Common Clinical Neuropathies in El Paso, TX
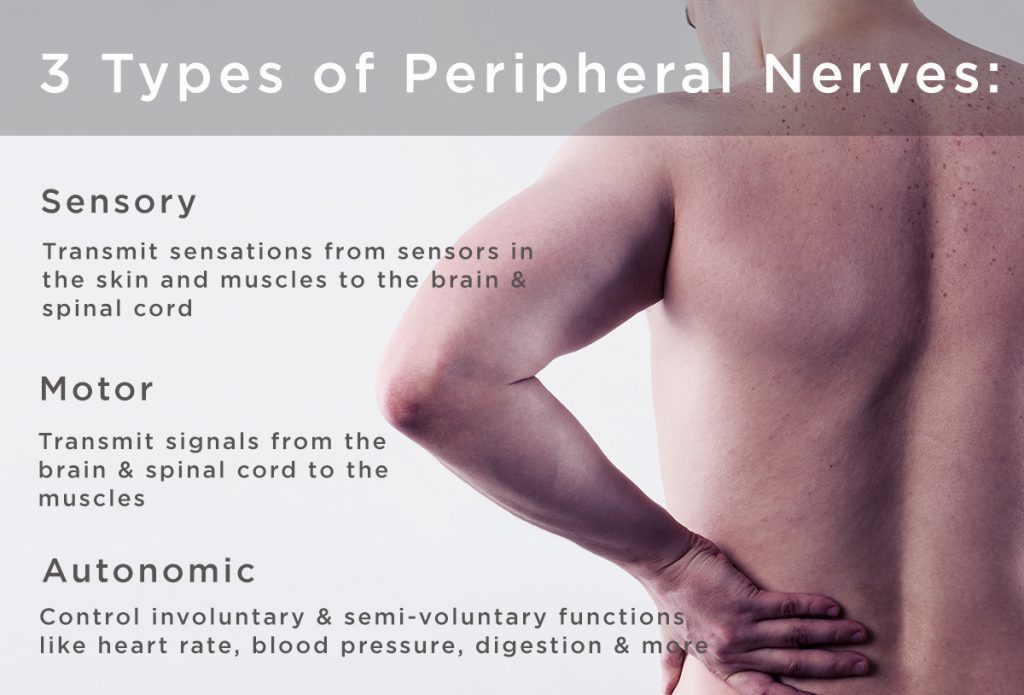
Neuropathy is a medical term used to describe a collection of general diseases or malfunctions which affect the nerves. The causes of neuropathy, or nerve damage, can vary greatly among each individual and these may be caused by a number of different diseases, injuries, infections and even vitamin deficiency states. However, neuropathy can most commonly affect the nerves that control the motor and sensory nerves. Because the human body is composed of many different kinds of nerves which perform different functions, nerve damage is classified into several types. Neuropathy can also be classified according to the location of the nerves being affected and according to the disease causing it. For instance, neuropathy caused by diabetes is called diabetic neuropathy. Furthermore, depending on which nerves are affected will depend on the symptoms that will manifest as a result. Below we will discuss several specific types of neuropathies clinically treated by chiropractors, physical therapists and physical medicine doctors alike, as well as briefly describing their causes and their symptoms.
Brachial Plexopathies
Brachial plexopathy is a type of peripheral neuropathy, which affects the nerves that transmit messages from the brain and the spinal cord to the rest of the body. This kind of nerve damage occurs when harm affects the brachial plexus, a region found on each side of the neck where nerve roots from the spinal cord branch out into each arm’s nerves. Damage, injury or a condition that impacts these nerve roots can result in pain, decreased mobility and reduced sensation in the arm and shoulder. In some cases, no cause can be identified.
