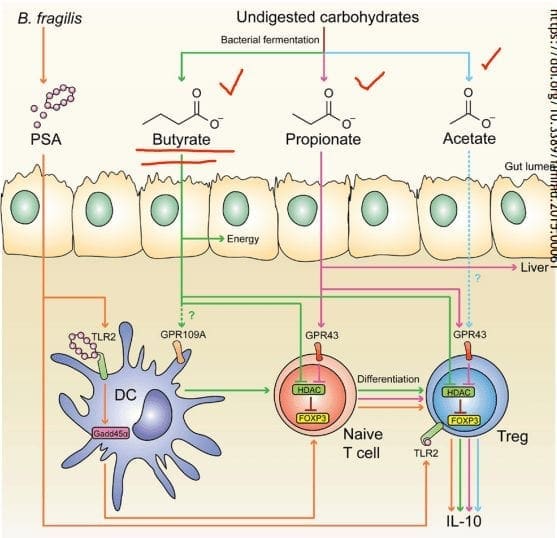
- SCFAs (Short Chain Fatty Acids): The food we consume gets fermented for good bacteria to feed on. SCFAs creates fermented fibers by commensal microbes into Butyrate, Propionate, Acetate. These three are essential to the intestinal immune system. These SCFAs can influence T-cells differentiation differently, but it still gets the same results.
- T-cell Differentiation: na�ve T-cells that activate the immune response to T-regs (police cells) to signal B-cells, and it can be a good thing. But if the T-cells activate and differentiate the wrong cells, it will cause inflammation.
When T-cells differentiation is less abundant, there will be a higher incidence of food sensitivities, autoimmune disease, asthma, and allergies. But when there is an abundance of butyrate, the patients have lower rates of colon cancer and colitis.
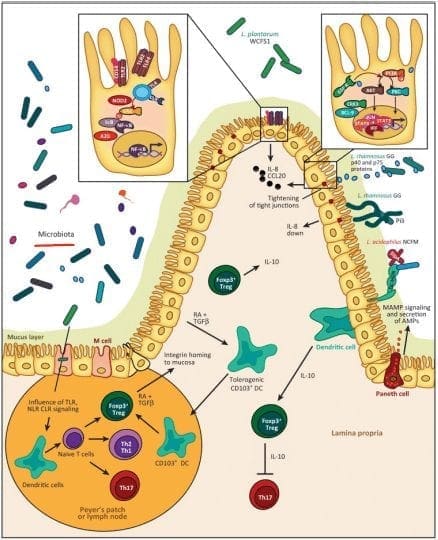
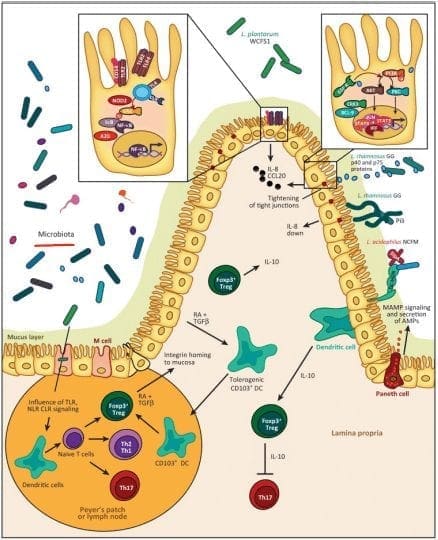
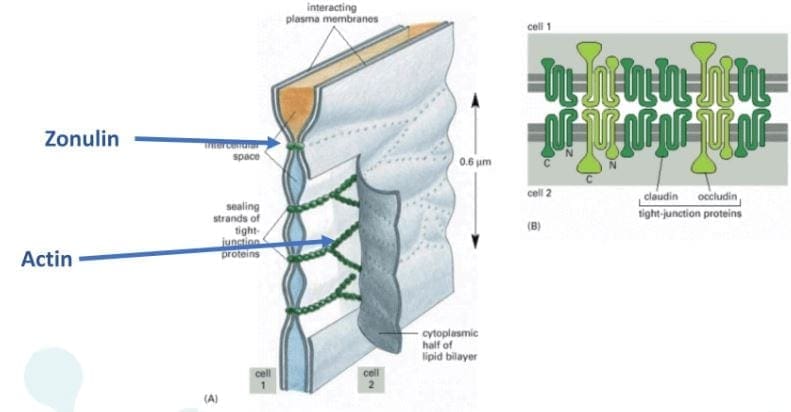
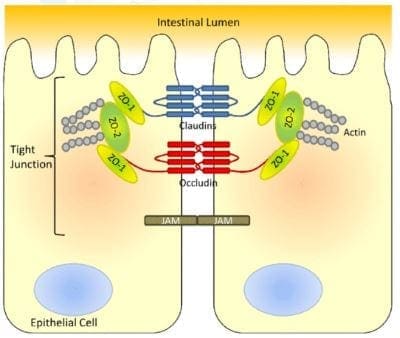
- Tight Junction: Lactobacillus plantarum and Lactobacillus rhamnosus are the reinforcers for the tight junction while inducing TLR (toll-like receptors) outside the intestinal epithelial walls, as well as increasing the abundance of zonulin-occludin into the tight junction.
SCFAs also play a vital role in the tight junction by lessening the extent propionate, inducing LOX (lipoxygenase) activity and increasing tight junction�s stability while reducing permeability.
Pathogens/Pathobionts: Can be an influence in the epithelial barriers as they can be opportunistic or conditionally pathogenic. Various pathogens like enteropathogenic E.coli can alternate the tight junction�s system. However, if there is a low abundance of L. plantarum, then it will lead to infections and disruption as well as disorganization of the actin cytoskeletons. This can be reversed by incubating the epithelial cells with L. plantarum to create a high density of actin filaments to the tight junction and repair itself.
- Zonulin, actin, and LPS: In the previous article, zonulin is the �gatekeeper� proteins that are responsible for opening and closing the tight junction. We talked about how if there is a low count of zonulin, it can cause inflammation, but if the zonulins are high, they can increase the IP and may facilitate enteric translocation by disassembling the tight junction. With less zonulin, it can be an overgrowth of b bacteria cells, thus causing more inflammation.
Actins are the structural and functional cells in the tight junction. However, if bacteria enter the actin cell walls, the bacteria will release toxins to the cell walls, it not only damages it but causes it to leak as well. This will make the damage actin cells not only paracellular but also intracellular to the damage actin cell walls.
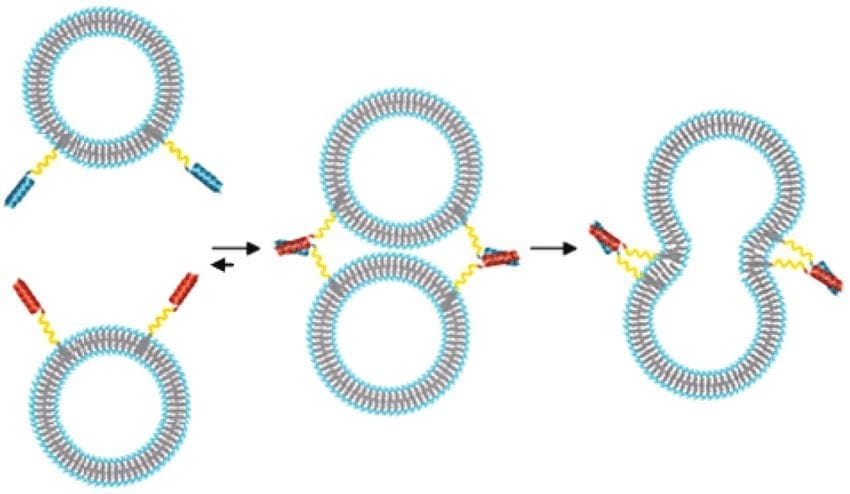
Actin walls can also be affected when surfactants are involved. Surfactants are food agents and are known to affect the absorption of food substances in the gastrointestinal tract. They are not problematic, but when there is a low count on TEER, it can increase permeability and disband the tight junction.
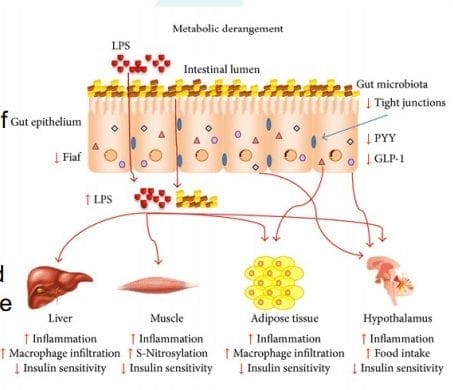
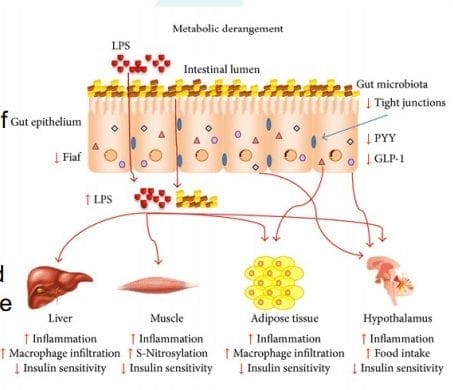
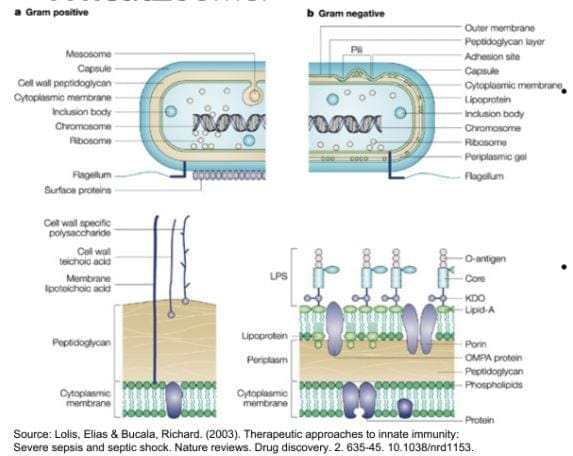
LPS (Lipopolysaccharide) acts as a barrier and is recognized by the immune system as a marker for detecting bacterial pathogen invasion. It�s responsible for the development of inflammatory response in our gut.
