- Diagnosis of the diseases of the abdomen can be classified into:
- Abnormalities of the gastrointestinal tract (esophagus, stomach, small & large bowel, and the appendix)
- Abnormalities of the accessory digestive organs (Hepatobiliary & pancreatic disorders)
- Abnormalities of the genitourinary & reproductive organs
- Abnormalities of the abdominal wall and major vessels
- This presentation aims to provide the most basic understanding of general diagnostic imaging approach and appropriate clinical management of patients with the most common diseases of the abdomen
- Imaging modalities used during an investigation of the abdominal complaints:
- AP abdomen (KUB) and upright CXR
- Abdominal CT scanning (with oral and I.V. contrast and w/o contrast)
- Upper and Lower GI Barium studies
- Ultrasonography
- MRI (most used as Liver MRI)
- MRI enterography & enteroclysis
- MRI rectum
- Endoscopic Retrograde Cholangiopancreatography (ERCP)- mostly hepatobiliary and pancreatic ductal pathology
- Nuclear imaging
Contents
Why Order An Abdominal X-ray?

- Include a preliminary evaluation of bowel gas in an emergent setting. For example, a negative study in a low probability patient may obviate the need for a CT or other invasive procedures
- Evaluation of radiopaque tubes, lines, and radiopaque foreign bodies
- Post-procedural evaluation intraperitoneal/retroperitoneal free gas
- Monitoring the amount of bowel gas and resolution of postoperative (adynamic) ileus
- Monitoring the passage of contrast through the bowel
- Colonic transit studies
- Monitoring renal calculi
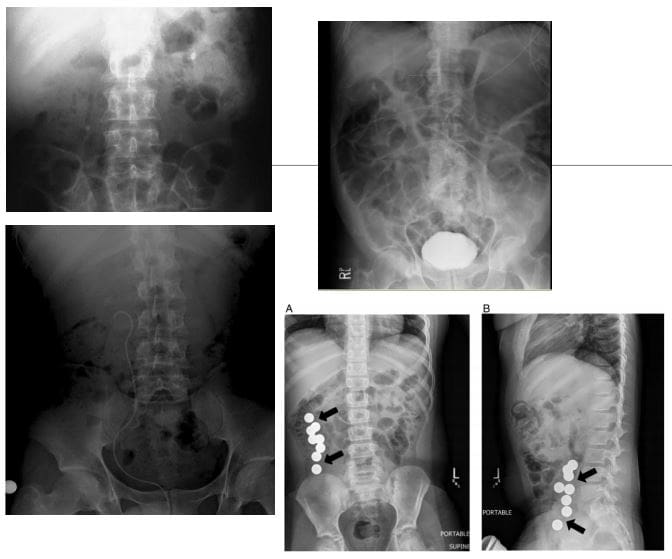
What to Note on AP Abdomen: Supine vs. Upright vs. Decubitus
- Free Air (pneumoperitoneum)
- Bowel obstruction: Dilated loops: SBO vs LBO (3-6-9 rule) SB-upper limit-3-cm, LB-upper limit-6-cm, Caecum-upper limit-9-cm. Note loss of haustra, note dilation (presence) of valvule conivente (plica semilunaris) in SBO
- SBO: note different heights air-fluid levels on upright film step ladder� appearance, typical of SBO
- Note paucity of rectal/colonic gas (evacuated) in SBO
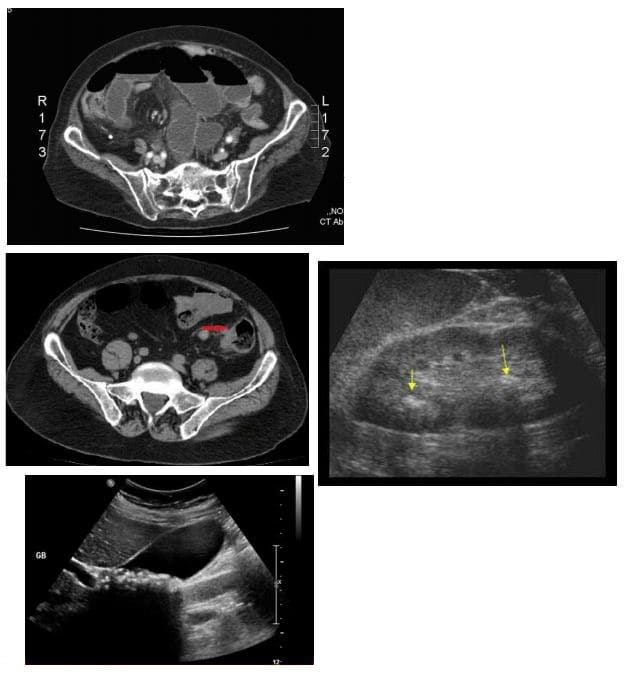
- Abdominal CT scanning -modality of choice during the investigation of acute and chronic abdominal complaints especially in adults. For example, abdominal malignancy can be successfully diagnosed and staged providing clinical information for care planning
- Abdominal, renal and pelvic ultrasound can be performed to help the diagnosis of appendicitis (esp. in children), acute & chronic vascular pathology, hepatobiliary abnormalities, obstetric and gynecological pathology
- Use of ionizing radiation (x-rays & CT) should be minimized in children and other vulnerable groups.