Erb’s Palsy
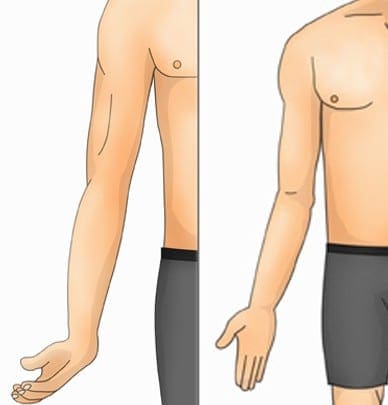
Erb’s Palsy, also known as�Erb�Duchenne palsy or Waiter’s tip palsy, is identified as a paralysis of the arm caused by damage or injury to the nerves in the neck which form part of the brachial plexus. The most common mechanism of injury in adults with Erb’s Palsy is a patient who fell forward while holding onto something behind them. Erb�Duchenne palsy can also happen to an infant during childbirth, most commonly, but not exclusively, from shoulder dystocia during a difficult birth. To be more precise, this type of brachial plexopathy results from damage to the C5-C6 nerve roots along the brachial plexus in the neck. Symptoms of Erb’s Palsy include dermatomal distribution of sensory disruption followed by weakness or paralysis in the deltoid, biceps, and brachialis muscles, leading to the �waiter�s tip� position associated with this type of neuropathy. While many infants can recover on their own from this type of brachial plexopathy, some may require rehabilitation.
Klumpke’s Palsy
Klumpke’s Palsy, also known as Klumpke’s paralysis or�Dejerine�Klumpke palsy, is a partial palsy in the nerve roots of the brachial plexus located along the cervical spine, or neck. It is named after�Augusta D�jerine-Klumpke, an American-born French medical doctor acknowledged for her work in neuroanatomy. Klumpke’s Palsy is characterized as a form of paralysis involving the muscles of the forearm and hand, which occurs to�infants during childbirth if their arm is pulled overhead.�Dejerine�Klumpke palsy can also occur to adults with overhead traction injuries caused by harm to the C8-T1 nerve roots in the brachial plexus and upper thoracic region of the spine. Symptoms of Klumpke’s paralysis include dermatomal distribution of sensory disruption, weakness or paralysis, in the wrist flexors and pronators as well as in the muscles of the hand. This type of brachial plexopathy may often lead to Horner�s syndrome, a collection of symptoms which manifest when a set of nerves, known as the sympathetic trunk, are damaged or injured due to T1 involvement. This form of neuropathy is identified by resulting�in a �claw hand� appearance, where the forearm is supinated with the wrist hyperextended, together with finger flexion.
Entrapment Neuropathies
Entrapment neuropathy, also known as nerve compression syndrome or compression neuropathy, is best-known as nerve damage or a type of neuropathy caused by direct pressure on a nerve. Common symptoms include pain and discomfort, tingling or burning sensations, numbness and muscle weakness which affects only a particular part of the human body, depending on which nerve is affected. A nerve can become compressed as a result of a constant external force or due to a lesion, such as a tumor. Additionally, some conditions can make the nerves more susceptible to compression, including diabetes, where the nerves are rendered more sensitive to minor degrees of compression due to their already compromised supply of blood. Nerve damage caused by a single episode of harm can be considered an entrapment neuropathy, however, it is generally not classified under this group of compression neuropathy or nerve compression syndrome.
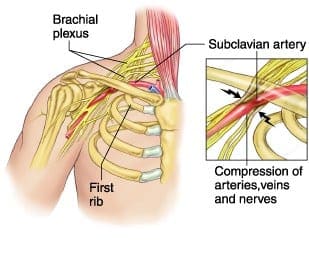
Thoracic Outlet Syndromes
Thoracic outlet syndromes are a group of disorders which develop when the nerves or blood vessels between the collarbone and the thoracic outlet, located in the region of the first rib, are compressed. As a result, this can cause pain and discomfort in the neck and shoulders as well as numbness in the fingers. There are a number of types of thoracic outlet syndromes, including neurogenic, or neurological, thoracic outlet syndrome, specifically caused by the compression of the brachial plexus, vascular thoracic outlet syndrome, which is caused specifically by the compression of the veins, known as venous thoracic outlet syndrome, or arteries, known as arterial thoracic outlet syndrome, and nonspecific-type thoracic outlet syndrome, which is considered to be idiopathic and has been described to worsen with activity. Several healthcare professionals believe that nonspecific-type thoracic outlet syndrome doesn’t exist, while others claim it to be a common disorders. However, the majority of thoracic outlet syndromes are often classified as neurogenic.