Diet and Lifestyle
Diet and lifestyle contributions to the epithelial barrier integrity and breakdown. With the Wheat and Gut Zoomer helping out our intestinal barriers. Specific diets and lifestyles can also play effect to what is causing discomfort to our gut. These factors can cause our gut to be an imbalance, gastro discomfort, inflammation on our intestinal epithelial barriers.
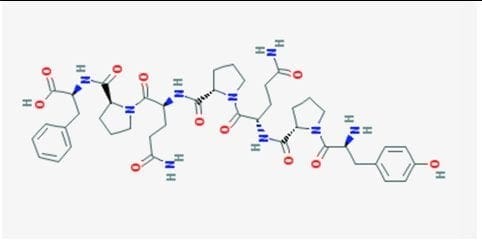
- Gluten: Gliadin is the main peptide that can cause gluten sensitivity. The gliadin protein can bind with many microbes, causing discomfort to our intestines and gut. Plus giving us an autoimmune disease, skin allergens, and chronic illnesses.

- Keto/High Fat Intake: Increase fat meals cause an increase of permeability, and if a patient has a high gram-negative, it will cause problems. But it can be beneficial, to those who don�t have the gram-negative bacteria in their system but, certain microbes like SCFAs do cling onto these fatty substances. In order to give patients an accurate result use both the Gut Zoomer and Wheat Zoomer to better the chances. Higher fat meals suppress beneficial bacteria. Causing a double risk of toxins in the bloodstream as well as inflammation.

- Alcohol: Patients are more willing to give up alcohol than gluten. Alcohol can be a stress reliever but can lead to addiction. It can be one of the causes of redistribution of the junctional proteins. One glass of wine a day is ok, but some patients don�t see alcohol as a mediator for reducing problems.
- Lectins: Lectins are contributors to permeability and impair the integrity of the intestinal epithelial layer, allowing passage through. Antibiotics for WGA can help lower the permeability of the intestinal wall barriers.

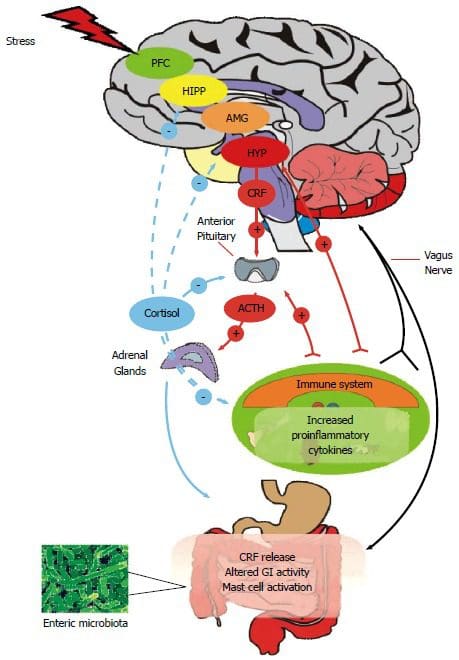
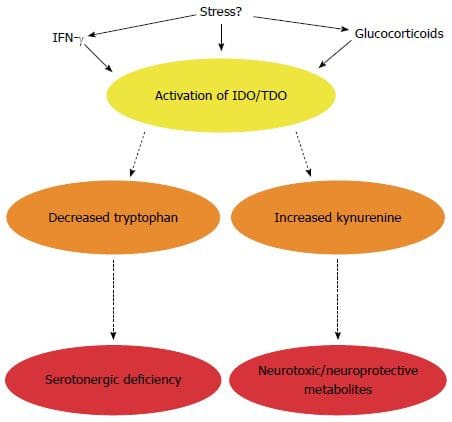
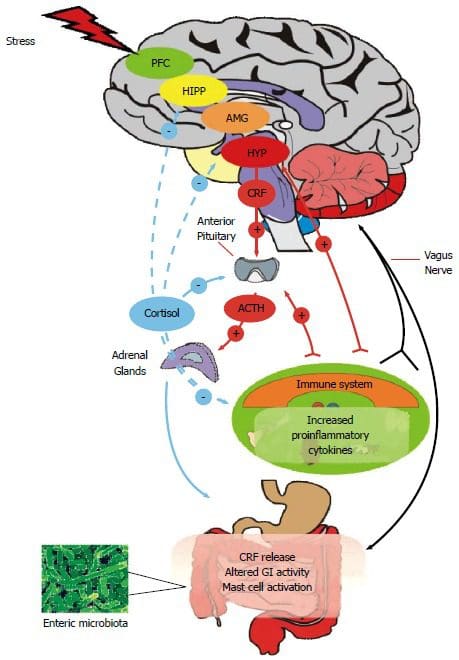
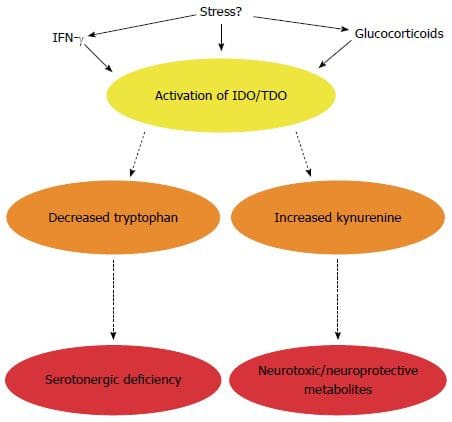
- Stress: Stress can cause discomfort and permeability in the intestinal epithelial barrier from high levels of cortisol.
Conclusion
Yes, gluten can cause inflammation in the intestinal epithelial barriers, but many factors that we discussed are also factors that can cause physiological assaults on the barrier�s integrity and stability of the intestinal ecosystem. Dr. Alexander Jimenez informs our patients about the importance of how functional medicine works with the combination of the Gut Zoomer and the Wheat Zoomer. This is not only protecting our gut but by giving us the information on what we can do to prevent a leaky gut.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Gut and Intestinal Health, Health, Wellness
Today local chiropractors will be giving a description of the wheat zoomer. We will be giving a brief description of each panel, its markers, and the basic interpretations of the test. We will also be discussing the considerations for the patients and providers before we take The Wheat Zoomer test.
What is a Wheat Zoomer test?
The Vibrant wheat zoomer has 6 test in one to identify if the patient has wheat and gluten sensitivity. The Vibrant wheat zoomer does give our patients a thorough evaluation and we ask our patients if they started to be gluten-free or was gluten-free, either from birth or not and how much gluten-contained food did they eat. One of the best ways to ensure that our patients may have a gluten sensitivity is that if they have a food diary for us to look over and that way we can determine how severe of the wheat zoomer.
IgA vs IgG
In order for us to know about the wheat zoomer in our patient�s body, we must know about the immunoglobulins. The first one is IgA. IgA immunoglobulins are mucosal and are found primarily in the epithelial lining of the body: intestinal tract, lungs esophagus, blood-brain barrier and around internal organs. They are:
- The first line of defense.
- More accurate to our gut.
IgG immunoglobulins found in the blood system and are numerous in the body They are considered �systemic� and are non-specific to any one location. Not all IgG antibodies are sensitive though, some of them can indicate that an antigen has �leaked� into the blood and the immune system tagged that antigen as a �non-self�. And they are not diagnostic as IgG+IgA, but if IgA is absent, the antibodies are more relevant.
- If the patient is recently gluten-free, the antibodies will tell us that the antigen hasn�t cleared out in the patient�s system from past weeks of eating gluten.
Celiac
Celiac is a growing autoimmune disease, about 1% of the population is affective and 1 in 7 Americans have a reaction to wheat or wheat gluten disorder. The Vibrant test can determine a 99% sensitivity and 100% specify on the celiac antibodies.
- Total IgA and Total IgG measure both the IgA and IgG to determine the patient�s reactivity to gluten
- Cut off for IgA is 160 as well as a bottom 1/3rd
- Not all traditional markers for celiac disease doesn�t need to be elevated if tTg2 is elevated.
Intestinal Permeability
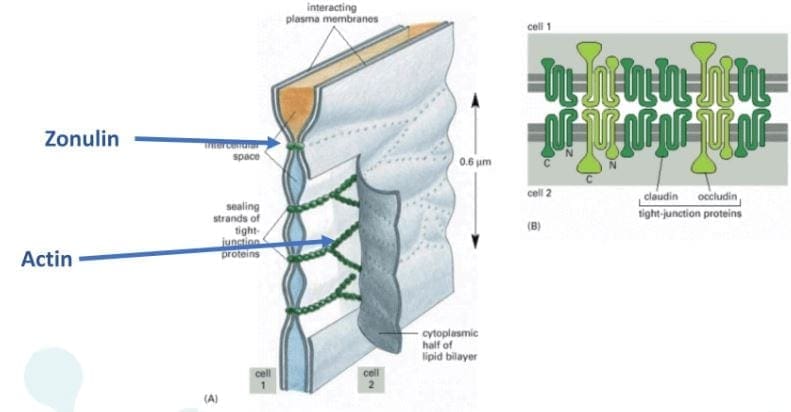
Zonulin is the gatekeeper for the intestines and controls nutrient flows and molecules across the membrane. It is a protein complex inside the intestinal tight junctions and can be increased by either gluten and high-fat meals.

Anti-Actin, especially f-Actin is in the smooth muscle of the intestines. Actin is part of the actomyosin complex. Vibrant can isolate f-Actin to get a more accurate picture of the patient�s immune response to the intestines. While antibodies in actin can identify intestinal destruction and indicate autoimmune diseases like connective tissue disease and autoimmune hepatitis.
