Axial neck pain is also known as uncomplicated neck pain, whiplash, and cervical/neck strain. They refer to pain and discomfort running along the back or posterior of the neck. Axial is defined as forming or around an axis. This type of pain stays around the neck and immediate surrounding structures. It does not spread/radiate out to the arms, hands, fingers, and other areas of the body. Axial neck pain differs from two other neck conditions. They are:
Cervical radiculopathy describes irritation or compression/pinching of the nerve as it exits the spinal cord. The nerves of the cervical spine are known as the peripheral nerves. They are responsible for relaying signals to and from the brain to specific areas of the arms and hands. The signals sent from the brain are for muscle movement, while signals going to the brain are for sensation.

When one of these nerve/s gets irritated, inflamed, or injured, it can result in:
- Muscle pain
- Weakness
- Numbness
- Tingling sensation
- Burning pain
- Other types of abnormal sensations in the arms, hands, or fingers.
Cervical myelopathy describes compression of the spinal cord itself. The spinal cord is the information highway/pipeline to all parts of the body. There is a range of symptoms that can include:
- Same symptoms as cervical radiculopathy
- Balance problems
- Coordination problems
- Loss of fine motor skills
- Bowel and bladder incontinence
Contents
Axial neck pain
Axial neck pain is a quite common type of neck pain. It affects around 10% of the population. However, the majority of these cases do not involve severe symptoms that limit daily activity.
Symptoms
Pain in the back of the neck is the primary and most common symptom. Sometimes the pain travels to the base of the skull, shoulder, or shoulder blade. Other symptoms include:
- Neck stiffness
- Headaches
- Localized muscle pain
- Warmth
- Tingling

Developmental Risk factors
Poor posture, lack of ergonomics, and muscle weakness increase the chances of developing axial neck pain. Risk factors for development include:
- Age
- Trauma – Auto accident, sports, personal, work injury
- Headaches
- Depression
- Chronic neck pain
- Sleep problems
Diagnosis
Based on symptoms and physical exam findings are how a diagnosis is usually achieved. A doctor will typically order an x-ray, CT, or MRI of the cervical spine. This calls for an immediate visit to a hospital/clinic for evaluation. There could be severe symptoms that could indicate something more dangerous, causing pain like infection, cancer, or fracture. These symptoms include:
- Prior trauma/injury from a fall, automobile accident, sports, work injury
- Fever
- Weight loss
- Night sweats
- Constant night pain
Rheumatic conditions/diseases that cause neck pain can include morning stiffness and immobility that gets better as the day progresses. If symptoms continue for more than 6 weeks, imaging of the spine could be recommended, especially for individuals that have had previous neck or spine surgery or if it could be cervical radiculopathy or myelopathy.
Treatment
There is a wide range of treatment options. Surgery is rarely required except for severe cases. Returning to normal activities almost right away is one of the most important things to prevent the pain from becoming chronic. First-line treatments typically begin with:
- Physical therapy
- Chiropractic
- Stretching routine
- Strengthening exercises
- Acetaminophen
- Anti-inflammatory medication/s
- Muscle relaxants are sometimes prescribed
If a cervical spine fracture has been diagnosed, a neck brace could be recommended for short-term use. A soft collar could be utilized if the pain is severe, but a doctor usually discontinues use after 3 days. Other non-invasive treatment options include:
- TENS – transcutaneous electrical nerve stimulation
- Electromagnetic therapy
- Qigong
- Acupuncture
- Low-level laser therapy
- Cognitive-behavioral therapy
Invasive treatments like injections, nerve ablation, and surgery are rarely required. But if necessary, it can be beneficial for those cases.

Causes
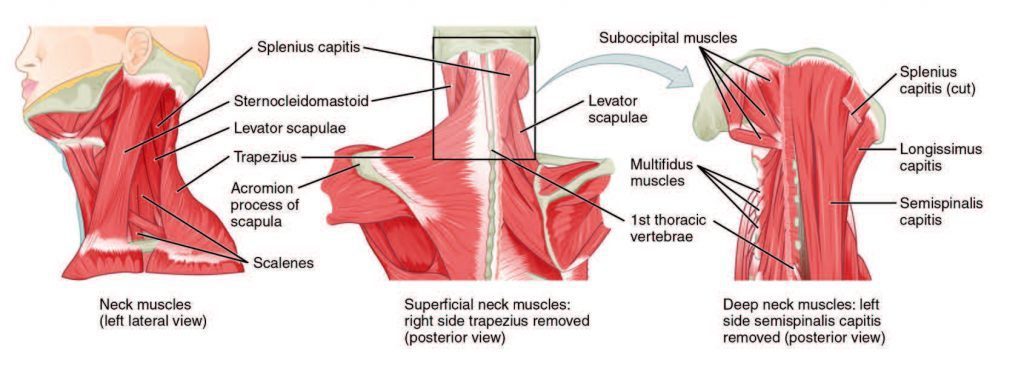
A variety of the neck’s anatomical structures can contribute to the pain. Common causes include:
- Poor posture
- Age
- Degeneration
- Ergonomics
- Injury to muscles or ligaments
- Arthritis
All of these can affect vertebral bodies, discs, and facet joints. Shoulder arthritis or a rotator cuff tear can imitate axial neck pain. Dysfunction of the temporomandibular jaw joint or the blood vessels of the neck can cause axial pain, but it is rare.
Prognosis
Symptoms are usually alleviated within 4-6 weeks from when the pain started. Pain that continues beyond this should encourage a visit to a chiropractic physician.
Prevention
- Keep neck muscles strong with exercise.
- Stretch the neck regularly.
- A healthy diet specifically for bone support.
- Proper sleep posture, for example, sleeping on the back or side with a pillow that supports the natural curve of the neck.
- If on a computer for work or a long period, align the eyes with the top third of the screen.
- Avoid looking down when on the phone, reading, etc., for a long time by keeping the arms supported on an armrest.
- Glasses should be pushed up on the nose bridge; if they slide down, there is a tendency for the head to follow.
- Don’t forget to look up frequently.
Optimizing posture, ergonomics, and muscle strengthening can help prevent the onset of pain and help alleviate the symptoms.
Whiplash Neck Pain Treatment
General Disclaimer, Licenses and Board Certifications *
Professional Scope of Practice *
The information herein on "Axial Neck Pain and Whiplash" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and on our family practice-based chiromed.com site, focusing on naturally restoring health for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez, DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card