Thoracic outlet syndromes are caused by the compression of the cervical rib, an extra “rib” in the seventh cervical vertebra, subclavius muscle tension, improper posture or�excessive thoracic kyphosis, physical trauma, repetitive activity, obesity and pregnancy. Thoracic outlet syndromes can vary depending on which structures are compressed. Thoracic outlet syndromes can be diagnosed using tests, such as the Adsons test, the Allen maneuver, the Costoclavicular maneuver, the Halstead maneuver, the�Reverse bakody maneuver, the Roos test, the Shoulder compression test and the Wright test. Thoracic outlet syndromes can cause permanent neurological damage if not diagnosed and treated early.
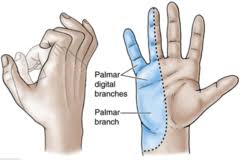
Median Nerve Entrapment
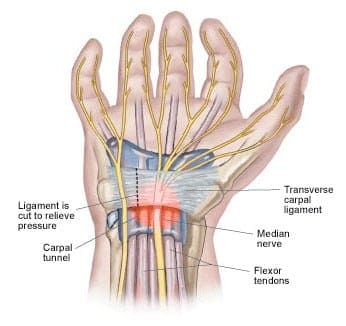
Median nerve entrapment or median nerve entrapment syndrome, is a mononeuropathy, a condition that impacts only a single nerve or nerve group outside the brain and spinal cord, which affects the movement of or sensation in the hand. Median nerve entrapment is caused by the compression of the median nerve found in the elbow or distally in the forearm or wrist. Symptoms include sensory disruption in the lateral portion of the palmar aspect of the hand and dorsal finger tips of the same fingers. In addition, motor fibers may also be affected in the forearm, if applicable, including the muscles of the thenar eminence, such as the abductor pollicis brevis, the opponens pollicis, and the flexor pollicis brevis. Other forms of median nerve entrapment syndromes include: pronator teres syndrome and carpal tunnel syndrome.
Pronator teres syndrome is characterized as the compression of the median nerve at the elbow. It is considered rare compared to carpal tunnel syndrome. Pronator teres syndrome is caused by repetitive movement, pronator teres muscle inflammation and thickened bicipital aponeurosis. Clinical findings for this type of neuropathy include, tenderness with palpation of the pronator teres muscle, pain with resisted pronation of the arm, flexor pollicus longus and flexor digitorum profundus involvement, otherwise, symptoms manifestations for pronator teres syndrome may appear similar to carpal tunnel syndrome but without positive wrist orthopedics.
Carpal tunnel syndrome is characterized as the compression of the median nerve at the wrist. Carpal tunnel syndrome is identified by symptoms of pain and discomfort, tingling sensations in the thumb, index finger, middle finger and the thumb side of the ring fingers, and numbness. These can generally start gradually and may extend up the arm. Advanced instances of carpal tunnel syndrome may cause weakened grip strength where the muscles at the base of the thumb may waste away if left untreated for an extended period of time. In many cases, carpal tunnel syndrome may affect both hands or arms. Carpal tunnel syndrome is caused by repetitive movements, hypothyroidism, obesity, rheumatoid arthritis, diabetes and pregnancy. Orthopedic tests utilized to diagnose carpal tunnel syndrome include the use of the Tinel�s Sign, positive if tapping over the median nerve reproduces/exacerbates symptoms, the�Phalen�s Maneuver/Prayer Sign, performed by bringing the hands together, with wrists flexed, and is repeated in reverse with the wrists extended, for at least 60 seconds, and is considered positive if tests reproduce/exacerbate symptoms, and the�Wringing Test, if wringing a towel produces paresthesia.