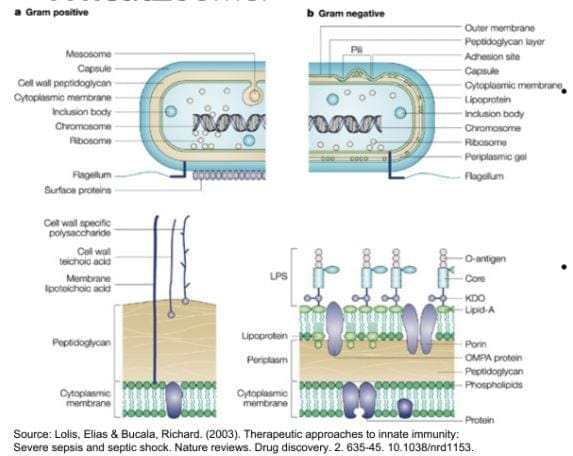
Lipopolysaccharide (LPS) is produced by gram-negative enterobacteria. It is very potent and can cause inflammation. Plus it�s one of the indications of a leaky gut. Practitioners can draw additional lab test for cardiovascular, inflammatory markers, and diabetes/insulin resistance.
Here at Injury Medical Clinic, we suggest to our patients to try a Vibrant GutZoomer to identify the source of their ailments before we add the Vibrant WheatZoomer.
Gluten-mediated Autoimmunity
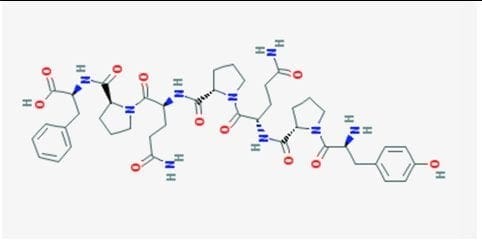
Fusion Peptide is the new addition to Wheat Zoomer in 2017. It is cross-linked to tTg and can identified celiac progression from 14 months to 4 years.
Differential Transglutaminases can detect autoimmune reactions to gluten that are not celiac or are becoming celiac. However, gluten is still a trigger but react differently in the celiac autoimmune disease such as:
- Transglutaminase 3= skin manifestations of autoimmunity like dermatitis herpetiformis, eczema, and psoriasis.
- Transglutaminases 6= neurological manifestations of autoimmunity in the cerebellum like gluten ataxia, gate abnormalities, balance and coordination issues.
Wheat Germ Agglutinin
Wheat Germ Agglutinin is the lectin component of wheat but, it is not a component to gluten. Dr. Jimenez can detect a patient’s low level of Vitamin D absorption from the patient�s results. And Wheat Germ Agglutinin is commonly used as an additive in supplements and the supplement can still be called gluten-free due to the different protein structure.
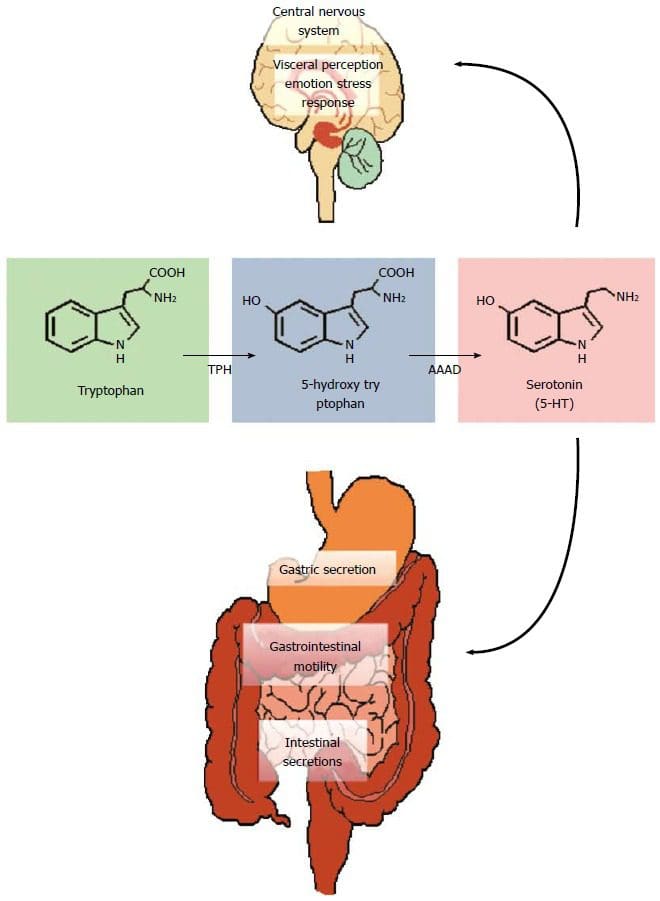
Gliadin, Glutenin, and Prodynorphin
Gliadin and glutenin are what makes up the super protein in gluten. Most people are reacting to the Gliadin portion of gluten and gliadin binds with tTg2 in celiac and binds zonulin to a leaky gut in patients. Gliadin reacts to any antigens can indicate a sensitivity to gluten in patients and gluteomorphin are peptides in wheat and react as a euphoria receptor to the brain. Prodynorphins antibodies can indicate that gluten reacts to signaling hormones and affect the patient’s mood.
Sadly though, patients do have a hard time withdrawing gluten in their diet since their antibodies are used to the compound and it up to us, here at Injury Medical Clinic to gently push our patients to have the will power to fix what is causing them to have ailments.
Wheat Allergin
Wheat Allergen is the true allergen body. Some patients that already know that they are allergic to wheat from a young age but it doesn�t decrease when wheat is eliminated and can remain long term after the allergic response happens.
Glutenin
Glutenin is the other part of the gluten compound. However it is less common to some people, but some individuals do show reactivity to glutenin, thus still have a gluten sensitivity. But there is no clinical difference to the reactivity to glutenin from high to low molecular weight.
Non-Gluten Wheat Proteins
Surprisingly Vibrant has an advantage to their test as they have a panel for patients that don�t have a gluten sensitivity but a wheat sensitivity. The Vibrant advantage to the unique non-gluten wheat panel shows us that:
- Proteins in wheat unrelated to gluten but relevant to immune reactions.
- It is 30% of the protein molecular weight of wheat.
- Some individuals are more reactive to wheat proteins than gluten itself.
If they are trying to be gluten-free, patients still have to read the labels to see if any hidden wheat starches are in the ingredients. But not all food products are gluten-free if they have the wheat protein in them.
Conclusion
If the patient is trying to be gluten-free but previously ate gluten compound food. They can still feel the reaction if they discovered that they have a sensitivity to gluten by their practitioner. And must take precautions when they are reading the labels of the products they are going to buy and consume. In the next four articles, we will discuss what the Wheat Zoomer can provide as well as, discussing about what causes leaky gut, what actually goes on in our patient�s intestines, and wrapping up on what to do after the Wheat Zoomer heals and restores the gut barrier.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Gut and Intestinal Health
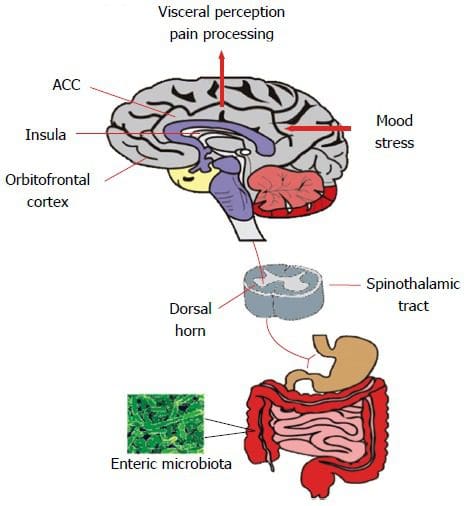
The microbiome is a crucial part of the body and how effectively it functions.� The microbiome plays a significant role in the immune system, the digestion of food, how the body metabolizes drugs, detoxification, vitamin production, as well as protection from foreign innovators. However, just like many other parts of the human body, it is greatly influenced by stress, environmental factors, and sleep which can ultimately impact intestinal permeability.
Ideally, the best functioning microbiome is diversified. The more diversity a microbiome has, the more stable and resilient to antibiotics it becomes. In addition to this, a diversified microbiome also has stronger pathogen resistance.


The microbiome is filled with many different bacteria strains that all play essential roles in keeping the gut healthy and controlling intestinal permeability.
- Bacillus is a spore-forming bacteria whose major role is the production of B and K2 vitamins in the gut.
- Clostridia compromise about 10-50% of the microbiome and are anaerobes that are not found in probiotics. These thrive on high fiber and polyphenols.
- Akkermansia makes up 1-3% of the microbiome and helps to reduce inflammation and protect against inflammatory bowel disease.
