The rule of 4 of the brainstem: a simplified method for understanding brainstem anatomy and brainstem vascular
syndromes for the non-neurologist.
Contents
The Rule Of 4 & The Brainstem
The rule of 4 is a simple method developed to help �students of neurology� to remember the anatomy of the brainstem and thus the features of the various brainstem vascular syndromes. As medical students, we are taught detailed anatomy of the brainstem containing a bewildering number of structures with curious names such as superior colliculi, inferior olives, various cranial nerve nuclei and the median longitudinal fasciculus. In reality when we do a neurological examination we test for only a few of these structures. The rule of 4 recognizes this and only describes the parts of the brainstem that we actually examine when doing a neurological examination. The blood supply of the brainstem is such that there are paramedian branches and long circumferential branches (the anterior inferior cerebellar artery (AICA), the posterior inferior cerebellar artery (PICA) and the superior cerebellar artery (SCA). Occlusion of the paramedian branches results in medial (or paramedian) brainstem syndromes and occlusion of the circumferential branches results in lateral brainstem syndromes. Occasionally lateral brainstem syndromes are seen in unilateral vertebral occlusion. This paper describes a simple technique to aid in the understanding of brainstem vascular syndromes.
Any attempt to over simplify things runs the risk of upsetting those who like detail and I apologize in advance to the anatomists among us, but for more than 15 years this simple concept has helped numerous students and residents understand, often for the first time, brainstem anatomy and the associated clinical syndromes that result.
In The Rule Of 4 There Are 4 Rules:
- There are 4 structures in the �midline� beginning with M.
- There are 4 structures to the side beginning with S.
- There are 4 cranial nerves in the medulla, 4 in the pons and 4 above the pons (2 in the midbrain).
- The 4 motor nuclei that are in the midline are those that divide equally into 12 except for 1 and 2, that is 3, 4, 6 and 12 (5, 7, 9 and 11 are in the lateral brainstem).
If you can remember these rules and know how to examine the nervous system, in particular the cranial nerves, then you will be able to diagnose brainstem vascular syndromes with ease.
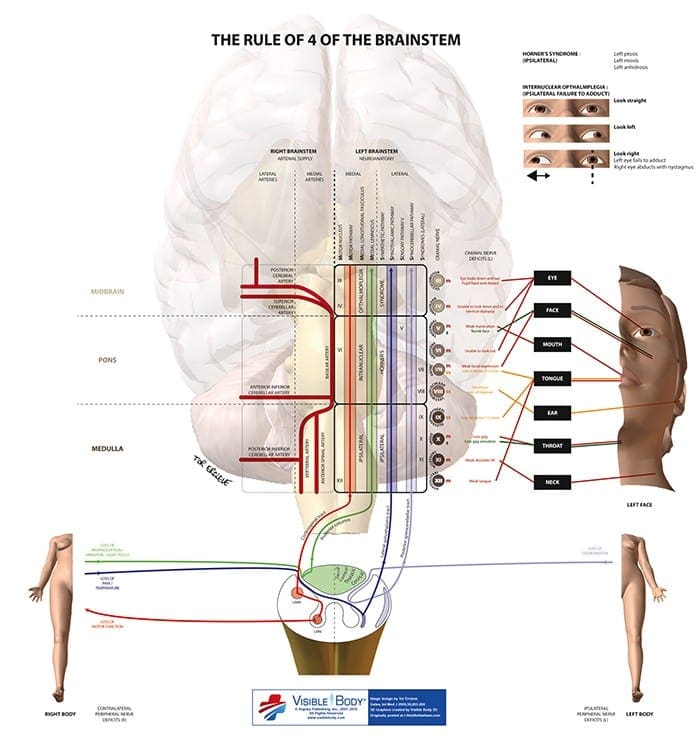
Figure 1 shows a cross-section of the brainstem, in this case at the level of the medulla, but the concept of 4 lateral and 4 medial structures also applies to the pons, only the 4 medial structures relate to midbrain vascular syndromes.