Diagnostic Imaging of Major Diseases of the Gastrointestinal System
- 1) Esophageal disorders
- 2) Gastric carcinoma
- 3) Gluten Sensitive Enteropathy
- 4) Inflammatory Bowel Disease
- 5) Pancreatic ductal adenocarcinoma
- 6) Colorectal carcinoma
- 7) Acute Appendicitis
- 8) Small bowel obstruction
- 9) Volvulus
Esophageal disorders
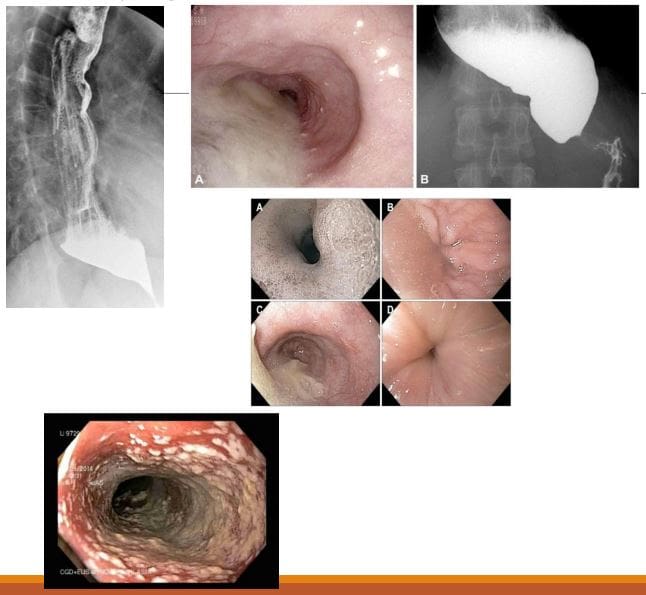
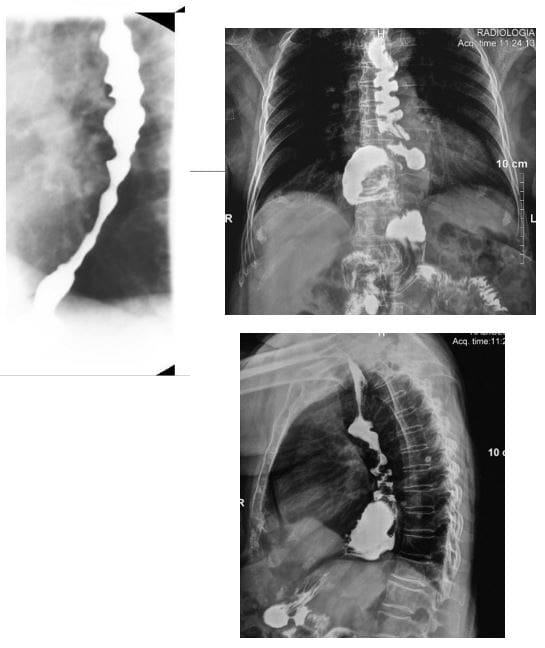
- Achalasia (primary achalasia): failure of organized esophageal peristalsis d/t impaired relaxation of the lower esophageal sphincter (LOS) with marked dilatation of the esophagus and food stasis. Obstruction of the distal esophagus (often due to tumor) has been termed “secondary achalasia” or “pseudoachalasia.� Peristalsis in the distal smooth muscle segment of the esophagus may be lost due to an abnormality of Auerbach plexus (responsible for smooth muscle relaxation). Vagus neurons can also be affected
- Primary: 30 -70s, M: F equal
- Chagas disease (Trypanosoma Cruzi infection) with the destruction of the Myenteric plexus neurons of the GI system (megacolon & esophagus)
- However, the heart is the M/C affected organ
- Clinically: Dysphagia for both solids and liquids, in comparison to dysphagia for solids only in cases of esophageal carcinoma. Chest pain and regurgitation. M/C mid esophageal squamous cell carcinoma in approximately 5% due to chronic irritation of the mucosa by stasis of food and secretions. Aspiration pneumonia may develop. Candida esophagitis
- Imaging: �Bird -beak� on upper GI barium swallow, dilated esophagus, loss of peristalsis. An endoscopic exam is crucial.
- Rx: difficult. Calcium channel blockers (short -term).Pneumatic dilatation, effective in 85% of patients with 3 -5% risk of bleeding/perforation. Botulinum toxin injection lasts only approx. 12 months per treatment. May scar the submucosa leading to increased risk of perforation during subsequent myotomy. Surgical myotomy (Heller myotomy)
- 10 -30% of patients develop gastroesophageal reflux (GERD)
- Presbyesophagus: used to describe the manifestations of degenerating motor function in the aging esophagus >80-y.o. Due to interruption of the reflex arc with decreased sensitivity to distension and alteration in peristalsis.
- Patients may complain of dysphagia or chest pain, but most are asymptomatic
- Diffuse/distal esophageal spasm (DES) is a motility disorder of the esophagus that may appear as a corkscrew or rosary bead esophagus on barium swallow.
- 2% of non-cardiac chest pain
- Manometry is the gold-standard diagnostic test.
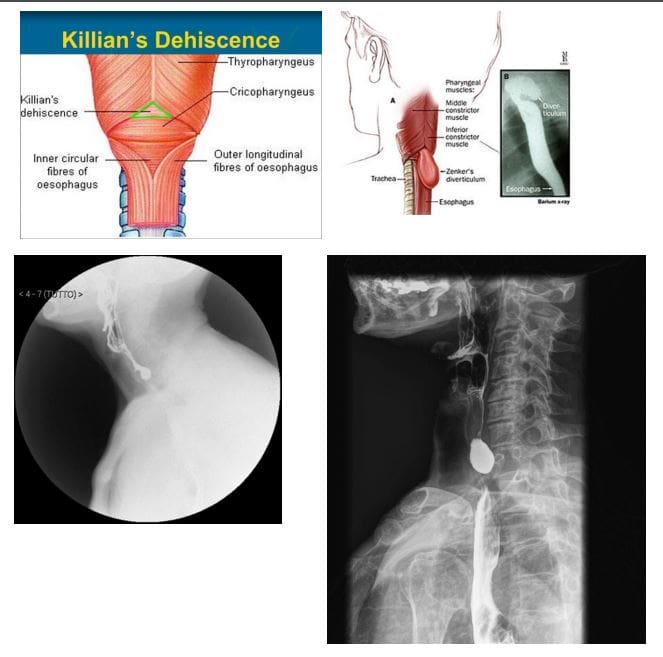
- Zenker diverticulum (ZD) aka pharyngeal pouch
- An outpouching at the level of the hypopharynx, just proximal to the upper esophageal sphincter, known as the Killian dehiscence or Killian triangle
- Patients are 60-80 y.o and present with dysphagia, regurgitation, halitosis, globus sensation
- May complicate with aspiration and pulmonary abnormalities
- Patients may accumulate medications
- ZD- is a pseudodiverticulum or pulsion diverticulum resulting from herniation of the submucosa through the Killian dehiscence, forming a sac where food and other contents may accumulate.
