The autonomic concomitants of cervical pathomechanics?(the posterior cervical sympathetic syndrome) have been?widely reported. The literature documenting the autonomic? manifestations of thoracic and lumbar articular dysfunctions? has not been as extensive. The present study? attempts to determine the incidence and nosography of ?vertebrogenic autonomic dysfunction (V.A.D.) in a sample?of 250 consecutive back pain subjects. Thirty-nine per cent?of all back pain subjects exhibited probable evidence of ?V.A.D. The incidence of V.A.D. was distributed as follows:?cervicogenic cephalalgia – 60%76 (i.e., disturbed?vision, dysequilibrium, gastrointestinal upset); thoracalgia?- 54% (ie., nausea, flatus); and lumbalgia – 31% (i e.,?constipation, urinary frequency, menstrual disturbances).
It is a well known clinical fact that diseases of the internal? organs may produce functional changes and symptoms ?or signs in the musculoskeletal system of the body. These ?somatic manifestations of visceral disease are fairly commonplace ?and are considered to be of importance in the?diagnosis and localization of internal disease. All clinicians ?have observed the conspicuous costovertebral angle muscle?spasm resulting from acute renal disorders (1). Abdominal?wall tension and tenderness are characteristic of certain?intra-abdominal and intrapelvic diseases (2-7). Coronary? disease is frequently accompanied by painful trigger areas?in the muscles of the chest and shoulder (8-9).?The premise that disorders of the musculoskeletal?system may reflexly cause autonomic dysfunction and?symptoms attributable to visceral malfunction is common?to both the chiropractic (10) and osteopathic schools (11),?but is not widely accepted by the medical profession. Physiologic ?research, based primarily on animal experimentation,?has demonstrated that somatovisceral reflex activity?is indeed a physiologic fact (12-19); however, much remains?to be done to understand the importance of these?reflexes in normal and abnormal human physiology. The ?literature of the osteopathic and chiropractic disciplines?has historically contained an abundance of anecdotal and?conceptual data in support of the somatovisceral reflex?hypothesis as a mechanism for symptom production in?man. Very little controlled clinical data has been presented?to support this hypothesis.
Palmer in 1895 (20) was probably one of the first to?report a simple cause and effect relationship regarding? somatovisceral symptom production in a patient. His subject?had apparently been working in a cramped position?and felt something “give in his back.” He claimed that he?simultaneously became deaf. Palmer examined the?patient’s spine and found a “displaced fourth dorsal vertebra”?(sympathetic vasomotor nerves to the cranium) and?corrected it with a manipulation. The patient’s hearing?was restored. Palmer thus deduced that the hearing loss?had been vertebrogenic in origin.
Three decades later, the allopathic observers, Barre in?1925 and Lieou in 1928, reported similar series of cases in?which disorders of the cervical spine were accompanied by?dysfunction of the organs of the head (21,22). In addition?to hearing loss, the following cervicogenic symptoms have?been observed: vertigo, dysequilibrium, tinnitus, scotomata,?decreased vision, dysphagia, dysphonia, cough, anxiety?and asthenia. (23)
The Barr6-Lieou syndrome (posterior cervical sympathetic ?syndrome) has been repeatedly recorded in the literature?since 1928. This syndrome represents a generally?accepted classic example of somatovisceral reflex?pathology and is to be found in much of the authoritative?orthopaedic literature of today (24).
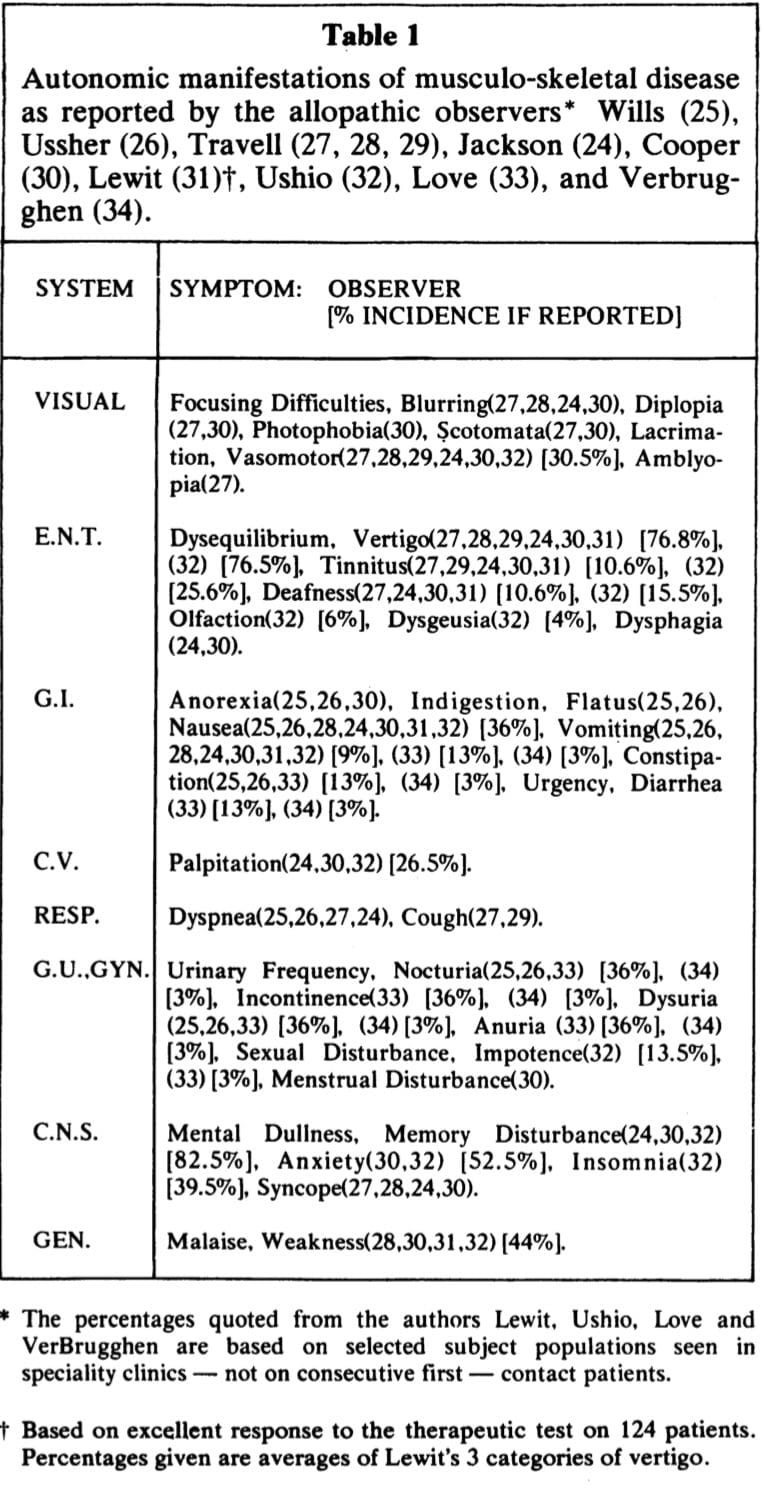
Reports of somatically-induced visceral dysfunction have? not been confined to the cervical region, nor have they?been restricted to the literature of the chiropractic and?osteopathic schools. This is noteworthy, insofar as allopathic?training does not usually emphasize (or even include)?studies of somatovisceral reflex physiology. One?would therefore expect that allopathic observers would?approach their clinical observations with an absence of?bias and a low index of suspicion for somatovisceral?pathology. Nevertheless, such disorders have been obvious?enough to be noted and reported. Table 1 summarizes allopathic?observations in this regard as reported by Wills?(25), Ussher (26), Travell (27,28,29), Jackson (24), Cooper?(30), Lewit (31), Ushio et al (32), Love (33) and Ver Brugghen?(34).