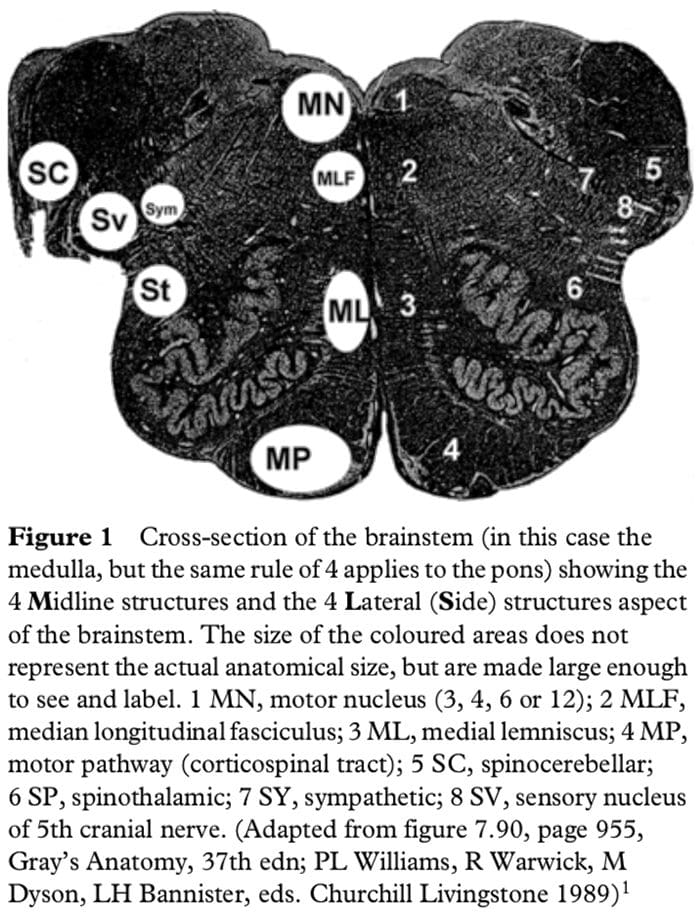
The 4 Medial Structures & The Associated Deficit Are:
- The Motor pathway (or corticospinal tract): contra lateral weakness of the arm and leg.
- The Medial Lemniscus: contra lateral loss of vibration and proprioception in the arm and leg.
- The Medial longitudinal fasciculus: ipsilateral inter- nuclear ophthalmoplegia (failure of adduction of the ipsilateral eye towards the nose and nystagmus in the opposite eye as it looks laterally).
- The Motor nucleus and nerve: ipsilateral loss of the cranial nerve that is affected (3, 4, 6 or 12).
The 4 Lateral Structures & The Associated Deficit Are:
- The Spinocerebellar pathways: ipsilateral ataxia of the arm and leg.
- The Spinothalamic pathway: contra lateral alteration of pain and temperature affecting the arm, leg and rarely the trunk.
- The Sensory nucleus of the 5th: ipsilateral alteration of pain and temperature on the face in the distribution of the 5th cranial nerve (this nucleus is a long vertical structure that extends in the lateral aspect of the pons down into the medulla).
- The Sympathetic pathway: ipsilateral Horner�s syndrome, that is partial ptosis and a small pupil (miosis)
These pathways pass through the entire length of the brainstem and can be likened to �meridians of longitude� whereas the various cranial nerves can be regarded as �parallels of latitude�. If you establish where the meridians of longitude and parallels of latitude intersect then you have established the site of the lesion.
Figure 2 shows the ventral aspect of the brainstem.
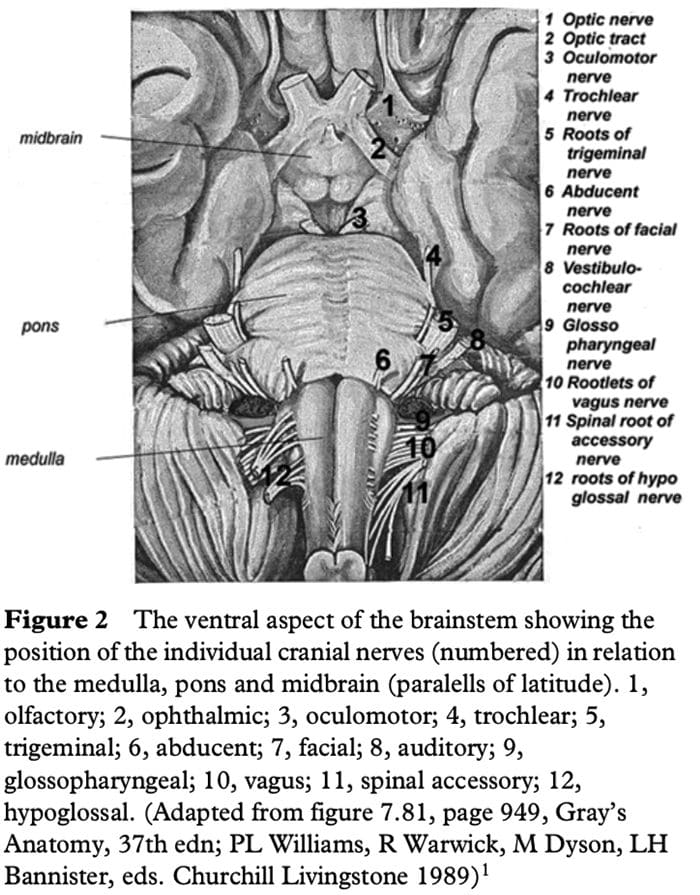
The 4 Cranial Nerves In The Medulla Are:
9 Glossopharyngeal: ipsilateral loss of pharyngeal sensation.
10 Vagus: ipsilateral palatal weakness.
11 Spinal accessory: ipsilateral weakness of the trapezius and sternocleidomastoid muscles.
12 Hypoglossal: ipsilateral weakness of the tongue.
The 12th cranial nerve is the motor nerve in the midline of the medulla. Although the 9th, 10th and 11th cranial nerves have motor components, they do not divide evenly into 12 (using our rule) and are thus not the medial motor nerves.
The 4 Cranial Nerves In The Pons Are:
5 Trigeminal: ipsilateral alteration of pain, temperature and light touch on the face back as far as the anterior two-thirds of the scalp and sparing the angle of the jaw.
6 Abducent: ipsilateral weakness of abduction (lateral movement) of the eye.
7 Facial: ipsilateral facial weakness.
8 Auditory: ipsilateral deafness.
The 6th cranial nerve is the motor nerve in the pons.
The 7th is a motor nerve but it also carries pathways of taste, and using the rule of 4 it does not divide equally in to 12 and thus it is not a motor nerve that is in the midline. The vestibular portion of the 8th nerve is not included in order to keep the concept simple and to avoid confusion. Nausea and vomiting and vertigo are often more common with involvement of the vestibular connections in the lateral medulla.
The 4 Cranial Nerves Above The Pons Are:
4 Olfactory: not in midbrain.
5 Optic: not in midbrain.
6 Oculomotor: impaired adduction, supraduction and infraduction of the ipsilateral eye with or without a dilated pupil. The eye is turned out and slightly down.
7 Trochlear: eye unable to look down when the eye is looking in towards the nose.
The 3rd and 4th cranial nerves are the motor nerves in the midbrain.
Thus a medial brainstem syndrome will consist of the 4 M�s and the relevant motor cranial nerve, and a lateral brainstem syndrome will consist of the 4 S�s and either the 9�11th cranial nerve if in the medulla, or the 5th, 7th and 8th cranial nerve if in the pons.
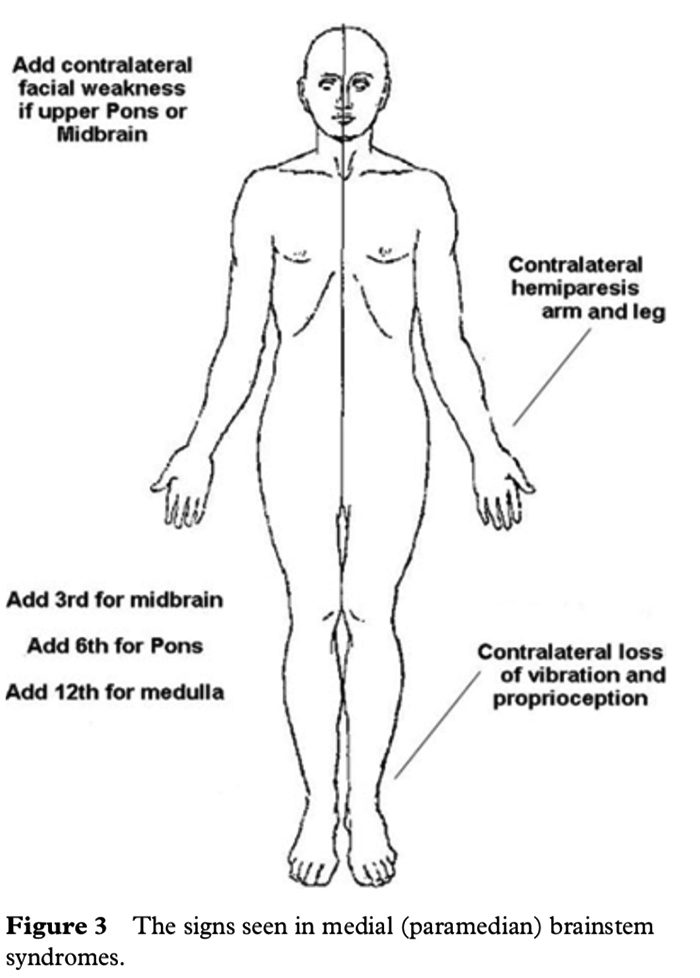
MEDIAL (PARAMEDIAN) BRAINSTEM SYNDROMES
Let us assume that the patient you are examining has a brainstem stroke. If you find upper motor neurone signs in the arm and the leg on one side then you know the patient has a medial brainstem syndrome because the motor pathways is paramedian and crosses at the level of the foramen magnum (decussation of the pyramids). The involvement of the motor pathway is the �meridian of longitude�. So far the lesion could be anywhere in the medial aspect of the brainstem, although if the face is also affected it has to be above the mid pons, the level where the 7th nerve nucleus is.