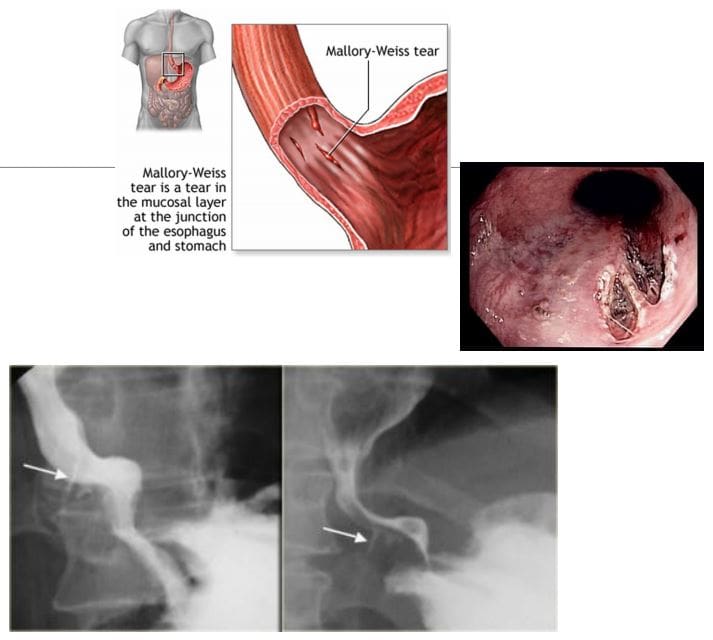
- Mallory-Weiss syndrome refers to mucosal and submucosal tears of the distal oesophageal venous plexus associated with violent retching/vomiting and projection of gastric contents against the lower esophagus. Alcoholics are at particular risk. Cases present with painless hematemesis. Treatment is typically supportive.
- Dx: imaging plays little role, but contrast esophagram may demonstrate some mucosal tears filled by contrast (bottom right image). CT scanning may help to exclude other causes of upper GI bleeding
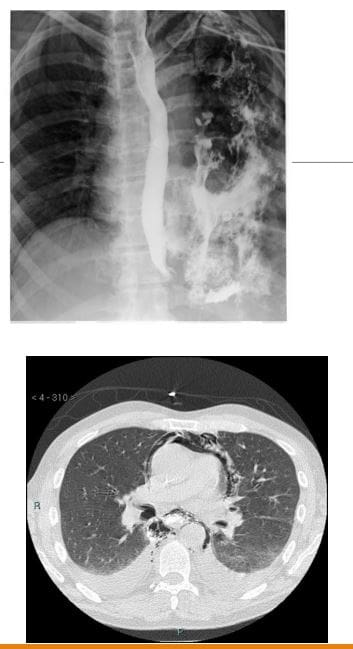
- Boerhaave syndrome: esophageal rupture secondary to forceful vomiting
- Presentation: M>F, vomiting, chest pain, mediastinitis, septic mediastinum, pneumomediastinum, pneumothorax pleural effusion
- In the past, was invariably fatal
- Mechanisms involve forceful expulsion of gastric contents especially with large undigested foods when esophagus forcefully contracts against closed glottis with 90% occurring along left posterolateral wall
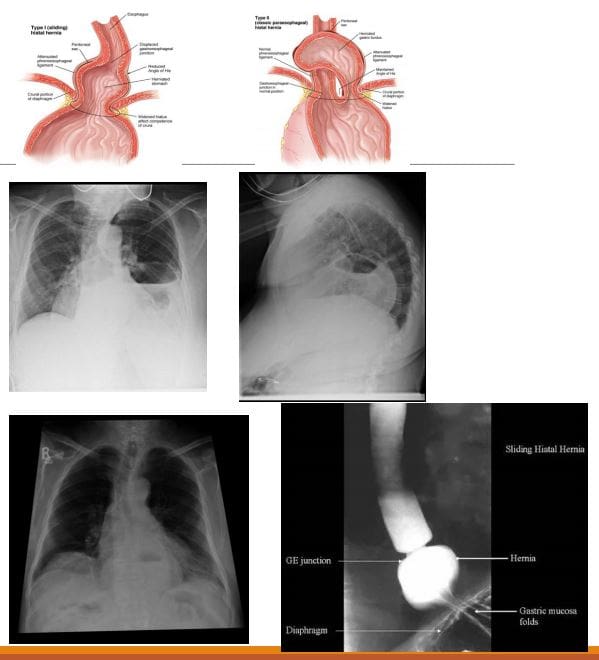
- Hiatus hernias (HH): herniation of abdominal contents through the esophageal hiatus of the diaphragm into the thoracic cavity.
- Many patients with HH are asymptomatic, and it is an incidental finding. However, symptoms may include epigastric/chest pain, postprandial fullness, nausea and vomiting
- Sometimes HH is considered synonymous with gastro-oesophageal reflux disease (GORD), but there is a poor correlation between the two conditions!
- 2-types: sliding hiatus hernia 90% & rolling (paraoesophageal) hernia 10%. The latter may strangulate leading to ischemia and complications.
- Esophageal Leiomyoma is the M/C benign esophageal neoplasm. It is often large but yet non-obstructive. Gastrointestinal stromal tumors (GIST) are the least common in the esophagus. Should be differentiated from Esophageal carcinomas.
- Imaging: contrast esophagram, upper GI barium swallow, CT scanning. Gastroesophagoscopy is the Dx method of choice.