Ulnar Nerve Entrapment
Ulnar nerve entrapment is a condition where the ulnar nerve itself becomes physically trapped or pinched, resulting in symptoms of pain, numbness and weakness which extends throughout the little finger, the ulnar half of the ring finger and throughout the intrinsic muscles of the hand. Symptoms or ulnar nerve entrapment ultimately involve sensory disruption in the medial two digits of the palmar and dorsal aspects of the hand. Symptoms of ulnar nerve entrapment may vary depending on the specific location of the ulnar nerve compression or impingement. These may also be classified as motor, sensory or both, depending on the location of the injury. If motor fibers are affected in the hand, all fingers, besides the thumb, may become weakened, described as general hand weakness. The most common location of ulnar nerve entrapment is within the cubital tunnel. Other forms of ulnar nerve entrapment include: cubital tunnel syndrome and tunnel of Guyon syndrome.
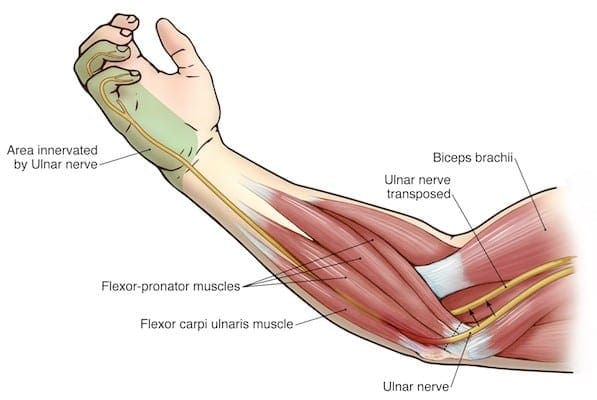
Cubital tunnel syndrome is identified by the compression or impingement of the ulnar nerve in the cubital tunnel at the elbow. It is considered to be the second most common entrapment neuropathy which affects the upper extremities, following carpal tunnel syndrome. Symptoms of cubital tunnel syndrome are characterized by pain and discomfort along the region of the ulnar nerve entrapment, along with sensory impairment, paresis and paresthesia.�Causes of cubital tunnel syndrome include, repetitive movements, hypothyroidism, obesity, diabetes, physical trauma or injury to the cubital tunnel, and prolonged sitting with pressure on bent elbow.
Tunnel of Guyon syndrome, or Guyon’s canal syndrome, is identified by the compression or impingement of the ulnar nerve at the wrist, particularly along an anatomical space in the wrist known as Guyon’s canal. Guyon’s canal syndrome may also be referred to as ulnar tunnel syndrome. Symptoms of tunnel of Guyon syndrome are similar to those of cubital tunnel syndrome with slight variations depending on the region of ulnar nerve entrapment.�Causes of tunnel of Guyon syndrome include, repetitive movements, long term crutch use, fracture of the hamate, a carpal bone, due to a ganglion cyst, hypothyroidism, obesity, rheumatoid arthritis and diabetes.�Orthopedic tests utilized to diagnose Guyon’s canal syndrome include the use of the�Tinel�s Sign, positive if test over the ulnar nerve at the wrist elicits symptoms, the Wartenberg Sign, positive if the 5th digit abducts when patient performs hard grip strength test or attempts to squeeze fingers together and reduced two-point discrimination in the hand.
Radial Nerve Entrapment
Radial nerve entrapment, also known as radial tunnel syndrome, is a condition caused by the compression of the radial nerve, which travels from the brachial plexus, to the hand and wrist. Healthcare professionals believe that radial tunnel syndrome occurs because the radial nerve becomes irritated or inflamed due to the friction caused by the impingement of the muscles in the forearm. Radial nerve entrapment manifests symptoms of sensory disruption in the lateral three and a half digits of the dorsal aspect of the hand. Motor�fibers may also be affected along the�posterior arm and extensor compartment of the forearm, and wrist drop may be seen. Other forms of radial tunnel syndrome include: spiral groove entrapment, where all radial nerve innervated muscles below entrapment are affected,�Saturday night palsy caused due to sleeping on your own arm and the brachioradialis & triceps reflexes are both diminished, supinator syndrome, caused by the compression at the arcade of Frohse with no change in reflexes. Posterior interosseous syndrome, or radial tunnel syndrome, also elicits no change in reflexes.