The literature cited here would tend to indicate that ?somatically induced visceral dysfunction and symptom?production is indeed a clinical problem. The prevalence of?the problem is not known. The investigators reviewed in ?Table 1 have for the most part, not attempted to discover?the percentile incidence of autonomic symptoms in musculoskeletal?disease, nor have they made it clear whether?their data was based on consecutive groups of first-contact?patients or on treatment-resistant subjects who were referred?to their departments for special care.
The purpose of this investigation was to determine the frequency of symptoms attributable to vertebrogenic autonomic dysfunction in a consecutive group of first-contact chiropractic patients.
Contents
Method
A pilot study, of the prospective-descriptive format, was designed. The focus of the study was on the anamnesis, with particular attention given to the sequence of clinical events. (For example, do patients with back pain simultaneously develop autonomic symptoms? If so, how often? 52 Do the autonomic symptoms disappear upon recovery from the spinal pain?) The emphasis then, was on seeking a parallelism between the development and disappearance of back pain with the development and disappearance of visceral symptoms.
Inclusion/Exclusion and Data Gathering:
The following guidelines for data gathering were adhered to throughout the study:
1. Two hundred and fifty consecutive first-contact patients who presented with back pain (cervical, thoracic or lumbar) comprised the sample for analysis.
2. After a thorough case-history was obtained from each subject, careful notation was made of associated symptoms. The phrasing of this latter aspect of the interview was as follows: “Have you, since the onset of your back pain, developed any other seemingly unrelated symptoms for example, have you felt generally ill? Have you been constipated? Have you had to empty your bladder more frequently – or less frequently?” Usually, four or five examples of known vertebrogenic symptoms were mentioned. See Table 1. A systems review followed. As additional symptoms were uncovered, it was determined whether or not their onset in any way paralleled the onset of back pain.
3. The patient was not given a r6sume prior to the beginning of treatment for his back pain. No further comment was made regarding the subject’s visceral symptoms, if present. No mention was made of any relationship between the spinal pain and the visceral symptoms. A chart of the autonomic nervous system was removed from the office. The patient was not told that analytical data was being gathered. The attempt here was to limit, as much as possible, the introduction of accentuated placebogenic and/or Hawthorne effects (35) into the study.
4. The subjects who were accepted as chiropractic patients were treated with spinal manipulative therapy (primarily chiropractic high velocity, controlled amplitude adjustment). In some cases, ancillary physical therapeutic methods were utilized as indicated. Patients who were referred to other health disciplines for care (i.e. surgery) remained in the study providing that follow-up data were available. (This study was not designed to test the effectiveness of manipulative therapy its sole purpose was to investigate spinovisceral symptom parallelism see illustrative case 4.)
5. The subjects were re-evaluated when they became asymptomatic with respect to their back pain or were much improved (at least 80%o by mutual patient-examiner agreement). The patients were at this time questioned regarding the status of any associated visceral symptoms that had been previously reported. The observation that recovery from visceral symptoms paralleled recovery from the spinal pain was taken to be confirmatory evidence of vertebrogenic autonomic dysfunction in that subject.
Subjects were excluded from the study for the following reasons: non-acceptance as a patient because of organic pathology or other contraindications, non-compliance, self-discharge from care, unsatisfactory recovery from the spinal complaint and incomplete admission or follow-up records. When a patient was dropped from the study, the next consecutive patient history was admitted to the data pool so that the target number of 250 subjects could be met.