The motor cranial nerve �the parallels of latitude� indicates whether the lesion is in the medulla (12th), pons (6th) or midbrain (3rd). Remember the cranial nerve palsy will be ipsilateral to the side of the lesion and the hemiparesis will be contralateral. If the medial lemniscus is also affected then you will find a contra lateral loss of vibration and proprioception in the arm and leg (the same side affected by the hemiparesis) as the posterior columns also cross at or just above the level of the foramen magnum. The median longitudinal fasciculus (MLF) is usually not affected when there is a hemiparesis as the MLF is further back in the brainstem.
The MLF can be affected in isolation �a lacunar infarct� and this results in an ipsilateral internuclear ophthalmoplegia, with failure of adduction (movement towards the nose) of the ipsilateral eye and leading eye nystagmus on looking laterally to the opposite side of the lesion in the contra lateral eye. If the patient had involvement of the left MLF then, on being asked to look to the left, the eye movements would be normal, but on looking to the right the left eye would not go past the midline, while there would be nystagmus in the right eye as it looked to the right.
Figure 3 shows the clinical features of the medial brainstem syndromes.
 LATERAL BRAINSTEM SYNDROMES
LATERAL BRAINSTEM SYNDROMES
Once again we are assuming that the patient you are seeing has a brainstem problem, most likely a vascular lesion. The 4 S�s or �meridians of longitude� will indicate that you are dealing with a lateral brainstem problem and the cranial nerves or �parallels of latitude� will indicate whether the problem is in the lateral medulla or lateral pons.
A lateral brainstem infarct will result in ipsilateral ataxia of the arm and leg as a result of involvement of the Spinocerebellar pathways, contralateral alteration of pain and temperature sensation as a result of involvement of the Spinothalamic pathway, ipsilateral loss of pain and temperature sensation affecting the face within the distribution of the Sensory nucleus of the trigeminal nerve (light touch may also be affected with involvement of the spinothalamic pathway and/or sensory nucleus of the trigeminal nerve). An ipsilateral Horner�s syndrome with partial ptosis and a small pupil (miosis) is because of involvement of the Sympathetic pathway. The power tone and the reflexes should all be normal. So far all we have done is localize the problem to the lateral aspect of the brainstem; by adding the relevant 3 cranial nerves in the medulla or the pons we can localize the lesion to this region of the brain.