Sciatic Nerve Entrapment
Sciatic nerve entrapment is a condition caused by the compression of the sciatic nerve, the longest and largest nerve in the human body, which travels from the low back, down through the buttocks, thighs, legs and into the foot. The collection of symptoms which manifest as a result of sciatic nerve entrapment, including pain and discomfort, tingling and burning sensations, and numbness as well as weakness in the lower extremitites, is commonly known as sciatica. Sciatic nerve entrapment, or sciatica, can be caused by a variety of injuries and/or aggravated conditions which can lead to the compression of the sciatic nerve, including, but not limited to, disc herniation and spinal stenosis. However, symptoms of sciatic nerve entrapment may vary depending on the location of the compression of the sciatic nerve. Other conditions caused by the compression of the sciatic nerve include: piriformis syndrome, peroneal nerve entrapment and tarsal tunnel syndrome.
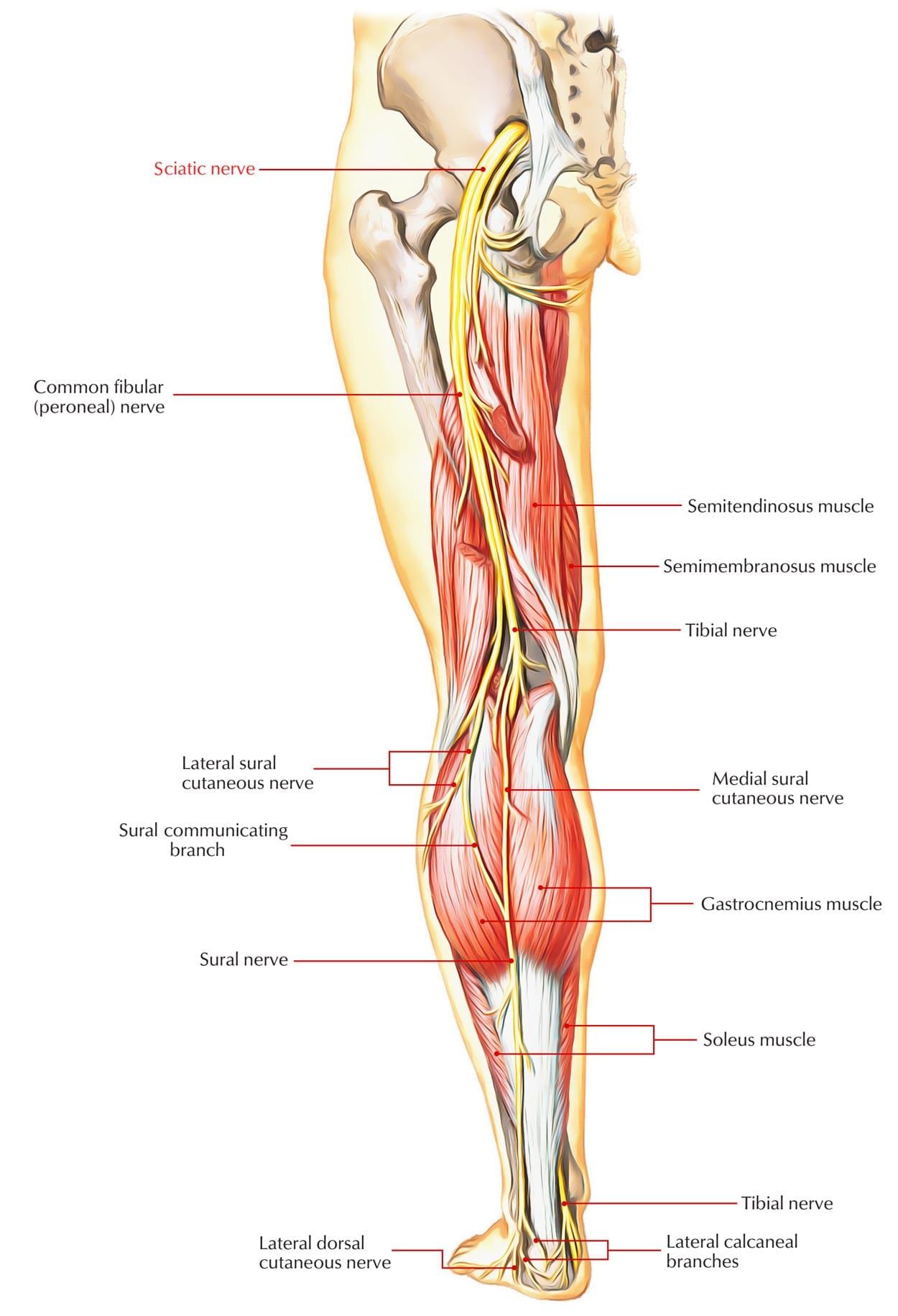
Piriformis syndrome is a condition which occurs due to the compression of the sciatic nerve as a result of the irritation or inflammation of the piriformis muscle. Symptoms of piriformis syndrome may include pain and discomfort, followed by numbness in the buttocks and down the leg. Symptoms may worsen with regular activities, such as sitting and running. Piriformis syndrome is caused by anatomic variation or due to piriformis overuse/tension. Piriformis syndrome diagnosis exams include, a positive Lase?gue test, where the healthcare professional�extends the patient�s leg passively, while the patient is lying supine,�test is positive if the maneuver is limited by pain, and through the use of tenderness and palpable tension in piriformis muscle which elicits symptoms.