A survey of drug usage by patients in this study revealed the following: 52% of patients did not use drugs at all; 32% has self-administered approximately 1 to 6 non-prescription analgesic tablets (i.e. aspirin, codeine) and had subsequently sought professional care; 16% were on regular therapeutic dosages of physician prescribed or self-administered pharmaceuticals either for spinal pain or for other unrelated conditions. Most of the subjects who had used pharmaceuticals remained in the study. They were included or excluded after careful analysis of the individual data (see data analysis guidelines).
Vertebrogenic Data Analysis:
The presence or absence of vertebrogenic autonomic dysfunction (V.A.D.) was determined from the admission and follow-up records on each subject. The likelihood of vertebrogenicity was determined on the strength of the gathered data. The information on each case was then categorized as yielding probable, possible or negative evidence of vertebrogenic autonomic dysfunction. The guidelines for categorization were as follows:
1. Probable: Patients who exhibited an unequivocal parallelism between the onset and abatement of back pain with the onset and abatement of visceral symptoms were considered to have evidence of probable vertebrogenic autonomic dysfunction.
2. Possible: If there was any doubt regarding the accuracy of the gathered data (e.g. inconsistency of the subject’s responses to questions) the findings were categorized as “possible V.A.D.” If any discrepancies were noted in spinovisceral symptom parallelism, the data was considered to yield evidence of possible vertebrogenic autonomic dysfunction. For example, patients who fully recovered from spinal pains, but were left with vestiges of autonomic symptoms or patients who recovered from autonomic symptoms but were left with some spinal pain, were placed in the V.A.D. possible category.
3. Negative: Subjects who developed back pain but did not experience any symptoms attributable to autonomic dysfunction were classified as “V.A.D. negative”.
As stated in the previous section, data from patients who had used pharmaceuticals were individually scrutinized for inclusion or exclusion, and categorization. This analytical process would best be illustrated by the following examples:
Case 1: This patient developed acute lumbalgia. He self-administered four 222 tablets� (total 32 mgs. codeine) on day 1 and presented here the next morning. He reported constipation as an associated symptom. The constipation resolved on day 3 although the lumbalgia continued. He remained in the study and was classified as “negative V.A.D.”
Case 2: This patient developed cervicalgia and self-administered 6 aspirin over day 1. She presented on day 2 and reported dizziness, gastric upset and flatus as associated symptoms. She discontinued her aspirin, but the autonomic symptoms persisted throughout the course of her treatment. All spinal and associated symptoms abated during the 3rd week. She remained in the study and was classified as “possible V.A.D.”
Case 3: This patient developed a severe cervical-brachial neuralgia. Her family physician prescribed Tylenol� and diazepam. She presented on day 10. She reported anorexia, nausea, flatus, blurred vision, dizziness and mental fogging as associated symptoms. On day 24 her cervicalgia and all associated symptoms had cleared, yet she remained on the prescribed medication. She was classified as “probable V.A.D.”
Results
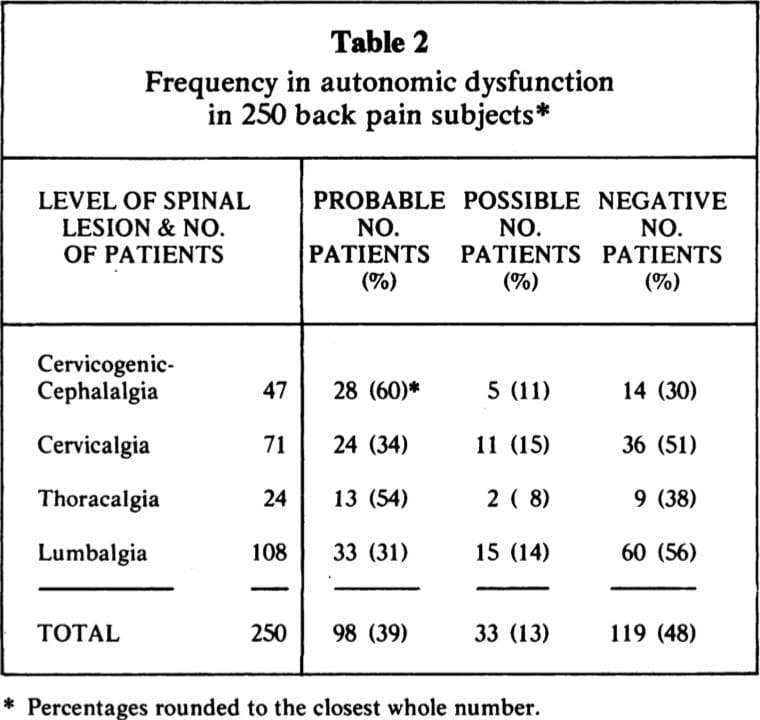
Of the original 250 subjects who met the criteria for admission to the study, 22 were subsequently lost (20 with self-discharges and/or poor results, 2 with organic disease found on continuing examination) and replaced by next consecutive patients. Ninety-eight (39%) of all subjects exhibited “probable” and thirty-three (13%) exhibited “possible” autonomic dysfunction. Also noteworthy was the observation that four (2%) of the subjects experienced reactivation (relapse) of previously quiescent visceral disease during their back pain episodes (2 duodenal ulcers, 2 lower genitourinary infections).
The levels of spinal complaint fell into the following four categories:
1. cervicalgia with cephalalgia,
2. cervicalgia (with or without upper extremity pain),
3. thoracalgia, and
4. lumbalgia (with or without lower extremity pain).