- Lipopolysaccharides are bound on gram negatives residing in the gut and protecting the bacteria from bile salts. (Lipopolysaccharides are normal in the gut, but they are not normal in the bloodstream)
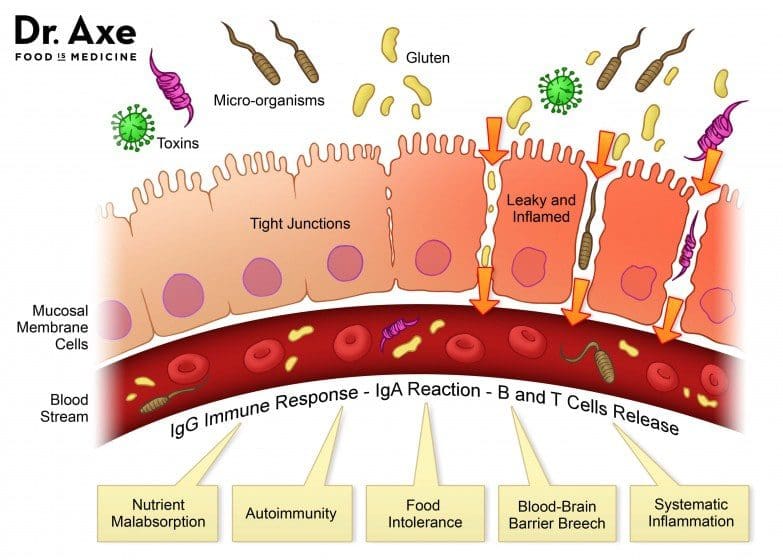
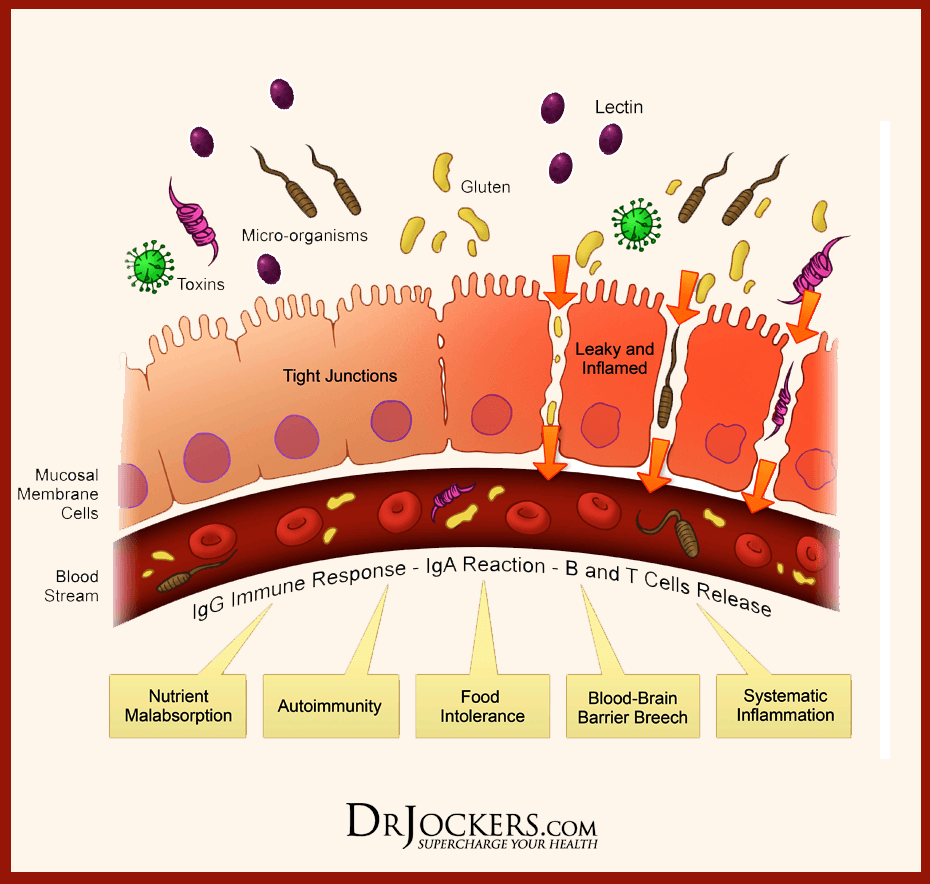
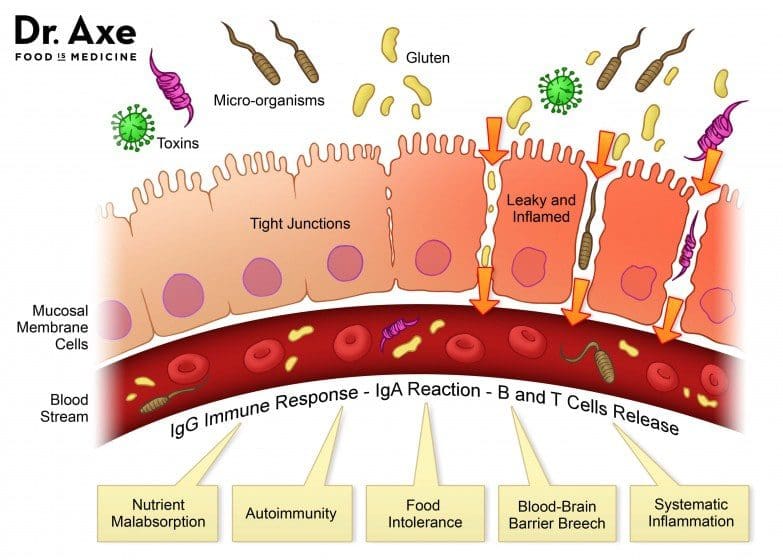
The main reason it is important to have a diversified and healthy gut is to avoid problems with intestinal permeability or “leaky gut syndrome”.� A leaky gut refers to how easily substances that are not fully digested pass through the intestinal wall. This occurs when the tight junctions of the walls become loose, allowing the gut to be more permeable.� This is how bacteria and toxins pass from the gut into the bloodstream, causing inflammation and other autoimmune diseases.
Keys to a healthy gut:
- Eat more organic fruits, vegetables, and fermented food
- Try to limit the amount of food that is boiled as boiled foods contain fewer polyphenols
- �Supplements such as Vitamin D, Vitamin C and Omega 3’s
- Detox: sauna, yoga, meditation, and regular exercise
- Prebiotics and Probiotics

It is important to remember that the best thing for a healthy gut is diet. Suppliments and pills can help, but in the long run, a diet is the most important and influenctial factor to the gut. A gut healthy diet will aslo help to maximize liver detoxifaction. If you do not know where to begin, I recommend getting a gut zoomer blood test and consulting with a doctor about what probiotics and diet are best for you. – Kenna Vaughn, Health Coach�
by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Gastro Intestinal Health, Gut and Intestinal Health
Now and days, mostly everyone has a gluten sensitivity or a gluten allergen in their bodies. This could happen to anyone whenever they are eating gluten-contained food or products and suddenly feel unwell or their gut acts differently throughout the day. Or they actually get tested by their physicians and realizes that they have celiac disease. In the last article and the previous one after that, we talked about the 8 products that have hidden gluten in them; as well as the introduction of the wheat zoomer we use for our patients.
Here at Injury Medical Clinic, Dr. Alexander Jimenez consults with our patients about certain zoomers that can actually aid the patient�s body. In this article, we review the factors that affect test results such as medication and fasting after taking the Wheat Zoomer, as well as, focusing heavily on the mechanism of the intestinal permeability, the structure and function of the epithelium. We also focus about important immunomodulatory metabolites, epithelial cell types and the roles in the epithelial barrier.
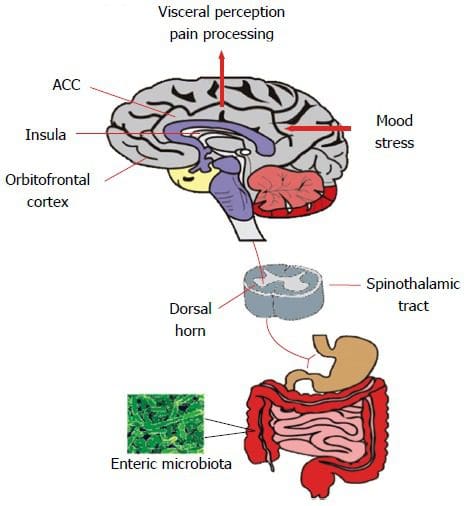
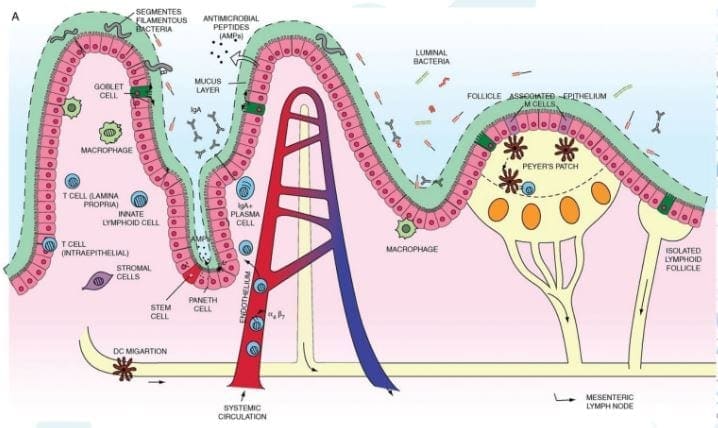
Intestinal Permeability
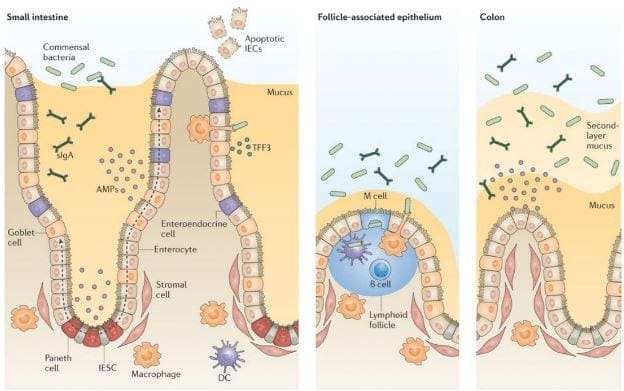
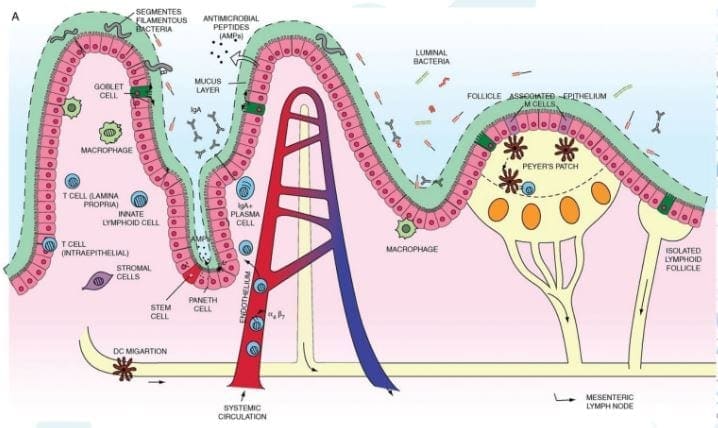
Let�s start with the mechanisms of intestinal permeability. The main purpose of the intestinal epithelium is to keep the good things in and the bad things out. While the system is complex and ever changing, it still sends out a message to the host and maintain balance both physical and biochemical as a protective barrier.� There is an abundance of antigen sampling to regulates the flow of nutrients in the host�s body, as well as, keeping an eye on the body by the mucosal immune system. Not only that, if you have an injury or an acute inflammation, the intestinal epithelium will support tissue repair by coordinating with microbiota.
Another thing that the epithelium does is that it responds to the microbial signals that will make our bodies tolerate any continuous exposure to commensal bacteria. But we do want to keep the good bacteria in our bodies but get rid of the bad bacteria, so our bodies feel good. The intestinal epithelium also convey microbial signals to the mucosal immune cells, while promoting a coordinating immune response to battle against commensal bacteria and the enteric pathogens, since these two microsomes should not be in places they are not allowed in.