Peroneal nerve entrapment is a condition which occurs when the peroneal or the fibular branch of the sciatic nerve are compressed at the fibular head. Tinel�s sign may be present at the fibular region of the head and/or neck. Peroneal nerve entrapment generally affects the common peroneal nerve, therefore, motor and sensory symptoms may manifest, including, weakness of the ankle dorsiflexion and eversion, or the tibialis anterior. Other symptoms of peroneal nerve entrapment may include sensory disruption on the dorsum of the foot and lateral aspect of the calf. Common peroneal nerve entrapement at the fibular head is the most common nerve entrapment syndrome in the lower extremities.
Tarsal tunnel syndrome, also known as posterior tibial neuralgia, is a condition caused by the compression of the tibial nerve as it travels through the tarsal tunnel, found along the region of the inner leg, posterior to the medial malleolus, or the bump on the inside of the ankle. Tarsal tunnel syndrome can manifest symptoms of pain and discomfort, burning or tingling sensations, and numbness along the big toe and the first three toes. However, symptoms may vary slightly depending on the area of compression, where the entire foot may manifest the symptoms previously described. Other symptoms associated with posterior tibial neuralgia include sensory changes in the sole of the foot. Tinel�s sign may be present with percussion posterior to the medial malleolus. The exact cause of tarsal tunnel syndrome may be difficult to determine and it is essential to receive a proper diagnosis to determine the source of the symptoms.
Radiculopathy
Radiculopathy is a mononeuropathy,�a condition that impacts only a single nerve or nerve group outside the brain and spinal cord, which affects the movement of or sensation in one specific area. It is often associated with neuropathy involving spinal nerve roots and presents as changes in sensory and/or motor function affecting a single or a few nerve root level(s). The most common types of radiculopathies include: sciatica and cervical radiculopathy. The most prevalent causes of radiculopathy include, disc herniation, osteophytes, spinal stenosis, trauma, diabetes, epidural abscess or metastasis, nerve sheath tumors, such as schwannomas and neurofibromas, Guillain-Barre? syndrome, Herpes Zoster, or shingles, Lyme disease, cytomegalovirus, myxedema and/or thyroid disorder, and idiopathic neuritis.
Narrowing down some of the most common causes of radiculopathy, symptoms can manifest due to disc herniation which most commonly affects the nerve roots along the C6, C7, L5 & S1 vertebrae of the spine, spinal stenosis and lumbar stenosis which may produce neurogenic claudication, and pain and weakness with ambulation. Cervical stenosis may present with mixed radiculopathy and myelopathy due to long tract involvement. Symptoms may also manifest due to trauma, because it may lead to compression, trauma or avulsion of the nerve roots, diabetes, which is most�likely to cause a polyneuropathy, but mononeuropathy is possible, and Herpes Zoster, or shingles, most often on the trunk, accompanied by vesicular lesions in a single dermatome. If pain persists past vesicular regression, radiculopathy may instead be considered post-herpetic neuralgia.