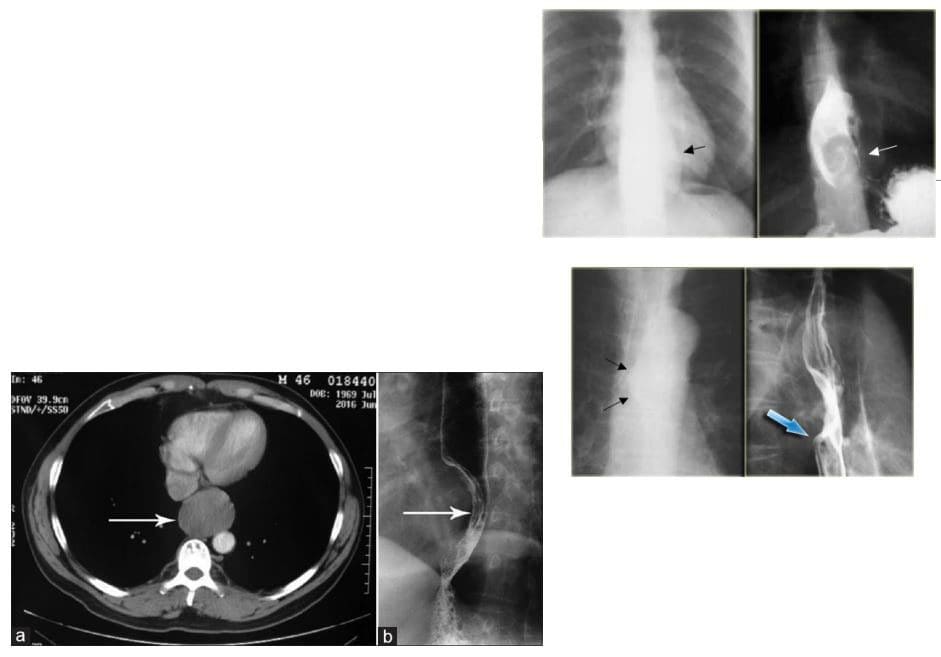
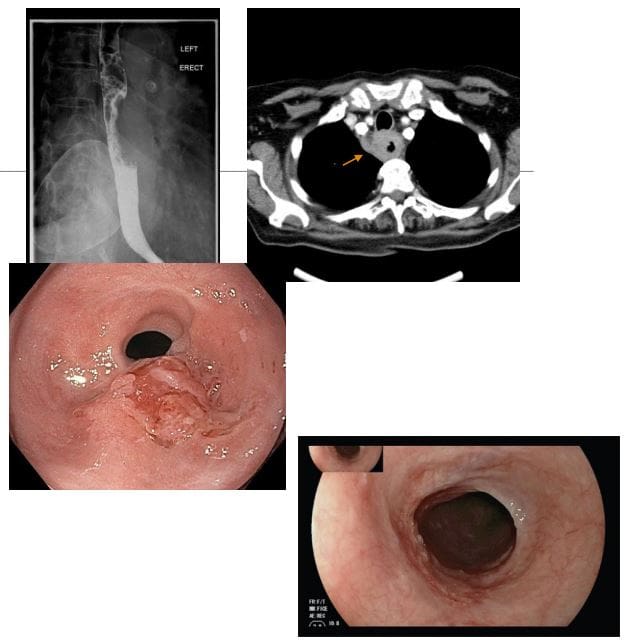
- Esophageal carcinoma: presented with increasing dysphagia, initially to solids and progressing to liquids with obstruction in more advanced cases
- <1% of all cancers and 4-10% of all GI malignancies. There is recognized male preponderance with the squamous cell subtype due to smoking and alcohol. Barrett esophagus and adenocarcinoma
- M: F 4:1. Black individuals are more susceptible than White individuals 2:1. Poor prognosis!
- A barium swallow can be sensitive in identifying esophageal mass. Gastroesophagoscopy (endoscopy) confirms the diagnosis with tissue biopsy
- Overall the most common malignancy is 2ndary gastric fundal carcinoma invading distal esophagus
- Squamous cell is typically found in the mid esophagus, Adenocarcinoma in the distal region
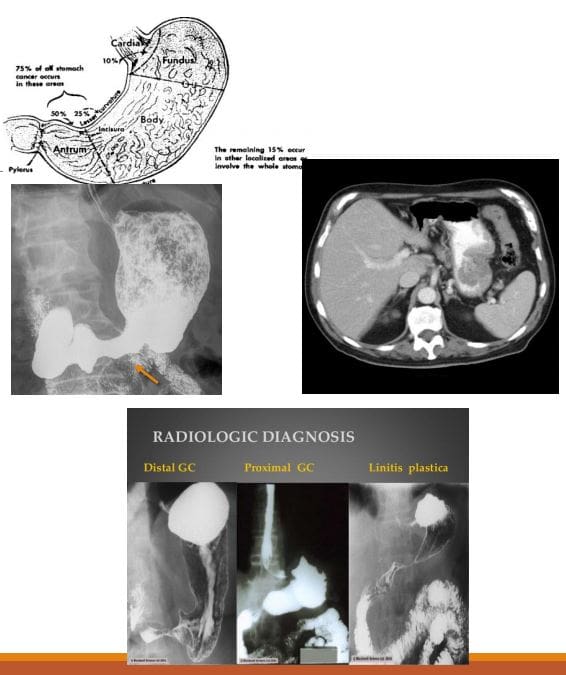
- Gastric carcinoma: primary malignancy of gastric epithelium. Rare before the age of 40. The median age at diagnosis in the United States is 70 years for males and 74 years for females. Japan, South Korea, Chile, and Eastern European countries have one of the highest rates of stomach cancer in the world. Stomach cancer rates are declining worldwide. Gastric cancer is the 5th causes of cancer-related death. Association with Helicobacter pylori infection 60- 80%, but only 2% population with H. Pyloris develop Stomach cancer. 8-10% have an inherited familial component.
- Gastric Lymphoma is also linked to H. Pyloris infection. Gastrointestinal Stromal Cell Tumour or GIST is another neoplasm affecting the stomach
- Clinically: No symptoms when it is superficial and potentially curable. Up to 50% of patients may have non-specific GI complaints. Patients may present with anorexia and weight loss (95%) as well as vague abdominal pain. Nausea, vomiting, and early satiety d/t obstruction may occur with bulky tumors or infiltrative lesions that impair stomach distension.
- Prognosis: Most gastric cancers diagnosed late and may reveal local invasion with regional adenopathy, liver, and mesenteric spread. A 5-year survival rate of 20% or less. In Japan and S. Korea, early screening programmes increased survival to 60%
- Imaging: Barium upper GI study, CT scanning. Endoscopic examination is the method of choice for the diagnosis. On imaging, Gastric cancer may appear as an exophytic (polypoid) mass or Fungative type, Ulcerative or Infiltrative/diffuse type (Linitis Plastica). CT scanning is important to evaluate local invasion (nodes, mesentery, liver, etc.)