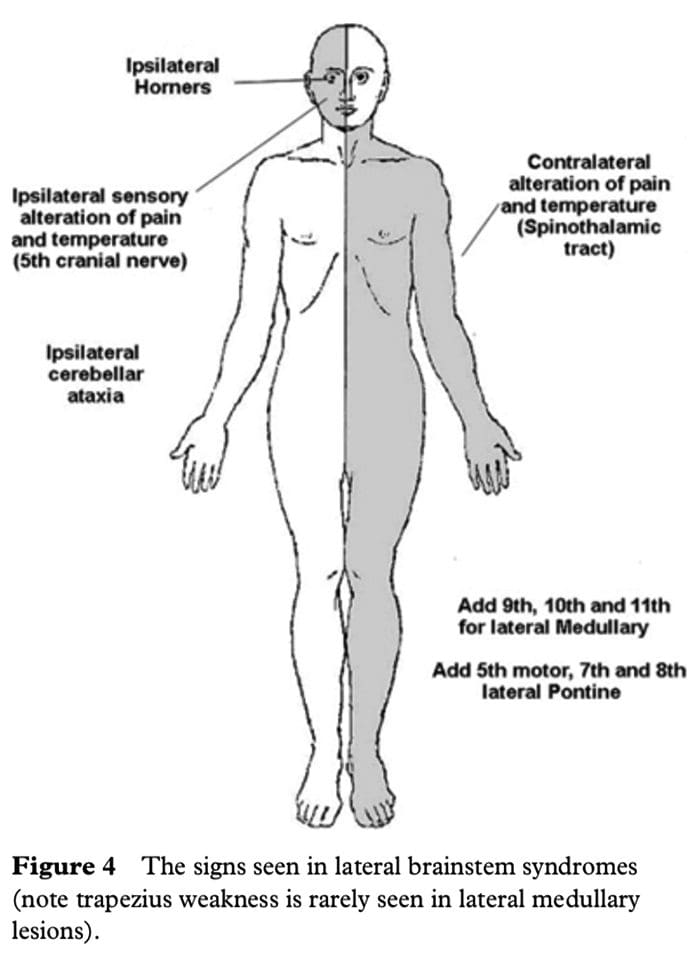 The lower 4 cranial nerves are in the medulla and the 12th nerve is in the midline so that 9th, 10th and 11th nerves will be in the lateral aspect of the medulla. When these are affected, the result is dysarthria and dysphagia with an ipsilateral impairment of the gag reflex and the palate will pull up to the opposite side; occasionally there may be weakness of the ipsilateral trapezius and/or sternocleidomastoid muscle. This is the lateral medullary syndrome usually resulting from occlusion of the ipsilateral vertebral or posterior inferior cerebellar arteries.
The lower 4 cranial nerves are in the medulla and the 12th nerve is in the midline so that 9th, 10th and 11th nerves will be in the lateral aspect of the medulla. When these are affected, the result is dysarthria and dysphagia with an ipsilateral impairment of the gag reflex and the palate will pull up to the opposite side; occasionally there may be weakness of the ipsilateral trapezius and/or sternocleidomastoid muscle. This is the lateral medullary syndrome usually resulting from occlusion of the ipsilateral vertebral or posterior inferior cerebellar arteries.
The 4 cranial nerves in the pons are: 5th, 6th, 7th and 8th. The 6th nerve is the motor nerve in the midline, the 5th, 7th and 8th are in the lateral aspect of the pons, and when these are affected there will be ipsilateral facial weakness, weakness of the ipsilateral masseter and pterygoid muscles (muscles that open and close the mouth) and occasionally ipsilateral deafness. A tumour such as an acoustic neuroma in the cerebello-pontine angle will result in ipsilateral deafness, facial weakness and impairment of facial sensation; there may also be ipsilateral limb ataxia if it compresses the ipsilateral cerebellum or brainstem. The sympathetic pathway is usually too deep to be affected.
If there are signs of both a lateral and a medial (paramedian) brainstem syndrome, then one needs to consider a basilar artery problem, possibly an occlusion.
In summary, if one can remember that there are 4 pathways in the midline commencing with the letter M, 4 pathways in the lateral aspect of the brainstem commencing with the letter S, the lower 4 cranial nerves are in the medulla, the middle 4 cranial nerves in the pons and the first 4 cranial nerves above the pons with the 3rd and 4th in the midbrain, and that the 4 motor nerves that are in the midline are the 4 that divide evenly into 12 except for 1 and 2, that is 3, 4, 6 and 12, then it will be possible to diagnose brainstem vascular syndromes with pinpoint accuracy.
P. GATES
The Geelong Hospital, Barwon Health, Geelong, Victoria, Australia
REFERENCES
1 Chapter 7. Neurology. In: Williams PL, Warwick R, Dyson M, Bannister LH, eds. Gray�s Anatomy, 37th edn. Edinburgh: Churchill Livingstone; 1989; 860�1243.
General Disclaimer, Licenses and Board Certifications *
Professional Scope of Practice *
The information herein on "Brainstem And The Rule Of 4 | El Paso, TX." is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and on our family practice-based chiromed.com site, focusing on naturally restoring health for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez, DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card