Patients with a history of radiculopathy will often complain of burning pain or tingling sensations which radiates or shoots down an affected area in a “dermatomal” pattern. Occasionally, patients will complain of motor weakness, however if onset is recent, there is often no motor involvement. The diagnosis of radiculopathy can depend on a variety of exams.�Most often, hypoesthesia may be present in the affected dermatome level. It’s recommended to�evaluate for pain, as light touch can be difficult for these patient�s to distinguish. Fasciculations and/or atrophy may be seen if radiculopathy is chronic, due to the lower motor neuron being compressed or impinged. Motor weakness may be seen in muscles innervated by the same root level. Orthopedic tests for the diagnosis of radiculopathy may include: the straight-leg raise test (SLR), where pain between 10 to 60 degrees likely indicates nerve root compression, the�Well-leg raise/Crossed straight-leg raise test (WLR), where if positive, 90 percent specificity for L/S nerve root compression may be present, the Valsalva Maneuver, where its considered positive if there is an increase in radicular symptoms, and spinal percussion, where pain may indicate metastatic disease, abscess or osteomyelitis.
How to Do the Motor Examination for Neuropathy
How to Do the Sensory Exam for Neuropathy
How to Test Reflexes
Specific radiculopathy patterns may also develop as a result of different regions being affected. Radiculopathy along the T1 can cause Horner�s syndrome, a combination of symptoms caused by the disruption of a nerve pathway from the brain to the face and eye on one side of the body. This is due to its effect on cervical sympathetic ganglia, includind ptosis, miosis, anhidrosis. Radiculopathy below the L1, can cause Cauda Equina syndrome, a condition caused by damage or injury to the bundle of nerves found below the end of the spinal cord, known as the cauda equina. This type of radiculopathy may manifest symptoms of saddle anesthesia, sensory loss in the S2-S5 distribution, urinary retention or overflow incontinence, constipation, decreased rectal tone or fecal incontinence, and loss of erectile function. Individuals with these signs and symptoms must be referred for emergency care immediately to prevent permanent dysfunction.
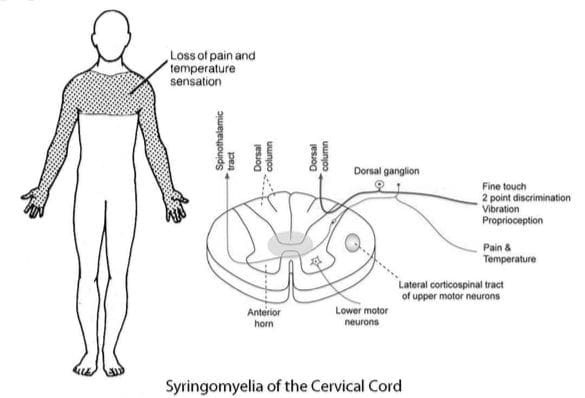
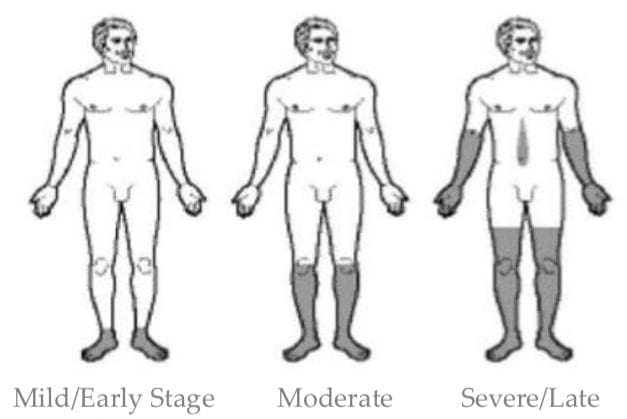
Other patterns of neuropathy can include the cape/shawl distribution of symptoms, identified by an intramedullary lesion, such as syringomyeli, intramedullary tumor and central cord damage. Stocking and glove distribution of symptoms may manifest as a result of diabetes mellitus,�B12 deficiency, alcoholism and/or hepatitis,�HIV, and thyroid dysfunction and/or myxedema.