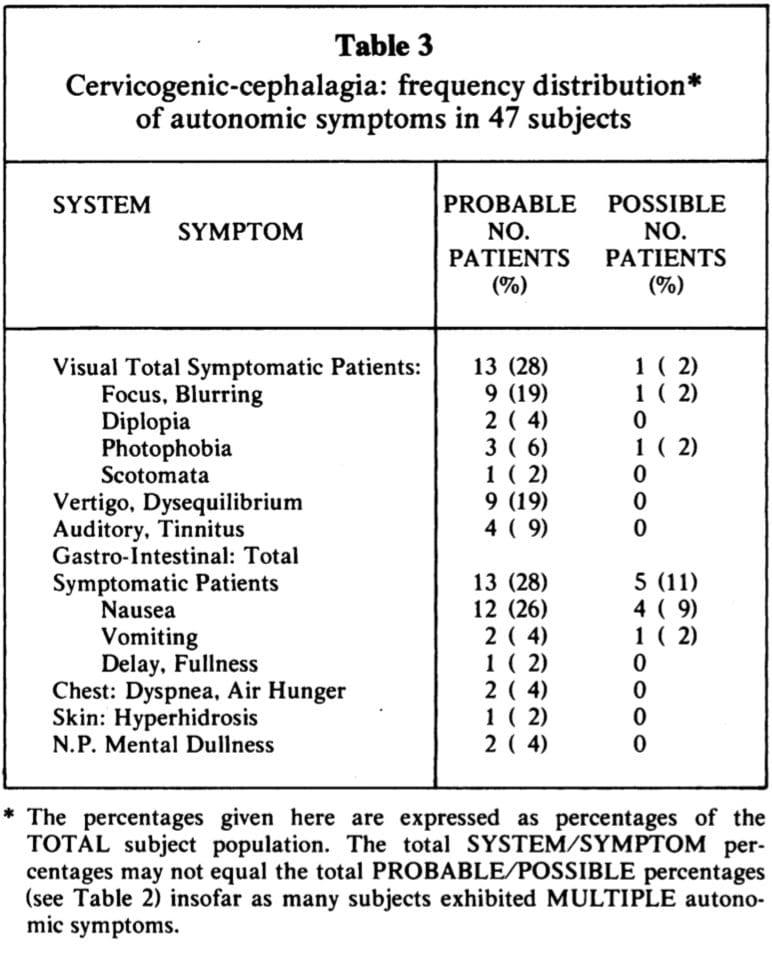
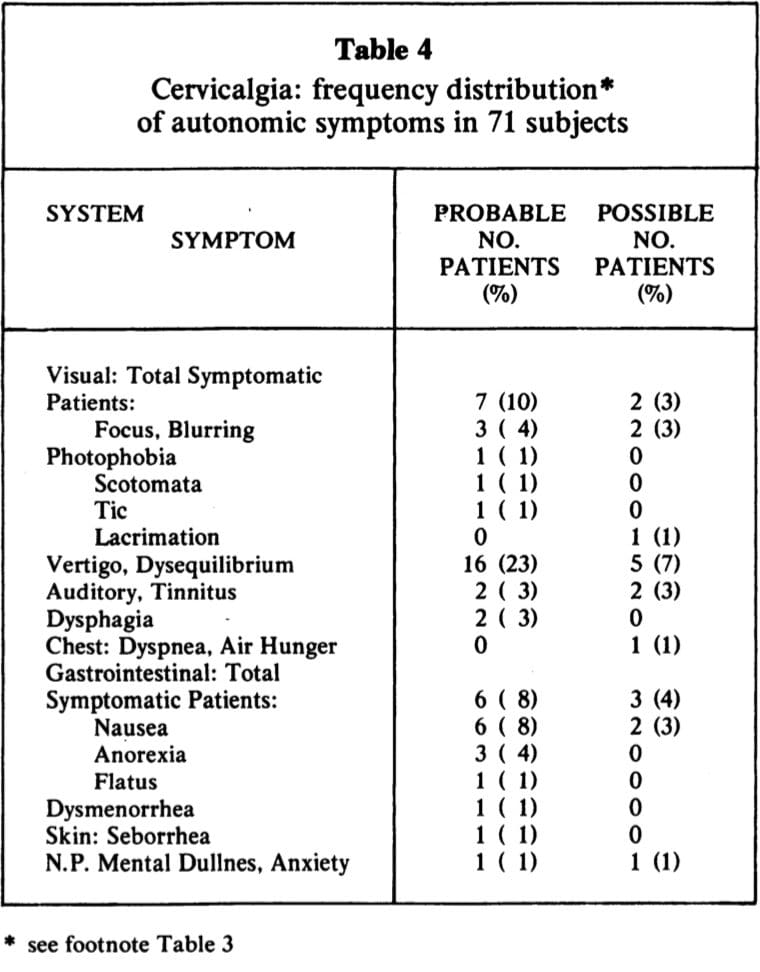
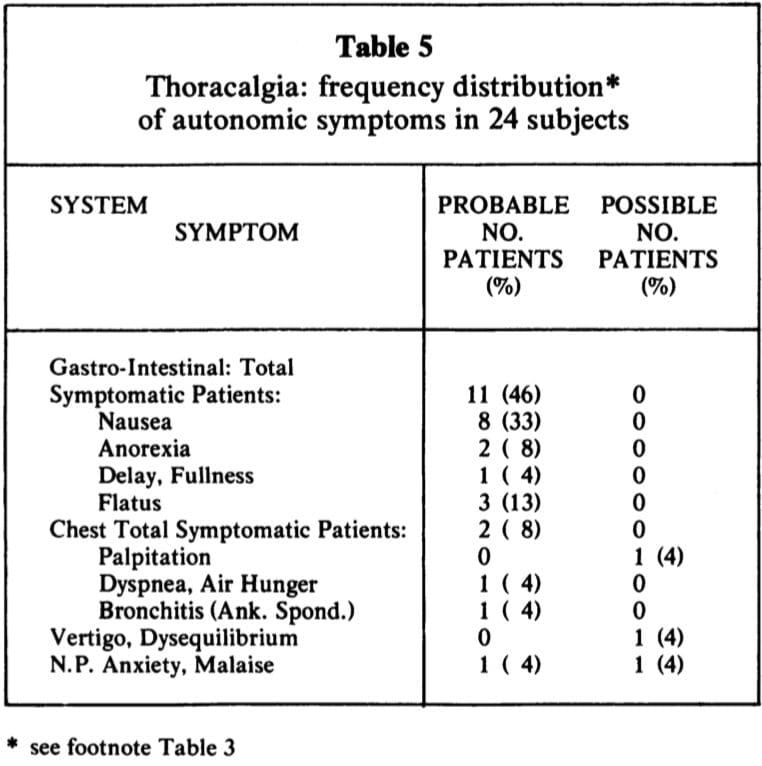
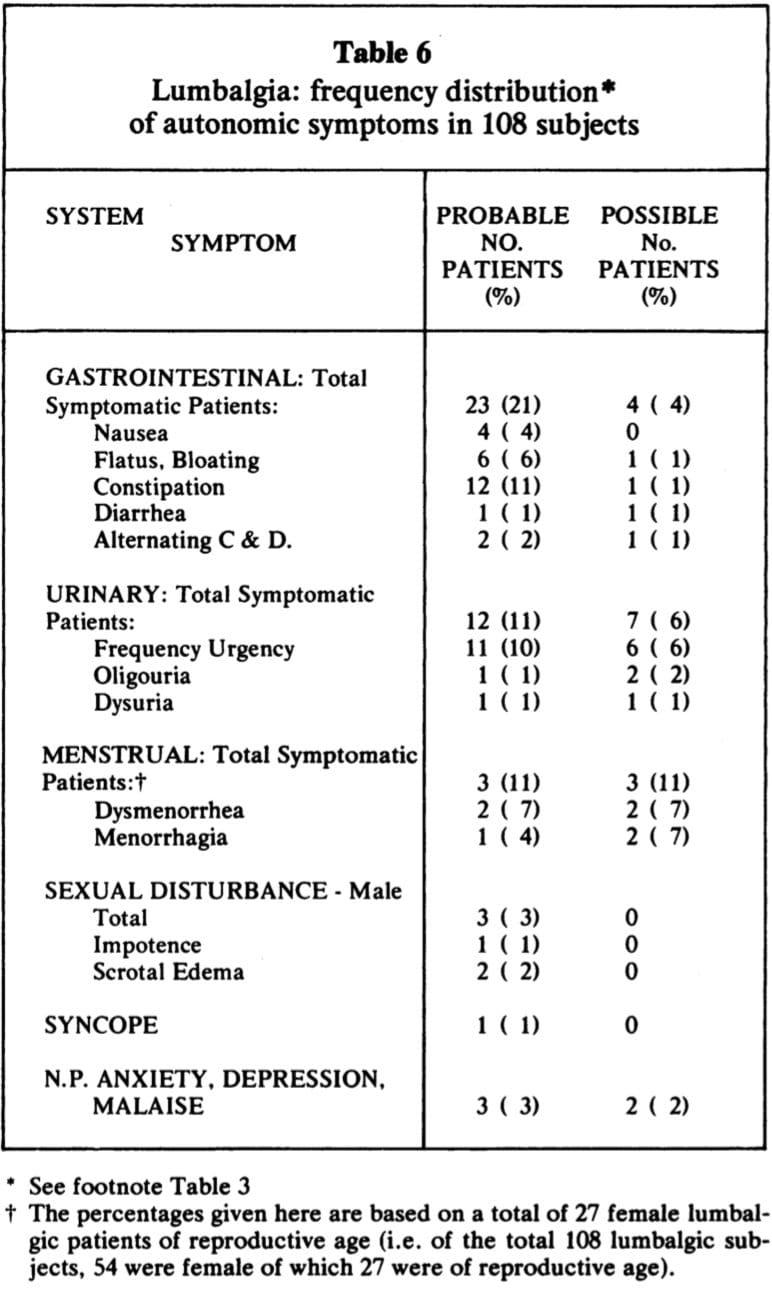
The frequency of autonomic dysfunction for each category is given in Table 2. The frequency distributions of the various autonomic manifestations observed are given in Tables 3 – 6.
While Tables 3 – 6 give the frequency of symptoms observed in the present study, they do not give an accurate picture of vertebrogenic autonomic dysfunction as actually seen in clinical practice. Many of the subjects had multiple autonomic symptoms and these symptom complexes are not accurately portrayed by tables. The following case studies are instructive:
Case 4: Mrs. F. presented with neck pain and headaches. She had sustained a whiplash injury 2 years previously and her symptoms had cleared with chiropractic therapy. Her present symptoms had recurred 2 months prior to her consultation here. She complained of a constant, moderate to severe upper cervical ache which radiated into the occipital-frontal regions. The cephalalgia occurred daily and intensified in the mid afternoon. She reported associated dizziness and difficulty in focusing her eyes. She could not clearly focus on close objects and stated that while driving, the windshield seemed to move back and forth in relation to her eyes. She was constantly squinting in an effort to see clearly. She had been seen by an optometrist 3 weeks previously with negative findings. On examination, cervical extension, right side-bending and left rotation were painful and limited. There was palpable paravertebral muscle spasm and restriction of motion in the upper cervical articulations. Trigger points were found here which reproduced the cephalalgia.