While the epithelium is battling with the bad bacteria in our system, it also regulates the B and T cell response to either, control inflammation, squash inflammation, or cause inflammation on the intestinal barrier, depending on the situation. Plus the epithelium locally regulates the immune response at the intestinal barrier by influencing innate and adaptive immune responses to the body�s intestines.
However, if there is something disrupting the intestines, like chronic inflammation or leaky gut; the epithelium barrier can be compromised. In order for us to fix a leaky gut, we must learn what is causing the inflammation in the first place. The epithelium is home to many microbes, immune cells and can determined if we need the immune response on any harsh exposure. If we can learn more about these mechanisms, then we can calm down the inflammation by resetting it back to its calm, natural state.
But the immune cells in our intestinal epithelium can also cause disruption on our gut by leaking out of the protective barriers and attacking the pathogens anywhere in our system. So epithelial permeability can not only cause inflammation but prevent it in our intestines, which is both good and bad depending on the situation.
Dr. Alexander Jimenez consults with our patients with natural alternatives of healing inflammation in their gastral intestines.� If he can find the sources of what causes the inflammations in your gut, then he can work with aiding them with functional medicines while informing you what they can do to heal your gut.
Now let�s looks at the intestines and the many microsomes that they contain. Here are some microsomes we will be discussing as well as what is their key roles in the intestines; so we can figure out how to prevent a leaky gut.
�
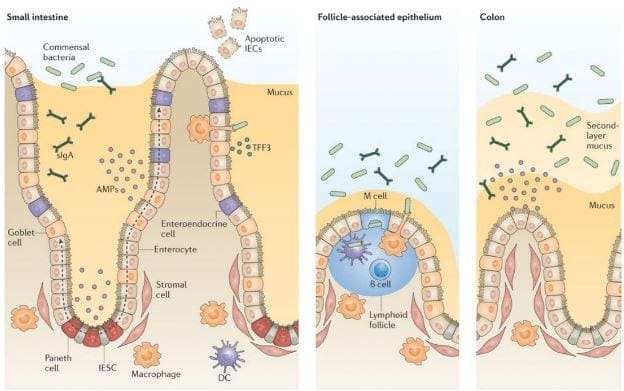
The Mucosa
This is in both the small intestines and the large intestines and are completely different. The small intestines has one mucus layer and has limited microbes inside it�s mucosa, while the large intestines has an attached inner mucosa and a loose outer mucosa. The mucosa plays an important role in the intestines because it can tell �Friend� from �Foe� in the immune system.
Important Tight Junction Proteins
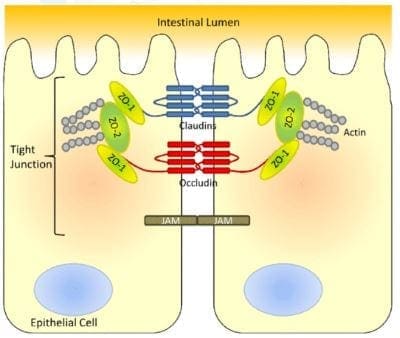
The tight junction is an important function in the intestinal epithelium as it is one of the barriers that separates what comes in and what comes out in our gut.

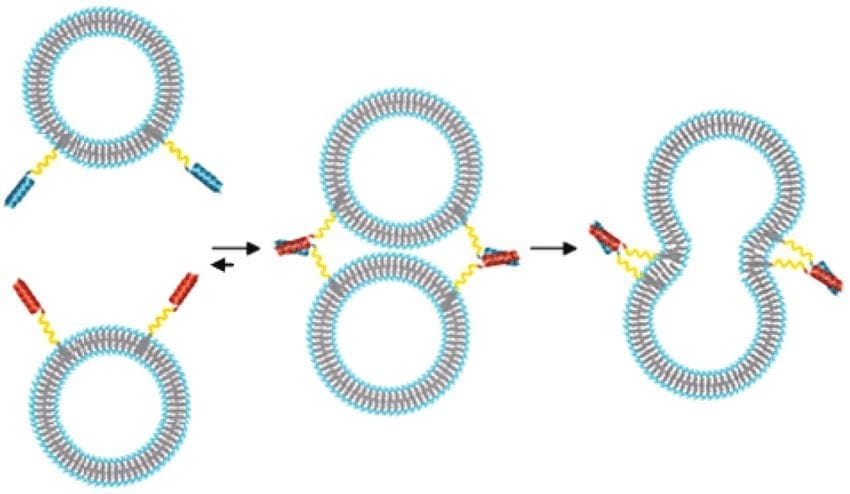
Actin: Are the structure and functions of tight junctions. But they constantly disassemble and reassemble actin filaments if they are anti-Actins. It is controlling the tight junctions cells as it acts like a contractable belt by pulling or contracting the junctions in the intestinal cells.
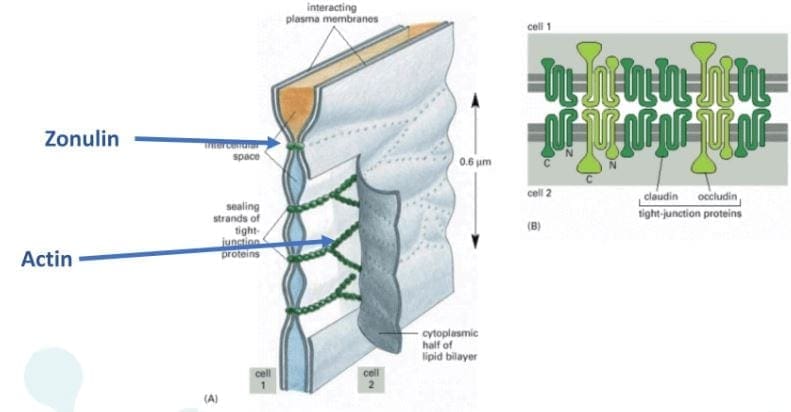
Zonulin: They are the �gatekeeper� proteins that are responsible for opening or closing the tight junctions. Zonulin acts the mortar of the intestines and is associated when gluten sensitivity is present, if there are low counts of zonulin thus causing inflammation.
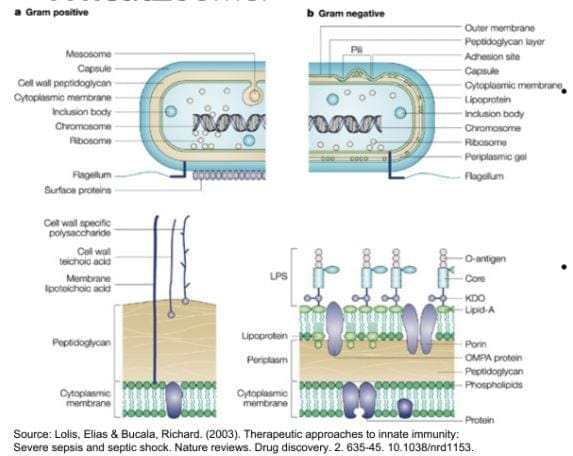
LPS(Lipopolysaccharide): These sent out a signal to the tight junction permeability as they find signs of bacterial endotoxin by translocating across the epithelial barrier and entering circulation. LPS is made up of gram negative bacteria in the GI tract. LPS outside the epithelial cell wall and reacts to fatty acids, which can lead to obesity for individuals.
Cell Receptors Involved in the Barrier Integrity
These cells are protectors of the epithelial barrier walls as they strengthen the immune intolerance and digestive tract, as well as causing or preventing inflammation when necessary.
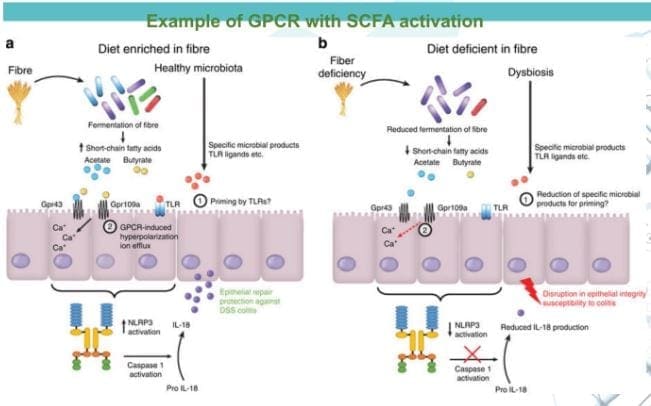
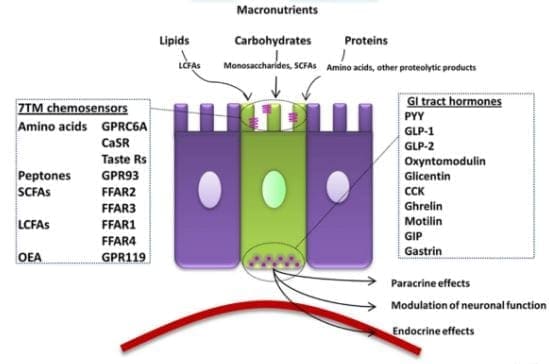
G Protein Coupled Receptors (GPCRs): GPCRs are the main players of the immune system in the epithelial system. A wide variety of substances can bind with GPCRs depending what the substances are. Short chain fatty acids, omega-3�s and any food that we eat is fermented by our gut and stimulate repair on the epithelial barrier. However if there is a consumption of low or zero-fiber in our diet, the food will not be fermented and causes inflammation.
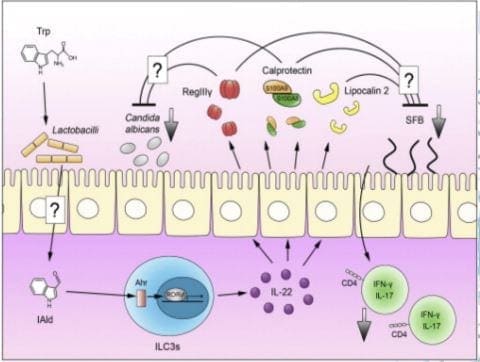
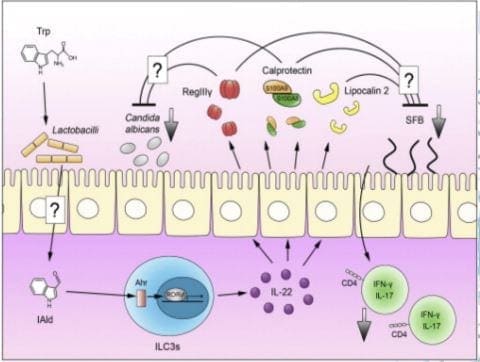
Aryl Hydrocarbon Receptors (AhRs): AhRs interact with a range of aromatic hydrocarbons like food and microbes both in and out of the gut. These receptors respond strongly to compounds found in cruciferous vegetables, thus preventing a heighten immune reaction and reducing epithelial damage as well as promoting functioning intraepithelial lymphocytes (IELs).