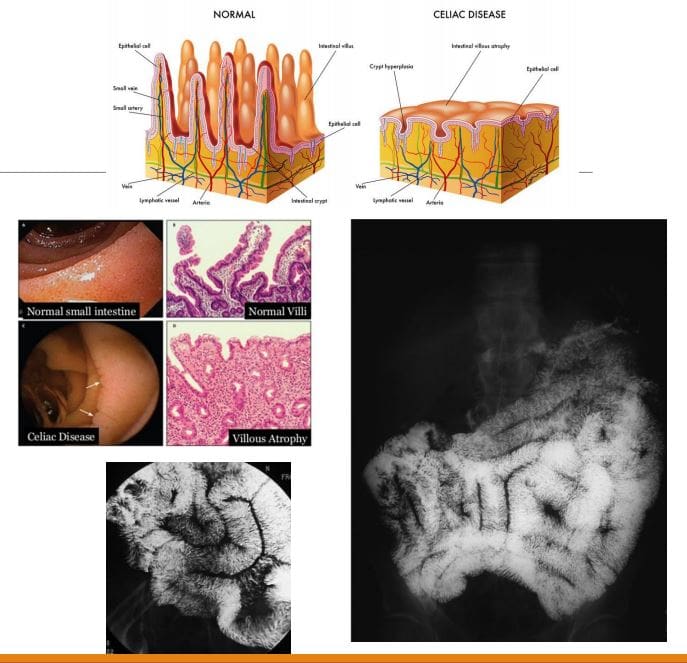
- Celiac disease aka non-tropical sprue aka Gluten-sensitive enteropathy: A T-cell mediated autoimmune chronic gluten-induced mucosal damage resulting in loss of villi in the proximal small bowel and gastrointestinal malabsorption (i.e., sprue). Considered in some cases of iron deficiency anemia of undetermined cause. Common in Caucasians (1 in 200) but rare in Asian and black individuals. Two peaks: a small cluster in early childhood. Typically in 3rd and 4th decades of life.
- Clinically: Abdominal pain is the m/c symptom, malabsorption of nutrients/vitamins: IDA and guaiac-positive stools, diarrhea, constipation, steatorrhea, weight loss, osteoporosis/osteomalacia, dermatitis herpetiformis. Increased association with T-cell lymphoma, Increased association with esophageal squamous cell carcinoma, SBO
- Dx: Upper GI endoscopy with multiple duodenal biopsies is considered a diagnostic standard for celiac disease. Histology reveals T-cell infiltration and lymphoplasmacytosis, Villi atrophy, Crypts hyperplasia, Submucosa, and Serosa are spared. Rx: elimination of gluten-containing products
- Imaging: Not required for Dx but on Barium swallow fluoroscopy: mucosal atrophy and obliteration of mucosal folds (advanced cases only). SB dilation is the most typical finding. Nodularity of the duodenum (bubbly duodenum). Reversal of jejunal and ileal mucosal folds:
- �The jejunum looks like ileum, the ileum looks like the jejunum, and the duodenum looks like hell.�
Inflammatory Bowel Disease: Crohn Disease (CD) & Ulcerative Colitis (UC)
- CD: chronic relapsing-remitting autoimmune inflammation that affects any part of the GI tract from the mouth to the anus but at onset most typically involves the terminal ileum. M/C presentation: abdominal pain/cramping and diarrhea. Path: granulomata formation that unlike UC is transmural, potentially leading to strictures. Areas affected by the inflammation are typically patchy
- Complications are numerous: malabsorption of nutrients/vitamins (anemia, osteoporosis, developmental delay in children, susceptibility to GI malignancy, bowel obstruction, fistula formation, extra-abdominal manifestations: uveitis, arthritis, AS, erythema nodosum and others. 10- 20% may require abdominal surgery after 10-years of CD usually for strictures, fistiluzation, BO.
- Dx: clinical, CBC, CMP, CRP, ESR, serological tests: DDx of IBD: anti-Saccharomyces cerevisiae antibodies (ASCA), perinuclear antineutrophil cytoplasmic antibody (p-ANCA) histologically or in serum. Fecal Calprotectin test helps to DDx IBS and evaluate response to treatment, disease activity/relapses.
- Dx of choice: endoscopy, ileoscopy, and multiple biopsies may reveal endoscopic and histological changes. Video capsule endoscopy (VCE), Imaging may help with Dx of complications. Rx: immunomodulatory drugs, complementary medicine, diet, probiotics, operative. No cure but the aim is to induce remission, control symptoms and prevent/treat complications
- Imaging Dx: KUB to DDx SBO, Barium enema (single and double contrast), small bowel follow through. Findings: skip lesions, aphthous/deep ulcerations, fistula/sinus tracts, String sign, creeping fat pushed loops of LB, cobblestone appearance d/t fissures/ulcers pushing mucosa, CT scanning with oral and IV contrast.
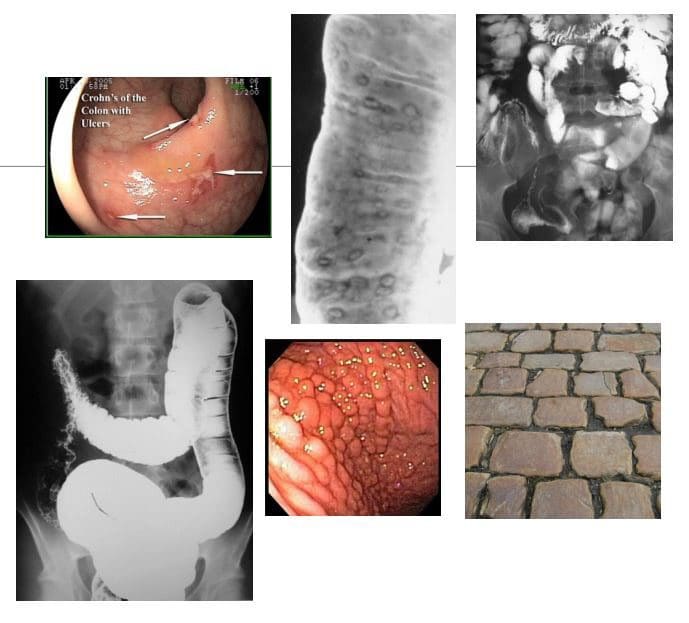
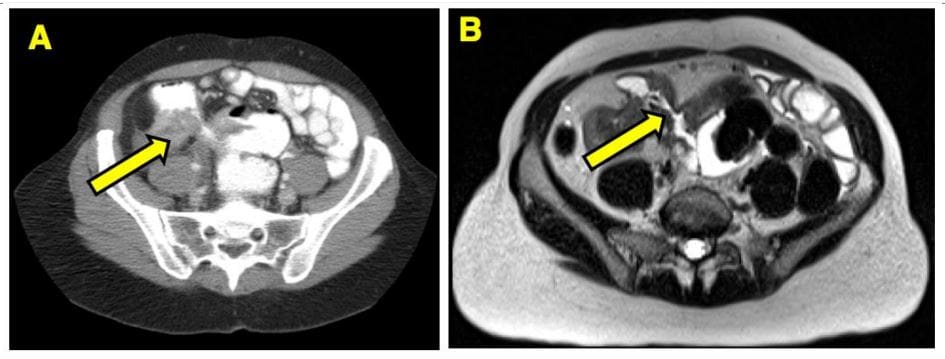
- Imaging from a Crohn’s patient who had a small bowel resection for obstruction.