Cervicogenic autonomic dysfunction was objectivated with the following manoeuvres:
1. Triggers: Firm pressure over the right lamina of C2 precipitated an immediate bout of blurred vision and diplopia.
2. Resisted Motion: Resisted cervical extension (with the head fixed so as to exclude vestibular motion) resulted in an episode of “swooning” and vertigo.
3. Cervical Torsion: The patient’s head was fixed by an assistant (so as to exclude vestibular motion) and the torso was rotated, flexed, extended, side-bent and circumducted under the immobilized cranium. These maneuvers precipitated vertigo.
Cervicogenic autonomic dysfunction was further confirmed by the therapeutic test. The patient was treated with the manual adjustment of the upper cervical spine. The results were as follows:
1. The initial manipulation caused a transitory aggravation of the dizziness and the visual symptoms.
2.�This was quickly relieved by manual traction.
3.�The patient was fully recovered from all articular (pain) and non-articular (autonomic) symptoms by the tenth office visit. She remained asymptomatic over a 4 month follow-up period.
Case 5: Mrs. J. presented with low cervical, right scapular and right mid-thoracic pain of several months duration. There was associated dizziness, staggering and blurred vision. She had been referred to an ENT specialist who was non-commital in regards to a diagnosis. On examination, a trigger point was located on the antero-lateral aspect of C6-7 which reproduced her pain. The cervical torsion test was strongly positive the patient requiring support because of the precipitated vertigo. The lower cervical segments were adjusted and all symptoms abated after 5 visits. The patient has had several relapses over the ensuing months. Dysequilibrium has been a constant concomitant of each attack.
Case 6: Mr. R. Complained of a constant, dull mid-thoracic ache of 3 weeks duration. The symptoms had occurred after the patient spent several days working in the stooped forward position. The patient also complained of nausea and a feeling of a “lump” in the epigastric region. He stated that his food remained in his stomach for several hours after ingestion. He regurgitated frequently and was troubled with belching and flatus. He occasionally had crampy abdominal pains. On examination, the spinous processes and right costotransverse articulations of T4 to T7 were exquisitely tender. There was rhomboid. spasm on the right and mid-thoracic motion was�restricted. A single adjustment to this level was followed by immediate pain relief together with several minutes of massive gaseous eructation. All other symptoms cleared over the next few hours and did not recur over a 3 month follow-up period.
 Case 7: Mr. V. presented with acute lumbo-sciatica of one week’s duration. The pain had occurred after a straight-legged lift. Mr. V. reported that since the occurrence of his injury he had been troubled with alternating bouts of constipation and diarrhea, urinary frequency, nocturia, partial urinary retention, impotence and “retraction” of the testes. He exhibited sciatic kyphoscoliosis. All trunk movements were limited and painful. Straight-leg raising, foot dorsiflexion and Valsalva maneuvers were positive. Deep springing of the L4 vertebra aggravated his pain. Sphincter tone was normal. A trial of manipulation afforded only temporary (hours-days) relief. The left Achilles reflex became sluggish and the patient was referred for neurosurgery. An L4 discotomy resulted in complete recovery from all spinal and visceral symptoms.
Case 7: Mr. V. presented with acute lumbo-sciatica of one week’s duration. The pain had occurred after a straight-legged lift. Mr. V. reported that since the occurrence of his injury he had been troubled with alternating bouts of constipation and diarrhea, urinary frequency, nocturia, partial urinary retention, impotence and “retraction” of the testes. He exhibited sciatic kyphoscoliosis. All trunk movements were limited and painful. Straight-leg raising, foot dorsiflexion and Valsalva maneuvers were positive. Deep springing of the L4 vertebra aggravated his pain. Sphincter tone was normal. A trial of manipulation afforded only temporary (hours-days) relief. The left Achilles reflex became sluggish and the patient was referred for neurosurgery. An L4 discotomy resulted in complete recovery from all spinal and visceral symptoms.
Case 8: Mrs. R. presented with an acute lumbalgia which referred to the left groin. The pain had occurred 4 days previously and since that time she had been troubled with constipation, flatus, urinary frequency and a burning dysuria. Her urinalysis was negative for abnormality. Lower lumbar and left sacroiliac dysfunctions were corrected with manipulation. All symptoms had cleared by the fourth office visit.
At the time of discharge from care, Mrs. R. asked if her bowel and bladder symptoms could have anything to do with the lower back. She stated that every time she had a lower back episode she developed the same pelvic symptoms. She, had had several unremarkable bowel, gall bladder and urinary investigations in regards to these symptoms.
Discussion:�Vertebrogenic Autonomic Dysfunction
The exact mechanism of spinovisceral symptom production is not conclusively known. Several pathophysiologic hypotheses could be advanced to explain these clinical phenomena. It is also possible that different pathological processes are operant in different individuals. Postulated mechanisms of spinovisceral symptom production are summarized below:
Pain: The autonomic concomitants of severe pain are well known. They are due to mass sympathetic stimulation and include such symptoms as agitation, hyperhidrosis, pupillary dilation and vomiting.