But if we are not eating enough cruciferous vegetables, the IELs are being produced less, the epithelial barrier is compromised and will cause inflammation.
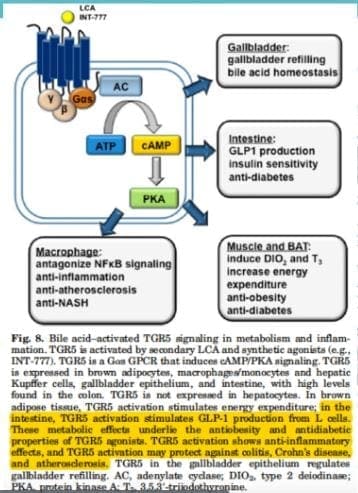
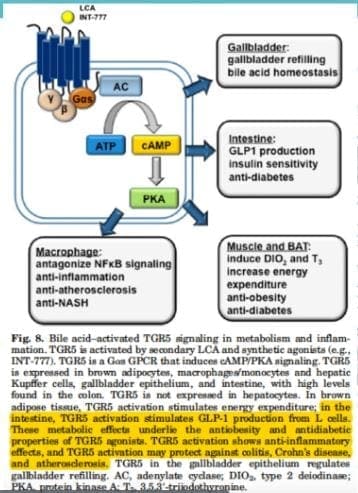
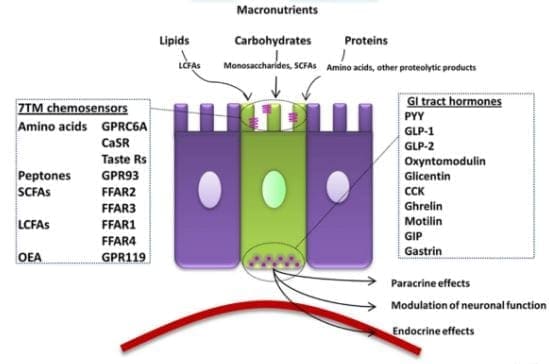
Bile Acid Receptors (BARs): BARs recognize primary and secondary bile acid. The primary bile acids comes from the liver and then transformed into secondary bile acids by microbes. BARs play an important role in in metabolic regulation, however if there is suppression of bile in the GI tract; then the intestinal barrier is more susceptible to destruction. However, if you are producing a low bile count or obstructed bile flow, it can be the result of the microbes translocating to the small intestines and causing mucosal inflammation, SIBO and leaky gut.
Epithelial Cells Involved in the Barrier Integrity
These cells are very important to the intestinal epithelial barrier as they can either protect the barrier walls or can lead them to their demised.
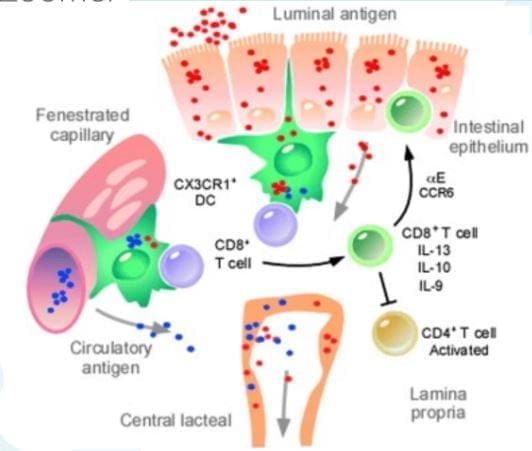
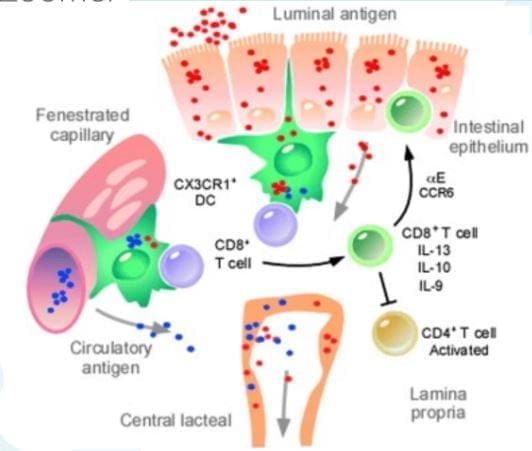
Dendritic cells: Dendritic cells are presenting antigen cells that are found the epithelial layer. These cells sample and present antigens it to Tcells, thus activating immune response. Dendritic cells help the Tcells tell the difference between self and non-self because if we eat commonly consumed foods or foreign antigens are present, we don�t want our immune system to rise up�most of the times.

Goblet cells: Goblet cells are very important of the epithelial barrier because they provide the mucus barrier that coats and protects the intestinal walls. Without this mucus barrier, we will sick and any harmful bacteria will come in and out of the intestinal barriers.
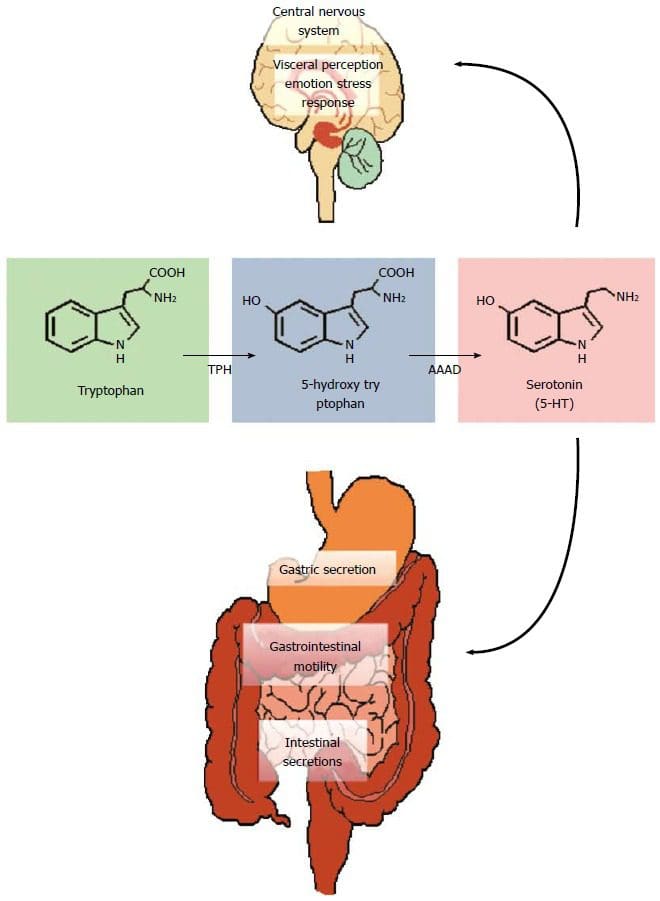
Enteroendocrine cells: Enteroendocrine cells host receptors and produce a wide range of hormones, enzymes and neurotransmitters that affect or control our appetite, digestive functions, motility and interacts with microbial communities. However, these cells can either be beneficial or not if the host diet is in played.
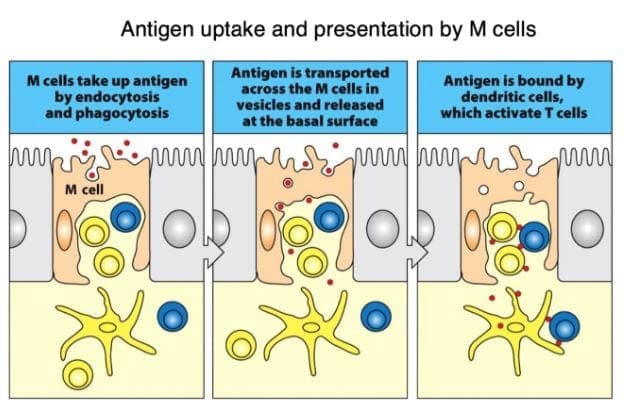
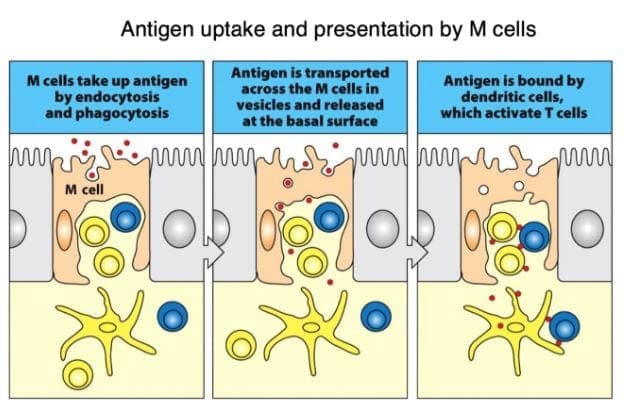
M cells: Microfold cells or M cells are located over the Peyer�s patches and they constantly sample outside the intestinal epithelial barriers for any microbes that pose a threat. They also present antigens from the outside to the dendritic cells to activate the Tcell response, as well as consuming the antigen by neutralizing it. Without the M cells, we risk of losing tolerance to microbes, thus causing inflammation on our intestinal barriers.
Conclusion
In total, we now have a deeper knowledge of our gut system as well as taking an in depth look on what our intestinal gut goes through to stop inflammation. In order to stop leaky gut, we must change our eating habits gradually when we want a healthier life. Dr. Alexander Jimenez does discuss to our patients the importance of protecting our gut with functional medicine as well as, encouraging our patients to take that first step into a healthy lifestyle.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Gut and Intestinal Health
Ah� the bathroom, nature�s thinking room. The one place where we create many thoughts that turn into ideas, a place to read, and the place where we want peace and quiet. Known as many different names,� the bathroom is the one place where we flush out our systems after consuming quantities of food. However, did you know that the bile inside your body plays a huge important role in our system?