- (A) CT scan shows non-specific inflammation whereas
- (B) MRE of the same area shows a fibrostenotic stricture
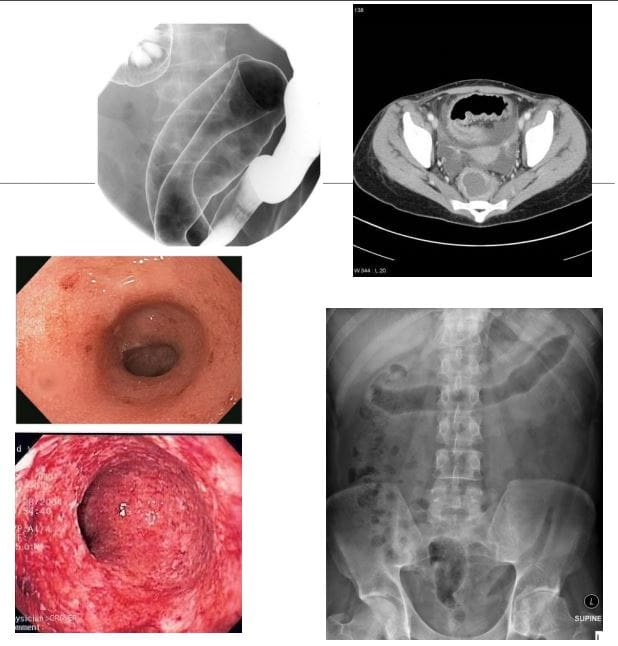
- UC: characteristically involves only the colon but backwash ileitis may develop. Onset is typically at 15-40s and is more prevalent in males, but the onset after the age of 50 is also common. More common in North America and Europe (hygiene hypothesis). Etiology: A combination of environmental, genetic and gut microbiome changes are involved. Smoking and early appendectomy tend to show a negative association with UC, unlike in CD considered some of the risk factors.
- Clinical Features: Rectal bleeding (common), diarrhea, rectal mucous discharge, tenesmus (occasionally), lower abdominal pain and severe dehydration from purulent rectal discharge (in severe cases, especially in the elderly), fulminant colitis and toxic megacolon can be fetal but are rare complications. Pathology: No granulomata. Ulcerations affect mucosa and submucosa. Pseudopolyps present as elevated spared mucosa.
- An initial process always affects the rectum and remain a local disease (proctitis) in (25%). 30% Proximal disease extension may occur. UC may present as left-sided (55%) and pancolitis (10%). Majority of cases are mild to moderate
- Dx: colonoscopy with ileoscopy with multiple biopsies confirm Dx. Labs: CBC, CRP, ESR, Fecal calprotectin, Complications: anemia, toxic megacolon, colon cancer, extra-colonic disease: arthritis, uveitis, AS, Pyoderma gangrenosum, Primary sclerosing cholangitis. Rx: 5-aminosalicylic acid oral or rectal topical therapy, corticosteroids, immunomodulatory drugs, colectomy is curative.
- Imaging: not required for Dx but barium enema may reveal ulcerations, thumbprinting, in advanced cases loss of haustra and narrowing of the colon producing �lead-pipe colon.� CT scanning may help with Dx seen as mucosal thickening detected only in moderate and severe cases. CT may help with of Dx of complications. Plain film image reveals �lead-pipe colon� and sacroiliitis as Enteropathic arthritis (AS)
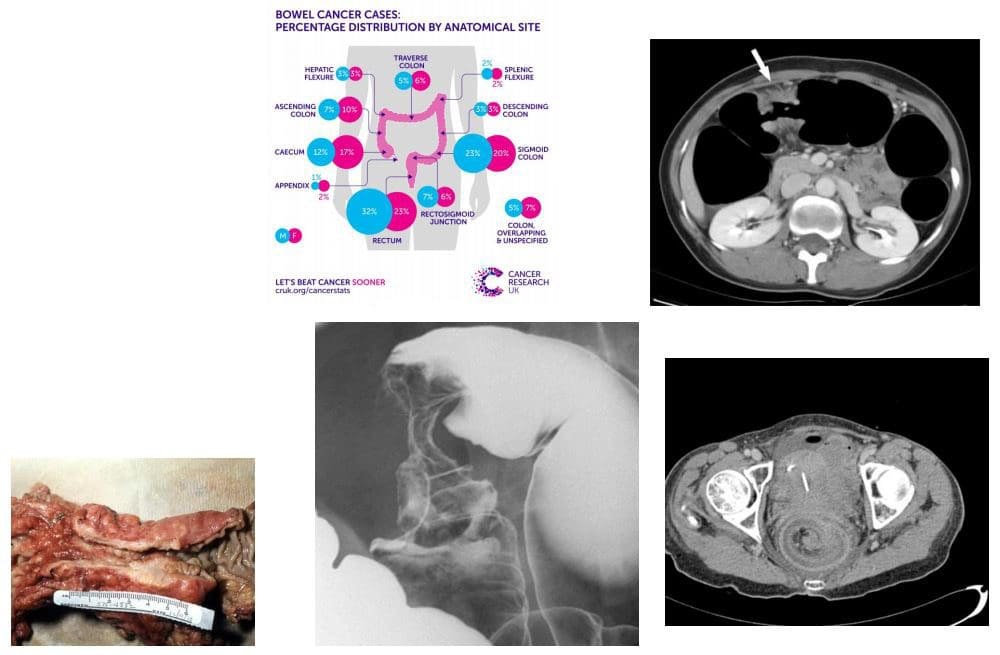
- Colorectal carcinoma (CRC) m/c cancer of the GI tract and the 2nd most frequent malignancy in adults. Dx: endoscopy and biopsy. CT is the modalities most frequently used for staging. Surgical resection may be curative although the five-year survival rate is 40- 50% depending on staging. Risk factors: low fiber and high fat and animal protein diet, obesity (especially in men), chronic ulcerative colitis. Colonic adenomas (polyps). Familial adenomatous polyposis syndromes (Gardener syndrome) and Lynch syndrome as non-familial polyposis.