Stress-Endocrine: Selye (36) has pointed out that many disease states are accompanied by two groups of symptoms – the symptoms produced by the stressor and another group of symptoms resulting from the body’s endocrinal defense responses to the stressor. Using the eosinophil count as a stress indicator, I presented evidence which would suggest that 54% of severe lumbalgic episodes are accompanied by an alarm-endocrine reaction (37). It is possible that some of the symptoms observed in this study have an endocrine-chemical basis.
Somato-Psycho-Visceral Reflexes: It is well known that certain patients look at their pains through a psychological magnifying glass and develop all manner of unrelated symptoms. Psychogenic symptom production, no doubt, introduces an artifact into this study. It is, however, very interesting to note that most of the symptoms observed here, bear a segmental relationship to the level of spinal lesion (only one patient in this series had any knowledge of the anatomy of the autonomic nervous system). These segmental spino-psycho-visceral relationships may be explained by osteopathic research. In a brilliant experiment, Korr et al have shown that when the psyche is stimulated, maximum sympathetic outflow occurs at hyperirritable cord levels which have been previously sensitized (facilitated) by proprioceptive input from preexisting spinal joint lesions (38).
Somato-Visceral Reflexes: Somato-autonomic reflexes in the laboratory animal are a physiologic fact. They are observed under certain conditions in man. The postulated modus operandi in spinal lesions is as follows: the lesioned spinal joints trigger an increased afferent input (pain, proprioception) into the related cord segments. The lateral horn cells are facilitated via the internuncial neurons and impulses spill over into the sympathetic efferents causing activation (motor, vasomotor, secretory) of the target 56 viscera. Such sustained pathophysiologic activity could well be responsible for spinovisceral symptoms observed in back pain subjects.
Nerve Compression: It is well known that discal lesions, vertebral exostoses and stenosis may compress nervous tissue and cause autonomic dysfunction or paresis. It is also possible that root compression may interfere with axoplasmic flow. If, for the purpose of survey, one considers paresthesia/anesthesia to be indicative of nerve-tissue compromise, then 30% of first-contact patients presenting at this office have nerve compression syndromes. This could be responsible for autonomic dysfunction in selected patients.
Vascular Compromise: Cervical degenerative lesions may compromise the vertebral arteries and cause cranial symptoms. This mechanism could have been operative in aged patients; however, the slowly progressive cerebral dysfunction (39), which allegedly occurs with sustained neck torsion in this condition, was not observed in any of the subjects.
Proprioceptive Cross-Talk: It is possible that unequal cervical muscle tensions might feed the central nervous system with confusing proprioceptive information so as to disturb normal righting reflexes. This mechanism could explain the high incidence of dysequilibrium in subjects with neck injuries.
Other: The constipation observed in severe lumbalgic patients may be antalgic or due to lack of exercise.
The spinovisceral syndromes described here are typical of the symptom complexes observed in the everyday clinical practices of all manipulative practitioners. Further studies, to more precisely explore these common clinical problems, are warranted. The present study represents a first-attempt prospective investigation and the presented statistics may be considered to be “ball-park” figures only. A much larger subject population is required. Analysis of the gathered data in a preliminary study such as this, almost invariably exposes deficiencies in the original prospective design which could be corrected to improve future investigations (40). The following recommendations should be considered:
Investigator Artifact: Solo investigators who study their own patient populations may be subject to impaired objectivity. Future studies should utilize a multi-disciplinary team of investigators to design and carry out the project.
Data Artifacts: All data gathering methods (verbal interviews and questionnaires) are subject to error (40,41). The interview method was used in the present study. Future studies should include both verbal interviews and written questionnaires to facilitate cross-checking of the accuracy of the gathered data.
Psychologic Artifacts: Clinical studies are frequently criticized for failing to establish psychological base-lines for the studied subjects. Written questionnaires could incorporate standard psychological testing proforma.
Pharmacologic Artifacts: Investigator judgement (bias) was used in categorizing data on drug users. Future studies should exclude these subjects, or at least analyze their data in a separate category.
Statistical Artifacts: A much larger study population is required in order to establish accurate prevalence rates for vertebrogenic autonomic dysfunction. Formal statistical analysis is also required.
Follow-Up: The foregoing study was designed to be an acute investigation of a common clinical syndrome. It asked simple, straight-forward questions regarding the sequence of events during back pain episodes. While many of the subjects were followed for months, and even years, it is debatable if long term follow-up would bring forth any additional answers to the questions asked. It is important to note, however, that historical chiropractic and osteopathic theory, in common with the psychosomatic school, hypothesizes that long standing functional disorders may eventually lead to organic pathology. Follow-up of patients with recurrent spinal lesions, over many years, might constitute one way of testing this hypothesis.
Conclusions:�Vertebrogenic Autonomic Dysfunction
The autonomic manifestations of back pain have been explored. This preliminary study indicates that 39%o of all back pain subjects have symptoms attributable to irritation of the- autonomic nervous system by spinal lesions. Further studies, which incorporate more rigid protocol, are required to accurately describe the nosographic features of these common clinical syndromes.
blank
References:
1. Guyton A. Textbook of medical physiology. Fifth edition. Philadelphia:
W B Saunders, 1976.
2. Brobeck JR. Physiologic basis ofLmedical practice. Tenth edition.
Baltimore: Williams and Wilkins, 1979.
3. Guyton A. Basis human physiology. Second edition. Philadelphia:
W B Saunders, 1977.
4. Beeson P, McDermott W. Textbook of medicine. Fourteenth edition.
Philadelphia: W B Saunders, 1975.