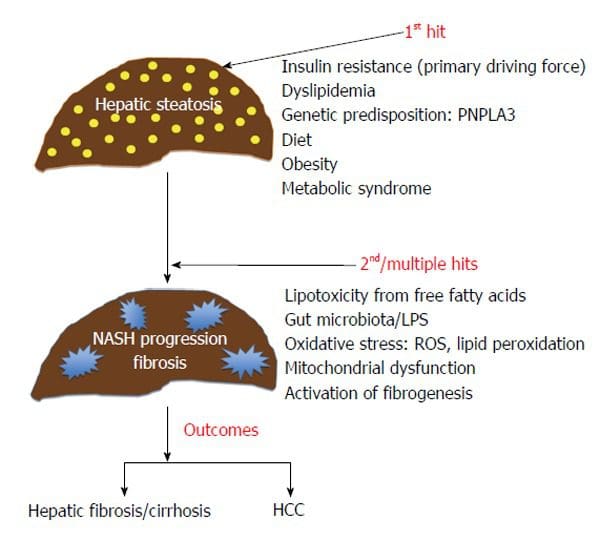
Bile is a vital body fluid that absorbs nutrients in our small intestines and flushes the toxins out of the liver. Bile continuously is being produced in the liver and then stored in the gallbladder. It also works as a signal molecule for both inside and outside the liver as well. When the liver and bile is disruptive, it can cause many problems for the body.
TCM (Traditional Chinese Medicine) stated that the liver is known as the �master organ� and it is the causative factor in many of the body�s ailments. When there are major imbalances on our bodies, it causes liver dysfunction. In TCM, the liver actually helps with detoxification; enzyme, hormone, and bile production, immune cell activation and stores vitamins and iron.
How Does the Liver Work?
The liver�s main job is to get rid of bile in our internal system. Not only that but the liver plays an important role by distributing nutrients by converting those nutrients into metabolizing energy. As well as storing vitamins and minerals for later use.
However, in today�s fast-paced society, the liver can�t perform right as we don�t give the liver it�s essential nutrients that it needs to function. Which causes blockage in the gallbladder, diseases, and digestive issues.
The Importance of Bile
As stated, bile has many functions that play an important part in the liver. Bile actually lubricates our small intestines and stool for easy disposal. But when there is less lubrication in our small intestines and stool, it can lead to constipation and too much lubrication can lead to diarrhea.
There is also a chance of blockage in bile where it can increase the accumulation of toxins in our body which creates oxidative stress and back up our waste matter. When we eat too much food and it�s still in our intestines, it will ferment and causes a leaky gut as toxic gasses penetrate the intestinal lining.
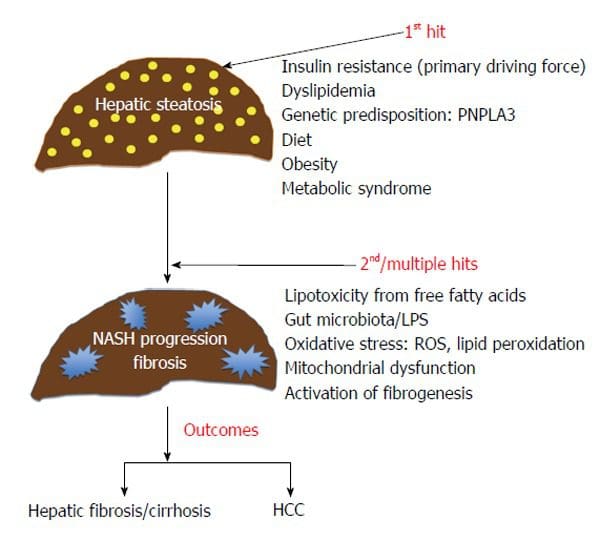
Another function is that the bile salts break down and processes fats that are essential for weight loss. Bile can also transport toxins out of our liver to feces while keeping everything free-flowing. When there isn�t enough bile being produced, cholesterol stones are forming.
Vitamins like, vitamin A, D, E and K can break down the excess fat in the body if there is an adequate amount of bile. But if patients had gallbladder surgery must be taken to account that they don�t have a bile storage system, and must manage their bile production.
Liver Functions for Hormonal Balance
Did you know that the liver and thyroid have a synergistic relationship? That�s because the T4 is converted to T3 for the liver. It turns out that the T3 is more potent in the thyroid hormone and is metabolized from iodine. When a patient has a thyroid problem, it could actually be the result of a bile or liver malfunction.
When our mood and mental state is imbalanced, it can be the results of a sick or fatty liver. Due to the fact that the liver influencing on our hormones. Because our mental state and our moods correlate to our hormones, it is important to keep the liver healthy but also finding a good place in our state of mind to make sure that we keep our liver healthy as well.
Signs of Liver Imbalance
There are many symptoms that can cause the liver to be imbalanced and can contribute to a low bile count:
- Constipation, bloating, gas
- Leaky gut
- Fatigue
- Weight gain
- Irregular stool
- High cholesterol
- Tendon problems
Ways to Support the Liver and Produce More Bile
Now that we understand what symptoms that causes our liver to be imbalanced, here are 5 ways to make sure that you are protecting your liver and producing a healthy amount of bile.
- Removing Causative Factors
The first and foremost factor in protecting your liver is to get rid of the causative factors that are harming your liver. Things like an excessive amount of lactate in coffee, sugars, alcohol, and processed foods can disrupt your liver�s health. It�s ok to enjoy those things sparsely but, if you are trying to maintain a healthy liver, it�s best to ease up on the consumption of those lactate factors as much as possible.
- Eating Liver Supportive Foods
There are many foods that actually help support the liver. Grapefruit, blueberries, cranberries, prickly pears, and bitter greens are just some of the foods that can actually help your liver and bile production. We here at Injury Medical Clinic, always inform our patients the importance of whole nutritious food to heal and repair what ailments in our patient�s bodies.
- Practicing Deep Breathing Exercise
Practicing deep breathing exercises have been known to lower stress and diaphragmatic breathing exercises is no exception. Since the liver is positioned below the diaphragm, when we do any deep breathing exercises; these motions actually massages our liver and stimulate bile production. Hence why singers do these exercises when they are getting ready to perform. They are massaging their liver without even knowing it.
- Intermittent Fasting
Since we now know that bile is continuously being produced in the liver and being stored into the gallbladder when we are not eating, intermittent fasting is a good way to increase the bile production in the gallbladder. Plus it has been known for weight loss and beneficial for the body to heal while getting rid of the junk in our cells.
- Stress Less
Stress is one of the huge factors that can either cause our body to improve our immune system or causes the body to chronic illness. Emotional stress is known to cause a huge burden to our organs because it is tied to our hormones. When we get emotionally stressed, our liver cannot get rid of the excess toxins and hormones.� So we have to find ways to de-stressed ourselves so we won�t hurt our organs, especially the liver.
Conclusion
So when it comes to our liver, we must make sure that the bile that we are producing is turning into energy all the way to feces. So, when we have to go to the bathroom we can let out the toxins naturally without any complications. If we can lower the factors that are causing us to have an inadequate bowel movements, then we can improve our body�s ability to detoxify.
NCBI Resources
Western diets, high in sugar and fat, cause liver inflammation, especially in males, according to a new animal study in�The American Journal of Pathology. Inflammation was most pronounced in males that lacked farnesoid x receptor (FXR), a bile acid receptor.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Gut and Intestinal Health, Oxidative Stress
Ever wondered why you feel sluggish from a long day? Or feel sick to the stomach when you ate something bad or overindulged on your favorite food? Could it be that your gut is showing signs of stress and discomfort due to certain habits that you may encounter and didn�t even know about it?
In our previous article, we talked about the six types of food that our gut needs to be healthy. Since our gut contains trillions of microbiomes, both good and bad, these microbiomes play an important role in our overall health. A healthy microbiome improves our gut health, heart health, brain health, controls our weight and regulates our blood sugar. With the good bacteria in our gut, the bacteria benefit us with a good digestive system and destroys the harmful bacteria. But certain lifestyles and diet choices can actually increase the bad bacteria and lower the good bacteria and overall health.
Here are five surprisingly lifestyle choices that are hurting your gut:
Not Eating a Wide Range of Foods
Our gut plays an important role in our overall health. When we eat good whole foods, our gut is happier; we have more energy to complete any task that is thrown at us and we are getting nutrients for our gut flora. However, during the past couple of decades, we have been leaning more into processed foods due to the economic pressures of increased food productions. FOA stated that �75 percent of the world�s food is generated from only 12 plants and five animal species� and that is very bad to our gut flora.
Here at Injury Medical & Chiropractic Clinic, we inform our patients about the importance of eating nutritious, whole foods to promote not only a healthy gut but a healthy mind. When the body gets introduced to a wide variety of whole foods (with a high fiber content), our gut starts to repair the damage of processed food that we may have consumed internally.
Inadequate Prebiotic Consumption
Prebiotics are the fibers that don�t need to be digested and can pass through our gut. That may seem like a waste however, prebiotics encourages friendly bacteria to grow in our gut. Any high-fiber fruits like apples can actually help to grow helpful microbes like Bifidobacteria.
However, when you disregard prebiotics to your diet, you are harming your digestive health. Without prebiotics, our digestive system slows down the development and diversity for our gut flora. So in order to have a healthy microbiome development, you need to incorporate foods filled with both digestible and indigestible fibers to your diet. Some foods included in this category are oats, nuts, onions, garlic, leeks, asparagus, bananas, pears, chickpeas, and beans.
Sticking to a high fiber diet maybe challenging however, there is the option of taking prebiotic supplements. If you have a food allergen or food sensitivity to any high enriched fiber foods, taking prebiotic supplements can actually help grow Bifidobacterium and Faecalibacterium in your gut and be beneficial to your health without the discomfort.
Excessive Alcohol Consumption
Every adult enjoys alcohol once in a while. Yes, it�s one of those beverages that help you relax a bit after a long day, however, too much of it can lead to alcohol abuse and addiction. So, did you know that consuming that much alcohol is bad for your heart, liver, and brain; thus hurting your gut health and giving you dysbiosis?