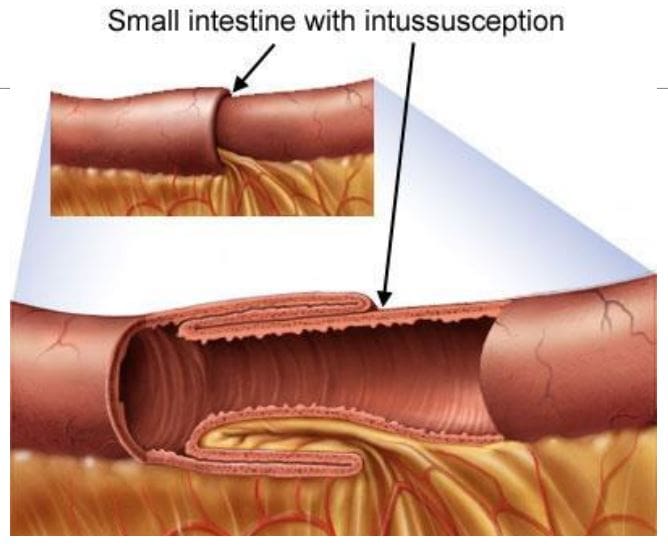
- Clinically: insidious onset with altered bowel habits, fresh blood or melena, iron deficiency anemia from chronic occult blood loss especially in the right-sided tumors. Bowel obstruction, intussusception, heavy bleeding and metastatic disease especially to the Liver may be initial presentation. Path: 98% are adenocarcinomas, arise from pre-existing colonic adenomas (neoplastic polyps) with malignant transformation. The five-year survival rate is 40-50%, with stage at operation the single most important factor affecting prognosis. M/C rectosigmoid tumors (55%),
- N.B. Some adenocarcinomas esp. mucinous types typically presented late and usually carry poor prognosis due to late presentation and mucin secretion and local/distant spread
- Imaging: Barium enema is sensitivities for polyps >1 cm, single contrast: 77-94%, double contrast: 82-98%. Colonoscopy is a modality of choice for prevention, detection, and identification of colorectal carcinoma. Contrast-enhanced CT scanning is used for staging and prognosis evaluation of mets.
- Screening: colonoscopy: men 50 y.o.-10-years if normal, 5-years if polypectomy, FOB, 1st degree relative with CA begin surveillance at 40 y.o
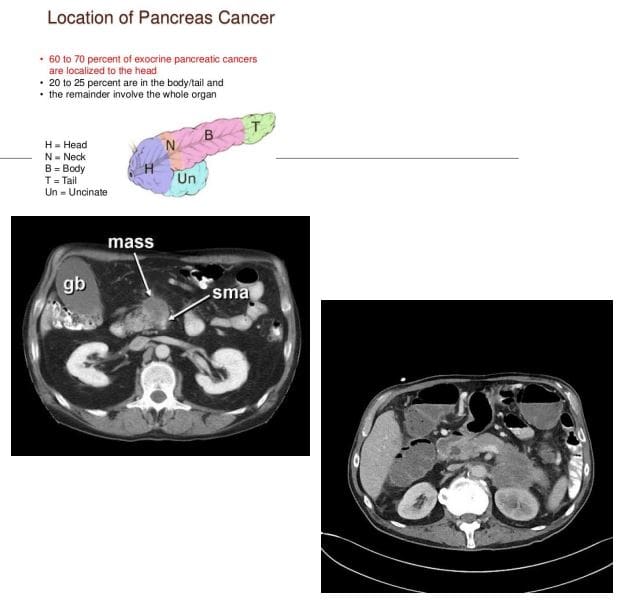
- Pancreatic Cancer: ductal epithelial adenocarcinoma (90%), very poor prognosis with high mortality. 3rd M/C abdominal cancer. Colon is #1, stomach #2. Pancreatic cancer accounts for 22% of all deaths due to gastrointestinal malignancy, and 5% of all cancer deaths. 80% of cases in 60+. Cigarette smoking is the strongest environmental risk factor, a diet rich in animal fats and protein. Obesity. Family history. M/C detected in the head and uncinate process.
- Dx: CT scanning is crucial. Invasion of Superior Mesenteric Artery (SMA) indicates unresectable disease. 90% of pancreatic adenocarcinomas are unresectable at Dx. Most patients die within 1-year of Dx. Clinically: painless jaundice, abd. Pain, Courvoisier�s gallbladder: painless jaundice and enlarged gallbladder, Trousseau�s syndrome: migratory thrombophlebitis, new onset diabetes mellitus, regional and distant metastasis.
- CT Dx: pancreatic mass with strong desmoplastic reaction, poor enhancement, and slightly lower attenuation compared to the adjacent normal gland, SMA invasion.
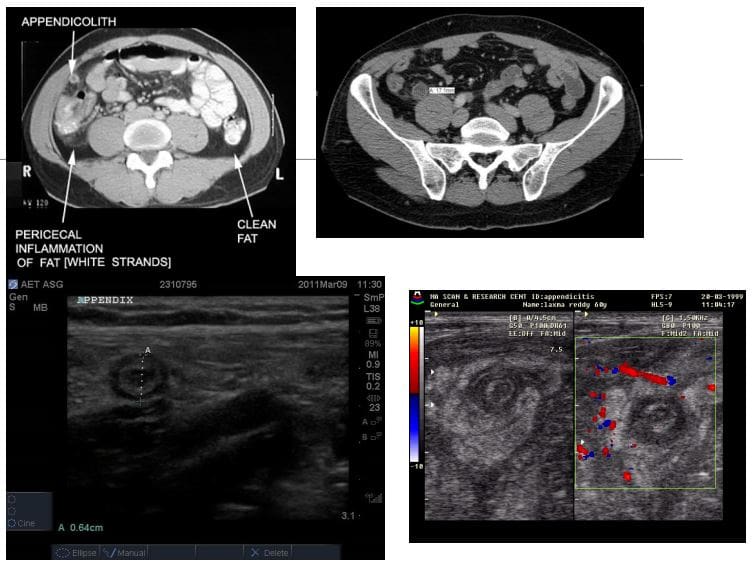
- Appendicitis: very common condition in general radiology practice and is a major cause of abdominal surgery in young patients
- CT is the most sensitive modality to detect appendicitis
- Ultrasound should be employed in younger patients and children
- KUB Radiographs should play no role in the diagnosis of appendicitis
- On imaging, appendicitis reveals inflamed appendix with wall thickening, enlargement, and periappendiceal fat stranding. Similar findings of wall thickening and enlargement are noted on US. Typical �target sign� is noted on short axis US probe position.