5. Cecil R, Loeb R. Textbook of medicine. Ninth edition. Philadelphia:.
W B Saunders, 1955.
6. Adams J. Outline of orthopaedics. Sixth edition. Edinburgh: Livingston,
1967.
7. Pottenger F. Symptoms of visceral disease. Seventh edition. St Louis:
CV Mosby, 1953.
8. Pinzler S, Travell J. Therapy directed at the somatic component of
cardiac pain. Am H J 1948; 35: 248-268.
9. Travell J, Pinzler S. The myofascial genesis of pain. Postgraduate
Medicine 1952; 11: 425-430.
10. Verner J. The science and logic of chiropractic. Englewood: J Verner,
1941.
11. MacDonald G, Hargrave-Wilson W. The osteopathic lesion. London:
Heinemann, 1935.
12. Sato A, Schmidt R. Somato sympathetic reflexes: afferent fibers,
central pathways, discharge characteristics. Physiological Reviews
1973; 53: 916-947.
13. Sato A, Sato Y, Shimada F, Torigata Y. Changes in vesical function
produced by cutaneous stimulation in rats. Brain Research 1975; 94:
465-474.
14. Sato A, Sato Y, Shimada F, Torigata Y. Changes in gastric motility
produced by nociceptive stimulation of the skin in rats. Brain Research
1975; 87: 151-159.
15. Sato A, Sato Y, Shimada F, Torigata Y. Varying changes in heart
rate produced by nociciptive stimulation of the skin in rats at different
temperatures. Brain Research 1976; 110: 301-311.
16. Haldeman S. Interactions between the somatic and visceral nervous
systems. JCCA 1971; 15(3): 20-25.
17. Sato A. The importance of somato-autonomic reflexes in the regulation
of visceral organ function. JCCA 1976; 20(4): 32-38.
18. Coote J. Somatic sources of afferent input as factors in aberrant
autonomic, sensory and motor function. In: Korr IM, ed. The neurobiologic
mechanisms in manipulative therapy. New York: Plenum
Press, 1978: 91-127.
19. Appenzeller 0. Somatoautonomic reflexology – normal and abnormal.
In:- Korr IM, ed. The neurobiologic mechanisms in nmanipulative
therapy. New York: Plenum Press, 1978: 179-217.
20. Palmer D. The science, art and philosophy of chiropractic. Portland:
Portland Printing House, 1910: 18.
21. Barre J. Rev Neurol 1926; 33: 1246
22. Lieou Y. Syndrome sympathique cervical posterieur et arthrite cervicale
chronique. These de Strasbourg, 1928. (Fre)
23. Gayral L, Neuwirth E. Oto-neuro-ophthalmologic manifestations of
cervical origin. NY State J Med 1954; 54: 1920-1926.
24. Jackson R. The cervical syndrome. Springfield: Charles C Thomas,
1966: l31-144.
25. Wills 1, Atsatt R. The viscerospinal syndrome: a confusing factor in
surgical diagnosis. Arch Surg 1934; 29: 661-668.
26. Ussher N. The viscerospinal syndrome – a new concept of visceromotor
and sensory changes in relation to deranged spinal structures.
Ann Int Med 1940; 13(2): 2057-2090.
27. Travell J, Bigelow N. Role of somatic trigger areas in the patterns of
hysteria. Psychsom Med 1947; 2: 353-363.
28. Travell J. Referred pain from skeletal muscle. NY State J Med; 1955
Feb: 331-340.
29. Travell J. Mechanical headache. Headache 1967 Feb: 23-29.
30. Cooper A. Trigger-point injection: its place in physical medicine.
Arch Phys Med Rehab 1961; 704-709.
31. Lewit K. Menieres disease and the cervical spine. Rev Czechoslovak
Med 1961; 7(2): 129-139.
32. Ushio N, Hinoki M, Hine S, Okada S, Ishida Y, Koike S, Shizuba S.
Studies on ataxia of lumbar origin in cases of vertigo due to whiplash
injury. Agressologie 1973; 14(D): 73-82.
33. Love J, Schorn V. Thoracic disc protrusions. JAMA 1%5;
43-62.
34. Ver Brugghen A. Massive extrusions of lumbar intervertebral discs.
Surg Gynecol Obstet 1945; 81: 269.
35. Treece E, Treece J. Elements of research in nursing. First edition.
Saint Louis: CV Mosby, 1973.
36. Selye H. The stress of life. New York: McGraw-Hill, 1956.
37. Johnston R. Vertebrogenic stress eosinopenia. JCCA 1974; 18(4):
14-20.
38. Korr l, Thomas P, Wright R. Symposium on the functional implications
of segmental faciliation. JAOA 1955; 54: 173.
39. Houle J. Assessing hemodynamics of the vertebro-basilar complex
through angiothlipsis. JCCA 1972 June: 35-36, 41.
40. Friedman G. Primer of epidemiology. First edition. New York:
McGraw-Hill, 1974.
41. Koran L. The reliability of clinical- methods, data and judgments.
New Engl J Med 1975; 293: 642-646.
Close Accordion
Professional Scope of Practice *
The information herein on "Vertebrogenic Autonomic Dysfunction Subjective Symptoms: A Prospective Study" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Our information scope is limited to Chiropractic, musculoskeletal, physical medicines, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somatovisceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and/or functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez, DC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, RN*, CCST, IFMCP*, CIFM*, ATN*
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807, New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Florida
Florida License RN License # RN9617241 (Control No. 3558029)
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Dr. Alex Jimenez DC, MSACP, RN* CIFM*, IFMCP*, ATN*, CCST
My Digital Business Card