The cape/shawl pattern of neuropathy is characterized by symptoms occurring due to an intramedullary lesion, such as a tumor, syringomyelia or a hyperextension injury in patient with C/S spondylosis. It can also be characterized by loss of pain and temperature sensation in C/T dermatomes because of the arrangement of the lateral spinothalamic tract. The stocking and glove pattern may progress gradually depending on its specific stage. It can also be characterized as a symmetrical polyneuropathy, where the feet and legs are generally affected first, followed by the hands and arms. A vibration-like sensation in the smallest toes are also typically the first to go and the neuropathy symptoms may progress across the foot to the big toe and then upward through the ankle and leg, then hands, arms and finally to the trunk if the condition becomes severe. The most likely cause of this pattern may be attributed to diabetes mellitus, but other possible causes include, B12 deficiency, alcoholism, HIV, chemotherapy treatment, thyroid dysfunction and multiple other causes.
Diabetic Neuropathy
Diabetic neuropathy is medically defined as a collection of nerve damaging disorders associated with diabetes. These conditions are believed to occur as a result of a diabetic microvascular injury involving the small blood vessels, known as the vasa nervorum, which supply the nerves. Additionally, macrovascular conditions have also been considered to accumulate and cause diabetic neuropathy.�Diabetic neuropathy often presents as a polyneuropathy, or the simultaneous damage or disease of many peripheral nerves throughout the body, but it can also present as a mononeuropathy, usually with acute onset. Diabetic neuropathy most commonly affects the CN III, femoral and sciatic nerves. Diabetic neuropathy can affect all peripheral nerves, including the sensory neurons, motor neurons and, although rarely, the autonomic nervous system. As a result, diabetic neuropathy can affect all organs and systems, as these are all innervated. Diabetic neuropathy can manifest into a wide array of symptoms, including, but not limited to, pain, burning or tingling sensations, numbness, dizziness and trouble with balance.
Demyelinating Neuropathies
Demyelinating neuropathies can be individually defined by its two types: Acute inflammatory demyelinating polyneuropathy, best known as�Guillain-Barre? syndrome, or Chronic inflammatory demyelinating polyneuropathy.�Guillain-Barre? syndrome, abbreviated as AIDP, is identified as a rapid-onset muscle weakness caused when the immune system damages, harms or destroys the peripheral nervous system. Onset has been reported by around one to two weeks following viral infection with progressive weakness, loss of DTRs/areflexia, paresthesia in the hands and feet, more motor involvement than sensory, potential autonomic fiber involvement, elevated CSF protein, and EMG/NCV studies indicating demyelination.�Guillain-Barre? syndrome may require treatment with plasmapheresis or IV Ig therapy.�Chronic inflammatory demyelinating polyneuropathy, abbreviated as CIDP,�is identified as an acquired immune-mediated inflammatory disorder of the peripheral nervous system which appears similar to AIDP but does not follow infection. Symptoms must be present for at least 8 weeks for this diagnosis to be considered positive.�Anti-inflammatory treatments may help treat CIDP.
The scope of our information is limited to chiropractic as well as to spinal injuries and conditions. To discuss the subject matter, please feel free to ask Dr. Jimenez or contact us at 915-850-0900 .
Curated by Dr. Alex Jimenez
Additional Topics: Sciatica
Sciatica is medically referred to as a collection of symptoms, rather than a single injury and/or condition. Symptoms of sciatic nerve pain, or sciatica, can vary in frequency and intensity, however, it is most commonly described as a sudden, sharp (knife-like) or electrical pain that radiates from the low back down the buttocks, hips, thighs and legs into the foot. Other symptoms of sciatica may include, tingling or burning sensations, numbness and weakness along the length of the sciatic nerve. Sciatica most frequently affects individuals between the ages of 30 and 50 years. It may often develop as a result of the degeneration of the spine due to age, however, the compression and irritation of the sciatic nerve caused by a bulging or herniated disc, among other spinal health issues, may also cause sciatic nerve pain.

EXTRA IMPORTANT TOPIC: Chiropractor Sciatica Symptoms