- If the appendix is retro-caecal than US may fail to provide accurate Dx and CT scanning may be required
- Rx: operative to avoid complications
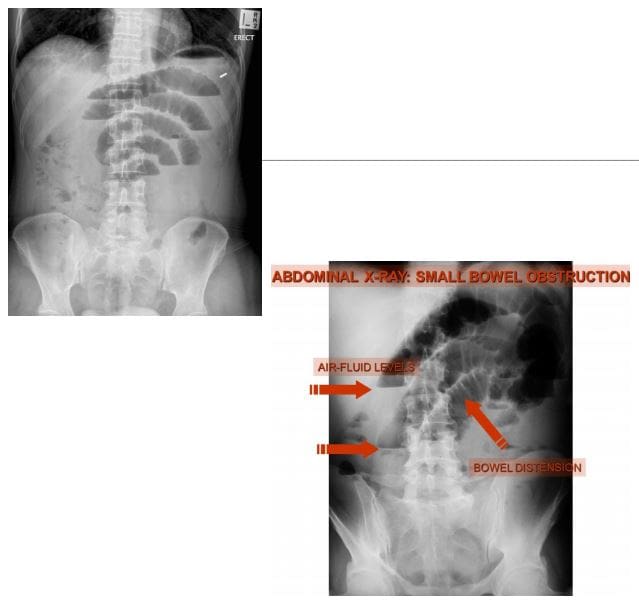
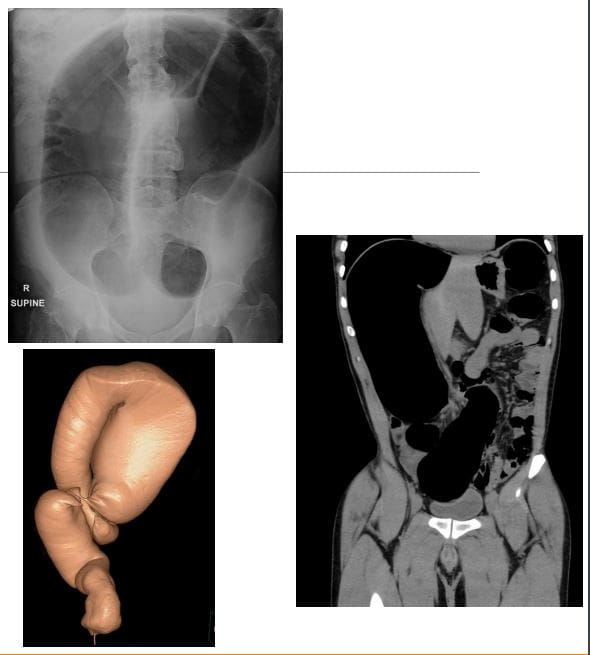
- Small bowel obstruction (SBO)-80% of all mechanical intestinal obstruction; the remaining 20% result from large bowel obstruction. It has a mortality rate of 5.5%
- M/C cause: any Hx of previous abdominal surgery and adhesions
- Classical presentation is constipation, increasing abdominal distension with nausea and vomiting
- Radiographs are only 50% sensitive for SBO
- CT will demonstrate the cause of SBO in 80% of cases
- There are variable criteria for maximal small bowel obstruction, but 3.5 cm is a conservative estimate of dilated bowel
- On Abd x-ray: supine vs. upright. Dilated bowel, stretched valvulae conivente (mucosal folds), alternative air-fluid levels �step ladder.� Absent gas in the rectum/colon
- Rx: operative as �acute abdomen.�
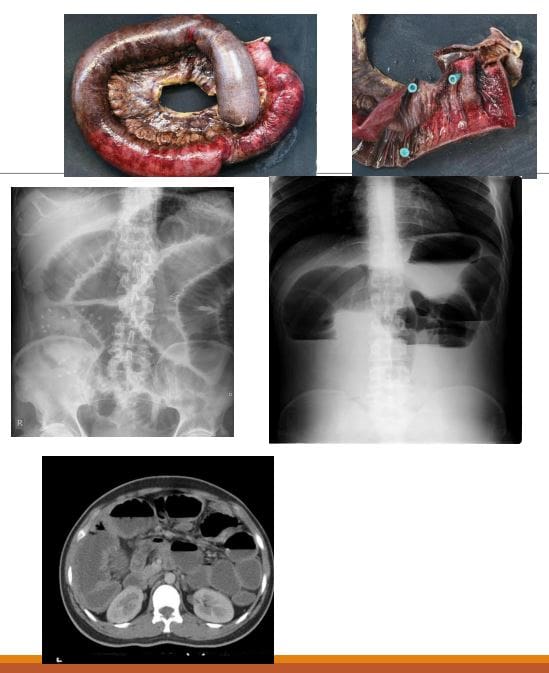
- Volvulus-m/c in the Sigmoid colon esp. in elderly. The main reason: chronic constipation with redundant sigmoid twisting on sigmoid mesocolon. Leads to Large bowel obstruction (LBO). Other common causes: a colon tumor. Sigmoid vs. Caecum volvulus
- Clinically: signs of LBO with constipation, abdominal bloating, pain, nausea, and vomiting. Onset may be acute or chronic
- Radiographically: loss of haustra in the LB, LB distension (>6-cm), �coffee bean sign� next slide, the lower end of volvulus points to the pelvis
- N.B: Rule of thumb for dilated bowel should be 3-6-9 where 3-cm SB, 6-cm LB & 9-cm Coecum
- Rx: operative as �acute abdomen.�
References
General Disclaimer, Licenses and Board Certifications *
Professional Scope of Practice *
The information herein on "The Abdomen: Diagnostic Imaging Approach | El Paso, TX." is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and on our family practice-based chiromed.com site, focusing on naturally restoring health for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez, DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card