One study stated, that the alcoholics with dysbiosis had a lower median abundance of Bacteroidetes and a high abundance of Proteobacteria. The ones that weren�t alcoholics were not affected by the study.
However; there is some good news on limiting yourself to alcoholism and that it can be beneficial to your gut bacteria. If you moderately consumed red wine responsibly, the polyphenols in the wine can help benefit your gut flora. So, enjoy a glass of wine once in a while as a small treat that should not be taken for granted.
Inadequate Sleep
In one of the previous articles, we talked about how to achieve a good night sleep through herbs. When we get little to no sleep through our hectic lives, it affects us through various health problems, including heart disease and obesity. In a 2016 study, researchers discovered the effect of short-term sleep deprivation on the gut microbiota after two days.
When our body doesn�t receive the recommended 8 hours of sleep, our gut takes a huge toll as we feel sluggish and exhausted. So, to make sure that our gut microbiome will be taken care of, we recommended to turn off your electronical devices at least 30 minutes before you get ready to settle down for the night. Turn off all the lights, and don�t drink any liquids at least two hours before bed, close your eyes and take a deep breath in a meditative state, and relax as you drift off into slumber town.
Inadequate Exercise
Through our fast-paced lifestyle and stressful jobs, it�s hard to find time to exercise. But when we actually do find time to exercise, not only do our minds feel good; but our body and gut feel good as well. However, things always come up when we are in an exercise routine and we have to skip exercising altogether. It happens to all of us and it�s hard to pick up where we left off when we tried to exercise.
When we don�t exercise at least a couple of times out of the week, our bodies take a huge toll on us as we gained weight, our stress is way too high, and we have a higher chance of getting a chronic disease. When this happens our gut flora is a huge disadvantage. Here at the clinic, we strive to inform our patients about the importance of exercising and that it not only changes their lives but also changes their mood entirely.
However, don�t just go into a hard exercise routine where you will injure yourself. Start off with a low-intensity workout then build it up as you go because your gut flora will thank you for it.
As a final say, we here at Injury Medical want to keep you informed on nutrition and ways to help you improve your ailments with these 5 surprises. But to also educate you on what may be hurting your gut. With these surprises and slight changes to your daily life, your gut will be thanking you for the long haul.
NCBI Resources
According to evidence from a 2016 research study, the gut�s immune system is fundamental towards preventing a variety of diseases and it may often contribute to metabolic disorders. However, it might also help provide a treatment goal when observing systemic inflammation in insulin resistance. Moreover, modified gut immunity has been linked with changes to the gut microbiota, intestinal barrier function, gut-residing immune cells, and resistance to antigens which enter the gastrointestinal, or GI, system. Although this has been previously believed to raise the danger of esophageal ailments including, pathogenic infections and chronic inflammation, which may ultimately lead to chronic health issues.

by Dr Alex Jimenez DC, APRN, FNP-BC, CFMP, IFMCP | Gut and Intestinal Health
Vibrant America is at the forefront of modern medicine and is a leader in autoimmune diagnostics. Vibrant America has the ability and technology to get high-quality, accurate test results down to the peptide level.
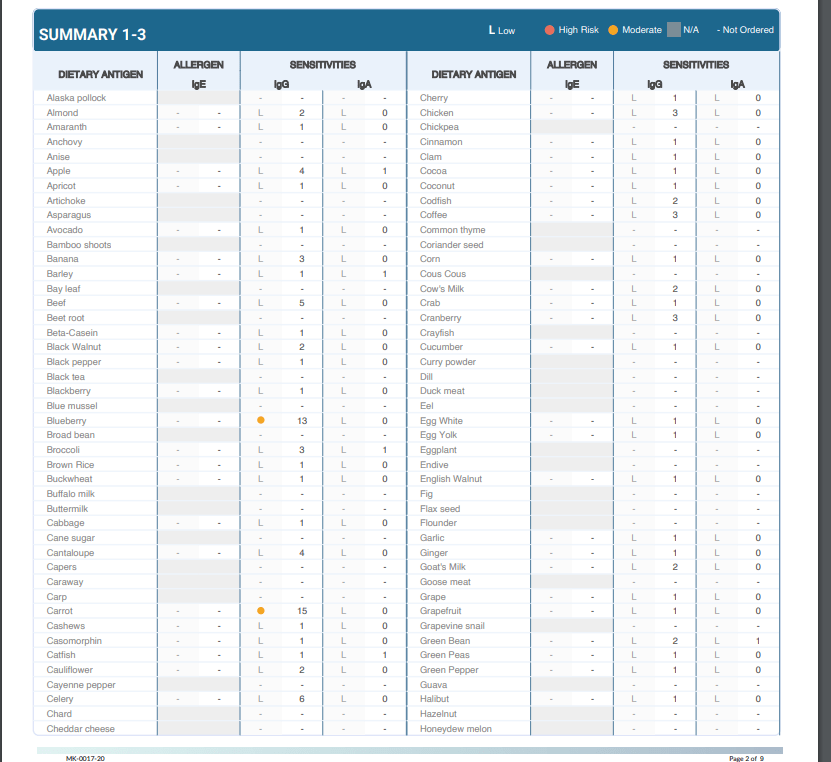
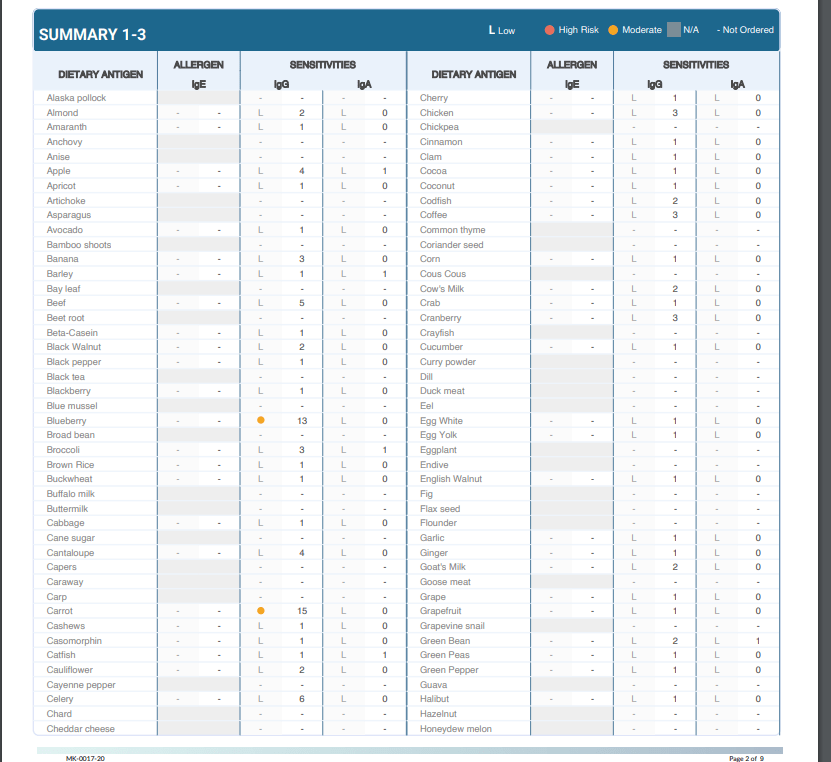
One of the many tests we utilize from Vibrant America at Injury Medical & Chiropractic Clinic is Food Sensitivity. With this test, we are able to analyze 96 of the most common foods that are consumed. This is important because food sensitivities can occur hours or days after the food is consumed. Many individuals who suffer from digestive orders, migraines, weight gain, and inflammation might not realize it is from food sensitivities.
Why test for Food Sensitivity?
Not only do food sensitivities leave you with uncomfortable side effects days after ingestion, but they are damaging your gut. In a healthy gut, the intestinal lining will provide immunity to food antigens. The food we eat is not supposed to cross the intestinal barrier. However, in an unhealthy gut, the intestinal lining becomes damaged due to inflammation and an under abundance of healthy flora. This allows food particles to pass through into the bloodstream which then causes an IgG antibody response. This is commonly referred to as a “leaky gut”. This can result in further inflammation and can contribute to some diseases.
What Is Leaky Gut Syndrome And How Do You Fix It?
When to test:
At Injury Medical, we want all of our patients to feel their best. On top of chiropractic care, we also offer functional medicine. When a patient mentions to us that they are having symptoms correlated to “leaky gut” such as abdominal pain, bloating, gas, skin itchiness, rashes like eczema, nausea, vomiting, joint pain, muscle stiffness, or feeling weak, we recommend running a food sensitivity panel.
How it works:
Once we sit down and have a detailed conversation, we send you to the labs with a “kit”. This “kit” provides the phlebotomist with everything they need in order to draw blood for the tests we order.
From here, the blood gets sent to Vibrant America. The blood is then examined all the way down to the peptide level. This allows a team of clinicians to discover the IgG and IgA antibody numbers in reaction to 96 foods (including dairy, meat, seafood, fruits, vegetables, grains, nuts, etc.).
Next, the results are sent back to us at Injury Medical Clinic. Dr. Jimenez and I ( Kenna Vaughn, Senior Health Coach), study these results to determine a proper treatment protocol. In addition to this, we have a team of clinicians that review each case with us, in order to fully understand what each result looks like and how to best approach it with the patient’s specific lifestyle.
Below is an example of how a patients test results would look:
Why this works
As mentioned above, food sensitivities have a delayed response. This testing works because it allows us to see what foods are responsible for the symptoms/reactions without the patient having to do an elimination diet.� With these results, the patient can start to make adjustments to their diet with our help in order to start feeling better and reducing their symptoms. The key to a healthy life is a healthy gut.
No one should have to live with uncomfortable symptoms or pain. If you or someone you know is experiencing these symptoms, come into Injury Medical Clinic where we can assess your needs and help you get on track to feeling better! – Kenna Vaughn, Senior Health Coach
Disclaimer: It is important to remember that food sensitivity testing and food allergy testing are not the same. Food allergies involve an IgE antibody and are an immediate reaction and can occur within minutes.